Abstract
Background
Since pregnant women are considerably underrepresented in clinical trials, information on optimal dosing in pregnancy is widely lacking. Physiologically based pharmacokinetic (PBPK) modeling may provide a method for predicting pharmacokinetic changes in pregnancy to guide subsequent in vivo pharmacokinetic trials in pregnant women, minimizing associated risks.
Objectives
The goal of this study was to build and verify a population PBPK model that predicts the maternal pharmacokinetics of three predominantly renally cleared drugs (namely cefazolin, cefuroxime, and cefradine) at different stages of pregnancy. It was further evaluated whether the fraction unbound (f u) could be estimated in pregnant women using a proposed scaling approach.
Methods
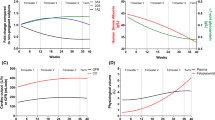
Based on a recent literature review on anatomical and physiological changes during pregnancy, a pregnancy population PBPK model was built using the software PK-Sim®/MoBi®. This model comprised 27 compartments, including nine pregnancy-specific compartments. The PBPK model was verified by comparing the predicted maternal pharmacokinetics of cefazolin, cefuroxime, and cefradine with observed in vivo data taken from the literature. The proposed scaling approach for estimating the f u in pregnancy was evaluated by comparing the predicted f u with experimentally observed f u values of 32 drugs taken from the literature.
Results
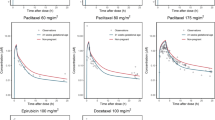
The pregnancy population PBPK model successfully predicted the pharmacokinetics of cefazolin, cefuroxime, and cefradine at all tested stages of pregnancy. All predicted plasma concentrations fell within a 2-fold error range and 85% of the predicted concentrations within a 1.25-fold error range. The f u in pregnancy could be adequately predicted using the proposed scaling approach, although a slight underestimation was evident in case of drugs bound to α1-acidic glycoprotein.
Conclusion
Pregnancy population PBPK models can provide a valuable tool to predict a priori the pharmacokinetics of predominantly renally cleared drugs in pregnant women. These models can ultimately support informed decision making regarding optimal dosing regimens in this vulnerable special population







Similar content being viewed by others
References
Mitchell AA, Gilboa SM, Werler MM, Kelley KE, Louik C, Hernández-Díaz S, et al. Medication use during pregnancy, with particular focus on prescription drugs: 1976–2008. Am J Obstet Gynecol. 2011;205(1):51.e1–8.
Lupattelli A, Spigset O, Twigg MJ, Zagorodnikova K, Mårdby A-C, Moretti ME, et al. Medication use in pregnancy: a cross-sectional, multinational web-based study. BMJ Open. 2014;4(2):e004365.
Herring C, McManus A, Weeks A. Off-label prescribing during pregnancy in the UK: an analysis of 18,000 prescriptions in Liverpool Women’s Hospital. Int J Pharm Pract. 2010;18(4):226–9.
Costantine MM. Physiologic and pharmacokinetic changes in pregnancy. Front Pharmacol. 2014;5:65.
Tasnif Y, Morado J, Hebert MF. Pregnancy-related pharmacokinetic changes. Clin Pharmacol Ther. 2016;100(1):53–62.
Isoherranen N, Thummel KE. Drug metabolism and transport during pregnancy: how does drug disposition change during pregnancy and what are the mechanisms that cause such changes? Drug Metab Dispos. 2013;41(2):256–62.
Hebert MF. Impact of pregnancy on maternal pharmacokinetics of medications. In: Mattison DR, editor. Clinical pharmacology during pregnancy, 1st ed. Waltham: Academic Press, Elsevier Inc.; 2013. p. 17–39.
Baylis F. Pregnant women deserve better. Nature. 2010;465(7299):689–90.
Foulkes MA, Grady C, Spong CY, Bates A, Clayton JA. Clinical research enrolling pregnant women: a workshop summary. J Womens Health (Larchmt). 2011;20(10):1429–32.
McCormack SA, Best BM. Obstetric pharmacokinetic dosing studies are urgently needed. Front Pediatr. 2014;2:9.
Belton J. The desperate need to include pregnant women in clinical research: proposed recommendations to increase enrollment of pregnant women in research. 2015. Law School Student Scholarship. Paper 660. http://scholarship.shu.edu/student_scholarship/660. Accessed 17 Mar 2017.
Ayad M, Costantine MM, editors. Epidemiology of medications use in pregnancy. Semin Perinatol. 2015;39:508–11.
Faden R, Lyerly A, Little M. A custom drug. New York Times; 2009. p. WK10.
Luecke RH, Wosilait WD, Pearce BA, Young JF. A physiologically based pharmacokinetic computer model for human pregnancy. Teratology. 1994;49(2):90–103.
Gaohua L, Abduljalil K, Jamei M, Johnson TN, Rostami-Hodjegan A. A pregnancy physiologically based pharmacokinetic (p-PBPK) model for disposition of drugs metabolized by CYP1A2, CYP2D6 and CYP3A4. Br J Clin Pharmacol. 2012;74(5):873–85.
Ke A, Nallani S, Zhao P, Rostami-Hodjegan A, Unadkat JD. A PBPK model to predict disposition of CYP3A-metabolized drugs in pregnant women: verification and discerning the site of CYP3A induction. CPT Pharmacomet Syst Pharmacol. 2012;1(9):1–10.
Xia B, Heimbach T, Gollen R, Nanavati C, He H. A simplified PBPK modeling approach for prediction of pharmacokinetics of four primarily renally excreted and CYP3A metabolized compounds during pregnancy. AAPS J. 2013;15(4):1012–24.
Wagner C, Zhao P, Pan Y, Hsu V, Grillo J, Huang S, et al. Application of physiologically based pharmacokinetic (PBPK) modeling to support dose selection: report of an FDA public workshop on PBPK. CPT Pharmacomet Syst Pharmacol. 2015;4(4):226–30.
Dallmann A, Ince I, Meyer M, Willmann S, Eissing T, Hempel G. Gestation-specific changes in the anatomy and physiology of healthy pregnant women: an extended repository of model parameters for physiologically based pharmacokinetic modeling in pregnancy. Clin pharmacokinet. 2017. doi:10.1007/s40262-017-0539-z.
Eissing T, Kuepfer L, Becker C, Block M, Coboeken K, Gaub T, et al. A computational systems biology software platform for multiscale modeling and simulation: integrating whole-body physiology, disease biology, and molecular reaction networks. Front Physiol. 2011;2(4):1–10.
PK-Sim user manual and software, 6.3. Leverkusen, Germany: Bayer Technology Services GmbH; 2016.
Willmann S, Höhn K, Edginton A, Sevestre M, Solodenko J, Weiss W, et al. Development of a physiology-based whole-body population model for assessing the influence of individual variability on the pharmacokinetics of drugs. J Pharmacokinet Pharmacodyn. 2007;34(3):401–31.
Willmann S, Lippert J, Sevestre M, Solodenko J, Fois F, Schmitt W. PK-Sim®: a physiologically based pharmacokinetic ‘whole-body’model. Biosilico. 2003;1(4):121–4.
Gyssens IC. Preventing postoperative infections. Drugs. 1999;57(2):175–85.
Nightingale CH, Greene DS, Quintiliani R. Pharmacokinetics and clinical use of cephalosporin antibiotics. J Pharm Sci. 1975;64(12):1899–927.
Ueo H, Motohashi H, Katsura T, Inui KI. Human organic anion transporter hOAT3 is a potent transporter of cephalosporin antibiotics, in comparison with hOAT1. Biochem Pharmacol. 2005;70(7):1104–13.
Uwai Y, Saito H, Inui KI. Rat renal organic anion transporter rOAT1 mediates transport of urinary-excreted cephalosporins, but not of biliary-excreted cefoperazone. Drug Metab Pharmacokinet. 2002;17(2):125–9.
Ci L, Kusuhara H, Adachi M, Schuetz JD, Takeuchi K, Sugiyama Y. Involvement of MRP4 (ABCC4) in the luminal efflux of ceftizoxime and cefazolin in the kidney. Mol Pharmacol. 2007;71(6):1591–7.
Philipson A, Stiernstedt G, Ehrnebo M. Comparison of the pharmacokinetics of cephradine and cefazolin in pregnant and non-pregnant women. Clin Pharmacokinet. 1987;12(2):136–44.
Fahey JO. Clinical management of intra-amniotic infection and chorioamnionitis: a review of the literature. J Midwifery Womens Health. 2008;53(3):227–35.
Mittal P, Wing DA. Urinary tract infections in pregnancy. Clin Perinatol. 2005;32(3):749–64.
Foord R. Cefuroxime: human pharmacokinetics. Antimicrob Agents Chemother. 1976;9(5):741–7.
Garton A, Rennie R, Gilpin J, Marrelli M, Shafran S. Comparison of dose doubling with probenecid for sustaining serum cefuroxime levels. J Antimicrob Chemother. 1997;40(6):903–6.
Verhagen C, Mattie H, Strijen E. The renal clearance of cefuroxime and ceftazidime and the effect of probenecid on their tubular excretion. Br J Clin Pharmacol. 1994;37(2):193–7.
Philipson A, Stiernstedt G. Pharmacokinetics of cefuroxime in pregnancy. Am J Obstet Gynecol. 1982;142(7):823–8.
Bousfield P, Browning A, Mullinger B, Elstein M. Cefuroxime: potential use in pregnant women at term. Br J Obstet Gynaecol. 1981;88(2):146–9.
Ugwumadu A. Managing bacterial infections in pregnancy and the puerperium. Prescriber. 2010;21(21):53–7.
Rattie ES, Bernardo PD, Ravin LJ. Pharmacokinetic interpretation of cephradine levels in serum after intravenous and extravascular administration in humans. Antimicrob Agents Chemother. 1976;10(2):283–7.
Neiss ES. Cephradine—a summary of preclinical studies and clinical pharmacology. J Ir Med Assoc. 1973;Suppl.:1–12.
Mischler TW, Sugerman AA, Willard DA, Brannick LJ, Neiss ES. Influence of probenecid and food on the bioavailability of cephradine in normal male subjects. J Clin Pharmacol. 1974;14(11):604–11.
Cihlar T, Ho ES. Fluorescence-based assay for the interaction of small molecules with the human renal organic anion transporter 1. Anal Biochem. 2000;283(1):49–55.
Tanihara Y, Masuda S, Sato T, Katsura T, Ogawa O, Inui KI. Substrate specificity of MATE1 and MATE2-K, human multidrug and toxin extrusions/H+-organic cation antiporters. Biochem Pharmacol. 2007;74(2):359–71.
Zappala AF, Holl WW, Post A. Cefazolin. In: Florey K, editor. Analytical profiles of drug substances. New York: Academic Press; 1975. p. 1–20.
PubChem. https://pubchem.ncbi.nlm.nih.gov/. Accessed 04 Mar 2016.
Gulyaeva N, Zaslavsky A, Lechner P, Chait A, Zaslavsky B. Relative hydrophobicity of organic compounds measured by partitioning in aqueous two-phase systems. J Chromatogr B Biomed Sci Appl. 2000;743(1):187–94.
Nau R, Sörgel F, Eiffert H. Penetration of drugs through the blood-cerebrospinal fluid/blood-brain barrier for treatment of central nervous system infections. Clin Microbiol Rev. 2010;23(4):858–83.
Yamana T, Tsuji A. Comparative stability of cephalosporins in aqueous solution: kinetics and mechanisms of degradation. J Pharm Sci. 1976;65(11):1563–74.
Karalis V, Tsantili-Kakoulidou A, Macheras P. Quantitative structure–pharmacokinetic relationships for disposition parameters of cephalosporins. Eur J Pharm Sci. 2003;20(1):115–23.
Park E-S, Maniar M, Shah JC. Biodegradable polyanhydride devices of cefazolin sodium, bupivacaine, and taxol for local drug delivery: preparation, and kinetics and mechanism of in vitro release. J Control Release. 1998;52(1):179–89.
DrugBank. http://www.drugbank.ca/. Accessed 02 Mar 2016.
Yalkowsky SH, Dannenfelser RM. Aquasol database of aqueous solubility. Tucson: College of Pharmacy, University of Arizona; 1992.
Poulin P, Schoenlein K, Theil FP. Prediction of adipose tissue: plasma partition coefficients for structurally unrelated drugs. J Pharm Sci. 2001;90(4):436–47.
Poulin P, Theil FP. A priori prediction of tissue: plasma partition coefficients of drugs to facilitate the use of physiologically-based pharmacokinetic models in drug discovery. J Pharm Sci. 2000;89(1):16–35.
Schmitt W. General approach for the calculation of tissue to plasma partition coefficients. Toxicol In Vitro. 2008;22(2):457–67.
Arayne MS, Sultana N, Afzal M. Cephradine antacids interaction studies. Pak J Pharm Sci. 2007;20(3):179–84.
Rodgers T, Rowland M. Physiologically based pharmacokinetic modelling 2: predicting the tissue distribution of acids, very weak bases, neutrals and zwitterions. J Pharm Sci. 2006;95(6):1238–57.
Mrestani Y, Mrestani-Klaus C, Bretschneider B, Neubert RH. Improvement of lipophilicity and membrane transport of cefuroxime using in vitro models. Eur J Pharm Biopharm. 2004;58(3):653–7.
Willmann S, Schmitt W, Keldenich J, Lippert J, Dressman JB. A physiological model for the estimation of the fraction dose absorbed in humans. J Med Chem. 2004;47(16):4022–31.
Sloop CH, Dory L, Roheim PS. Interstitial fluid lipoproteins. J Lipid Res. 1987;28(3):225–37.
Castellucci M, Kaufmann P. A three-dimensional study of the normal human placental villous core: II. Stromal architecture. Placenta. 1982;3(3):269–85.
Jones C, Harris L, Whittingham J, Aplin J, Mayhew T. A re-appraisal of the morphophenotype and basal lamina coverage of cytotrophoblasts in human term placenta. Placenta. 2008;29(2):215–9.
Meuldermans W, Hurkmans R, Heykants J. Plasma protein binding and distribution of fentanyl, sufentanil, alfentanil and lofentanil in blood. Arch Int Pharmacodyn Ther. 1982;257(1):4–19.
Meuldermans W, Woestenborghs R, Noorduin H, Camu F, van Steenberge A, Heykants J. Protein binding of the analgesics alfentanil and sufentanil in maternal and neonatal plasma. Eur J Clin Pharmacol. 1986;30(2):217–9.
Herngren L, Ehrnebo M, Boreus L. Drug binding to plasma proteins during human pregnancy and in the perinatal period. Studies on cloxacillin and alprenolol. Dev Pharmacol Ther. 1983;6(2):110–24.
Crawford JS, Hooi HW. Binding of bromsulphthalein by serum albumin from pregnant women, neonates and subjects on oral contraceptives. Br J Anaesth. 1968;40(10):723–9.
Wulf H, Münstedt P, Maier C. Plasma protein binding of bupivacaine in pregnant women at term. Acta Anaesthesiol Scand. 1991;35(2):129–33.
Zhang F, Xue J, Shao J, Jia L. Compilation of 222 drugs’ plasma protein binding data and guidance for study designs. Drug Discov Today. 2012;17(9):475–85.
Bardy A, Hiilesmaa V, Teramo K, Neuvonen P. Protein binding of antiepileptic drugs during pregnancy, labor, and puerperium. Ther Drug Monit. 1990;12(1):40–6.
Obach RS, Lombardo F, Waters NJ. Trend analysis of a database of intravenous pharmacokinetic parameters in humans for 670 drug compounds. Drug Metab Dispos. 2008;36(7):1385–405.
Bourget P, Fernandez H, Quinquis V, Delouis C. Pharmacokinetics and protein binding of ceftriaxone during pregnancy. Antimicrob Agents Chemother. 1993;37(1):54–9.
Crauwels H, Kakuda T, Ryan B, Zorrilla C, Osiyemi O, Yasin S, et al. Pharmacokinetics of once-daily darunavir/ritonavir in HIV-1–infected pregnant women. HIV Med. 2016;17:643–52.
Tsuei SE, Petersen MC, Ashley JJ, McBride WG, Moore RG. Disporition of synthetic glucocorticoids. II. Dexamethasone in parturient women. Clin Pharmacol Ther. 1980;28(1):88–98.
Osathanondh R, Tulchinsky D, Kamali H, deM Fencl M, Taeusch HW. Dexamethasone levels in treated pregnant women and newborn infants. J Pediatr. 1977;90(4):617–20.
Perucca E, Ruprah M, Richens A. Altered drug binding to serum proteins in pregnant women: therapeutic relevance. J R Soc Med. 1981;74(6):422–6.
Wood M, Wood AJ. Changes in plasma drug binding and α1-acid glycoprotein in mother and newborn infant. Clin Pharmacol Ther. 1981;29(4):522–6.
Ridd MJ, Brown KF, Nation RL, Collier CB. The disposition and placental transfer of diazepam in cesarean section. Clin Pharmacol Ther. 1989;45(5):506–12.
Hebert M, Easterling T, Kirby B, Carr D, Buchanan M, Rutherford T, et al. Effects of pregnancy on CYP3A and P-glycoprotein activities as measured by disposition of midazolam and digoxin: a University of Washington Specialized Center of Research Study. Clin Pharmacol Ther. 2008;84(2):248–53.
Kim J. Pharmacokinetics and pharmacodynamics of the selective serotonin reuptake inhibitors, fluoxetine and paroxetine, during pregnancy and the nursing period. Vancouver: University of British Columbia; 2000.
Cutler RE, Blair AD. Clinical pharmacokinetics of frusemide. Clin Pharmacokinet. 1979;4(4):279–96.
Riva E, Farina P, Tognoni G, Bottino S, Orrico C, Pardi G. Pharmacokinetics of furosemide in gestosis of pregnancy. Eur J Clin Pharmacol. 1978;14(5):361–6.
Aweeka F, Stek A, Best B, Hu C, Holland D, Hermes A, et al. Lopinavir protein binding in HIV-1-infected pregnant women. HIV Med. 2010;11(4):232–8.
Pond SM, Kreek MJ, Tong TG, Raghunath J, Benowitz NL. Altered methadone pharmacokinetics in methadone-maintained pregnant women. J Pharmacol Exp Ther. 1985;233(1):1–6.
Högstedt S, Lindberg B, Peng DR, Regårdh CG, Rane A. Pregnancy-induced increase in metoprolol metabolism. Clin Pharmacol Ther. 1985;37(6):688–92.
Asali L, Brown K. Naloxone protein binding in adult and foetal plasma. Eur J Clin Pharmacol. 1984;27(4):459–63.
Mazoit JX, Samii K. Binding of propofol to blood components: implications for pharmacokinetics and for pharmacodynamics. Br J Clin Pharmacol. 1999;47(1):35–42.
Gin T, Yau G, Jong W, Tan P, Leung R, Chan K. Disposition of propofol at caesarean section and in the postpartum period. Br J Anaesth. 1991;67(1):49–53.
Lalonde RL, Tenero DM, Burlew BS, Herring VL, Bottorff MB. Effects of age on the protein binding and disposition of propranolol stereoisomers. Clin Pharmacol Ther. 1990;47(4):447–55.
Belpaire F, Wynant P, Trappen P, Dhont M, Verstraete A, Bogaert M. Protein binding of propranolol and verapamil enantiomers in maternal and foetal serum. Br J Clin Pharmacol. 1995;39(2):190–3.
Morton C, Bloomfield S, Magnusson A, Jozwiak H, McClure J. Ropivacaine 0.75% for extradural anaesthesia in elective caesarean section: an open clinical and pharmacokinetic study in mother and neonate. Br J Anaesth. 1997;79(1):3–8.
Crawford JS, Hooi HW. Binding of salicylic acid and sulphanilamide in serum from pregnant patients, cord blood and subjects taking oral contraceptives. Br J Anaesth. 1968;40(11):825–33.
Gardner M, Schatz M, Cousins L, Zeiger R, Middleton E, Jusko W. Longitudinal effects of pregnancy on the pharmacokinetics of theophylline. Eur J Clin Pharmacol. 1987;32(3):289–95.
Connelly TJ, Ruo TI, Frederiksen MC, Atkinson AJ. Characterization of theophylline binding to serum proteins in pregnant and nonpregnant women. Clin Pharmacol Ther. 1990;47(1):68–72.
Gross AS, Heuer B, Eichelbaum M. Stereoselective protein binding of verapamil enantiomers. Biochem Pharmacol. 1988;37(24):4623–7.
Kramer MS. Determinants of low birth weight: methodological assessment and meta-analysis. Bull World Health Organ. 1987;65(5):663–737.
Wu G, Baraldo M, Furlanut M. Calculating percentage prediction error: a user’s note. Pharmacol Res. 1995;32(4):241–8.
De Sousa Mendes M, Hirt D, Urien S, Valade E, Bouazza N, Foissac F, et al. Physiologically-based pharmacokinetic modeling of renally excreted antiretroviral drugs in pregnant women. Br J Clin Pharmacol. 2015;80(5):1031–41.
Abduljalil K, Furness P, Johnson TN, Rostami-Hodjegan A, Soltani H. Anatomical, physiological and metabolic changes with gestational age during normal pregnancy. Clin Pharmacokinet. 2012;51(6):365–96.
Christensen T, Klebe JG, Bertelsen V, Hansen HE. Changes in renal volume during normal pregnancy. Acta Obstet Gynecol Scand. 1989;68(6):541–3.
Cietak K, Newton J. Serial qualitative maternal nephrosonography in pregnancy. Br J Radiol. 1985;58(689):399–404.
Farrell D, Morrissey I, De Rubeis D, Robbins M, Felmingham D. A UK multicentre study of the antimicrobial susceptibility of bacterial pathogens causing urinary tract infection. J Infect. 2003;46(2):94–100.
Chitty LS, Altman DG. Charts of fetal size: kidney and renal pelvis measurements. Prenat Diagn. 2003;23(11):891–7.
Arant BS. Developmental patterns of renal functional maturation compared in the human neonate. J Pediatr. 1978;92(5):705–12.
Verner M-A, Ayotte P, Muckle G, Charbonneau M, Haddad S. A physiologically based pharmacokinetic model for the assessment of infant exposure to persistent organic pollutants in epidemiologic studies. Environ Health Persp. 2009;117(3):481.
Yoon M, Schroeter JD, Nong A, Taylor MD, Dorman DC, Andersen ME, et al. Physiologically based pharmacokinetic modeling of fetal and neonatal manganese exposure in humans: describing manganese homeostasis during development. Toxicol Sci. 2011;122:297–316.
Verner M-A, Loccisano AE, Morken N-H, Yoon M, Wu H, McDougall R, et al. Associations of perfluoroalkyl substances (PFAS) with lower birth weight: an evaluation of potential confounding by glomerular filtration rate using a physiologically based pharmacokinetic model (PBPK). Environ Health Perspect. 2015;123(12):1317–24.
De Sousa Mendes M, Hirt D, Vinot C, Valade E, Lui G, Pressiat C, et al. Prediction of human fetal pharmacokinetics using ex vivo human placenta perfusion studies and physiologically based models. Br J Clin Pharmacol. 2016;81:646–57.
De Sousa Mendes M, Lui G, Zheng Y, Pressiat C, Hirt D, Valade E, et al. A physiologically-based pharmacokinetic model to predict human fetal exposure for a drug metabolized by several CYP450 pathways. Clin Pharmacokinet. 2016; doi:10.1007/s40262-016-0457-5 (Epub 2016 Oct 21).
El-Masri H, Kleinstreuer N, Hines RN, Adams L, Tal T, Isaacs K, et al. Integration of life-stage physiologically based pharmacokinetic models with adverse outcome pathways and environmental exposure models to screen for environmental hazards. Toxicol Sci. 2016;152(1):230–43. doi:10.1093/toxsci/kfw082.
Zhang Z, Unadkat JD. Verification of a maternal-fetal physiologically based pharmacokinetic model for passive placental permeability drugs. Drug Metab Dispos. 2017; doi:10.1124/dmd.116.073957 (Epub 2017 Jan 3).
Routledge P. The plasma protein binding of basic drugs. Br J Clin Pharmacol. 1986;22(5):499–506.
Webb D, Buss D, Fifield R, Bateman D, Routledge P. The plasma protein binding of metoclopramide in health and renal disease. Br J Clin Pharmacol. 1986;21(3):334–6.
Bailey DN, Briggs JR. The binding of selected therapeutic drugs to human serum α-1 acid glycoprotein and to human serum albumin in vitro. Ther Drug Monit. 2004;26(1):40–3.
Acknowledgements
The authors would like to thank Kirstin Thelen (Bayer AG) and Christoph Niederalt (Bayer AG) for valuable discussions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This publication and the work involved were funded by Bayer AG.
Conflict of interest
Andre Dallmann is a PhD student at the University of Münster and is employed on a grant from Bayer AG. Ibrahim Ince, Juri Solodenko, Michaela Meyer, Stefan Willmann, and Thomas Eissing were employed by Bayer AG during preparation of this manuscript and are potential stock holders of Bayer AG. Georg Hempel has received a research grant from Bayer AG since 2008.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dallmann, A., Ince, I., Solodenko, J. et al. Physiologically Based Pharmacokinetic Modeling of Renally Cleared Drugs in Pregnant Women. Clin Pharmacokinet 56, 1525–1541 (2017). https://doi.org/10.1007/s40262-017-0538-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-017-0538-0