Abstract
Introduction
Patient registries, ‘organised systems that use observational methods to collect uniform data on a population defined by a particular disease, condition, or exposure, and that is followed over time’, are potentially valuable sources of data for supporting regulatory decision-making, especially for products to treat rare diseases. Nevertheless, patient registries are greatly underused in regulatory assessments. Reasons include heterogeneity in registry design and in the data collected, even across registries for the same disease, as well as unreliable data quality and data sharing impediments. The Patient Registries Initiative was established by the European Medicines Agency in 2015 to support registries in collecting data suitable to contribute to regulatory assessments, especially post-authorisation safety and effectiveness studies.
Methods
We conducted a qualitative synthesis of the published observations and recommendations from an initiative-led multi-stakeholder consultation and four disease-specific patient registry workshops. We identified the primary factors facilitating the use of registry data in regulatory assessments. We generated proposals on operational measures needed from stakeholders including registry holders, patients, healthcare professionals, regulators, marketing authorisation applicants and holders, and health technology assessment bodies for implementing these.
Results
Ten factors were identified as facilitating registry use for supporting regulatory assessments of medicinal products. Proposals on operational measures needed for implementation were categorised according to three themes: (1) nature of the data collected and registry quality assurance processes; (2) registry governance, informed consent, data protection and sharing; and (3) stakeholder communication and planning of benefit-risk assessments.
Conclusions
These are the first explicit proposals, from a regulatory perspective, on operational methods for increasing the use of patient registries in medicines regulation. They apply to registry holders, patients, regulators, marketing authorisation holders/applicants and healthcare stakeholders broadly, and their implementation would greatly facilitate the use of these valuable data sources in regulatory decision-making.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Patient registries are potentially valuable sources of data for supporting regulatory decision-making on medicines, but they are greatly underused owing to heterogeneity in registry design, the data collected and its quality, as well as to data sharing impediments. |
The European Medicines Agency’s Patient Registries Initiative aims to support registries in collecting data suitable to contribute to regulatory assessments, especially post-authorisation safety and effectiveness studies. |
We have generated operational proposals on patient registry data, quality assurance processes, governance and stakeholder communication that will help to increase the use of these valuable resources in regulatory benefit-risk assessments of medicines. |
1 Introduction
Health-related real world data provide crucial support for regulatory decision-making, especially in post-authorisation assessments of medicinal products [1]. There are multiple sources including patient (disease) registries, electronic health records, insurance claims databases, health surveys, and prescription dispensing databases [2]. Patient registries, ‘organised systems that use observational methods to collect uniform data on a population defined by a particular disease, condition, or exposure, and that is followed over time’, are a potentially rich source of data, especially for evaluating the course of rare diseases and effects of new treatments [3,4,5]. Despite this, they are greatly underused in regulatory assessments of medicines. There are many reasons, including heterogeneity in registry design within individual disease areas, unreliable data quality and data sharing barriers, all amplified by limited national and international collaboration [5, 6].
1.1 Use of Patient Registries for Supporting Regulatory Assessments
In pivotal studies supporting marketing authorisation of medicinal products, randomised controlled trial (RCT) data are preferred by regulators. However, in situations where RCT data are limited or where RCTs are not ethical or are not feasible, as with many rare diseases, patient registry data may provide crucial support for regulatory decision-making. For example, in the case of haemophilia, the updated guideline on Factor VIII products removes the obligation to perform clinical trials in previously untreated patients but requires post-authorisation studies based on a set of core data elements to be collected in patient registries [7]. For products granted conditional marketing approval, registry studies may provide post-authorisation data to fulfil regulator-imposed specific obligations to confirm safety and/or effectiveness, as is the case with the recently authorised chimeric antigen receptor (CAR) T-cell products, tiagenlecleucel and axicabtagene ciloleucel [8, 9]. Some registries may be of particular value in terms of the patient population size and representativeness, the duration of follow-up data for treatment-exposed patients and availability of information not collected in other real world repositories.
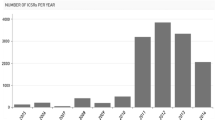
Notwithstanding such potential, the under-use of patient registries in the regulatory context is striking [10, 11]. Of 335 products recommended for approval between 2005 and 2013 by the main scientific committee of the European Medicines Agency (EMA), the Committee for Medicinal Products for Human Use (CHMP), 31 registries were requested to fulfil a condition of the marketing authorisation, but by December 2017, just ten had been completed [11]. Potentially, registries could provide data permitting comparisons of outcomes from different treatments across different countries and healthcare settings over time as well as assessment of the impact of measures taken to minimise risks of medicinal products [12, 13]. Their limitations for such assessments are well-described, but a description of the features needed to encourage increased use is lacking [4, 12,13,14]. Our aim with this work was to provide proposals, from a regulatory perspective, on how registry stakeholders could fill this gap.
2 Methods
We conducted a qualitative synthesis of the observations and recommendations published in five reports arising from a multi-stakeholder consultation and four disease-specific workshops conducted as part of EMA’s Patient Registries Initiative.
From the consultation report, we identified the primary factors considered by stakeholders as facilitating the use of registry data for supporting medicines regulation.
From each of the four disease-specific workshop reports, we abstracted the participant observations and recommendations on utilising patient registry data in regulatory assessments along with the measures needed from stakeholders in order to implement them. We then generated operational proposals, applicable to patient registries and stakeholder groups broadly, for implementing these measures.
3 Patient Registries Initiative
In 2015, EMA established a Patient Registries Initiative to support a systematic and standardised approach for registry contribution to medicines assessment, especially for post-authorisation safety studies (PASS) and post-authorisation effectiveness studies (PAES) [6]. The initiative aims to create a registry framework with collaboration between registry coordinators, including healthcare professionals’ and patients’ associations, academic institutions and national agencies responsible for overseeing healthcare services, and potential users of registry data, such as medicines regulators, reimbursement bodies, and pharmaceutical companies. Key elements of its strategy include facilitating the use of existing patient registries within the current legal and regulatory framework for medicinal products and providing methodological support for the establishment of new registries [15].
4 Multi-Stakeholder Consultation and Disease-Specific Registry Workshops
At a consultation in October 2016, 122 expert stakeholders, including registry holders, patients, healthcare professionals, regulators, marketing authorisation holders and applicants (MAHs/MAAs), and health technology assessment (HTA) and reimbursement bodies, and European Commission representatives shared their views on barriers to and facilitators of registry use and on optimising the use of registries for regulatory assessments [16]. The discussions provided the groundwork for four disease-specific registry workshops held during 2017 and 2018 that explored the use of registry data for supporting regulatory assessments in four areas of active product development where new products had recently been approved or were undergoing assessment (Appendix Table 1, see the electronic supplementary material): cystic fibrosis [17], multiple sclerosis [18], CAR T-cell therapies [19], and haemophilia therapies [20].
The four workshops together included 266 participants representing all of the stakeholder groups in each case. The individual workshop reports providing participants’ observations and recommendations, along with the report of the multi-stakeholder consultation, are published on the EMA patient registries webpage [6]. The objectives and methods of the individual patient registry workshops are described in Appendix Table 2 (see the electronic supplementary material). This work did not require ethics approval.
5 Results
5.1 Factors Supporting the Use of Registries
Synthesis of the participant observations from the multi-stakeholder consultation report generated a list of factors that facilitated the use of patient registries for regulatory assessments. They included the use of common core data sets, common coding terminologies, complete data collection, especially on medications, facility for data access and sharing, data linkage capacity, quality assurance processes and governance, early consideration of registries in the regulatory process, stakeholder communication, registry sustainability and the availability of a registry framework. Their value in facilitating registry use is described in Table 1. In each case, absence or incompleteness greatly impeded registry use.
5.2 Proposals on Operational Measures to Increase Registry Use in Regulatory Assessments
Three themes, generalisable to patient registries broadly, emerged from the published observations and recommendations made by the participants in each of the four disease-specific patient registry workshops:
-
1.
Nature of the data collected and registry quality assurance processes
-
2.
Registry governance, informed consent, data protection and sharing
-
3.
Stakeholder communication and planning of benefit-risk assessments.
5.2.1 Nature of the Data and Registry Quality Assurance Processes
The need for registries in a given disease area to collect core common data elements, commonly defined, was acknowledged by all stakeholders as essential for ensuring that data from multiple registries in a given disease area could be combined to enhance both the generalisability and the power of studies that could be conducted using the data (Table 2, Box 1). EMA scientific advice may assist in clarifying the suitability of individual registries for defined purposes [23]. Knowledge of data quality is fundamental for regulatory assessments. Quality may be judged according to three components: consistency, accuracy, and completeness. Table 2 defines each quality component, summarises potential indicators of quality that could be applied in registries, and describes the systems or solutions needed to facilitate these in operational terms.
5.2.2 Registry Governance, Informed Consent, Data Protection and Sharing
Proposals are summarised in Table 3 for measures needed on registry governance, informed consents, and data sharing and protection in order to ensure that data are accessible for regulatory assessments and may be shared in the context of the applicable legal and governance frameworks.
Examples of recommendations from the individual workshop reports are quoted in Box 2. Registry sustainability measures were not a focus of the disease-specific workshop discussions given the regulatory context, but were acknowledged by all stakeholders as crucial for registry stability and development.
5.2.3 Communication with Stakeholders
Acknowledged areas of improvements needed to support the use of registry data in regulatory assessments include communication between stakeholders early in the marketing authorisation process in order to plan for post-authorisation studies (Fig. 1, Box 3). The studies are needed so that marketing authorisation, if granted, may be followed-up with timely evidence on the benefit-risk balance of new products for patient and public health, most especially for products with specific obligations where delays in study completion are common [25,26,27]. Opportunities arise early in the marketing authorisation process to pro-actively identify likely data needs, especially for post-authorisation studies. These opportunities are illustrated in Fig. 1. Where registry data could potentially contribute, there should be three-way contact involving regulators, MAAs/MAHs and registry holders to explore data availability.

Source: Clin Pharmacol Ther 2019 https://doi.org/10.1002/cpt.1414
Opportunities during the regulatory cycle to identify where registry data may be needed for post-authorisation follow-up.
6 Discussion
6.1 Priorities for Implementation of Proposals
Our proposals have been synthesised from the published reports of a consultative discussion and four disease-specific workshops that together included almost 400 specialist stakeholders with patient registry expertise. In doing so, we have leveraged the deep knowledge of participants in each disease area to generate proposals that apply to registries broadly. Implementation of the proposals by registry stakeholders collectively would help to establish a harmonised patient registry environment within many other individual disease areas, thereby increasing the suitability of registry data for regulatory assessments of related medicinal products.
From a regulatory perspective, the priorities for the development of a European Union-wide framework on patient registries are:
-
Availability of core common data sets, specific for individual disease areas, with commonly defined data elements across registry networks
-
Registry operational procedures for MAAs/MAHs and regulators to access data in accordance with national regulation and European General Data Protection Regulation [20]
-
Transparent quality assurance processes in registries.
Therefore, in addressing the factors described in Table 1, the proposals on data elements, quality assurance, governance, patient consents, and data protection summarised in Tables 2 and 3, together with communication and planning early in the authorisation process, are critical if the potential of patient registry data for regulatory assessments of medicinal products is to be realised.
6.2 EMA Actions to Increase Registry Use
EMA has provided scientific advice to support CHMP qualification opinions on two patient registries regarding their suitability for supporting regulatory assessments of medicines, the European Cystic Fibrosis Society Patient Registry and the cellular therapy module of the European Blood and Marrow Transplant registry [19]. In both cases, the opinions describe contexts of use for which the registry data are considered suitable by CHMP for undertaking pharmacoepidemiology studies. The possibility for registries to obtain scientific advice to support a qualification opinion may go some considerable way in assuring stakeholders that registries so qualified are satisfactory for regulatory studies.
Internally, EMA has instituted measures to identify products during pre-submission stages of authorisation processes (pre-submission meetings, scientific advice and priority medicines [PRIME] discussions [28]) (Figure 1) where registry or other real world data may be needed for post-authorisation follow-up if marketing authorisation is granted. This action anticipates and permits pro-active planning for post-authorisation assessments and reflects the regulatory policy of benefit-risk assessment throughout the product lifecycle. To assist stakeholders in identifying potentially relevant registries, a publicly available inventory of patient registries is hosted on the European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCePP) resources database [29].
EMA should not duplicate other initiatives aiming to enhance registry use in healthcare. Therefore, its patient registries strategy aligns with the European Commission policy framework on rare diseases as well as with priorities of the European Research Networks for rare diseases, the Horizon 2020 programme and Joint Action initiatives such as the European Network for Health Technology Assessment (EUnetHTA), and takes into account national endeavours such as those underway in the Netherlands and Sweden [30,31,32,33,34,35]. The European Platform on Rare Diseases Registration (EU RD Platform) has developed a ‘Set of common data elements for RD Registration’ [36]. It is aimed at the European Reference Network’s existing registries and registries under development; other rare disease registries at national, regional, and local levels in EU Member States; researchers and patient organisations.
From a regulatory perspective, the ultimate requirement of patient registries is that they permit the conduct of high-quality studies that evaluate the safety and effectiveness of medicines. Recognising the benefits and challenges inherent in using observational data for medicines assessments, in 2019, EMA will publish methodological and operational advice on handling registry data in post-authorisation studies, taking into account responses to its open consultation on a preliminary discussion paper [6]. Application of the advice will be underpinned by clear understanding of the differences between a registry and a registry study (Table 4).
7 Conclusions
This is the first time that the factors necessary for patient registry data to adequately support regulatory assessments, together with operational proposals required for their implementation, have been set out explicitly from a regulatory perspective. In explaining what is needed, taking account of the current legal and regulatory framework for medicinal products, the proposals empower stakeholders seeking to capitalise on the potential of patient registries broadly to support and contribute to regulatory decision-making on medicines.
Actions by all stakeholders, registry owners as well as MAAs/MAHs, regulators, patients/their representatives, healthcare professionals, and HTA and medicines reimbursement bodies, are required to implement the proposals and thereby consolidate registry value in patient and public health.
Change history
05 September 2019
The fourth sentence under the heading “1.1 Use of Patient Registries for Supporting Regulatory Assessments” in “1 Introduction” section should read as below.
References
Sherman RE, Anderson SA, Dal Pan GJ, Gray GW, Gross T, Hunter NL, et al. Real-world evidence—what is it and what can it tell us? N Engl J Med. 2016;375(23):2293–7.
Makady A, de Boer A, Hillege H, Klungel O, Goettsch W, on behalf of GetReal Work Package 1. What is real-world data? a review of definitions based on literature and stakeholder interviews. Value Health J Int Soc Pharmacoecon Outcomes Res. 2017;20(7):858–65.
Gliklich RE, Dreyer NA, eds. Registries for Evaluating Patient Outcomes: A User’s Guide. Agency for Healthcare Research and Quality. 2007. https://effectivehealthcare.ahrq.gov/sites/default/files/pdf/registries-guide_research.pdf. Accessed 30 June 2019.
Zaletel, M, Kralj, M, Magajne, M, Doupi, P. Methodological Guidelines and Recommendations for Efficient and Rational Governance of Patient Registries. PARENT. Vol. 25. 2015. https://ec.europa.eu/health/sites/health/files/ehealth/docs/patient_registries_guidelines_en.pdf. Accessed 30 June 2019.
European Medicines Agency. Patient Registries. http://www.ema.europa.eu/ema/index.jsp?curl=pages/regulation/general/general_content_000658.jsp&mid=WC0b01ac0580961211. Accessed 30 June 2019.
Forrest CB, Bartek RJ, Rubinstein Y, Groft SC. The case for a global rare diseases registry. Lancet. 2011;377:1057–9.
European Medicines Agency. Guideline on the clinical investigation of recombinant and human plasma-derived factor VIII products [Draft]. https://www.ema.europa.eu/documents/scientific-guideline/draft-guideline-clinical-investigation-recombinant-4-human-plasma-derived-factor-viii-products_en.pdf. Accessed 30 June 2019.
European Medicines Agency. Kymriah. Summary of Product Characteristics. https://www.ema.europa.eu/documents/product-information/kymriah-epar-product-information_en.pdf Accessed 25 Mar 2019.
European Medicines Agency. Yescarta. Summary of Product Characteristics. https://www.ema.europa.eu/documents/product-information/yescarta-epar-product-information_en.pdf.
Jonker CJ, van den Berg HM, Kwa MSG, Hoes AW, Mol PGM. Registries supporting new drug applications. Pharmacoepidemiol Drug Saf. 2017;26(12):1451–7.
Pacurariu A, Plueschke K, Olmo CA, Kurz X. Imposed registries within the European post-marketing surveillance system: extended analysis and lessons learned for regulators. Pharmacoepidemiol Drug Saf. 2018;27(7):823–6. https://doi.org/10.1002/pds.4449.
Bessonova L, Volkova N, Higgins M, Bengtsson L, Tian S, Simard C, et al. Data from the US and UK cystic fibrosis registries support disease modification by CFTR modulation with ivacaftor. Thorax. 2018. https://doi.org/10.1136/thoraxjnl-2017-210394.
Ferreira-Gonza´lez I, Marsal JR, Mitjavila F, Parada A, Ribera A, Cascant P, et al. Patient Registries of Acute Coronary Syndrome: Assessing or Biasing the Clinical Real World Data? Circ Cardiovasc Qual Outcomes. 2009;2:540–7.
European Network of Centres for Pharmacoepidemiology and Pharmacovigilance [ENCePP]. Guide on methodological standards in pharmacoepidemiology: Patient Registries http://www.encepp.eu/standards_and_guidances/methodologicalGuide4_3.shtml. Accessed 30 June 2019.
European Medicines Agency. Initiative for patient registries - strategy and pilot phase. EMA/176050/2014 [Internet]. 2015. http://www.ema.europa.eu/docs/en_GB/document_library/Other/2015/10/WC500195576.pdf. Accessed 30 June 2019.
European Medicines Agency. Patient Registries Workshop, 28 October 2016—Observations and recommendations arising from the workshop. EMA/69716/2017 [Internet]. 2017. http://www.ema.europa.eu/docs/en_GB/document_library/Report/2017/02/WC500221618.pdf. Accessed 30 June 2019.
European Medicines Agency. Report on Cystic Fibrosis registries: Workshop 14 June 2017, Patient Registries Initiative. https://www.ema.europa.eu/en/documents/report/report-cystic-fibrosis-registries_en.pdf. Accessed 30 June 2019.
European Medicines Agency. Report on Multiple Sclerosis registries: Workshop 7 July 2017, Patient Registries Initiative. https://www.ema.europa.eu/en/documents/report/report-multiple-sclerosis-registries_en.pdf. Accessed 30 June 2019.
European Medicines Agency. Report on CAR T-cell therapy registries: Workshop 9 February 2018, Patient Registries Initiative. https://www.ema.europa.eu/en/documents/report/report-car-t-cell-therapy-registries-workshop_en.pdf. Accessed 30 June 2019.
European Medicines Agency. Report on Haemophilia registries: Workshop 8 June 2018, Patient Registries Initiative. https://www.ema.europa.eu/en/documents/report/report-haemophilia-registries-workshop_en.pdf. Accessed 30 June 2019.
Medical Dictionary for Regulatory Activities [MedDRA®]; https://www.meddra.org/. Accessed 30 June 2019.
European Medicines Agency. Guideline on good pharmacovigilance practices; Module Vlll—Post- authorisation safety studies http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2012/06/WC500129137.pdf. Accessed 30 June 2019.
European Medicines Agency. Qualification of novel methodologies for medicine development. http://www.ema.europa.eu/ema/index.jsp?curl=pages/regulation/document_listing/document_listing_000319.jsp&mid=WC0b01ac0580022bb0. Accessed 30 June 2019.
EU General Data Protection Regulation [GDPR]. https://eugdprportal.godaddysites.com/. Accessed 30 June 2019.
Banzi R, Gerardi C, Bertele’ V, Garattini S. Approvals of drugs with uncertain benefit-risk profiles in Europe. Eur J Intern Med. 2015;26(8):572–84.
Pease AM, Krumholz HM, Downing NS, Aminawung JA, Shah ND, Ross JS. Post-approval studies of drugs initially approved by the FDA on the basis of limited evidence: systematic review. BMJ. 2017;3(357):j1680.
Moore TJ, Furberg CD. Development times, clinical testing, post-market follow-up, and safety risks for the new drugs approved by the US food and drug administration: the class of 2008. JAMA Intern Med. 2014;174(1):90–5.
European Medicines Agency. PRIME: PRIority MEdicines http://www.ema.europa.eu/ema/index.jsp?curl=pages/regulation/general/general_content_000660.jsp&mid=WC0b01ac05809f8439. Accessed 30 June 2019.
European Network of Centres for Pharmacoepidemiology and Pharmacovigilance [ENCePP]. ENCePP Resourced Database; http://www.encepp.eu/encepp/resourcesDatabase.jsp. Accessed 30 June 2019.
European Commission. European Reference Networks https://ec.europa.eu/health/ern_en. Accessed 30 June 2019.
European Network for Health Technology Assessment [EUnetHTA] https://www.eunethta.eu/. Accessed 30 June 2019.
European Commission. Implementation report on the Commission Communication on rare diseases; 2014; https://ec.europa.eu/health/sites/health/files/rare_diseases/docs/2014_rarediseases_implementationreport_en.pdf. Accessed 30 June 2019.
European Commission. Horizon 2020 Work programme 2018-2020. http://ec.europa.eu/research/participants/data/ref/h2020/wp/2018-2020/main/h2020-wp1820-health_en.pdf. Accessed 30 June 2019.
Healthcare Institute Netherlands. Register of registries https://www.zorginstituutnederland.nl/actueel/nieuws/2019/04/02/zorginstituut-start-project-regie-op-registers-voor-dure-geneesmiddelen. Accessed 30 June 2019.
Swedish National Data Service. Register based research. https://snd.gu.se/en/data-management/register-based-research. Accessed 30 June 2019.
European Commission. European Platform on Rare Diseases registration; Set of Common Data Elements. https://eu-rd-platform.jrc.ec.europa.eu/set-of-common-data-elements. Accessed 30 June 2019.
Acknowledgements
We acknowledge the support of EMA’s Cross Committee Task Force on Patient Registries. We thank Filipa Da Mota for commencing the Inventory of Registries and for her support, along with Valerie Muldoon, of the stakeholder consultation and patient registry workshops. We acknowledge the generous input of expertise and time by the multiple stakeholders who contributed to the consultation, the disease-specific workshops, and the creation of the five published reports arising from these endeavours.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this study.
Conflict of interest
The authors, Patricia McGettigan, Carla Alonso Olmo, Kelly Plueschke, Mireia Castillon, Daniel Nogueras Zondag, Priya Bahri, Xavier Kurz and Peter Mol, have no conflicts of interest that are directly relevant to the content of this study.
Patient consent
Patient consent was not required for this work.
Disclaimer
The views expressed in this article are those of the authors and may not be understood or quoted as reflecting the views of their respective institutions or of the European Medicines Agency or one of its committees or working parties.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
McGettigan, P., Alonso Olmo, C., Plueschke, K. et al. Patient Registries: An Underused Resource for Medicines Evaluation. Drug Saf 42, 1343–1351 (2019). https://doi.org/10.1007/s40264-019-00848-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-019-00848-9