Abstract
Introduction
Pharmacovigilance includes analysis of large databases of information on drugs and events using algorithms that detect disproportional frequencies of associations. In order to test such algorithms, attempts have been made to provide canonical reference lists of so-called ‘positive controls’ and ‘negative controls’. Reference sets with even modest levels of misclassification may result in under- or overstatement of the performance of algorithms.
Aim
We sought to determine the extent to which ‘negative control’ drug–event pairs in the Observational Medical Outcomes Partnership (OMOP) database are misclassified
Methods
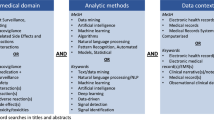
We searched the medical literature for evidence of associations between drugs and events listed by OMOP as negative controls.
Results
The criteria used in OMOP to classify positive and negative controls are asymmetric; drug–event associations published only as case series or case reports are classified as positive controls if they are cited in Drug-Induced Diseases by Tisdale and Miller, but as negative controls if case series or case reports exist but are not cited in Tisdale and Miller. Of 233 drug–event pairs classified in the 2013 version of OMOP as negative controls, 21 failed to meet pre-specified OMOP adjudication criteria; in another 19 cases we found case reports, case series, or observational evidence that the drug and event are associated. Overall, OMOP misclassified, or may have misclassified, 40 (17 %) of all ‘negative controls.’
Conclusions
Results from studies of the performance of signal-detection algorithms based on the OMOP gold standard should be viewed with circumspection, because imperfect gold standards may lead to under/overstatement of absolute and relative signal detection algorithm performance. Improvements to OMOP would include omitting misclassified drug–event pairs, assigning more specific event labels, and using more extensive sources of information.
Similar content being viewed by others
References
Hauben M, Norén GN. A decade of data mining and still counting. Drug Saf. 2010;33(7):527–34.
Observational Medical Outcomes Partnership (OMOP). http://fnih.org/what-we-do/major-completed-programs/omop. Accessed 21 Jan 2016.
Observational Medical Outcomes Partnership. http://omop.org. Accessed 21 Jan 2016.
Cardoso JR, Pereira LM, Iversen MD, Ramos AL. What is gold standard and what is ground truth? Dental Press J Orthod. 2014;19(5):27–30.
Ryan PB, Madigan D, Stang PE, Overhage JM, Racoosin JA, Hartzema AG. Empirical assessment of methods for risk identification in healthcare data: results from experiments of the Observational Medical Outcomes Partnership. Stat Med. 2012;31(30):4401–15.
Ryan PB, Schuemie MJ, Welebob E, Duke J, Valentine S, Hartzema AG. Defining a reference set to support methodological research in drug safety. Drug Saf. 2013;36(Suppl 1):S33–47.
Harpaz R, DuMouchel W, LePendu P, Shah NH. Empirical Bayes model to combine signals of adverse drug reactions. Proceedings of the 2013 ACM SIGKDD International Conference on Knowledge Discovery and Data Mining (KDD’13); 2013. p. 1339–47.
Harpaz R, DuMouchel W, LePendu P, Bauer-Mehren A, Ryan P, Shah NH. Performance of pharmacovigilance signal-detection algorithms for the FDA adverse event reporting system. Clin Pharmacol Ther. 2013;93(6):539–46.
White RW, Harpaz R, Shah NH, DuMouchel W, Horvitz E. Toward enhanced pharmacovigilance using patient-generated data on the internet. Clin Pharmacol Ther. 2014;96(2):239–46.
Harpaz R, DuMouchel W, Shah NH. Comment on: “Zoo or Savannah? Choice of training ground for evidence-based pharmacovigilance”. Drug Saf. 2015;38(1):113–4.
Norén GN, Castor O, Juhlin K, Lindquist M. Authors’ reply to Harpaz et al. comment on: “Zoo or Savannah? Choice of training ground for evidence-based pharmacovigilance”. Drug Saf. 2005;38(1):115–6.
Li Y, Ryan PB, Wei Y, Friedman C. A method to combine signals from spontaneous reporting systems and observational healthcare data to detect adverse drug reactions. Drug Saf. 2015;38(10):895–908.
Hauben M, Reich L, et al. Response to letter by Levine. Br J Clin Pharmacol. 2006;61(1):115–7.
Phelps CE, Hutson A. Estimating diagnostic accuracy using a “fuzzy gold standard”. Med Decis Making. 1995;15:44–57.
Tisdale JE, Miller DA. Drug-induced diseases: prevention, detection, and management. 2nd ed. Bethesda: American Society of Health-System Pharmacists; 2010.
European Medicines Agency. Guideline on good pharmacovigilance practices (GVP) Annex I—definitions (Rev 3). http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2013/05/WC500143294.pdf. Accessed 21 Jan 2016.
Girard M. Conclusiveness of rechallenge in the interpretation of adverse drug reactions. Br J Clin Pharmacol. 1987;23(1):73–9.
Aronson JK, Hauben M. Anecdotes that provide definitive evidence. BMJ. 2006;333(7581):1267–9.
Hauben M, Aronson JK. Gold standards in pharmacovigilance: the use of definitive anecdotal reports of adverse drug reactions as pure gold and high-grade ore. Drug Saf. 2007;30(8):645–55.
Valenstein PN. Evaluating diagnostic tests with imperfect standards. Am J Clin Pathol. 1990;93(2):252–8.
Council for International Organizations of Medical Sciences. Practical aspects of signal detection in pharmacovigilance: report of CIOMS Working Group VIII. http://www.cioms.ch/index.php/publications/available-publications?task=view&id=27&catid=54. Accessed 21 Jan 2016.
Saito T, Rehmsmeier M. The precision-recall plot is more informative than the ROC plot when evaluating binary classifiers on imbalanced datasets. PLoS One. 2015;10(3):e0118432.
Hawkins DM, Garrett JA, Stephenson B. Some issues in resolution of diagnostic tests using an imperfect gold standard. Stat Med. 2001;20(13):1987–2001.
EP550. Verification bias and tarnished gold standards. February 2, 2012. http://www.uphs.upenn.edu/dgimhsr/documents/Lecture.verificationbias.handout.pdf. Accessed 21 Jan 2016.
Overhage JM, Ryan PB, Schuemie MJ, Stang PE. Authors’ reply to Hennessy and Leonard’s comment on “Desideratum for evidence-based epidemiology”. Drug Saf. 2015;38(1):105–7.
Hennessy S, Leonard CE. Comment on: “Desideratum for evidence-based epidemiology”. Drug Saf. 2015;38(1):101–3.
Patanè S, Marte F, Di Bella G, Chiofalo S, Currò A, Coglitore S. Acute myocardial infarction and Kounis syndrome. Int J Cardiol. 2009;134(2):e45–6.
Caglar IM, Vural A, Turhan Caglar FN, Ugurlucan M, Karakaya O. Kounis syndrome together with myocardial bridging leading to acute myocardial infarction at young age. Case Rep Med. 2011;2011:490310.
Jackson CW, Sheehan AH, Reddan JG. Evidence-based review of the black-box warning for droperidol. Am J Health Syst Pharm. 2007;64(11):1174–86.
Mittleman MA, Lewis RA, Maclure M, Sherwood JB, Muller JE. Triggering myocardial infarction by marijuana. Circulation. 2001;103(23):2805–9.
Patel A, Jones SA, Ferro A, Patel N. Pharmaceutical salts: a formulation trick or a clinical conundrum? Br J Cardiol. 2009;16(6):281–6.
Ferner RE, Coleman J, Pirmohamed M, Constable SA, Rouse A. The quality of information on monitoring for haematological adverse drug reactions. Br J Clin Pharmacol. 2005;60(4):448–51.
Pfistermeister B, Saß A, Criegee-Rieck M, Bürkle T, Fromm MF, Maas R. Inconsistencies and misleading product information officially approved prescribing information from three major drug markets. Clin Pharmacol Ther. 2014;96(5):616–24.
Harpaz R, Odgers D, Gaskin G, DuMouchel W, Winnenburg R, Bodenreider O, Ripple A, Szarfman A, Sorbello A, Horvitz E, White RW, Shah NH. A time-indexed reference standard of adverse drug reactions. Sci Data. 2014;1:140043.
http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=073201aa-556d-4a70-918e-84e9616fd88d. Accessed 21 Jan 2016.
Cohen A. Gastrointestinal blood loss induced by bromfenac sodium, aspirin, and placebo. Clin Ther. 1995;17(6):1110–7.
Worm SW, Sabin C, Weber R, Reiss P, El-Sadr W, Dabis F, De Wit S, Law M, Monforte AD, Friis-Møller N, Kirk O, Fontas E, Weller I, Phillips A, Lundgren J. Risk of myocardial infarction in patients with HIV infection exposed to specific individual antiretroviral drugs from the 3 major drug classes: the Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D) study. J Infect Dis. 2010;201(3):318–30.
Durand M, Sheehy O, Baril JG, Lelorier J, Tremblay CL. Association between HIV infection, antiretroviral therapy, and risk of acute myocardial infarction: a cohort and nested case–control study using Québec’s public health insurance database. J Acquir Immune Defic Syndr. 2011;57(3):245–53.
http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=92b37df9-4602-442f-b8ef-32744f5f412b. Accessed 21 Jan 2016.
http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=304fdee6-0290-4717-be3d-b367bec7e411. Accessed 21 Jan 2016.
Orman ES, Conjeevaram HS, Vuppalanchi R, Freston JW, Rochon J, Kleiner DE, Hayashi PH; DILIN Research Group. Clinical and histopathologic features of fluoroquinolone-induced liver injury. Clin Gastroenterol Hepatol. 2011;9(6):517–523.e3.
Coleman CI, Spencer JV, Chung JO, Reddy P. Possible gatifloxacin-induced fulminant hepatic failure. Ann Pharmacother. 2002;36(7–8):1162–7.
http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=af318d5d-cc39-4a63-a590-b87c50f2694f. Accessed 21 Jan 2016.
http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=d18108f5-98ca-1220-d145-bcf4e71ceaee. Accessed 21 Jan 2016.
Giallauria F, Paragliola T, Del Forno D, Baiano A, de Cristofaro A, Rossi M, Vigorito C. Riabilitazione Cardiologica in paziente HIV-positivo trattato con inibitori di proteasi. [Cardiac rehabilitation in a HIV-patient treated with protease inhibitors.]. Monaldi Arch Chest Dis. 2003;60(1):92–6.
Flynn TE, Bricker LA. Myocardial infarction in HIV-infected men receiving protease inhibitors. Ann Intern Med. 1999;131(7):548.
http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=5bbdc95b-82a1-4ba5-8185-6504ff68cc06. Accessed 21 Jan 2016.
Roche Products Limited. Xenical 120 mg hard capsules. http://www.medicines.org.uk/emc/medicine/1746. Accessed 21 Jan 2016.
Courtney AE, O’Rourke DM, Maxwell AP. Rapidly progressive renal failure associated with successful pharmacotherapy for obesity. Nephrol Dial Transplant. 2007;22(2):621–3.
Singh A, Sarkar SR, Gaber LW, Perazella MA. Acute oxalate nephropathy associated with orlistat, a gastrointestinal lipase inhibitor. Am J Kidney Dis. 2007;49(1):153–7.
Weir MA, Beyea MM, Gomes T, Juurlink DN, Mamdani M, Blake PG, Wald R, Garg AX. Orlistat and acute kidney injury: an analysis of 953 patients. Arch Intern Med. 2011;171(7):703–4.
Kunin CM. Nephrotoxicity of antibiotics. JAMA. 1967;202(3):204–8.
Ottervanger JP, Wilson JH, Stricker BH. Drug-induced chest pain and myocardial infarction. Reports to a national centre and review of the literature. Eur J Clin Pharmacol. 1997;53(2):105–10.
Kent Pharmaceuticals Ltd. Phenoxymethyl Penicillin 125 mg/5 ml Oral Solution Sugar Free BP. http://www.medicines.org.uk/emc/medicine/27479. Accessed 21 Jan 2016.
http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=12d9728e-6b5c-4aee-bfb0-745e542ed2e4. Accessed 21 Jan 2016.
Zhang B, de Vries F, Setakis E, van Staa TP. The pattern of risk of myocardial infarction in patients taking asthma medication: a study with the General Practice Research Database. J Hypertens. 2009;27(7):1485–92.
http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=f85a48d0-0407-4c50-b0fa-7673a160bf01. Accessed 21 Jan 2016.
http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=f55bcc41-2e8d-4ee5-9993-05c7d86f2d2c. Accessed 21 Jan 2016.
Sidney S. Cardiovascular consequences of marijuana use. J Clin Pharmacol. 2002;42(11 Suppl):64S–70S.
Mach F, Montecucco F, Steffens S. Cannabinoid receptors in acute and chronic complications of atherosclerosis. Br J Pharmacol. 2008;153(2):290–8.
Charles R, Holt S, Kirkham N. Myocardial infarction and marijuana. Clin Toxicol. 1979;14(4):433–8.
Macinnes DC, Miller KM. Fatal coronary artery thrombosis associated with cannabis smoking. J R Coll Gen Pract. 1984;34(267):575–6.
Collins JS, Higginson JD, Boyle DM, Webb SW. Myocardial infarction during marijuana smoking in a young female. Eur Heart J. 1985;6(7):637–8.
Choi YS, Pearl WR. Cardiovascular effects of adolescent drug abuse. J Adolesc Health Care. 1989;10(4):332–7.
Papp E, Czopf L, Habon T, Halmosi R, Horvath B, Marton Z, Tahin T, Komocsi A, Horvath I, Melegh B, Toth K. Drug-induced myocardial infarction in young patients: report of two cases. Int J Cardiol. 2005;98(1):169–70.
Leblanc A, Tirel-Badets A, Paleiron N, Castellant P, Cornily JC, Andre M, Grassin F, Feuvrier Y, Blanchard C, Zagnoli F, Quiniou G, Vinsonneau U. Cannabis et infarctus du myocarde du sujet jeune : association fortuite? A propos d’une observation. [Cannabis and myocardial infarction without angiographic stenosis in young patient: guilty or not guilty? A case report]. Ann Cardiol Angeiol (Paris). 2011;60(3):154–8.
Tormey WP. Cannabis, possible cardiac deaths and the coroner in Ireland. Ir J Med Sci. 2012;181(4):479–82.
Tormey WP. Cannabis misinterpretation and misadventure in a coroner’s court. Med Sci Law. 2012;52(4):229–30.
Blank DW, Nanji AA, Schreiber DH, Hudman C, Sanders HD. Acute renal failure and seizures associated with chlorambucil overdose. J Toxicol Clin Toxicol. 1983;20(4):361–5.
Doan RJ, Callaghan WD. Clozapine treatment and neuroleptic malignant syndrome. Can J Psychiatry. 2000;45(4):394–5.
Elias TJ, Bannister KM, Clarkson AR, Faull D, Faull RJ. Clozapine-induced acute interstitial nephritis. Lancet. 1999;354(9185):1180–1.
Fraser D, Jibani M. An unexpected and serious complication of treatment with the atypical antipsychotic drug clozapine. Clin Nephrol. 2000;54(1):78–80.
Janssen-Cilag Ltd. Prezista 100 mg/ml oral suspension. http://www.medicines.org.uk/emc/medicine/28267. Accessed 21 Jan 2016.
Fisher PE, Silk DB, Menzies-Gow N, Dingle M. Ergotamine abuse and extra-hepatic portal hypertension. Postgrad Med J. 1985;61(715):461–3.
Deviere J, Reuse C, Askenasi R. Ischemic pancreatitis and hepatitis secondary to ergotamine poisoning. J Clin Gastroenterol. 1987;9(3):350–2.
Fedotin MS, Hartman C. Ergotamine poisoning producing renal arterial spasm. N Engl J Med. 1970;283(10):518–20.
Pusey CD, Rainford DJ. St Anthony’s fire and pseudochronic renal failure. Br Med J. 1977;2(6092):935.
Hofstädter F. Ergotaminabusus als Ursache einer Retroperitonealfibrose [Ergotamine abuse and retroperitoneal fibrosis.] Zentralbl Allg Pathol. 1976;120(2):83–7.
Lepage-Savary D, Vallières A. Ergotamine as a possible cause of retroperitoneal fibrosis. Clin Pharm. 1982;1(2):179–80.
Janssen van Doorn K, Van der Niepen P, van Tussenbroeck F, Verbeelen D. Acute tubulo-interstitial nephritis and renal infarction secondary to ergotamine therapy. Nephrol Dial Transplant. 2000;15(11):1877–9.
Pujadas R, Argimón J, Pelegrí A, Jané J. Insuficiencia renal y ergotismo. [Renal insufficiency and ergotism.]. Med Clin (Barc). 1985;84(5):208–9.
Barquinero Máñez J, Tovar Méndez JL, Vallès Prats M, de Luis Sánchez A. Ergotamina e insuficiencia renal aguda. [Ergotamine and acute renal insufficiency.] Med Clin (Barc). 1987;88(2):80–1.
Lund J. Prolonged renal impairment after chronic ergotamine intoxication. Nephrol Dial Transplant. 1992;7(8):879–80.
Luongo MA, Bjornson SS. Liver in ferrous sulfate poisoning—a report of three fatal cases in children and an experimental study. New Engl J Med. 1954;251(25):995–9.
Brown RJ, Gray JD. The mechanism of acute ferrous sulphate poisoning. Can Med Assoc J. 1955;73(3):192–7.
Tenenbein M. Toxicokinetics and toxicodynamics of iron poisoning. Toxicol Lett. 1998;102–103:653–6.
Altiparmak MR, Bilici A, Kisacik B, Ozguroglu M. Flutamide-induced acute renal failure in a patient with metastatic prostate cancer. Med Oncol. 2002;19(2):117–9.
Merck Sharp & Dohme Limited. Remicade 100 mg powder for concentrate for solution for infusion. http://www.medicines.org.uk/emc/medicine/3236. Accessed 21 Jan 2016.
http://www.mhra.gov.uk/home/groups/spcpil/documents/spcpil/con1437715112601.pdf. Accessed 21 Jan 2016.
Perrier A, Martin PY, Favre H, Muller AF, Urban P, Chevrolet JC. Very severe self-poisoning lithium carbonate intoxication causing a myocardial infarction. Chest. 1991;100(3):863–5.
Alvarez Navascués R, Bastardo Z, Fernández Díaz M, Guerediaga J, Quiñones L, Pinto J. Loratadina y nefritis intersticial aguda. [Acute interstitial nephritis induced by loratadine.] Nefrologia. 2003;23(4):355–8.
Girard JP, Haenni B, Bergoz R, Kapanci Y, Cruchaud A. Lupoid hepatitis following administration of penicillin. Case report and immunological studies. Helv Med Acta. 1967;34(1):23–35.
Goldstein L, Ishak KG. Hepatic injury associated with penicillin therapy. Arch Pathol. 1974;98(2):114–7.
Beeley L, Gourevitch A, Kendall MJ. Jaundice after oral penicillin. Lancet. 1976;2(7998):1297.
Oñate J, Montejo M, Aguirrebengoa K, Ruiz-Irastorza G, González de Zárate P, Aguirre C. Hepatotoxicity associated with penicillin V therapy. Clin Infect Dis. 1995;20(2):474–5.
Desmeules S, Bergeron MJ, Isenring P. Acute phosphate nephropathy and renal failure. N Engl J Med. 2003;349(10):1006–7.
Gonlusen G, Akgun H, Ertan A, Olivero J, Truong LD. Renal failure and nephrocalcinosis associated with oral sodium phosphate bowel cleansing clinical patterns and renal biopsy findings. Arch Pathol Lab Med. 2006;130(1):101–6.
Heher EC, Thier SO, Rennke H, Humphreys BD. Adverse renal and metabolic effects associated with oral sodium phosphate bowel preparation. Clin J Am Soc Nephrol. 2008;3(5):1494–503.
Anonymous. Oral sodium phosphate products. New alert on acute phosphate nephropathy. WHO Newslett. 2009;1:1.
Nyberg C, Hendel J, Nielsen OH. The safety of osmotically acting cathartics in colonic cleansing. Nat Rev Gastroenterol Hepatol. 2010;7(10):557–64.
Colic E, Marcussen N. Akut fosfatnefropati som komplikation til udrensning med oral natriumfosfat. [Acute phosphate nephropathy as a complication to bowel cleansing with oral sodium phosphate.]. Ugeskr Laeger. 2011;173(50):3270–1.
Kounis NG, Mazarakis A, Tsigkas G, Giannopoulos S, Goudevenos J. Kounis syndrome: a new twist on an old disease. Future Cardiol. 2011;7(6):805–24.
Bramstedt J, Dissmann R. Akutes prärenales Nierenversagen und Elektrolytentgleisung durch das Cannabis-induzierte Hyperemesis-Syndrom. [Cannabinoid hyperemesis syndrome inducing acute prerenal failure and electrolyte disturbance.]. Dtsch Med Wochenschr. 2011;136(34–35):1720–2.
Kumagai T, Hori Y, Kishida Y, Yakumaru K, Takahashi T, Itou T. Acute renal failure and nephrotic syndrome associated with zafirlukast therapy. Nephrol Dial Transplant. 2003;18(10):2202–3.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this study.
Conflicts of interest
Manfred Hauben is a full-time employee of Pfizer Inc, owns stock/stock options in Pfizer Inc, and owns stock in other pharmaceutical companies that may manufacture and/or market medicines mentioned in this article and/or medicines that may be considered competitor medicines.
Jeffrey K. Aronson has published articles and edited textbooks dealing with adverse drug reactions and has received royalties for textbooks and payments for reports dealing with adverse drug reactions.
Robin E. Ferner has no conflicts of interest that are directly relevant to the content of this study.
Rights and permissions
About this article
Cite this article
Hauben, M., Aronson, J.K. & Ferner, R.E. Evidence of Misclassification of Drug–Event Associations Classified as Gold Standard ‘Negative Controls’ by the Observational Medical Outcomes Partnership (OMOP). Drug Saf 39, 421–432 (2016). https://doi.org/10.1007/s40264-016-0392-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-016-0392-2