Abstract
Background and Objective
Several features favor paracetamol (acetaminophen) administration by the intravenous rather than the oral route in the postoperative setting. This study compared the pharmacokinetics and bioavailability of oral and intravenous paracetamol when given with or without an opioid, morphine.
Methods
In this randomized, single-blind, parallel, repeat-dose study in healthy adults, subjects received four repeat doses of oral or intravenous 1000 mg paracetamol at 6-h intervals, and morphine infusions (0.125 mg/kg) at the 2nd and 3rd intervals. Comparisons of plasma pharmacokinetic profiles were conducted before, during, and after opioid co-administrations.
Results
Twenty-two subjects were included in the pharmacokinetic analysis. Observed paracetamol peak concentration (C max) and area under the plasma concentration-time curve over the dosing interval (AUC0–6) were reduced when oral paracetamol was co-administered with morphine (reduced from 11.6 to 7.25 µg/mL and from 31.00 to 25.51 µg·h/mL, respectively), followed by an abruptly increased C max and AUC0–6 upon discontinuation of morphine (to 13.5 µg/mL and 52.38 µg·h/mL, respectively). There was also a significantly prolonged mean time to peak plasma concentration (T max) after the 4th dose of oral paracetamol (2.84 h) compared to the 1st dose (1.48 h). However, pharmacokinetic parameters of paracetamol were not impacted when intravenous paracetamol was co-administered with morphine.
Conclusions
Morphine co-administration significantly impacted the pharmacokinetics of oral but not intravenous paracetamol. The abrupt release of accumulated paracetamol at the end of morphine-mediated gastrointestinal inhibition following oral but not intravenous administration of paracetamol suggests that intravenous paracetamol provides a better option for the management of postoperative pain.
ClinicalTrials.gov Identifier
NCT02848729.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Morphine co-administration significantly impacts the pharmacokinetics of oral but not intravenous paracetamol by reducing/delaying its absorption and substantially increasing the inter-individual pharmacokinetic variability |
Intravenous paracetamol produces more predictable blood levels than oral paracetamol when either are co-administered with morphine, and thus provides a better option for the management of postoperative pain in the context of multimodal analgesia |
1 Introduction
Opioid agonists such as morphine continue to be important analgesics in the treatment of pain in the immediate perioperative and critical care settings [1], although they are associated with numerous adverse drug events [2]. In an effort to reduce opioid exposure and thus minimize opioid-related adverse drug events, non-opioid analgesics are being incorporated as foundational therapy into multimodal analgesia protocols for the management of postoperative pain. Numerous surgical and nonsurgical medical societies and accrediting and quality organization guidelines recommend the use of multimodal analgesia (MMA) in order to reduce exposure to opioids [3,4,5,6,7,8,9]. Many also recommend scheduled use of non-opioid analgesics (paracetamol [acetaminophen], non-steroidal anti-inflammatory drugs [NSAIDs]) as the first- line foundation of MMA.
A recent review [10] and the American Society of Anesthesiologists (ASA) guidelines [11] have suggested there is inadequate differentiation of intravenous and oral paracetamol to warrant the higher acquisition cost and longer time to administer the intravenous formulation. Given that opioids remain a key component of post-operative pain management, it is important to note that opioids, along with surgical stress may have a negative impact on orally administered drugs. Opioids inhibit gastrointestinal motility, including delaying gastric emptying [12] and thus the route of administration of analgesics used in multimodal regimens may be an important consideration. Specifically, absorption of orally administered paracetamol may be compromised in patients receiving opioids, which could reduce efficacy. Furthermore, delayed absorption of orally administered paracetamol in patients receiving opioids could result in gastric accumulation of paracetamol, thereby markedly changing the pharmacokinetic profile during and after opioid administration.
Paracetamol can significantly reduce the use of opioid analgesics when concomitantly administered for the treatment of acute pain [13]. The use of intravenous paracetamol concomitantly with opioids has gained increased popularity for postsurgical pain relief over orally administered paracetamol because it provides an immediate peak plasma concentration [14] and is thought to provide a faster analgesic effect. Bioavailability of intravenous paracetamol is 100%, whereas the oral bioavailability of paracetamol can be as low as 79% [15]. In a study comparing the pharmacokinetics of paracetamol 1 g administered via intravenous, oral, or rectal routes, cerebrospinal fluid (CSF) area under the concentration-time curve from 0 to 6 h (AUC0–6) was 24.9, 14.2, and 10.3 µg·h/mL, respectively. Absorption phase, variability in plasma and CSF were greater with oral and rectal administration than with intravenous administration [14].
Furthermore, in patients receiving opioids, the absorption of orally administered paracetamol may be delayed and could result in gastric accumulation of paracetamol, thereby markedly changing the pharmacokinetic profile. Opioid-induced inhibition of gastrointestinal function would not be expected to affect intravenous paracetamol pharmacokinetics.
To assess potential interaction, the current study evaluated whether an opioid, intravenous morphine, commonly used to treat postsurgical pain, affects the absorption of oral or intravenous paracetamol and results in altered pharmacokinetics during and after co-administration in healthy subjects.
2 Methods
This was an institutional review board (IRB)-approved, randomized, single-blind, parallel, single-site, repeat-dose study (NCT02848729) in healthy adult subjects from 18 to 55 years of age (inclusive). The study was completed with four cohorts of subjects: both males and non-pregnant females were enrolled in Cohort 1, and male subjects only in Cohorts 2–4. Subjects were randomly assigned to 1 of 2 parallel groups: 4 repeat doses of 1000 mg oral paracetamol (2 tablets, 500 mg/tablet; Mallinckrodt Inc., Hazelwood, Missouri, USA) at hours 0, 6, 12, and 18, and a dummy 15-min intravenous infusion of saline at the same time points, or 4 doses of intravenous paracetamol (1000 mg/100 mL; Ofirmev®, Mallinckrodt Inc., Hazelwood, Missouri, USA) delivered as an infusion at hours 0, 6, 12, and 18, and 2 placebo tablets at the same time points. Intravenous morphine infusions (0.125 mg/kg in 100 mL saline, approximately 15 min; morphine sulfate injection 10 mg/mL, 1 mL, West-Ward Pharmaceutical Corp., Eatontown, New Jersey, USA) occurred at hours 6 and 12 for all subjects. The total study duration for each subject was approximately 38 days. A drop-out rate of 50% was anticipated due to the required discontinuation of subjects who experienced emesis and the known association between morphine and emesis.
2.1 Bioanalytical Method to Determine Plasma Concentration of Paracetamol
Venous blood was collected by venipuncture in K2EDTA-containing tubes, and plasma was separated and stored at −80 °C. Quantification of paracetamol in plasma was performed via high-performance liquid chromatography (HPLC) with paired mass spectrometry (MS/MS). Analysis of human plasma samples began on 16 March 2016 and was completed on 01 April 2016. Plasma samples were analyzed with a lower limit of quantitation of 0.100 µg/mL and upper limit of quantitation of 50.0 µg/mL. Each calibration curve was calculated using a linear (1/concentration2 weighted) least-squares regression algorithm. Precision and accuracy were evaluated by replicate analyses of human plasma quality control pools prepared at five concentrations spanning the calibration range. To demonstrate reproducible quantitation of incurred subject samples, approximately 10% of the study samples were re-assayed. Incurred sample repeats were considered acceptable if the original and re-assay values from two-thirds of the repeated samples had a relative percent difference of ≤ 20%. The results of the incurred sample repeats met the acceptance criteria.
2.2 Pharmacokinetics
Venous blood samples (6 mL each) for measuring paracetamol concentrations were collected at the following times:
-
up to 30 min prior to the administration of the first dose of paracetamol;
-
at 15, 30, and 45 min (± 2 min), 1, 2, 3, 4, 6 h (± 5 min for hours 1, 2, 3, and 4; ± 10 min for hour 6) after the first paracetamol dose;
-
at 30 min (± 2 min), 1, 2, 3, 4 and 6 h (± 5 min for hours 1, 2, 3, and 4; ± 10 min for hour 6) after both second and third paracetamol doses;
-
and at 15, 30, and 45 min (± 2 min), 1, 2, 3, 4, 6, 8, 10, 12, and 18 h (± 5 min for hours 1, 2, 3, 4, 8, 10, 12 and 18; ± 10 min for hour 6) after the fourth dose of paracetamol.
Blood draws at 6 h after the first, second, and third paracetamol doses were collected before the next paracetamol dose that was to be administered.
A total of 33 blood samples were collected for each subject. The schedules for blood samples collection were the same for all study groups.
Approximately 200 mL of blood for determination of plasma concentrations of paracetamol was collected, and 18 mL was collected for clinical laboratory tests at the screening visit and check-in. The time (24-h clock) and date of collection for each sample was recorded.
2.3 Safety
The following safety assessments were evaluated: medical/surgical history, physical examination, pregnancy testing (Cohort 1 female subjects only) electrocardiogram, vital signs, clinical laboratory testing (including standard assessment of renal and hepatic function), pulse oximetry, concomitant medication use, and assessment of adverse events (AEs).
2.4 Statistical Analysis
This study was regarded as exploratory and thus sample size was not determined by power analysis. Two populations were identified and analyzed in this study. The safety population comprised subjects enrolled in the study that received any quantity of study drug. The per-protocol population comprised subjects who received all study drug doses and provided all 33 protocol-specified blood samples within required time frames without any major protocol deviations.
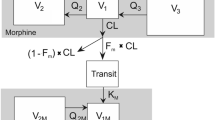
Pharmacokinetic simulations were performed to predict the paracetamol concentrations after the second, third, and fourth doses of paracetamol assuming no co-administration of morphine. The simulations were based on the observed pharmacokinetic values after the first dose of orally or intravenously administered paracetamol. Simulations were performed using Phoenix® WinNonlin® V 6.4 (Certara, Princeton, NJ).
Descriptive statistics for continuous variables included number of values (N), mean, standard deviation (SD), median, minimum, and maximum, unless otherwise noted. Frequency and percentages were calculated for categorical variables. In anticipation of having a limited number of subjects available for final analysis (due to a high rate of emesis-related drop-outs), the paired t-test was used in comparisons within the oral paracetamol group or within the intravenous paracetamol group, across paracetamol doses, and the two-sample t-test was used in comparisons across the oral and intravenous paracetamol groups. To control for multiple comparisons, both raw p values from the paired t-test and Hochberg adjusted p values were calculated, and only the adjusted p values were presented. All statistical significance testing was 2-tailed using α = 0.05.
Data summary and analyses were performed with SAS® 9.2 or higher.
3 Results
3.1 Subject Disposition
A total of 50 subjects were enrolled in the study, 23 subjects (46.0%) completed, and 27 subjects (54.0%) were discontinued early. Twenty-six subjects (52.0%) discontinued due to emesis and 1 subject withdrew consent to participate in the study; no subjects discontinued due to any other treatment-emergent adverse event (TEAE). A total of 22 subjects were included in the per-protocol population and used in the pharmacokinetic analysis. One subject completed the study but did not provide all pharmacokinetic samples and thus was excluded from the per-protocol population. No data imputation was performed.
3.2 Demographic and Baseline Characteristics
Of the 50 subjects enrolled, 34 (68%) were white and 16 (32%) were black or African American. The majority (64%; 32/50) were not Hispanic or Latino in ethnicity. Across all enrolled subjects, the mean age was 32.8 years (range 18–55 years), and the mean body mass index was 27.78 kg/m2. There were 41 (82%) male and 9 (18%) female subjects.
Of the 22 subjects included in the per-protocol population, the majority were white (16 of 22 subjects; 72.7%), and other subjects (6 of 22 subjects; 27.3%) were black or African American. Subjects in the per-protocol population had a mean age of 32.8 years (range 18–55 years), and had a mean body mass index of 28.03 kg/m2. There were 21 male subjects (95.5%) and 1 female subject (4.5%).
3.3 Pharmacokinetics
Mean plasma pharmacokinetic parameters of oral paracetamol administered before, during, and after morphine administration are presented in Table 1.
Observed paracetamol peak concentration (C max) and area under the plasma concentration-time curve over the 6-h dosing interval (AUC0–6) for paracetamol following oral administration were reduced when co-administered with morphine, and increased after morphine was discontinued. The mean AUC0–6 was decreased from 31.00 µg·h/mL after the second dose (28.51 µg·h/mL) and third dose (25.31 µg·h/mL) of oral paracetamol, and then sharply increased following the fourth dose (52.38 µg·h/mL), resulting in statistically significant increases between fourth and first dose (p < 0.001), and fourth and third dose (p = 0.004). The mean C max followed a similar trend, decreasing from 11.6 µg/mL after the first dose to 7.29 µg/mL after the second dose and 7.25 µg/mL after the third dose of paracetamol, and then increasing significantly after the fourth dose (13.5 µg/mL, p = 0.019, when compared with the third dose).
Time to peak plasma concentration (T max) for oral paracetamol was prolonged during and after co-administration of morphine. Significantly prolonged mean T max (i.e., delayed C max) values were also observed after the fourth (2.84 h, p = 0.031) dose of oral paracetamol when compared to the first dose (1.48 h).
Concomitant use of morphine also resulted in greater variability in orally administered paracetamol exposures, plasma concentrations, and T max (Table 1; Figs. 1 and 2a). The SDs of the pharmacokinetic parameters, AUC0–6, C max, plasma concentration at 6 h (C6), and T max, after the third and fourth doses of oral paracetamol, in most cases, were greater than those after the first and second doses, indicating greater inter-subject variability as a result of interaction with co-administered morphine (Table 1). Additionally, the concentration of the drug that produces 50% of the maximal effect (EC50), which for paracetamol is purported to be in the range of 10–15 µg/mL [16, 17], was rarely reached following oral administration (Fig. 3a).
Individual plasma concentration-time profiles of oral paracetamol showing large inter-subject variability. Subjects received Treatment A, i.e., 4 repeat doses of 1000 mg oral paracetamol (2 × 500 mg tablets) and an intravenous infusion of saline every 6 h [hours 0, 6, 12, and 18 (blue arrows)], and 2 infusions of intravenous morphine (0.125 mg/kg) at hours 6 and 12 (black arrows)
Predicted (solid blue) and observed (dashed red) pharmacokinetic profiles for a oral and b intravenous paracetamol. Subjects received Treatment A, i.e., 4 repeat doses of 1000 mg oral paracetamol (2 × 500 mg tablets) and an intravenous infusion of saline every 6 h (hours 0, 6, 12, and 18), and 2 infusions of intravenous morphine (0.125 mg/kg) at hours 6 and 12
In contrast, the values of all critical pharmacokinetic parameters after each intravenous dose of paracetamol, administered before, during, and after morphine administration, were found to be very similar (Fig. 2b). Furthermore, following intravenous administration of paracetamol, EC50 was reliably met in subjects following each dose (Fig. 3b).
Mean plasma pharmacokinetic parameters of intravenous paracetamol are presented in Table 2. Because no blood samples were collected at 0.25 h after intravenous paracetamol, doses 2 and 3, C max and T max values reflect the lack of sample collection before 0.25 h. Concentrations at 0.5 h after each dose were measured, which were comparable across all four doses of paracetamol. Therefore, C0.5 is more relevant in representing the early phase of the paracetamol concentrations when inter-dose comparison is needed. Overall, the values of all critical pharmacokinetic parameters after each intravenous dose of paracetamol were found to be similar. The AUC0–6, AUC0.5–6, C0.5, and C6 for doses 2, 3, and 4 are within the bioequivalence limits compared to the first dose but demonstrated a trend toward small increases with each additional dose. This is consistent with drug accumulation as expected in multi-dose paracetamol administration.
3.4 Safety
Overall, 39 subjects (78.0%) experienced at least 1 TEAE, all of which were mild or moderate in severity. The most frequently reported TEAEs (experienced by ≥ 10% of subjects) were vomiting (26 subjects, 52.0%), nausea (22 subjects, 44.0%), dizziness (8 subjects, 16.0%), and somnolence (5 subjects, 10.0%). No other TEAEs were reported in more than 4 subjects. Although statistical comparisons were not performed, there were fewer subjects with TEAEs after receiving intravenous paracetamol (73.9%) than after receiving oral paracetamol (81.5%). There were fewer subjects who experienced the TEAE of vomiting after receiving intravenous paracetamol (47.8%) than after receiving oral paracetamol (55.6%). A total of 26 subjects discontinued the study due to emesis. Ten of the 26 subjects discontinued due to emesis after receiving their first dose of morphine following their second paracetamol dose and the remaining 16 subjects discontinued after the second dose of morphine. Of the 10 subjects who discontinued due to emesis after receiving their first dose of morphine, 8 had previously received two doses of oral paracetamol and 2 had received intravenous paracetamol doses.
4 Discussion
Overall, this study demonstrated a substantial impact on the pharmacokinetic profile of oral paracetamol, but not intravenous paracetamol, when co-administered with morphine. Greater pharmacokinetic variability was seen following administration of paracetamol orally compared to intravenously, particularly after subjects were exposed to morphine. This variability could be attributed multiple factors: (1) much of the inter-individual inherent physiologic variability could be contributing to higher variance in absorption, (2) the uptake of paracetamol from the small intestine is much faster than from the stomach due to the greater surface area. An important consequence was that the absorption would be determined by the rate at which the drug was transferred from the stomach to the site of rapid absorption in the upper small intestine, (3) absorption also involved the process of dissolution from an orally administered solid dosage form and either the rate of transit from stomach or dissolution could be rate-limiting. Heading and colleagues [18] found that rapid gastric emptying in 14 convalescent patients was associated with the early appearance of high peak plasma paracetamol concentrations, whereas peak concentrations were low and appeared late when gastric emptying was slow.
Observed peak paracetamol concentration (C max) and area under the plasma concentration-time curve over the 6-h dosing interval (AUC0–6) were reduced in this study when oral paracetamol was co-administered with morphine, followed by an abruptly increased C max and AUC0–6 upon the discontinuation of morphine, indicating the absorption of the accumulated paracetamol entering the small intestine after the effect of morphine dissipated. Noticeable changes were also observed for time to reach maximum drug concentration (T max) after the 3rd and 4th doses. Variability in C max, AUC0–6, C6 (paracetamol concentration before the following dosing time), as well as T max around 3rd dose was significantly higher than that of first two doses, indicating the impact of morphine on oral paracetamol absorption varies substantially among individual subjects. In contrast, intravenous paracetamol demonstrated more predictable pharmacokinetics in the setting of concomitant opioid use.
In this study, only two 0.125 mg/kg doses of morphine were given, whereas in clinical practice, patients may need more than two doses, which could have an even greater impact on gastric emptying and gut motility, resulting in greater accumulation of paracetamol following repeat oral dose administration. Once gastric function is restored upon the discontinuation of morphine, there is an abrupt release of unabsorbed paracetamol that enters the small intestine [19]. We observed a resultant approximate doubling in AUC (after the 4th dose of oral paracetamol), which may produce significant changes in paracetamol metabolism, as common pathways such as glucuronidation/sulfation get saturated and more drug is converted into the free radical metabolite N-acetyl-p-benzoquinone imine (NAPQI), which binds to and causes death of hepatocytes.
In general, the pharmacokinetic profile of paracetamol following oral administration is known to exhibit considerable inter-subject variability due to differences in normal physiologic factors such as gastrointestinal movement [18]. The plasma concentrations of paracetamol and its absorption are apparently related to the rate of gastric emptying since faster gastric emptying is associated with the rapid appearance of high peak plasma concentrations, while the peaks occur late and are lower in patients with delayed gastric emptying. Gastric emptying likely influences paracetamol absorption directly by controlling the rate at which the drug is delivered to the small intestine. Consistent with the high inter-subject variability in pharmacokinetic profiles seen in the current study in subjects who received oral paracetamol, individual variation in the rate of drug absorption may be due largely to differences in the rate of gastric emptying [18]. Furthermore, concomitant use of morphine in the current study introduced even greater variability in orally administered paracetamol exposures, plasma concentrations, and T max.
The interaction between morphine and orally administered paracetamol could be even more pronounced in postsurgical patients where factors such as concomitant medications and surgical trauma may further impair gastric function. This may result in inadequate pain control from orally administered paracetamol during opioid co-treatment and subsequent absorption of accumulated paracetamol upon cessation of opioid treatment.
The results from this study are consistent with the pharmacokinetic results of the study by Singla et al 2012 [14]. With respect to efficacy, plasma and CSF levels need to be considered, though it is difficult to correlate paracetamol CSF levels with efficacy, —i.e., paracetamol has a central effect but concentrations in CSF are not predictive of (i.e., linearly related to) efficacy [20]. This is a limitation of the study by Singla et al [14]. The “effect compartment” is unknown and could be multiple locations (e.g., brain and spinal cord) [21]. Paracetamol conversion to the active metabolite AM404 may result in active analgesia [22].
Low plasma concentrations following oral administration of paracetamol could impact efficacy relative to the intravenous route of administration. Plasma C max may be a better predictor of efficacy than AUC, in that the passive diffusion of paracetamol into the CNS is highly dependent on the concentration gradient across the blood brain barrier [14]. Post-operative intravenous paracetamol previously has been demonstrated to provide faster onset of analgesia than a similar dose given orally [23] and, more recently, that only two-thirds of patients given an oral dose of 1 g paracetamol preoperatively achieved therapeutic plasma concentrations at any point compared to 96% in those given an intravenous dose of 1 g preoperatively [24].
In the context of multimodal analgesia, when choosing medications to administer, increased efficacy, decreased adverse effects, and opioid reduction are the primary objectives [25]. Therefore, selection of non-opioids is imperative, and route of administration should be factored in, given opioid impact on gut motility, which impacts the pharmacokinetics of agents administered orally; substantial inter-subject variability could be the result of morphine’s effect, or first- pass metabolism, or both.
Results of this study suggest intravenous paracetamol is a better choice than oral paracetamol in patients receiving concomitant opioids until normal gut function can be demonstrated. A future study should evaluate the extent of the “burst effect” (i.e., the abrupt release of accumulated paracetamol at the end of morphine-mediated GI inhibition following oral administration), to evaluate both pharmacokinetics and safety (in particular, the impact on liver enzyme levels). The study should also aim to measure metabolites to determine the extent of NAPQI formation following the burst effect.
5 Conclusion
This study demonstrated that morphine co-administration significantly impacted the pharmacokinetics of oral paracetamol, but not intravenous paracetamol, by significantly reducing/delaying its absorption and substantially increasing the inter-individual pharmacokinetic variability. The abrupt release of the accumulated paracetamol at the end of morphine-mediated gastrointestinal inhibition following oral administration of paracetamol is a safety concern, particularly given that additional postsurgical patient factors may impact gastric function. Intravenous paracetamol thus provides a better option for the management of postoperative pain in the context of multimodal analgesia.
References
ASA Task Force on Acute Pain Management. Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology. 2012;116:248–73.
Pasero C. Opioid-induced sedation and respiratory depression: evidence-based monitoring guidelines. J Perianesth Nurs. 2012;27(3):208–11.
American Society of Anesthesiologists Task Force on Acute. Pain Management. Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology. 2004;100:1573–81.
Jarzyna D, Jungquist CR, Pasero C, et al. American Society of Pain Management Nursing guidelines on monitoring for opioid-induced sedation and respiratory depression. Pain Manag Nurs. 2011;12(3):118–45.
Wells N, Pasero C, McCaffery M. Improving the quality of care through pain assessment and management. In: Hughes RG, ed. Patient safety and quality: an evidence-based handbook for nurses. AHRQ Publication No. 08-0043. Rockville, MD: Agency for Healthcare Research and Quality; March 2008.
The American Geriatrics Society. Pain management in the elderly. http://www.americangeriatrics.org/gsr/anesthesiology/pain_management.pdf. Accessed 10 Sep 2014.
Barr JU, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41(1):263–306.
American Academy of Orthopaedic Surgeons. Management of hip fractures in the elderly: evidence-based clinical practice guideline. September 5, 2014. http://www.aaos.org/Research/guidelines/HipFxGuideline_rev.pdf. Accessed 23 Mar 2015.
Feldman LS, Delaney CP, Ljungqvist O, Carli F. The SAGES/ERAS® Society manual of enhanced recovery programs for gastrointestinal surgery. New York: Springer; 2015.
Jibril F, Sharaby S, Mohamed A, Wilby KJ. Intravenous versus oral acetaminophen for pain: systematic review of current evidence to support clinical decision-making. Can J Hosp Pharm. 2015;68(3):238–47.
Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. Pain. 2016;17(2):131–57.
Kennedy JM, Tyers NM, Davey AK. The influence of morphine on the absorption of paracetamol from various formulations in subjects in the supine position, as assessed by TDx measurement of salivary paracetamol concentrations. J Pharm Pharmacol. 2003;55(10):1345–50.
Sinatra RS, Jahr JS, Reynolds LW, Viscusi ER, Groudine SB, Payen-Champenois C. Efficacy and safety of single and repeated administration of 1-gram intravenous acetaminophen injection (paracetamol) for pain management after major orthopedic surgery. Anesthesiology. 2005;102(4):822–31.
Singla NK, Parulan C, Samson R, et al. Plasma and cerebrospinal fluid pharmacokinetic parameters after single-dose administration of intravenous, oral, or rectal acetaminophen. Pain Pract. 2012;12(7):523–32.
Ameer B, Divoll M, Abernethy DR, Greenblatt DJ, Shargel L. Absolute and relative bioavailability of oral acetaminophen preparations. J Pharm Sci. 1983;72(8):955–8.
Anderson BJ, Holford NHG, Woollard GA, Kanagasundaram S, Mahadevan M. Perioperative pharmacodynamics of acetaminophen analgesia in children. Anesthesiology. 1999;90(2):411–21.
Gelotte CK. Cross-study pharmacokinetic and pharmacodynamic modeling of acetaminophen: comparison of Tylenol® extended relief caplets with regular-strength Tylenol® caplets. Fort Washington, PA: McNeil Consumer & Specialty Pharmaceuticals; 1995. Submitted to NDA 19-872 as Phase IV Commitment. Cited in McNeil Consumer Healthcare, a Division of McNeil-PPC, Inc. (a Johnson & Johnson Company), 2002 Submission to the Non-Prescription Drug Advisory Committee.
Heading RC, Nimmo J, Prescott LF, Tothill P. The dependence of paracetamol absorption on the rate of gastric emptying. Br J Pharmacol. 1973;47:415–21.
Srinivas NR. Acetaminophen absorption kinetics in altered gastric emptying: establishing a relevant pharmacokinetic surrogate using published data. J Pain Palliat Care Pharmacother. 2015;29(2):115–9.
Anderson BJ, Holford NG, Woollard GA, Chan PS. Paracetamol plasma and cerebrospinal fluid pharmacokinetics in children. Br J Pharmacol. 1998;46(3):237–43.
Toussaint K, Yang XC, Zielinski MA, et al. What do we (not) know about how paracetamol (acetaminophen) works? J Clin Pharm Ther. 2010;35(6):617–38.
Mallet C, Barrière DA, Ermund A, et al. TRPV1 in brain is involved in acetaminophen-induced antinociception. PLoS One. 2010;5(9):e12748.
Møller PL, Sindet-Pedersen S, Petersen CT, Juhl GI, Dillenschneider A, Skoglund LA. Onset of acetaminophen analgesia: comparison of oral and intravenous routes after third molar surgery. Br J Anaesth. 2005;94(5):642–8.
van der Westhuizen J, Kuo PY, Reed PW, Holder K. Randomised controlled trial comparing oral and intravenous paracetamol (acetaminophen) plasma levels when given as preoperative analgesia. Anaesth Intensive Care. 2011;39:242–6.
Raffa RB, Clark-Vetri R, Tallarida RJ, Wertheimer AI. Combination strategies for pain management. Expert Opin Pharmacother. 2003;4(10):1697–708.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Mallinckrodt Pharmaceuticals. These data were presented in part at the 15th Annual Pain Medicine Meeting of the American Society of Regional Anesthesia and Pain Medicine (ASRA), November 17–19, 2016, San Deigo, California.
Author contribution
Michael G. Baker, PhD of Samorn Biosciences, Inc., provided assistance with writing/formatting/proof reading collation of the author comments and this assistance was funded by Mallinckrodt Pharmaceuticals.
Conflict of interest
Robert B. Raffa is a former employee of Johnson & Johnson (1986–1996); he has received basic science laboratory analgesics research funding from pharmaceutical companies; he consults/presents on analgesics for several pharmaceutical companies, including Mallinckrodt, but he receives no royalties for sales of any products. Jayne Pawasauskas is a consultant to Mallinckrodt Pharmaceuticals Inc., Joseph V Pergolizzi Jr. is a consultant/ speaker and/or researcher for: Inspirion, Mallinckrodt, Collegium, Purdue Pharma LLP, Grunenthal GmhB, Inspirion, ENDO Pharmaceuticals Iroko, DepoMed and Mundipharma. Krishna Devarakonda, Jia Lu, Yin Chen, Sutan Wu, Lawrence Hill, Brant Jarrett, and Randi Fain are employees of Mallinckrodt Pharmaceuticals Inc.
Ethical approval
Prior to initiation of this single-center study, the protocol was reviewed and approved by the institutional review board IntegReview, Austin, Texas. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study. Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Raffa, R.B., Pawasauskas, J., Pergolizzi, J.V. et al. Pharmacokinetics of Oral and Intravenous Paracetamol (Acetaminophen) When Co-Administered with Intravenous Morphine in Healthy Adult Subjects. Clin Drug Investig 38, 259–268 (2018). https://doi.org/10.1007/s40261-017-0610-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-017-0610-4