Abstract
Introduction
Deliberate self-poisoning (DSP) using drugs is the preferred method of suicide at a global level. Its investigation is hampered by limited sample sizes and data reliability. We investigate the role of the US FDA Adverse Event Reporting System (FAERS), a consolidated pharmacovigilance database, in outlining DSP habits and toxidromes.
Methods
We retrieved cases of ‘intentional overdose’ and ‘poisoning deliberate’ from the FAERS (January 2004–December 2021). Using descriptive and disproportionality analyses, we estimated temporal trends, potential risk factors, toxidromes, case-fatality rates and lethal doses (LDs) for the most frequently reported drugs.
Results
We retrieved 42,103 DSP cases (17% fatal). Most cases were submitted in winter. Reports of DSP involved younger people, psychiatric conditions, and alcohol use, compared with non-DSP, and fatality was higher in men and older patients. Suspected drugs were mainly antidepressants, analgesics, and antipsychotics. Multiple drug intake was recorded in more than 50% of the reports, especially analgesics, psychotropics, and cardiovascular agents. The most frequently reported drugs were paracetamol, promethazine, amlodipine, quetiapine, and metformin. We estimated LD25 for paracetamol (150 g).
Conclusion
Worldwide coverage of the FAERS complements existing knowledge about DSP and may drive tailored prevention measures to timely address the DSP phenomenon and prevent intentional suicides.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The study of deliberate self-poisoning is hampered by ethical and data collection problems. Spontaneous reports allow hypotheses regarding risk factors, toxidromes, and lethality to be generated. |
Deliberate self-poisoning was more reported in young individuals with psychiatric diagnoses, but the reported fatality rate of DSP was higher in adult males with alcohol concomitance. Multiple drug intake occurred in more than 50% of DSP cases. |
We characterized the toxidromes of the most reported ingestants and derived an estimation of lethal dose for paracetamol (LD25 ≈ 150 g). |
1 Introduction
Suicidal acts are one of the leading causes of years of life lost worldwide [1], with the numbers of both completed and attempted suicides growing steadily in the US and around the world [2,3,4]. Methods employed in suicidal acts depend on culture [5] and means availability [6], but deliberate self-poisoning (DSP) is the preferred approach almost everywhere [6,7,8,9]. Its case-fatality rate (\(CFR= \frac{N^\circ deaths}{N^\circ attempts}\)) is 2% in the US: DSP contributes to 59.4% attempts and 13.5% deaths, and firearms and hanging contribute to 8.8% attempts and 75.3% deaths [6]. Nonetheless, distinct drug classes differ strongly in their CFR because of different availability, toxidrome, and lethal dose (LD; dose at which a given percentage of subjects will die). These differences are still poorly characterized [10].
For ethical motives, premarketing data on toxidromes and lethality have been primarily collected from studying rats and mice, studies that were suspended on 17 December 2002, to promote the implementation of more ethical methods [11]. Therefore, data on LDs in humans are scarce and only come from the postmarketing setting. Sources focusing on fatal intoxication are forensic autopsy records (integrating circumstantial, autoptic, and toxicological data), forensic toxicology databases (collecting post-mortem blood levels), and the Office for National Statistics. Forensic studies accurately report the causes and manner of death inferred from comprehensive post-mortem investigations but usually address small single-center samples [12,13,14,15,16] and search for few drugs [17,18,19]. Databases reporting toxicological results present data from multiple centers, but not always allow to infer the intention behind the intoxication (i.e., whether homicidal, accidental, or suicidal) [20], as post-mortem blood levels are not representative of ante-mortem levels or of doses taken [20,21,22]. National databases are useful in determining the manner of death as the International Classification of Diseases, Tenth Revision (ICD-10), used to code mortality data worldwide, includes multiple poisoning-related codes discriminating the intent of exposure. However, whenever evidence is not sufficient to identify with high confidence a death by drug intoxication as a suicide, coding the death as accidental or unintentional is usually preferred [23,24,25]. Therefore, many accidental deaths by drug intoxication likely refer to unrecognized intentional poisoning acts, and suicide is likely to be underestimated due to its less forensically and behaviorally overt nature [26].
Sources focusing on non-fatal intoxication are high-quality registries collecting information about DSP cases that required medical consultation, such as those collected by poisoning centers (passively collecting telehealth consultations) [27, 28], and the Toxicology Investigators Consortium (ToxIC: https://www.toxicregistry.org/; integrating bedside data). Besides the high-quality, these registries are highly selected and are often not representative of the general population exhibiting suicidal behavior. When investigating DSP, we are hampered by the difficulties in integrating data about fatal and non-fatal intoxications due to different sources and different data collected.
The US FDA Adverse Event Reporting System (FAERS) is a consolidated pharmacovigilance database gathering worldwide spontaneous reports of adverse events and medication errors following drug administration. It is employed to investigate unexpected drug reactions and it was recently explored to investigate drug misuse and abuse, including DSP [29], suicide ideation as an adverse reaction [30,31,32], and suicide prodromes [33]. We aimed to investigate its potential use as a complementary source to characterize the DSP phenomenon, including both fatal and non-fatal cases, with a particular focus on risk factors, temporal trends, medications used, toxidromes and LDs. Its ability to gather detailed spontaneous reports with a cheap and real-time strategy will constitute a powerful ally in the development of targeted preventative approaches to reduce fatalities and severe sequelae [23].
2 Materials and Methods
2.1 Study Design
We performed a composite pharmacovigilance study on the FAERS, including a descriptive analysis to identify drugs involved in DSP and potential risk factors, a time-series analysis to verify potential seasonality (i.e., a regular season-dependent pattern that recurs over years), a network analysis to investigate multiple drug intake, a disproportionality analysis to characterize toxidromes, and a logistic regression to estimate LDs. All analyses and visualizations were obtained using R version 4.1.2 (The R Foundation for Statistical Computing, Vienna, Austria).
2.2 Case Retrieval
We downloaded FAERS quarterly data [34] from January 2004 to December 2021, and preprocessed them for drug standardization, deduplication, and selection of the latest case version. The preprocessing strategy is documented in previous works [35]. Adverse events and reasons for use were coded using preferred terms (PTs, grouped into high-level group terms [HLGT]) from the hierarchical Medical Dictionary for Regulatory Activities (MedDRA®, version 25.0, developed under the auspices of the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use).
To specifically retrieve DSP reports and minimize potential misclassifications, we excluded drug-induced suicidal ideation (possibly enacted through non-drug-related media) and accidental overdose (i.e., overdose without self-injurious intent). We searched for ‘intentional overdose’ and ‘poisoning deliberate’ in the event and reason for use (indication) fields. We limited our investigation to drugs included in the Anatomical Therapeutic Chemical (ATC, 2022) classification [36], restricting to primary suspects to avoid the inclusion of medications recorded as concomitant and not overdosed.
2.3 Drugs Involved
We identified drugs involved in > 1% of DSPs, both by active ingredient and grouped by their ATC third-level class, and calculated their reported \(\mathrm{CFR}= \frac{\mathrm{N}^\circ \mathrm{ deaths}}{\mathrm{N}^\circ \mathrm{ reports}}\). To investigate polydrug intoxication, we visualized the co-reporting of multiple suspect drugs using a network analysis [37], with nodes representing drugs (≥ 1% of DSP reports) and links representing drug–drug combinations (≥ 100 reports). Nodes were color-coded by a multilevel algorithm (i.e., Louvain algorithm), identifying groups of drugs more often reported together in the same DSP report rather than with other drugs, to identify clusters of polydrug intoxication.
2.4 Risk Factors
To identify potential risk factors, we performed descriptive analyses comparing DSP and non-DSP reports, fatal and non-fatal DSP reports, and specific (for the five most reported drugs) and general DSP reports. We compared demographics (sex, age, weight, country), reporting characteristics (reporter occupation, submission), outcome, alcohol use, and psychiatric comorbidity. We tested for statistical significance using the Chi-square test for categorical variables and the Kruskal–Wallis test for continuous variables, correcting with Holm–Bonferroni for multiple tests.
2.5 Time-Series
We visualized temporal trends for all DSPs and the five most reported drugs. To investigate seasonality, we performed a graphical time-series analysis considering monthly data on the event date (not always present) and the receival date (not always close to the event). To isolate the trend-cycle component from seasonal and irregular ones, we also performed a time-series decomposition considering a 12-period moving average process. We graphically represented resulting trend-cycle components of both attempted and completed events.
2.6 Toxidromes
To characterize toxidromes, we identified, for each of the 10 most reported drugs, the events most recorded in DSP (≥ 5% DSP reports). Because the MedDRA dictionary is characterized by high redundancy, we performed this operation at the HLGT level and selected those events that were more often reported when the drug of interest was overdosed than at therapeutic ranges. Finally, to avoid including events more often reported with overdose in general rather than with the specific drug of interest (e.g., death), we prioritized the events according to disproportional reporting (reporting odds ratio, ROR025 > 1) relative to other drugs in the FAERS, a common pharmacovigilance approach [38].
2.7 Lethal Dose (LD) Estimation
For the five most reported drugs, we estimated LDs. We retrieved the dosages taken in the DSP attempt considering the six dose-related fields from the FAERS: ‘dose_amt’ and ‘dose_unit’ with the amount of drug reported; ‘dose_freq’, with the frequency of administration; ‘cum_dose_chr’ and ‘cum_dose_unit’, with the cumulative dose; and ‘dose_vbm’, with further information as free text. These fields, filled out mainly as free text by reporters, may be heterogeneous in the way dose is reported (e.g., sometimes in grams, other times in number of pills). For each drug, each of the six fields was manually screened and information was translated to a dose in grams. We also considered cases in which two data entries were submitted for the same patient: one specifying the formulation strength and one specifying the number of ingested pills. We excluded, from LD estimation, all the reports recording only information about formulation strength or posology without recording the dose taken in the DSP attempt. The reports for which we could not be sure of the conversion to grams were excluded from the LD estimation. Using the reported dosages in grams, we performed a logistic regression between CFR and exposure levels, and calculated a pseudo-R2 to estimate the goodness-of-fit of the model [39].
3 Results
3.1 Case Retrieval
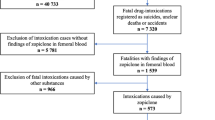
From 17,254,601 raw FAERS reports, 11,728,098 curated reports were finally retained, including 42,103 DSP reports (22,280 [52.9%], specifying a self-harm intent) [see electronic supplementary material (ESM) Table S1].
3.2 Drugs Involved
Most reported drug classes were antidepressants (14.0%), analgesics (11.0%), and antipsychotics (10.0%). The five most reported drugs were paracetamol (10.1%), promethazine (3.5%), amlodipine (3.4%), quetiapine (3.2%), and metformin (2.9%) (see Table 1). The CFR was highest for oxycodone (60.8%) and lowest for promethazine (0.5%) (see Fig. 1). Multiple drug intake (53.9%; 51.5% when excluding multiple drug intake exclusively due to one multi-ingredient medication) recorded a higher CFR (20.5% vs. 13.3% for single drug intake). Including secondary suspects, paracetamol was recorded in 7009 reports (16.7% DSPs) and hegemonized the multiple drug intake network (see Fig. 2), primarily in combination with other analgesics (ibuprofen, tramadol, hydrocodone) and alcohol. Two other clusters identified by the multilevel algorithm intertwined benzodiazepines, antidepressants, and antipsychotics. A fourth cluster included cardiovascular and metabolic drugs.
Reported case-fatality rate of drugs used to commit suicide. Drugs recorded as primary suspects in more than 1% of the DSP reports are shown on the y-axis, ordered by the number of DSP reports (in blue, right side of the pyramid plot). The reported case-fatality rate is visualized on the left side of the pyramid plot (in red). DSP deliberate self-poisoning
Multiple drug intake. Snapshot of the interactive network showing more frequent exposure (> 1%) as nodes, and more frequent polydrug intoxications (> 100) as links. More frequent drugs are represented by larger nodes and more frequent combined exposures are represented by more visible links. The nodes were clustered by color using a multilevel algorithm. We identified a pain cluster (pink), a cardiovascular cluster (green), and two psychotropic clusters (violet and blue). Only nodes with a link were included in the final graph, and in the snapshot, only drugs used in combination with paracetamol were colored. The interactive network is available at: https://osf.io/n5q8x/.
3.3 Risk Factors
Between DSP and non-DSP reports, we found significant differences in reporter (17.0% vs. 46.8% consumers), age (37 years [Q1 = 23 to Q3 = 51] vs. 58 years [42–70]; 12.3% vs. 2.6% teenagers), continent (47.7% vs. 14.8%, Europe; 40.2% vs. 74.8%, US), alcohol use (5.2% vs. 0.2%), psychiatric comorbidity (14.3% vs. 6.1%) (see ESM Table S2).
Among DSP reports, 7218 (17.3%) resulted in death. Fatal DSP reports were significantly different from non-fatal DSPs in sex (45.2% vs. 37.7% males), reporter (14.8% vs. 6.6% pharmacists), age (42 [30–54] vs. 36 [22–50] years), geographical area (65.5% vs. 35.5% North America), alcohol use (8.9% vs. 4.5%), and psychiatric comorbidity (9.6% vs. 15.3%). The most frequently reported drug was paracetamol, followed by oxycodone and bupropion in fatal intoxication, and promethazine and amlodipine in non-fatal intoxication (see ESM Table S3).
Between drug-specific DSPs, we found significant differences in sex (women: 75.3% promethazine, 67.1% paracetamol, 65.4% quetiapine, 56.7% amlodipine, 51.3% metformin vs. 61.2% of any reports of DSP), age (24 [18–33] promethazine, 31 [20–46] paracetamol, 42 [23–55] metformin, 47 [27–55] amlodipine vs. 37 [23–51]), and outcome (0.5% death, 0.3% life-threatening promethazine; 13.9%, 40.1% amlodipine; 20.3%, 32.5% metformin; 24.3%, 9.4% paracetamol vs. 17.1%, 15.3%). Alcohol use was highest in paracetamol (7.8%) and lowest in promethazine (0.1%). Psychiatric comorbidity was highest in quetiapine (25.1%) (see ESM Table S4).
Most DSP reports were submitted from the US and Europe, recording a higher fatality rate in the US (see ESM Fig. S1). We observed local differences in recorded drugs: paracetamol > 60% of DSPs in Ireland, promethazine > 50% of DSPs in Sweden (98.8% of promethazine DSPs), and metformin > 20% of DSPs in Turkey (data not shown).
3.4 Time-Series
Trend analysis showed an ongoing increase in DSP reporting to the FAERS, with local peaks in 2007–2008 and 2019–2020. The graphical representation of the monthly-spaced time series showed higher reporting peaks in December and January and lower peaks in June. Varenicline peaked in 2011, promethazine in 2019, and paracetamol in 2007, 2015, 2020 (see ESM Figs. S2–S4),
3.5 Toxidromes
To characterize toxidromes, we identified the events associated with the specific drug and more often reported in DSP (overdose) than at therapeutic ranges (see Fig. 3).
Toxidromes. The 10 most frequent suspected drugs in order of ATC code are shown on the x-axis, and events (at their MedDRA HLGT level) clustered by SOC are shown on the y-axis. A point was shown in the intersection if the drug was disproportionally reported with the event (on the entire FAERS), with a size proportional to the percentage of intentional overdose reports recording the event (i.e., a large dot identifies an event that occurs in a high percentage of the drug overdose report), and a white-red gradient based on the ratio between the reporting rate in intentional overdoses versus the therapeutic use (i.e., a red dot identifies an event that occurs much more often as a toxic effect than as an adverse effect). We included only events present in at least 5% of the drug overdose reports. Rows without disproportionalities are not shown. ATC Anatomical Therapeutic Classification, HLGT high-level group terms, MedDRA Medical Dictionary for Regulatory Activitives, SOC System Organ Class, FAERS US FDA Adverse Event Reporting System
Amlodipine DSPs recorded vascular (720 hypotension, 358 shock), metabolic (249 metabolic acidosis, 96 lactic acidosis, 90 hyperglycemia, 65 hypoglycemia, 48 hypokalemia), renal (263 acute kidney injury, 71 anuria), cardiac (184 bradycardia, 133 tachycardia, 132 cardiogenic shock, 112 cardiac arrest), and respiratory conditions (140 pulmonary edema, 101 respiratory failure, 96 non-cardiogenic pulmonary edema).
Metformin DSPs recorded metabolic (780 lactic acidosis, 315 hypoglycemia, 264 metabolic acidosis, 57 hyperglycemia, 46 hyperkalemia), vascular (283 hypotension, 116 shock), renal (241 acute kidney injury, 104 renal failure), gastrointestinal (120 vomiting), and respiratory conditions (75 tachypnoea, 60 respiratory failure).
Paracetamol recorded gastrointestinal (496 vomiting, 253 nausea) and hepatic conditions (342 acute hepatic failure, 189 hepatic failure).
Promethazine recorded neurological (183 depressed level of consciousness, 174 somnolence), movement (154 akathisia), perception (105 hallucination), ocular (95 mydriasis), anxiety disorders (91 anxiety, 88 agitation), and deliria (77 confusional state).
Quetiapine recorded neurological disorders (241 somnolence, 213 coma) and 47 pneumonia aspirations.
3.6 LD Estimation
Paracetamol exposure levels were specified in 1595 reports, with a median dose of 16 [Q1 = 10 to Q3 = 36] g. Interpolating them with CFR, we estimated LD25 ≈ 150 g, LD50 ≈ 250 g, LD75 ≈ 325 g, with a pseudo-R2 of 0.07 (see Fig. 4).
Lethal dose estimation for paracetamol. Observational data regarding doses (in grams) and fatality were fitted to a logistic model to estimate the lethal dose for different percentages. Reports were then grouped by dose (in logarithmic intervals—narrow near 0 and wider for higher doses—to account for the exposure distribution skewed to the right, i.e., many reports record lower doses, few record higher doses) and the case-fatality rate for each group was calculated. For each dose interval, we plotted a point over the logistic, with the x-coordinate the midpoint between dose limits, the y-coordinate the estimated case-fatality rate, and size of the logarithm of the number of reports. The pseudo-R2 of the model is 0.07, suggesting a low goodness of fit
Promethazine was recorded in only seven fatal cases and we did not estimate any models. Amlodipine (dose was specified in 824 reports) was taken at 0.3 [0.15–0.5] g, with an estimated LD10 ≈ 0.25 g and LD20 ≈ 1.00 g, with a pseudo-R2 of 0.66 (see ESM Fig. S5). Quetiapine (dose was specified in 668 reports) was taken at 2.26 [0.6–8.4] g with a negative slope, with a pseudo-R2 of 0.07 (see ESM Fig. S6). Metformin (dose was specified in 645 reports) was taken at 40 [10–65] g and resulted in a non-informative logistic regression, with a pseudo-R2 of 0.00 (see ESM Fig. S7).
4 Discussion
4.1 The US FDA Adverse Event Reporting System (FAERS): A Complementary Source of Intoxication Data
The stable growth in the reporting of DSPs to the FAERS in the last two decades, primarily from the US and Europe, is plausibly related to both the evolution of spontaneous reporting systems and to the increase in suicides observed in the US [3]. Reassuringly, we observed no increase in fatal DSPs, supporting the efficacy of current preventative approaches focused on reducing the fatality of available means rather than the frequency of attempts. With more than 40,000 DSP reports at the end of 2021, the FAERS is emerging as an alternative source of fatal and non-fatal intoxication data, complementing already in-use forensic and non-forensic sources.
4.1.1 Monitoring Trends and Seasonality
FAERS data provide a source to timely and cheaply monitor variations in DSP reporting. We found a seasonality with higher peaks of reporting in the winter and lower peaks in June, and major peaks in DSP reporting in 2007–2008 and 2019–2020. Studies supporting winter [40] and spring peaks [41, 42] exist, and major events, such as the global financial crisis in 2007–2008 and the coronavirus disease 2019 (COVID-19) pandemic in 2019–2020, may indeed have precipitated cases of suicidal ideation [43]. Nonetheless, whether trends in the reporting represent trends in events is highly debatable. When investigating the available event dates, most of these results were lost. Therefore, speculations about DSP trends should carefully consider the kind of date chosen, and also the potential bias resulting from regulatory actions and mass media communications [44]. For example, we observed a peak in varenicline DSP in 2007, in correspondence with an FDA investigation on varenicline-induced suicidal ideation and self-harm. The FDA added a black-box warning to the varenicline package insert in 2009, but subsequent studies failed to establish causality and the warning was removed in 2016 [45].
4.1.2 Identifying Targets for Preventative Approaches
FAERS intoxication data provide a promising source to identify drugs reported in DSP and drive preventative actions. Coherently with recent studies [46], the most common means for DSP were psychotropic (i.e., antidepressants, antipsychotics, anxiolytics, and sedatives) and analgesic drugs (i.e., paracetamol, opioids, and NSAIDs), together with antiepileptics, antihistamines, amlodipine, metformin, and varenicline. Paracetamol was by far the most widely recorded drug, at least partly because of its availability. Anxiolytics and opioids played a less important role in DSP compared with previous findings [10]. This inconsistency can have both temporal and geographical explanations since FAERS data allow information to be obtained for quite an extended period (2004–2021) from many different countries.
More than 50% of DSP reports recorded multiple substance intake (elsewhere estimated at 56.3% [47]), which was associated with a higher CFR. The network analysis highlighted a trend to use drugs of the same therapeutic area together (i.e., psychotropic, analgesic, and cardiovascular/metabolic). This peculiar pattern of use is plausibly explained by availability, with paracetamol being present in every house. The other available drugs depend on the pathologies diagnosed to the house inhabitants [48].
Drugs from the pain cluster showed an important role in fatal DSPs (oxycodone, 60.8% of fatalities), because of both their lethality and their potential for abuse, but plausibly also for resistant pain as a risk factor for committing suicide [49]. Another drug with a high reported fatality was bupropion (CFR 34.6%), plausibly because it is more available to people with a higher determination towards suicide since it is approved to palliate suicidal ideation. Patients taking bupropion to commit suicide may therefore take higher doses, combine multiple drugs, or attempt suicide when and where it is more difficult for healthcare professionals to intervene. These results were in line with previous findings [10] that opioid and antidepressant overdoses are more lethal than overdoses with other pharmaceuticals, and point to the need for further preventative interventions targeting these drug classes.
4.1.3 Identifying Potential Risk Factors
A large body of research has focused on the demographics of suicide victims, the methods people use to take their own lives, and the means of prevention. It is well known that traumatic deaths are common in male victims, whereas females prefer less violent deaths and less fatal means, although this depends on age, nationality, and mental health status [1, 6, 50].
FAERS rich data allow to further characterize DSP demographics. We found a higher reporting of DSP in young adults (37 [23–51]), with fatalities being reported more often in older men. Both alcohol use and psychiatric comorbidities were more common in DSPs.
Alcohol represents the psychoactive substance most commonly identified in blood samples in suicidal poisonings [48, 51]. The recording of alcohol use, plausibly describing acute consumption of moderate-to-high doses, was more frequent in fatal DSPs. Alcohol may therefore not only be associated with an increased risk of suicide attempts [52] but also with a greater intent to die, although existing evidence suggests that at very high alcohol doses less lethal means are chosen [53].
The finding that psychiatric comorbidity was less recorded in fatal than in non-fatal DSPs may be related to not only the prophylactic value of the psychiatric care [54] but also to the fact that relapsing suicide attempters are usually diagnosed with a psychiatric condition and may contribute with multiple reports of attempted suicide.
4.1.4 Characterizing Drug-Specific Deliberate Self-Poisonings
FAERS data may also be used to characterize drug-specific DSPs, including their toxidrome.
Paracetamol overdose represents the most common DSP in the industrialized world [55] and a growing problem in developing countries [56]. Coherently, paracetamol was the main drug reported as a primary suspect in both fatal and non-fatal DSP cases. In 54% of cases, paracetamol recorded at least one concomitant (primarily analgesics and alcohol). It is the drug involved in DSP with the highest concomitance with alcohol use, with potential dose-dependent interactions [57, 58]. Being the most available drug, its temporal trend and demographic distribution shape and reflect the temporal trend and the demographic distribution of DSPs. It showed peaks of reporting in 2007, 2015 and 2020, and a higher contribution by women and younger people. The association of paracetamol overdose with hepatic disorders (e.g., acute hepatic failure) and nausea, coherently with the literature [59], supports the utility of our method to identify toxicity events. Its reported CFR was 24.3%, and higher in multiple drug intake (32%). This reported CFR, much higher than in clinical trials [59], may be related to a differential reporting rate of serious and non-serious DSP cases.
Promethazine DSP reports were mostly submitted in Sweden in 2018–2019. Indeed, in Sweden, both promethazine sales and DSP cases have recently peaked [60]. Promethazine overdoses are much more commonly reported in women (75.3%) and affect the youngest population among the five drugs investigated (24 [18–33]). In 37% of cases, it was reported with at least one concomitant, the most frequent being zopiclone, propiomazine, and paracetamol. Its reported CFR was the lowest (0.5%; only seven fatal cases). Although we found that almost all DSP reports with promethazine specified suicide as a reason for use, this active ingredient is used in many different formulations as a recreational (euphoric and hallucinogenic) drug (e.g., ‘purple drank’ [61]). A study on promethazine abuse/misuse in EudraVigilance (the European spontaneous reporting system) found 557 cases and a reported CFR of 55% [62]. This difference in the reported outcome should be further investigated and may be related to potential differences in the relevant catchment areas and peculiar pattern of drug use. We found the main feature of promethazine overdoses was delirium, associated with akathisia, anxiety, confusion, somnolence, and mydriasis, which were also the main events reported in observational studies [62]. We could not calculate the dose-lethality relationship since we only found seven fatal cases.
Amlodipine (a concomitant in at least 61% of cases) and metformin (a concomitant in at least 39% of cases) instead had a higher contribution by men and older people. Metformin recorded a higher reported CFR (20.3% death and 32.5% life-threatening overdoses), while amlodipine recorded fewer deaths (13.9%) but more life-threatening events (40.1%). Metformin overdose was associated primarily with acidosis, and also with shock, frequently concomitant with severe renal impairment. This toxidrome is commonly known as MALA (metformin-associated lactic acidosis), an event that rarely occurs at therapeutic doses [63] in the lack of independent risk factors [64]. Amlodipine was associated primarily with shock and also with acidosis. This toxidrome includes severe hypotension and reflex tachycardia, and may culminate in pulmonary edema and cardiovascular shock with fatal outcome [65]. Furthermore, we found that both drugs were reported with respiratory failure and acute kidney injury, and were reported to affect glycemia (mainly increased in amlodipine, decreased in metformin) and hypokalemia in amlodipine and hyperkalemia in metformin). Finally, metformin was associated with vomiting, while amlodipine was associated with cardiac arrhythmias and heart failure. In 119 cases they were reported together.
Quetiapine is frequently used for conditions at high suicide risk, such as psychotic and mood disorders [66]. The 2-week delay in therapeutic effect requires careful monitoring of these patients, especially in the early stages of treatment and following dosage changes. Quetiapine recorded a higher contribution by women (65.4%) and was often reported together with paracetamol, venlafaxine and diazepam, primarily with sedation and coma, and with aspiration pneumonia. In general, the reported signs and symptoms of quetiapine DSP can be attributed to enhancement of the known pharmacological effects of the drug [67].
4.1.5 Estimating LDs
FAERS data also include information about the therapy regimen and dosages. It may therefore allow a dose–lethality relationship in humans to be estimated.
For paracetamol, the high number of reports with a specified dose, and the heterogeneity in exposure levels, allowed us to investigate the relationship between doses and lethality. Our model estimated LD25 ≈ 150g, LD50 ≈ 250g, and LD75 ≈ 325g. Although it allowed the general trend of fatality in DSPs to be predicted, the paracetamol exposure level was only able to explain very little of the variability in individual outcomes, which plausibly depends also on weight, comorbidities, concomitants, dilution in time, medical intervention, and route of administration (e.g., a few cases specified that the drug was smashed and snorted). With FAERS data, which are often incomplete and unverified, it is difficult to have an homogenous compilation of all the fields, and therefore it is difficult to design more accurate models. Although the Rumack–Matthew nomogram already predicts the risk of hepatotoxicity associated with paracetamol concentration [68], it does not accurately work in case of repeated overdose, when the formulation is slow-release, when the time of ingestion is unknown, or when patients present after more than 24 h. Therefore, new tools have been developed to predict the risk of hepatotoxicity based on reported doses [56]. Our model may lead to the development of a complementary tool able to predict lethality.
The low number of reports specifying the accurate dose of intoxication for the other drugs did not allow us to obtain a satisfying logistic regression model. It is possible that, in the future, the collection of more data will allow a better logistic regression to be performed.
4.2 Limitations and Strengths
Our study has limitations inherent to spontaneous reporting systems analysis (e.g., underreporting, unverified and incomplete reports, notoriety bias). Therefore, the use of the FAERS is appropriate only to generate hypotheses to be verified by further studies.
A first, more specific, limitation lies within the definition of the query for case retrieval. Our study focused on DSP, identified using the MedDRA terms ‘self-poisoning deliberate’ and ‘intentional overdose’. In this way, we deliberately excluded unintentional pharmaceutical overdose deaths (estimated to be 83% of the total overdose deaths [69]) and accidental overdoses due to intentional exposure (e.g., a patient taking the dose twice because forgetting the first administration should be reported using more appropriate combinations of terms: ‘product dose confusion’, ‘extra dose administered’, ‘accidental overdose’). Instead, we could not exclude a priori that our query might retrieve some non-suicidal intentional overdose reports as DSP (e.g., opioid abuse [70], and promethazine to experience hallucinations [61]), but the fact that, a posteriori, most DSP reports retrieved also recorded suicide-related terms reassured us that this was a minor problem.
A second more specific limitation lies with the possibility that some specific systematic biases linked to suicide may confound our analyses. For example, it is possible that fatal attempts were reported more often than non-fatal attempts, leading to the reported CFR being an overestimation of the real fatality rate. On the other side, it is plausibly easier to obtain information on the dosage for non-fatal cases, resulting in underestimated (lower) dose-lethality curves. Furthermore, many factors, apart from the ingested dose, may influence the outcome, including the concomitants, the lack or delay of medical intervention, and the route of administration. Spontaneous reports do not allow us to confidently take them into account.
Because of its general scope, this study may have overlooked specific drugs that, while not being the most reported, are particularly lethal, on the rise [71, 72], or commonly abused in parties [73]. Furthermore, even if the FAERS gathers reports from the entire world, 94% of the cases are from North America and Europe, and its representativity for other continents, and in particular for the global South, is limited.
Apart from these limitations, spontaneous reporting systems allow the inexpensive collection of timely and large amounts of information from the entire world and from complex and heterogeneous conditions. Compared with other sources of forensic data, they allow the collection of information on both fatal and non-fatal events, and on any kind of drug. The high number of rich-in-information reports gathered by the FAERS may be used for a drug-by-drug assessment useful to design more informed and specific regulatory interventions. Its real-time representativity, in particular, may detect emerging problems in a timely manner and drive appropriate interventions to limit intentional overdose deaths. The dosage information, when enough data are gathered and accurately cleaned, may also be useful in estimating real-world LDs. Our methodology may therefore be applied to the FAERS to investigate more specific emerging problems. It could also be applied to other, more representative databases to gain a better insight on specific countries or regions.
5 Conclusion
Using the FAERS to characterize the DSP reports, we observed peaks in 2007–2008 and 2019–2020, with a higher contribution by young individuals and psychiatric diagnoses, and a higher fatality in older men and with alcohol use. We observed multiple drug intake in more than 50% of DSP cases, the most frequent co-ingestant being paracetamol, and with combined drugs usually restricted to a specific therapeutic area (e.g., analgesics, psychotropics, cardiovascular agents). Polydrug intoxication with analgesics reported the highest fatality. The five drugs most reported in DSP cases were paracetamol (hepatotoxic), promethazine (inducing delirium, but almost never fatal), amlodipine (inducing shock), quetiapine (inducing sedation and coma), and metformin (inducing acidosis). Due to the scarcity of detailed information about doses, we could only estimate LDs for paracetamol (LD25 ≈ 150 g). The continuous collection of DSP reports, possibly with higher quality and more complete compilation, will allow an even richer profile of the DSP phenomenon to be derived from the FAERS, integrating the evidence already gathered by currently used data sources.
References
Naghavi M. Global, regional, and national burden of suicide mortality 1990 to 2016: systematic analysis for the Global Burden of Disease Study 2016. BMJ. 2019;364: l94.
Hedegaard H, Curtin SC, Warner M. Suicide mortality in the United States, 1999–2019. NCHS Data Brief. 2021;1–8.
Bommersbach TJ, Rosenheck RA, Rhee TG. National trends of mental health care among US adults who attempted suicide in the past 12 months. JAMA Psychiat. 2022;79(3):219–31.
Yip PSF, Zheng Y, Wong C. Demographic and epidemiological decomposition analysis of global changes in suicide rates and numbers over the period 1990–2019. Injury prevention. BMJ. 2022;28:117–24.
Kawashima Y, Yonemoto N, Inagaki M, Yamada M. Prevalence of suicide attempters in emergency departments in Japan: a systematic review and meta-analysis. J Affect Disord. 2014;163:33–9.
Conner A, Azrael D, Miller M. Suicide case-fatality rates in the United States, 2007 to 2014: a nationwide population-based study. Ann Intern Med. 2019;171:885–95.
Bergen H, Hawton K, Waters K, Cooper J, Kapur N. Epidemiology and trends in non-fatal self-harm in three centres in England: 2000–2007. Br J Psychiatry. 2010;197:493–8.
Bi B, Tong J, Liu L, Wei S, Li H, Hou J, et al. Comparison of patients with and without mental disorders treated for suicide attempts in the emergency departments of four general hospitals in Shenyang, China. Gen Hosp Psychiatry. 2010;32:549–55.
Bilén K, Ottosson C, Castrén M, Ponzer S, Ursing C, Ranta P, et al. Deliberate self-harm patients in the emergency department: factors associated with repeated self-harm among 1524 patients. Emerg Med J. 2011;28:1019–25.
Miller TR, Swedler DI, Lawrence BA, Ali B, Rockett IRH, Carlson NN, et al. Incidence and lethality of suicidal overdoses by drug class. JAMA Netw Open. 2020;3: e200607.
Erhirhie EO, Ihekwereme CP, Ilodigwe EE. Advances in acute toxicity testing: strengths, weaknesses and regulatory acceptance. Interdiscip Toxicol. 2018;11:5–12.
Akhgari M, Kahfi MS, Akha HS. Analysis of intoxication deaths: causes and manners of death. Indian J Pharm Sci. 2019;81:32–8.
Kordrostami R, Akhgari M, Ameri M, Ghadipasha M, Aghakhani K. Forensic toxicology analysis of self-poisoning suicidal deaths in Tehran, Iran; trends between 2011–2015. Daru. 2017;25:15.
Sikary AK, Sasidharan A, Pillay VV, Andrade C. Prescription drug suicide in non-abusers: a 6-year forensic survey. Asian J Psychiatr. 2019;44:133–7.
Sinyor M, Howlett A, Cheung AH, Schaffer A. Substances used in completed suicide by overdose in Toronto: an observational study of coroner’s data. Can J Psychiatry. 2012;57:184–91.
Valipour R, Shekari A, Setareh M, Soltaninejad K. Pattern of suicide methods and postmortem toxicological findings in suicide-related deaths: a retrospective 7-year forensic-based study in Iran. Am J Forensic Med Pathol. 2021;42:23–9.
Darke S, Deady M, Duflou J. Toxicology and characteristics of deaths involving zolpidem in New South Wales, Australia 2001–2010. J Forensic Sci. 2012;57:1259–62.
Errico S, Bedocchi D, Drommi M, Barranco R, Bonsignore A, Ventura F. Forensic pathological study of methadone-related deaths in the Genoa (Italy) district: a six-year study. J Forensic Leg Med. 2021;79: 102149.
Steentoft A, Linnet K. Blood concentrations of clonazepam and 7-aminoclonazepam in forensic cases in Denmark for the period 2002–2007. Forensic Sci Int. 2009;184:74–9.
Jönsson AK, Söderberg C, Espnes KA, Ahlner J, Eriksson A, Reis M, et al. Sedative and hypnotic drugs–fatal and non-fatal reference blood concentrations. Forensic Sci Int. 2014;236:138–45.
Drummer OH, Kennedy B, Bugeja L, Ibrahim JE, Ozanne-Smith J. Interpretation of postmortem forensic toxicology results for injury prevention research. Inj Prev. 2013;19:284–9.
Walz L, Jönsson AK, Ahlner J, Östgren CJ, Druid H. Metformin—postmortem fatal and non-fatal reference concentrations in femoral blood and risk factors associated with fatal intoxications. Forensic Sci Int. 2019;303: 109935.
Snowdon J, Choi NG. Undercounting of suicides: where suicide data lie hidden. Glob Public Health. 2020;15:1894–901.
Chang S-S, Sterne JAC, Lu T-H, Gunnell D. “Hidden” suicides amongst deaths certified as undetermined intent, accident by pesticide poisoning and accident by suffocation in Taiwan. Soc Psychiatry Psychiatr Epidemiol. 2010;45:143–52.
Rockett IRH, Caine ED, Connery HS, D’Onofrio G, Gunnell DJ, Miller TR, et al. Discerning suicide in drug intoxication deaths: Paucity and primacy of suicide notes and psychiatric history. PLoS ONE. 2018;13: e0190200.
Rockett IRH, Caine ED, Connery HS, Nolte KB. Overcoming the limitations of “accident” as a manner of death for drug overdose mortality: case for a death certificate checkbox. Inj Prev. 2021;27:375–8.
Spiller HA, Appana S, Brock GN. Epidemiological trends of suicide and attempted suicide by poisoning in the US: 2000–2008. Leg Med (Tokyo). 2010;12:177–83.
Zakharov S, Navratil T, Pelclova D. Suicide attempts by deliberate self-poisoning in children and adolescents. Psychiatry Res. 2013;210:302–7.
Ding T, Chen ES. Mining drugs and indications for suicide-related adverse events. AMIA Annu Symp Proc. 2019;2019:1011–20.
Vakharia PP, Orrell KA, Lee D, Rangel SM, Lund E, Laumann AE, et al. Apremilast and suicidality—a retrospective analysis of three large databases: the FAERS, EudraVigilance and a large single-centre US patient population. J Eur Acad Dermatol Venereol. 2017;31:e463–4.
Cheng N, Rahman MM, Alatawi Y, Qian J, Peissig PL, Berg RL, et al. Mixed approach retrospective analyses of suicide and suicidal ideation for brand compared with generic central nervous system drugs. Drug Saf. 2018;41:363–76.
Gastaldon C, Raschi E, Kane JM, Barbui C, Schoretsanitis G. Post-marketing safety concerns with esketamine: a disproportionality analysis of spontaneous reports submitted to the FDA adverse event reporting system. Psychother Psychosom. 2021;90:41–8.
Nazir A, Ichinomiya T, Miyamura N, Sekiya Y, Kinosada Y. Identification of suicide-related events through network analysis of adverse event reports. Drug Saf. 2014;37:609–16.
FDA. FAERS quarterly data extract files. 2022. https://fis.fda.gov/extensions/FPD-QDE-FAERS/FPD-QDE-FAERS.html. Accessed 20 Mar 2022.
Gaimari A, Fusaroli M, Raschi E, Baldin E, Vignatelli L, Nonino F, et al. Amyotrophic lateral sclerosis as an adverse drug reaction: a disproportionality analysis of the food and drug administration adverse event reporting system. Drug Saf. 2022;45:663–73.
WHO Collaborating Centre for Drug Statistics Methodology. ATC classification index with DDDs. 2022. https://www.whocc.no/atc_ddd_index_and_guidelines/atc_ddd_index/. Cited 2 July 2022.
Fusaroli M, Raschi E, Gatti M, De Ponti F, Poluzzi E. Development of a network-based signal detection tool: the COVID-19 adversome in the FDA adverse event reporting system. Front Pharmacol. 2021;12:3542.
Rothman KJ, Lanes S, Sacks ST. The reporting odds ratio and its advantages over the proportional reporting ratio. Pharmacoepidemiol Drug Saf. 2004;13:519–23.
Zhang D. A coefficient of determination for generalized linear models. Am Stat. 2017;71:310–6.
Gavrielatos G, Komitopoulos N, Kanellos P, Varsamis E, Kogeorgos J. Suicidal attempts by prescription drug overdose in the elderly: a study of 44 cases. Neuropsychiatr Dis Treat. 2006;2:359–63.
Su MK, Chan PY, Hoffman RS. The seasonality of suicide attempts: a single poison control center perspective. Clin Toxicol (Phila). 2020;58:1034–41.
Yu J, Yang D, Kim Y, Hashizume M, Gasparrini A, Armstrong B, et al. Seasonality of suicide: a multi-country multi-community observational study. Epidemiology and psychiatric sciences. Cambridge University Press; 2020. https://www.cambridge.org/core/journals/epidemiology-and-psychiatric-sciences/article/seasonality-of-suicide-a-multicountry-multicommunity-observational-study/40EC27B6AC04D152AD6675C8E90F7E09. Cited 15 Apr 2022.
Gunnell D, Appleby L, Arensman E, Hawton K, John A, Kapur N, et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7:468–71.
Hawton K. United Kingdom legislation on pack sizes of analgesics: background, rationale, and effects on suicide and deliberate self-harm. Suicide Life Threat Behav. 2002;32:223–9.
Desai RJ, Good MM, San-Juan-Rodriguez A, Henriksen A, Cunningham F, Hernandez I, et al. Varenicline and nicotine replacement use associated with US Food and Drug Administration drug safety communications. JAMA Netw Open. 2019;2: e1910626.
Spyres MB, Aldy K, Farrugia LA, Kang AM, Love JS, Campleman SL, et al. The toxicology investigators consortium 2020 annual report. J Med Toxicol. 2021;17:333–62.
Gummin DD, Mowry JB, Spyker DA, Brooks DE, Beuhler MC, Rivers LJ, et al. 2018 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 36th annual report. Clin Toxicol (Phila). 2019;57:1220–413.
Jones AW, Holmgren A, Ahlner J. Toxicology findings in suicides: concentrations of ethanol and other drugs in femoral blood in victims of hanging and poisoning in relation to age and gender of the deceased. J Forensic Leg Med. 2013;20:842–7.
Jiang T, Nagy D, Rosellini AJ, Horváth-Puhó E, Keyes KM, Lash TL, et al. Suicide prediction among men and women with depression: a population-based study. J Psychiatr Res. 2021;142:275–82.
Kanchan T, Menon A, Menezes RG. Methods of choice in completed suicides: gender differences and review of literature. J Forensic Sci. 2009;54:938–42.
Gravensteen IK, Ekeberg Ø, Thiblin I, Helweg-Larsen K, Hem E, Rogde S, et al. Psychoactive substances in natural and unnatural deaths in Norway and Sweden—a study on victims of suicide and accidents compared with natural deaths in psychiatric patients. BMC Psychiatry. 2019;19:33.
Borges G, Bagge CL, Cherpitel CJ, Conner KR, Orozco R, Rossow I. A meta-analysis of acute use of alcohol and the risk of suicide attempt. Psychol Med. 2017;47:949–57.
Park CHK, Yoo SH, Lee J, Cho SJ, Shin M-S, Kim EY, et al. Impact of acute alcohol consumption on lethality of suicide methods. Compr Psychiatry. 2017;75:27–34.
Choi IY, Kim S-Y, Chang JG, Song HR, Kim WJ, Lee SY, et al. Lethality-associated factors in deliberate self-poisoning. Soa Chongsonyon Chongsin Uihak. 2021;32:17–27.
Larson AM, Polson J, Fontana RJ, Davern TJ, Lalani E, Hynan LS, et al. Acetaminophen-induced acute liver failure: results of a United States multicenter, prospective study. Hepatology. 2005;42:1364–72.
Duffull SB, Isbister GK. Predicting the requirement for N-acetylcysteine in paracetamol poisoning from reported dose. Clin Toxicol (Phila). 2013;51:772–6.
Zimmerman HJ, Maddrey WC. Acetaminophen (paracetamol) hepatotoxicity with regular intake of alcohol: analysis of instances of therapeutic misadventure. Hepatology. 1995;22:767–73.
Dargan PI, Jones AL. Should a lower treatment line be used when treating paracetamol poisoning in patients with chronic alcoholism? A case against. Drug Saf. 2002;25:625–32.
Chiew AL, Gluud C, Brok J, Buckley NA. Interventions for paracetamol (acetaminophen) overdose. Cochrane Database Syst Rev. 2018;2:CD003328.
Höjer J, Tellerup M. Promethazine—an old pharmaceutical that has got a renaissance. An avalanche-like increase in the number of overdose cases in Sweden [in Swedish]. Lakartidningen. 2018;115:E9EZ.
Miuli A, Stigliano G, Lalli A, Coladonato M, D’Angelo L, Esposito F, et al. “Purple Drank” (Codeine and Promethazine Cough Syrup): a systematic review of a social phenomenon with medical implications. J Psychoactive Drugs. 2020;52:453–62.
Chiappini S, Schifano F, Corkery JM, Guirguis A. Beyond the ‘purple drank’: Study of promethazine abuse according to the European Medicines Agency adverse drug reaction reports. J Psychopharmacol. 2021;35:681–92.
Salpeter S, Greyber E, Pasternak G, Salpeter E. Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus. Cochrane Database Syst Rev. 2006;1:CD002967.
Kuan IHS, Savage RL, Duffull SB, Walker RJ, Wright DFB. The association between metformin therapy and lactic acidosis. Drug Saf. 2019;42:1449–69.
Stanek EJ, Nelson CE, DeNofrio D. Amlodipine overdose. Ann Pharmacother. 1997;31:853–6.
Østergaard MLD, Nordentoft M, Hjorthøj C. Associations between substance use disorders and suicide or suicide attempts in people with mental illness: a Danish nation-wide, prospective, register-based study of patients diagnosed with schizophrenia, bipolar disorder, unipolar depression or personality disorder. Addiction. 2017;112:1250–9.
Suttajit S, Srisurapanont M, Maneeton N, Maneeton B. Quetiapine for acute bipolar depression: a systematic review and meta-analysis. Drug Des Dev Ther. 2014;8:827–38.
Hodgman MJ, Garrard AR. A review of acetaminophen poisoning. Crit Care Clin. 2012;28:499–516.
Jones CM, Mack KA, Paulozzi LJ. Pharmaceutical overdose deaths, United States, 2010. JAMA. 2013;309:657–9.
Cicero TJ, Ellis MS. Abuse-deterrent formulations and the prescription opioid abuse epidemic in the United States: lessons learned from OxyContin. JAMA Psychiat. 2015;72:424–30.
Pergolizzi JV, Webster LR, Vortsman E, Ann LeQuang J, Raffa RB. Wooden chest syndrome: the atypical pharmacology of fentanyl overdose. J Clin Pharm Ther. 2021;46:1505–8.
Torralva R, Janowsky A. Noradrenergic mechanisms in fentanyl-mediated rapid death explain failure of naloxone in the opioid crisis. J Pharmacol Exp Ther. 2019;371:453–75.
Schwartz RH. Adolescent abuse of dextromethorphan. Clin Pediatr (Phila). 2005;44:565–8.
Acknowledgements
Part of the results of this study have been presented at the International Conference on Pharmacoepidemiology & Therapeutic Risk Management (ICPE) 2022, held in Copenhagen on 24–28 August 2022. ER, FD, EP were supported by institutional research funds (Ricerca Fondamentale Orientata).
Funding
Open access funding provided by Alma Mater Studiorum - Università di Bologna within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No specific funding supported this research.
Conflict of interest
Michele Fusaroli, Guido Pelletti, Valentina Giunchi, Chiara Pugliese, Mattia Bartolucci, Elena Narmine Necibi, Emanuel Raschi, Fabrizio De Ponti, Susi Pelotti, and Elisabetta Poluzzi declare no conflicts of interest in relation to this research.
Ethics approval
Not applicable because spontaneous reports of the FAERS are anonymous and publicly available.
Consent to participate
Not applicable because spontaneous reports of the FAERS are anonymous and publicly available.
Consent for publication
Not applicable because spontaneous reports of the FAERS are anonymous and publicly available.
Availability of data and material
The data we used come from the US FAERS and is made publicly available by the FDA as quarterly data downloadable at https://fis.fda.gov/extensions/FPD-QDE-FAERS/FPD-QDE-FAERS.html. The interactive network is available at: https://osf.io/n5q8x/.
Code availability
The custom code will be made available to applicants upon reasonable request.
Author contributions
MF, GP, EN, ER, EP and SP conceptualized and designed the study. MF, VG, ER and EP developed the methodology. The formal analysis was performed by MF, VG, CP and MB. MF, VG and MB performed the visualization. MF wrote the original draft, and EP and SP supervised the work. All authors strongly contributed to the interpretation of the results, and to the review and editing of the draft. All authors read and approved the final version.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Fusaroli, M., Pelletti, G., Giunchi, V. et al. Deliberate Self-Poisoning: Real-Time Characterization of Suicidal Habits and Toxidromes in the Food and Drug Administration Adverse Event Reporting System. Drug Saf 46, 283–295 (2023). https://doi.org/10.1007/s40264-022-01269-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-022-01269-x