Abstract
Background and Objective
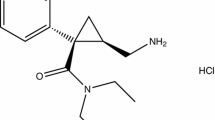
Dexmecamylamine (TC-5214) is a nicotinic channel modulator that was evaluated as a potential adjunct treatment to an antidepressant for patients with major depressive disorder. Dexmecamylamine is almost completely eliminated via the kidneys, with more than 90 % of a given dose excreted unchanged in urine. The aim of this study was to assess the single-dose pharmacokinetics of dexmecamylamine in subjects with various degrees of renal impairment and subjects undergoing hemodialysis.
Methods
A single-dose, open-label, parallel-group study was conducted at two study centers in the USA. There were four treatment groups with eight subjects in each, receiving a single dose of dexmecamylamine 8 mg (subjects with normal renal function and mild renal impairment) or TC-5412 2 mg [subjects with moderate renal impairment and end-stage renal disease (ESRD)]. The pharmacokinetics of dexmecamylamine in plasma, urine, and dialysate were evaluated using non-compartmental analysis.
Results
The plasma pharmacokinetics of dexmecamylamine were influenced by renal function. The increase in dose–normalized area under the plasma concentration–time curve (AUC) was statistically significant with an approximately doubled exposure in subjects with moderate renal impairment compared with subjects with normal renal function. The maximum plasma concentration was not impacted by renal function. Plasma clearance of dexmecamylamine in ESRD subjects appeared negligible, with flat plasma concentration–time profiles. Hemodialysis had a relatively modest effect on reduction of dexmecamylamine plasma concentrations. There was no discernable relationship between renal clearance and urinary pH.
Conclusion
Renal impairment increased the AUC, prolonged the elimination half-life, and decreased the clearance of dexmecamylamine following administration as a single oral dose. It is likely that renal function would need to be taken into account when setting the dose. Dexmecamylamine administration should be avoided or the dose significantly reduced in patients with severe renal impairment and ESRD.




Similar content being viewed by others
References
Targacept. AstraZeneca. (Data on file).
Freis ED, Wilson IM. Mecamylamine, a new, orally effective, hypotensive agent; experimental and clinical evaluation. AMA Arch Intern Med. 1956;97:551–61.
Dunbar G, Hosford D. The potential of the nicotinic channel blocker TC-5214 as augmentation treatment in patients with major depression. Eur Neuropsychopharmacol. 2010;20:S334.
Allanby KD, Trounce JR. Excretion of mecamylamine after intravenous and oral administration. Br Med J. 1957;2:1219–21.
Milne MD, Scribner BH, Crawford MA. Non-ionic diffusion and the excretion of weak acids and bases. Am J Med. 1958;24:709–29.
National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 2002;39(2 Suppl. 1):S1–266.
Posner K, Oquendo M, Stanley B, et al. Suicidality Classification Project. http://www.fda.gov/ohrms/dockets/ac/04/slides/2004-4065S1_06_FDA-Posner.ppt. Accessed 23 May 2013.
Srivastava T, Kainer G. Collection under paraffin is not necessary for stability of urine pH over 24 h. Pediatr Nephrol. 2004;19:169–71.
Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41.
Acknowledgments
The authors wish to thank Cecilia Hedlund for guidance and review of the statistical section of this manuscript. The authors thank Juliet West, on behalf of Complete Medical Communications, who provided editing support funded by AstraZeneca.
This study was sponsored by AstraZeneca and Targacept. The study was conducted by AstraZeneca. The authors were involved in study design, analysis, and interpretation of the data, and in preparation of the manuscript. Sofie Alverlind, Stéphane Barassin, Per Dalén, and Hans Eriksson were employees of AstraZeneca at the time the research was conducted. Yan Li and Raj Tummala are employees of AstraZeneca. Steven Toler is an employee of Targacept.
Author information
Authors and Affiliations
Corresponding author
Additional information
ClinicalTrials.gov identifier: NCT01240967; AstraZeneca study code: D4130C00008.
Rights and permissions
About this article
Cite this article
Alverlind, S., Barassin, S., Dalén, P. et al. Clinical Pharmacokinetics of the Nicotinic Channel Modulator Dexmecamylamine (TC-5214) in Subjects with Various Degrees of Renal Impairment. Clin Drug Investig 34, 457–465 (2014). https://doi.org/10.1007/s40261-014-0195-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-014-0195-0