Abstract
Background and Objective
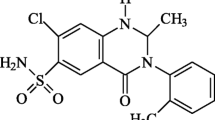
The pharmacokinetics of lurasidone have been studied in healthy Japanese and Caucasian subjects, but not in Chinese subjects. The objective of this study was to evaluate the pharmacokinetics, safety, and tolerability of oral lurasidone in healthy Chinese subjects.
Methods
This single-center, randomized, parallel-group, placebo-controlled, and double-blind study evaluated the pharmacokinetics, safety, and tolerability of oral lurasidone administered as a single dose (20, 40, and 80 mg) and multiple doses for 5 days (40 mg administered once daily) in healthy Chinese subjects. Serum lurasidone and its metabolites were quantified using high-performance liquid chromatography–mass spectrometry. Pharmacokinetic parameters for lurasidone and its metabolites were calculated using non-compartmental analysis of WinNonlin® version 6.2. Safety analyses were recorded using physical examinations, vital signs, electrocardiogram, and clinical laboratory tests.
Results
Serum concentrations of lurasidone reached maximum concentration (C max) within 1.0–3.0 h after each single dose, and then decreased biphasically, with a mean half-life (t ½) from 18.1 to 25.5 h over the dose range of 20–80 mg. The area under the concentration–time curve (AUC) and C max values increased approximately dose proportionally. Lurasidone steady state was achieved after 5 days of daily dosing and the accumulation index of the AUC during a dosage interval (AUCτ) was 1.25, smaller than theoretical cumulative coefficient (1.76). Similar results were observed for the metabolites (ID-14283, ID-14326, and ID-11614). No severe adverse events (AEs) were observed in the single- or multiple-dose studies and no subject discontinued from the study due to AEs. The most common reported AEs were somnolence, increased blood prolactin, and restlessness, with a higher rate as dose increased.
Conclusion
Lurasidone was safe and well-tolerated in healthy Chinese subjects, following single doses in the range of 20 to 80 mg and multiple doses of 40 mg/day for 5 days. Linear increase in lurasidone C max and AUC values were seen following single doses from 20 to 80 mg. There was no unexpected accumulation after multiple administrations of lurasidone at 40 mg/day, and the pharmacokinetic characteristics were consistent with the conclusion obtained in the previous studies.
Trial Registration: Clinicaltrials.gov identifiers NCT02174510 and NCT02174523.




Similar content being viewed by others
References
Schizophrenia facts and statistics. http://www.schizophrenia.com/szfacts.htm. Accessed 10 June 2017.
Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209–23.
Van Os J, Kapur S. Schizophrenia. Lancet. 2009;374(9690):635–45.
Citrome L. Asenapine for schizophrenia and bipolar disorder: a review of the efficacy and safety profile for this newly approved sublingually absorbed second-generation antipsychotic. Int J Clin Pract. 2009;63(12):1762–84.
Correll CU, Schenk EM. Tardive dyskinesia and new antipsychotics. Curr Opin Psychiatry. 2008;21(2):151–6.
Duggan L, Fenton M, Dardennes RM, El-Dosoky A, Indran S. Olanzapine for schizophrenia. Cochrane Database Syst Rev. 2000;(2):CD001359. doi:10.1002/14651858.CD001359.
Ishibashi T, Horisawa T, Tokuda K, Ishiyama T, Ogasa M, Tagashira R, et al. Pharmacological profile of lurasidone, a novel antipsychotic agent with potent 5-hydroxytryptamine 7 (5-HT7) and 5-HT1A receptor activity. J Pharmacol Exp Ther. 2010;334(1):171–81.
Latuda [package insert]. Marlborough: Sunovion Pharmaceuticals; 2013. http://www.latuda.com/LatudaPrescribingInformation.pdf. Accessed 14 Aug 2016.
Preskorn S, Ereshefsky L, Chiu YY, Poola N, Loebel A. Effect of food on the pharmacokinetics of lurasidone results of two randomized, open-label, crossover studies. Hum Psychopharmacol. 2013;28(5):495–505.
Citrome L. Lurasidone in schizophrenia: new information about dosage and place in therapy. Adv Ther. 2012;29(10):815–25.
Meyer JM, Loebel AD, Schweizer E. Lurasidone: a new drug in development for schizophrenia. Expert Opin Investig Drugs. 2009;18(11):1715–26.
Samalin L, Garnier M, Llorca PM. Clinical potential of lurasidone in the management of schizophrenia. Ther Clin Risk Manag. 2011;7:239–50.
Franklin R, Zorowitz S, Corse AK, Widge AS, Deckersbach T. Lurasidone for the treatment of bipolar depression: an evidence-based review. Neuropsychiatr Dis Treat. 2015;11:2143–52.
Citrome L. Lurasidone for schizophrenia: a review of the efficacy and safety profile for this newly approved second-generation antipsychotic. Int J Clin Pract. 2011;65(2):189–210.
Food and Drug Administration. Drug approval package. Latuda (lurasidone hydrochloride) tablets. Sunovion Pharmaceuticals, Inc. Clinical Review; Pharmacology Review(s); Clinical Pharmacology Biopharmaceutics Review(s). http://www.accessdata.fda.gov/drugsatfda_docs/nda/2010/200603Orig1s000PharmR.pdf. Accessed 10 June 2017.
European Medicines Agency. Latuda (lurasidone). http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/002713/human_med_001737.jsp&mid=WC0b01ac058001d124. Accessed 10 June 2017.
Acknowledgements
The authors would like to thank all of the subjects for their participation in this study; Yun Liu, Yanmei Liu, and Qian Chen for their contribution to this study as sub-investigators; Ye Liu, Xiaoyan Xu, Tingting Li, and Yating Wang for their contribution as nurses; and Tao Jia as the study monitor. The authors would like to thank Hao Xu for statistics assistance and Wenyan Tang for pharmacokinetic methodology preparation and sample analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The study was sponsored by Sumitomo Pharma (Suzhou) Co., Ltd. The writing of this article was completed without any external funding.
Conflict of interest
Xiaoyan Luo is an employee of Sumitomo. Chaoying Hu, Yijun Wang, Rong Song, Chen Yu, and Jingying Jia report no conflicts of interest regarding the content of this article in the last 36 months.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hu, C., Wang, Y., Song, R. et al. Single- and Multiple-Dose Pharmacokinetics, Safety and Tolerability of Lurasidone in Healthy Chinese Subjects. Clin Drug Investig 37, 861–871 (2017). https://doi.org/10.1007/s40261-017-0546-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-017-0546-8