Abstract
Background
Though biologic agents have significantly improved the treatment of inflammatory arthritis (rheumatoid arthritis, psoriatic arthritis, and axial spondyloarthritis), high costs, stringent regulations, strict reimbursement criteria, and existing patents have limited patient access to treatments. While being highly similar in quality, safety, and efficacy to biologic reference products, biosimilars can reduce the financial burden and prevent underutilization of medication.
Objective
The objective of this initiative was to develop an evidence-based consensus of overarching principles and recommendations aimed at standardizing the use of biosimilars in treating inflammatory arthritis in the Gulf region.
Methods
A task force of practicing rheumatologists, a clinical pharmacist, a health economist, patients, regulators, and payors from across the Gulf region developed recommendations and overarching principles based on the outputs of a systematic literature review conducted to address Patient-Intervention-Comparison-Outcome (PICO) questions specific to key challenges regarding the use of biosimilars for the treatment of inflammatory arthritis in the region. As the data before 2017 have been previously reviewed in another publication, the current review focused on data published between January 2017 and August 2022 (PROSPERO ID CRD42022364002). Consensus on each statement required a level of agreement of 70% or greater.
Results
Consensus was reached for five overarching principles and nine recommendations by the task force. The principles emphasize the importance of improving the awareness, understanding, and perception of biosimilars, as well as the need for regulated regional real-world data generation and protocols to make biosimilars a viable and affordable treatment option for all patients. The consensus recommendations advocate the need for shared treatment decisions between rheumatologists and patients when considering biosimilars. They further recommend that confirmation of a biosimilar’s efficacy and safety in a single indication is sufficient for extrapolation to other diseases for which the reference product has been approved. Finally, there is a need for pharmacovigilance and national health policies governing the adoption and prescription of biosimilars in clinical practice across the region.
Conclusions
These are the first consensus recommendations for the Gulf region based on a systematic literature review and Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) guidelines, integrating clinical evidence with clinical expertise to optimize decision making for the use of biosimilars in patients with inflammatory arthritis. They were formulated based on predominantly international data because of the limited regional data and therefore can be generalized to serve as recommendations for healthcare professionals in other parts of the world.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Competition by biosimilars can reduce the financial burden on healthcare and prevent the underutilization of medication while still being safe and effective in managing inflammatory rheumatic diseases. |
The adoption of biosimilars in the Gulf region is low because of the limited availability of regional guidelines, knowledge gaps among rheumatologists and other healthcare providers, and a dearth of regional literature on biosimilars. |
Our consensus provides insights to guide evidence-based clinical practice regarding the prescription of biosimilars for patients with inflammatory rheumatic diseases. |
The paper emphasizes the need for future educational and research initiatives, as well as the need for regional real-world registries, national policies, and pharmacovigilance to guide the broader adoption of these more cost-effective therapeutic alternatives for managing inflammatory rheumatic diseases. |
1 Introduction
Inflammatory rheumatic diseases are a group of complex and chronic musculoskeletal conditions, including rheumatoid arthritis (RA) and spondyloarthritis (SpA), that impact joints and other organs [1]. The global annual incidence rate of RA is 3 in every 10,000 people with a prevalence rate of 1% [2]. In 2019, the age-adjusted prevalence of RA was reported to be 0.16% in Bahrain, 0.12% in Kuwait, 0.11% in Qatar, and 0.10% each in Oman, the Kingdom of Saudi Arabia (KSA), and the United Arab Emirates (UAE) [3]. Comprehensive studies discussing the epidemiology of RA specifically in the region are limited [4]. Spondyloarthritis includes axial SpA (AxSpA) and psoriatic arthritis (PsA) that cause chronic back pain and musculoskeletal manifestations [5,6,7]. The prevalence of PsA has been reported to be 0.01% in the Middle East and North Africa [8]. The global prevalence of AxSpA has been estimated to be 0.3–1.4% [9], with a prevalence of 0.11% in the Middle East [10]. However, the true epidemiology of inflammatory rheumatic diseases needs to be better evaluated in the Gulf region by improving the reporting of diseases and establishing data and patient registries [4].
Disease-modifying antirheumatic drugs (DMARDs) are immunosuppressive and immunomodulatory drugs for the treatment of rheumatic diseases, including RA, PsA, and AxSpA [11]. Biologic DMARDs target specific immune mechanisms and are typically prescribed in patients who do not respond to conventional DMARDs such as methotrexate, leflunomide, hydroxychloroquine, sulfasalazine, and cyclosporine. Biologic DMARDs have significantly improved disease management and patient outcomes over the years [12]. It has been reported that fewer than 2% of patients with RA in the Middle East and North Africa region are treated with biologics compared with 40% in the USA [13]. The low prescription volumes of biologic originators for the management of rheumatic diseases in some Arab countries can be attributed to high treatment costs [13] and limited availability associated with expensive manufacturing processes, complex and stringent regulatory processes, and strict reimbursement criteria, thereby limiting treatment access to patients. Furthermore, the access to biologic drugs for residents in the Gulf countries may vary owing to the presence of diverse insurance plans. This has driven the need for the development of more affordable yet biologically similar alternatives for the treatment of rheumatic diseases.
Biosimilars are drugs that are highly similar to reference products in terms of physiochemical properties, quality, safety, and efficacy profiles [13, 14]. Biosimilars do not have a similar patent protection as the reference products [15], thereby limiting the market exclusivity of biosimilars. By promoting competition in a multi-source market [16, 17], they can reduce the financial burden on healthcare, and prevent the underutilization of medication while still being safe and effective in managing rheumatic disease [12, 14, 17,18,19]. The US Food and Drug Administration (FDA) describes a biosimilar as a biological product that is highly similar to and has no clinically meaningful differences from an existing FDA-approved reference product in terms of the safety, purity, and potency [20]. According to the European Medicines Agency (EMA), a biosimilar is a biological drug containing the active substance of an approved originator biologic to which similarity has been demonstrated following a thorough comparison of the two products [21]. The regulatory approval of biosimilars is based on the evaluation of pharmaceutical quality, safety, and efficacy that generally apply to all reference products. It is crucial for policymakers responsible for the approval and regulation of biosimilars to understand the distinctions between generic small molecules and biosimilars. The Gulf Cooperation Council (GCC) comprises six countries: Bahrain, KSA, Kuwait, Oman, Qatar, and the UAE, with a population of more than 54 million people [22, 23]. However, because of the heterogeneity of biosimilar regulatory approval processes in the Gulf, the availability of biosimilars varies significantly across the region (Table 1) [13]. Although the GCC Central Committee for Drug Registration oversees drug evaluation, registration, and post-marketing surveillance across the GCC [23], local authorities within the local markets in individual countries vary. For example, the Saudi Food and Drug Authority and the UAE regulatory authorities adapted their guidance from the FDA and EMA, with adaptations to the local and GCC requirements [13, 23, 24]. However, the availability of biosimilars depends on regulations by local markets and authorities’ regulations. Biosimilars in national markets are required to adhere to the country’s standards and guidance.
Despite various biosimilars being approved for use by the FDA, EMA, and other regulatory bodies, the general uptake of biosimilars across the world is relatively low [25,26,27]. The task force noted a similar trend in clinical practice in the Gulf region, which could be attributed to the following reasons. First, regional guidelines or recommendations regarding the use of biosimilars are limited. Second, existing gaps in knowledge and understanding of biosimilars may lead to a reluctance among rheumatologists to prescribe biosimilars and a negative perception of biosimilars among patients [20, 28]. Third, the greater number of published studies on reference drugs compared with biosimilars may diminish the confidence of prescribers on the latter. Furthermore, rheumatologists are likely to feel more comfortable when prescribing reference drugs, which are more widely available in the Gulf region than biosimilars. Fourth, numerous payors in the Gulf adopt a neutral stance regarding whether rheumatologists opt to prescribe reference medications or biosimilars. Last, the lack of efficient post-marketing pharmacovigilance on efficacy and safety has also negatively impacted the optimal utilization of biosimilars.
Global consensus-based recommendations and position papers on the use of biosimilars for the treatment of rheumatic disease have been previously published [12, 29,30,31]. Currently, specific pathways and recommendations for the use of biosimilars in rheumatic disease are available in some Gulf countries [32, 33]. However, regional guidelines and recommendations focused on standardizing the adoption and prescription of biosimilars for the treatment of rheumatic diseases in the Gulf region are either limited or unavailable. Therefore, a multidisciplinary task force of regional experts was formed in order to develop evidence-based principles and recommendations based on the outputs of a comprehensive systematic literature review (SLR) that aimed to standardize and drive alignment on best practices for the use of biosimilars in treating adult patients with rheumatic diseases, particularly RA and SpA (PsA and AxSpA).
2 Methods
2.1 Participants
A multidisciplinary task force of regional experts from Bahrain, KSA, Kuwait, Oman, Qatar, and the UAE, comprising seven expert rheumatologists, a healthcare economist, and a clinical pharmacist, as well as an external non-voting rheumatology advisor (TKK) from Norway, was formed. The members of the taskforce were identified from regional societal groups based on their expertise in the field, as well as their knowledge and interest in biosimilars, and were invited by the convenor (KAA) to participate in the development of the Gulf consensus overarching principles and recommendations. All task force members have at least 20 years of clinical practice. Additionally, a group of external validators comprising three patients, two payors, two regulators, and 13 practicing rheumatologists with experience in biosimilars from across the Gulf region was also identified by the taskforce.
2.2 PICO Questions and Systematic Literature Review
Sixteen specific Patient-Intervention-Comparison-Outcome (PICO) questions that addressed key topics and challenges concerning the use of biosimilars for the treatment of rheumatic diseases among patients in the Gulf region were formulated in order to guide an SLR. These questions were related to the comparability to reference products in terms of efficacy, safety, immunogenicity, and cost savings; extrapolation of indications; switching or transitioning patients from a reference product or to another approved biosimilar; retention rates; physician awareness; and prescription practices (Table 1 of the Electronic Supplementary Material [ESM]).
The SLR was conducted using PubMed and Cochrane databases (supplemented with Google Scholar) with the aim to identify, select, and critically appraise the quality of the overall body of evidence that demonstrated the value proposition of biosimilars in rheumatic disease. This was performed using defined eligibility criteria to include meta-analyses, clinical trials, and systematic reviews of adult patients aged 18 years or older with RA, PsA, and AxSpA who had received biosimilars at some point during their course of treatment. The search strategy is defined in Table 2 of the ESM. Publications that did not meet the eligibility criteria, including studies in healthy subjects and patients with other inflammatory conditions, were excluded from the SLR. As the data on outcomes of an SLR on the use of biosimilars prior to 2017 have already been reviewed in another publication, [12] the current review focused on data that was published between January 2017 and August 2022. The systematic review was registered on the International Prospective Register of Systematic Reviews (PROSPERO; registration ID CRD42022364002).
2.3 Development of the Overarching Principles and Recommendations
The expert task force reviewed the summary of evidence obtained from the SLR, based on which, overarching principles and consensus recommendations were developed. The recommendations were largely congruent with previously published guidelines, with adaptation for regional clinical practice and consideration of the nuances of the healthcare systems within the Gulf region. The task force critically reviewed the principles and recommendations to assess the quality of evidence and strength of recommendations. Voting for the level of agreement of the expert task force on the overarching principles and consensus statements was conducted anonymously through an online voting system. This was performed using a 5-point Likert scale (1, strongly agree; 5, strongly disagree) requiring a level of agreement (strongly agree or agree) of 70% or more among the expert task force members in order to reach a consensus on each of the statements. The external validators subsequently reviewed and validated the overarching principles and recommendations through a separate anonymous online survey requiring a level of agreement (strongly agree or agree) of 70% or greater to reach a consensus on each statement (Table 3 of the ESM).
3 Results
3.1 Systematic Literature Review
The search yielded 1111 results, which included meta-analyses, clinical trials, and systematic reviews published between January 2017 and August 2022 (Fig. 1). After screening by publication type, relevance, and duplicates, 1004 records were excluded, and a total of 107 relevant publications were incorporated in the summary of evidence. All methods were fully reported following the recommended Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA 2020) guidance [34].
3.2 Expert Consensus
After reviewing the results of the SLR, the expert task force convened to develop the overarching principles and recommendations, and live edits were made to align on the statements during the meeting. Based on outcomes of the SLR and expert opinions, particularly when there was no published evidence, five overarching principles and nine consensus recommendations were developed (Table 2). The expert task force reached a consensus on all the overarching principles and recommendations with a level of agreement greater than 70% in the first round of voting. The external validators validated each of the statements with a level of agreement that was greater than 80% (Table 2 of the ESM). The average level of agreement on the overarching principles and consensus recommendations between the expert task force and external validators was 96.4%.
4 Overarching Principles and Consensus Recommendations
The level of evidence and the grade of recommendations were evaluated based on the 2014 European Alliance of Associations for Rheumatology (EULAR) standard operating procedures [35].
4.1 Overarching Principles
-
A.
Rheumatologists, patients, and other stakeholders can benefit from awareness campaigns that educate and update them on the nature, approval processes, safety, and efficacy of biosimilars in comparison to reference products.
It is critical that rheumatologists, patients, and other stakeholders be made aware of the rigorous evaluation and approval processes of biosimilars in order to understand the similarities and differences in the nature, safety, and efficacy in comparison to reference products [20, 36]. Targeted awareness campaigns and educational initiatives aimed at healthcare professionals and the public can be used to regularly convey information and updates on biosimilars in order to strengthen the familiarity, augment the understanding, and promote the acceptance of biosimilars as safe and effective treatment options for rheumatic disease [25, 37]. Awareness campaigns have been sporadically carried out in the Gulf region, primarily instigated by pharmaceutical companies, with occasional involvement from health organizations like Abu Dhabi Health Services Company (SEHA) in the UAE and other non-profit rheumatological societies. Raising awareness about the benefits of biosimilars among various stakeholders besides rheumatologists and patients, such as regulatory bodies, healthcare administrators, pharmacists, policymakers, and those in charge of coverage decisions in the private and public sectors, is vital to facilitate the development of standardized policies for the adoption, prescription, and reimbursement of biosimilars. In the Gulf region, the number of biosimilar conferences has been on the rise, with the 2023 International Biosimilars Congress held in Dubai serving as a notable example, where rheumatologists, gastroenterologists, hematologists, dermatologists, oncologists, pharmacists, and charitable organizations were invited as speakers.
-
B.
A better understanding of biosimilars can help rheumatologists communicate the benefits of biosimilars more efficiently with patients, thereby reinforcing positive perceptions towards biosimilars and improving adherence.
A reluctance to prescribe biosimilars among clinicians in the Middle East has been observed as a result of a limited understanding of biosimilars and a lack of confidence in its efficacy and safety [13, 20]. Furthermore, some surveys found that pharmacists lacked adequate information about biosimilars in order to advise patients appropriately [38, 39]. Moreover, negative perceptions towards biosimilars can occur among patients because of the misconception that the lower cost of biosimilars is associated with inferior quality and poorer outcomes compared with reference products [40]. This can potentially lead to the development of nocebo effects among patients, resulting in increased non-adherence to biosimilars [13, 36, 40]. The negative perceptions and unrealistic expectations of patients towards newer therapies or changes to current therapy subsequently lead to poorer outcomes or failure of therapy [37, 41].
The approval of biosimilars is based on the totality of the evidence that demonstrates a high degree of similarity with the reference product following a rigorous comparative testing process [13, 26, 42]. Therefore, rheumatologists must understand the available evidence in order to confidently counsel patients regarding biosimilars as a viable and more affordable treatment option for rheumatic diseases [12]. This will enforce positive patient perceptions towards biosimilars and mitigate the impact of nocebo effects. The needs, perspectives, apprehensions, misconceptions, and expectations of patients must be considered and discussed during treatment planning.
-
C.
Rheumatic disease treatment decisions should be made collaboratively by the patient and their rheumatologists (shared decision making) and must be based on available clinical evidence and local healthcare regulatory guidelines/recommendations.
Shared decision making empowers patients to take control of their health and has been shown to improve patient satisfaction [12, 36, 37, 41]. Rheumatologists are obligated to provide patients with the necessary information that can improve the patient’s understanding of the disease, available treatment options, and the risks and benefits of each, including biosimilars [12]. This can create a positive perception towards biosimilars, thereby enabling patients to make informed decisions regarding their treatment preferences and goals, ultimately resulting in increased acceptance of biosimilars, better adherence to prescriptions, and improved treatment outcomes [31, 36, 37, 41, 43].
-
D.
Standardized protocols for collecting real-world data on both biosimilars and reference products must be established across the region.
The approval processes for biosimilars mandate a high level of similarity in the physiochemical characterization and clinical outcomes to that of reference products [12, 13, 42]. Although biosimilars are expected to remain highly comparable to their reference products over time, it is critical to gather real-world post-marketing efficacy and safety data in order to track clinical outcomes [12, 31, 44]. This is a common post-marketing requirement for all drugs, including biosimilars [12, 26, 45], and is particularly important in the Gulf region because of the dearth of regional real-world data, which can be useful in generating evidence demonstrating their comparability to reference products [45]. In the regional and local settings, this may be valuable in instilling confidence in biosimilars among clinicians.
-
E.
Biosimilars must be made available to all patients at significantly lower acquisition costs in order to widen access to treatment by providing more affordable treatment options.
Given the high degree of comparability in the efficacy and safety of biosimilars and reference products, cost can become a major determinant when selecting one treatment option over the other [12, 17]. Biosimilars have been shown to be lower cost alternatives to reference products, with an estimated treatment cost saving between 44 and 69% compared with reference products [17, 46]. For instance, a study reported that patients taking the infliximab biosimilar paid 12% less than the reference product [17, 47].The lower market price of biosimilars can potentially result in a significantly higher absolute cost saving compared with reference products [48]. In Europe, the cumulative savings resulting from biosimilar competition has been estimated to have surpassed €30 billion in 2022, which can be attributed to price reductions in the markets [16]. Additionally, the lower prices of a biosimilar could lead to a competitive domino effect in price reductions for other biosimilars [17, 49]. This can be observed in counties like Denmark and Norway that follow a tender system for controlling drug prices [17]. This is likely to widen the access to affordable treatment options for all patients. Switching patients with RA from infliximab to its biosimilar in the UK, France, and Germany was estimated to generate savings between 20% and 30% over 5 years, which could facilitate the treatment of over 7500 additional patients with RA with biosimilars [17, 50]. However, despite an increase in access to biosimilars, there is a disparity in their uptake across Europe [16].
4.2 Consensus Recommendations
Recommendation 1. Biosimilars are comparable to their respective reference products in terms of efficacy, safety, and immunogenicity profiles and can be considered a treatment alternative.
As mentioned earlier, the comparative pharmacokinetic, pharmacodynamic, efficacy, safety, and immunogenicity data are stringently reviewed and approved by regulatory agencies [12,13,14]. Since the approval of the first biosimilar in 2006, evidence from both clinical studies and real-world experience have validated the comparability between biosimilars and reference products and have shown no significant differences in physiochemical properties and post-translational modifications or impurities [12, 14, 51,52,53]. Therefore, approved biosimilars can be utilized as a more affordable treatment alternative to their respective reference products [12, 26, 36]. However, it is important that factors such as the need and preferences of the patient and access to the biosimilar be taken into account when considering treatment with biosimilars [26].
Recommendation 2. The formation of antidrug antibodies is not significantly different between biosimilars and reference products and therefore does not need to be routinely measured in clinical practice.
Monoclonal antibodies induce an immune response in some patients by triggering the production of antidrug antibodies, which may result in lowered trough drug concentrations and subsequently, decreased efficacy in some patients [12]. Neutralizing antibodies are typically detected within 6 months of exposure to a biologic agent and can negate drug efficacy. Over the past 17 years since the first approval of a biosimilar, studies have demonstrated no clinically significant differences in the formation of antibodies between biosimilars and reference products [14, 53, 54]. Therefore, antidrug antibodies to biosimilars do not need to be routinely measured in clinical practice [12].
Recommendation 3. Rheumatologists must be well informed about the safety, efficacy, and immunogenicity profiles of biosimilars to effectively explain treatment options to patients. This knowledge will help mitigate challenges related to retention rates, nocebo effects, and patient misconceptions regarding biosimilars.
Despite the rigorous clinical studies demonstrating the comparability of biosimilars and reference products, higher drug discontinuation rates have been observed among patients who were switched from reference products to biosimilars in clinical studies [41, 55]. The poorer retention rates because of adverse events that could not be attributed to the treatment’s effects have raised suspicions of potential nocebo effects [41, 56]. This can lead to intentional non-adherence and result in poorer treatment outcomes among patients taking biosimilars [55]. Studies have demonstrated significant improvements in retention rates of biosimilars when structured communication strategies were used, resulting in comparable discontinuation rates among patients taking biosimilars and reference products [41, 57]. Therefore, it is necessary for rheumatologists, pharmacists, nurses, and other allied healthcare professionals who interact with patients to be well informed about the various aspects of biosimilars in order to be an effective resource of information to patients [41, 58]. All relevant stakeholders, including healthcare personnel such as rheumatologists, pharmacists, and nurses, should be trained to ensure a standardized and unified approach to patient communication regarding biosimilars [43, 59]. This ‘One Voice’ approach can help clarify patient queries regarding biosimilars, clarify misconceptions and misinformation in a coherent and univocal manner, and as a result, reduce the occurrence of nocebo effects and improve retention rates among patients. Such a strategy has been associated with higher acceptance rates and better treatment outcomes with biosimilars among patients [43, 55]. It is important to note that patient characteristics such as age, level of education, perceived hypersensitivity to drugs, and the level of trust on the rheumatologist and the medication can influence the patient’s perceptions [40].
Recommendation 4. Switching/transitioning from a reference product to an approved biosimilar should be considered in clinical practice due to the comparable efficacy, immunogenicity, and long-term safety outcomes.
Non-medical switching is the changing of the medication of a stable patient from a reference drug to another clinically similar medication for reasons other than clinical ineffectiveness, tolerability, or adherence [20, 56, 60]. Non-medical switching is commonly associated with drug availability, formulary changes, or costs [56, 60]. However, because of limited regional guidelines on switching patients from a reference product to its biosimilar, clinicians in the Middle East are reluctant to initiate such a switch/transition [20, 28]. Furthermore, the lack of patient studies and the fear of occurrence of hypersensitivity reactions are the biggest concerns that impede the prescription of biosimilars [13]. Therefore, the decision to switch/transition patients from a reference product to an approved biosimilar must be based on evidence. Comparative randomized controlled trials have demonstrated the comparable efficacy, immunogenicity, and long-term safety of biosimilars and reference products [12, 18, 61,62,63,64]. Therefore, switching to a biosimilar is not expected to result in a different clinical outcome as compared to remaining on reference products [12, 63,64,65], while improving patient access to treatment and generating cost savings that could support the sustainability of the healthcare system [17, 50].
Recommendation 5. Switching/transitioning between approved biosimilars of the same reference product can be considered in clinical practice due to the comparable efficacy and safety outcomes.
Though switching from a reference product to a biosimilar has been explored in randomized controlled trials, switching between different approved biosimilars of the same reference product has not, owing to the high cost and complexity of additional clinical trials [12, 63]. Systematic reviews of evidence reported that switching from an infliximab, adalimumab, or etanercept biosimilar to another biosimilar of the same reference product was safe and effective in terms of disease activity, remission rate, loss of response, adverse events, and immunogenicity in patients with chronic inflammatory diseases [63, 66].
Recommendation 6. Confirmation of the efficacy and safety of a biosimilar in a single indication is sufficient for the extrapolation to other diseases for which the reference product has been approved.
Given the evidence confirming the similarity of biosimilars to their respective reference products on the basis of rigorous pre-approval evaluations, regulatory agencies permit the extrapolation of the efficacy and safety of biosimilars from one approved indication to others for which the reference product has been approved based on a single, successful, phase III, randomized controlled trial [12, 27]. Such extrapolation of indications may be approved even if the biosimilar has not been evaluated in the other indications if the reference product has the same mechanism of action in all of the other indications. Clinical decisions are generally based on robust clinical evidence, and biosimilars have always demonstrated comparable efficacy and safety to that of their reference products when used to treat extrapolated indications [12]. Therefore, confirmation of the efficacy and safety of a biosimilar in a single sensitive indication is sufficient to treat approved indications in which it has not been comparatively evaluated with its reference products [67, 68]. The sensitive indication should be one that can detect any clinically relevant differences in safety, immunogenicity, and efficacy [69]. This can potentially lower the costs, resources, and time needed for additional clinical studies for each indication [70], thereby leading to potential cost reductions and expedited approvals of biosimilars, ultimately resulting in improved patient access to medications. Approval of biosimilars by GCC regulatory bodies must be expedited and streamlined after assessing the evidence of their quality, efficacy, and safety [45].
Recommendation 7. Switching from a reference product to a biosimilar in stable patients should be a shared decision between patients and rheumatologists. Patients should be informed about the comparable efficacy, safety, and cost-saving benefits of biosimilars.
Shared decision making is a fundamental principle of patient-centric care where well-informed patients actively participate in the selection of the most appropriate treatment option [12, 71]. The reluctance among patients to accept the switch from a reference product to a biosimilar has been attributed to a lack of awareness and negative perceptions and misconceptions regarding biosimilars [36, 40, 55]. Uninformed switching to biosimilars by treating physicians has been reported as a cause of concern among patients. Therapeutic decisions to switch a stable patient from a reference product to a biosimilar must be made transparently and collaboratively following informed discussions with patients in order to promote their autonomy in the process [12, 55]. Rheumatologists must consider the patient’s preferences, perspectives, and expectations and avoid negatively influencing discussions [12, 40, 41].
Recommendation 8. Standardized pharmacovigilance initiatives must be established across the region to document post-marketing data and compare the outcomes of biosimilars and their reference products.
Biologics have the intrinsic potential to induce an immune response that may impact the safety and efficacy of the drug [72]. This may be influenced by product characteristics, treatment-related factors, patient-related factors, or disease-related factors. Biologics have intrinsic natural variability, which can result in variations between batches of the same product [73]. The regulatory approval of biosimilars differs from that of reference products, and although similar to each other, biosimilars can never be identical to reference products because of differences in the origin of the cell lines, as well as the complex manufacturing processes that may impact the translational and post-translation modifications and contaminants, biological activity, intrinsic heterogeneity, and stability [27, 74, 75]. Although comparability studies have demonstrated no differences in quality and impurities following a newer manufacturing process [72, 76], regulatory bodies are concerned about the potential of biosimilars to induce an immunogenic response.
The FDA, EMA, and World Health Organization recommend that national regulatory bodies develop stringent pharmacovigilance frameworks and appropriate naming systems for biosimilars [13, 31]. In this context, the task force recommended providing unique proprietary names and drug codes for biosimilars and reference products within the Gulf countries. This can improve the traceability of biosimilars to specific brands and batches that are associated with specific adverse events. This is important as post-translational modifications may occur during the manufacturing process of each batch that could potentially modify the immunogenicity of the drug [31, 42]. Although pharmacovigilance systems have been established in some Gulf countries, such as Kuwait, Oman, Qatar, KSA, and the UAE, they are either underutilized or not standardized for biosimilars [77, 78]. Local pharmacovigilance and post-marketing surveillance data can provide crucial insights that contribute towards the development of standardized national and regional health policies for the use of biosimilars [13, 77, 78]. In this context, it is important for rheumatologists to regularly report efficacy, safety, and immunogenicity data associated with their use. Additionally, these initiatives can contribute to the totality of available evidence [12].
Recommendation 9. National health policies should be developed to adopt prescribing biosimilars.
As of June 2023, the European Union had 93 approved biosimilars (17 withdrawn after receiving approval) and the USA had 40 approved biosimilars [79, 80]. However, the global adoption of biosimilars into healthcare formularies and clinical practice has been relatively low [16, 27, 81]. Concerns about safety, efficacy, and immunogenicity, particularly during indication extrapolation, have limited the prescription and acceptance of biosimilars by rheumatologists and patients, respectively, who are key stakeholders in fostering the uptake of biosimilars [13, 55, 82]. Regulatory approval processes for biosimilars differ across Gulf countries, wherein some follow the FDA approval guidance while others follow either EMA or World Health Organization guidance [13, 78]. Adoption of international guidelines for biosimilars into the Gulf health policies and guidelines necessitates careful consideration of the region's unique healthcare landscape and patient needs [21]. The national health policies for the use of biosimilars must promote evidence-based decision making and must be developed in collaboration with various stakeholders, including rheumatologists, pharmacists, policymakers, health advocates, payors, and healthcare administration [83]. However, it is important to note that Gulf countries have varying economies and healthcare infrastructures and policies [42]. Experts were of the opinion that a transparent streamlined biosimilar formulary and pricing process that incentivized rheumatologists, reduced cost sharing for patients, and increased reimbursement of biosimilars could drive an uptake in the prescription and use of biosimilars [81].
5 Discussion
To our knowledge, these Gulf consensus-based overarching principles and recommendations on the use of biosimilars in inflammatory rheumatic diseases are the fourth in the literature, and the first in the Arab world, that have been developed using a robust methodology. Though they are largely congruent with previously published recommendations and position papers [12, 13, 31], these principles and recommendations have been adapted to the regional clinical and healthcare context within the Gulf region. The statements were also externally validated by patients, regulators, payors, and practicing rheumatologists across the region.
Although early access to biologics for rheumatic disease is more common in high-income Gulf countries compared with many other countries, owing to financial support from the government, a few challenges remain for those residents without exclusive insurance plans, which may lead to some delays in treatment [28, 45, 84]. The availability of biosimilars allows for more affordable treatment options and improved quality of care for a larger number of patients with rheumatic disease in the Gulf region [42, 82]. It has been reported that most rheumatologists prefer reference products in the first-line setting, while biosimilars are used by a small proportion of clinicians in the second-line and third-line settings, particularly in patients who had not previously been treated with reference products [25]. Understanding the comparability of biosimilars to reference products, the approval process, and long-term financial benefits of biosimilars will not only encourage biosimilar prescription and use in the clinical setting, but will also encourage the system-wide adoption of biosimilars into national and regional healthcare formulary and reimbursement frameworks [37, 58]. Stakeholders at all levels, including physicians, healthcare systems, pharmacists, payors, policymakers, manufacturers, and patients, must be included in planning such strategies.
The adoption of biosimilars has been restricted by gaps in knowledge and awareness among rheumatologists and negative perceptions among patients [58]. Targeted educational initiatives must be developed to disseminate information across different stakeholder groups. The nocebo phenomenon can occur among patients as a result of a previous negative experience during intervention, negative expectations or perceptions, or misinformation, which can lead to decreased biosimilar acceptance and medication adherence [41, 55, 56, 58]. Patients must be educated on the benefits of biosimilars as well as any nocebo effects. Switching to biosimilars must be a shared decision between rheumatologists and patients based on informed discussions about evidence and clinical experience. Shared decision making encourages patients to collaborate and participate in treatment decisions. The decision to switch to a biosimilar must be tailored to the specific needs of each patient. The automatic substitution of biosimilars by pharmacists is highly discouraged, and prescribing decisions should be made by the rheumatologist with the consent of the patient.
Biosimilars are more affordable alternatives for the treatment of rheumatic diseases that may provide indirect economic benefits [58]. The average prices of both biosimilars and patented biologics have been observed to be decreasing across markets because of competition among manufacturers, thereby significantly improving patient access. This can also create conditions for competitiveness between reference products and biosimilars, where a subsequent reduction in the price of the biological originator is likely to occur [16, 17, 45, 49]. Switching from a reference product to a biosimilar is typically due to insurance mandates, implementation of pharmacy formulary changes to reduce costs, or because the patient has relocated to a region where the current prescription is not available [56, 60, 63]. Strategies for lowering patient treatment costs and the financial burden on the healthcare system while maintaining quality of care should be developed [58]. However, the decision to prescribe a biosimilar should not be based solely on cost; the patient’s needs must also be considered [12, 21]. Based on the rising healthcare expenditure, gross domestic product, and the increasing demand for more affordable and cost-effective treatment options, the Middle East market for biosimilars is expected to grow by 24.96% (compound annual growth rate) between 2021 and 2026 [42]. With the expected increase in the adoption of biosimilars in the region, regulated approval protocols, pharmacovigilance, and post-marketing surveillance must be developed/improved in the region [13]. However, the regulatory pathways for biosimilars have yet to be established in some Middle Eastern countries, and clear guidelines for switching from a reference product to a biosimilar are lacking in the region.
The task force recognized the lack of regional data from clinical trials, real-world experience, pharmacovigilance, and post-marketing surveillance regarding the use of biosimilars for the treatment of patients with rheumatic disease in the Gulf region. Furthermore, various challenges regarding patient perspectives, patient education and awareness, and the management of the nocebo effect among patients were identified. On the basis of these findings, a future research agenda was proposed (Table 3).
Our consensus-based overarching principles and recommendations were developed by a multidisciplinary task force of regional experts using a robust methodology and have been specifically tailored to the context of the regional clinical and healthcare landscape within the Gulf region. Furthermore, these statements were validated by a group of external validators comprising patients, payors, regulators, and practicing rheumatologists. The overarching principles and recommendations serve as a clinical guide to physicians and rheumatologists across the region to standardize the adoption and prescription of biosimilars for the treatment of patients with rheumatic disease. Additionally, this paper highlights the major gaps and challenges that limit the optimal utilization of biosimilars in clinical practice and pave the way for further research. Our SLR included PubMed and Cochrane databases, supplemented with Google Scholar. Data from other databases, such as Embase, were not employed in our analysis. Last, the SLR was conducted between January 2017 and August 2022 since the outcomes of an SLR on the use of biosimilars prior to 2017 have already been reviewed in another publication [12].
6 Conclusions
A robust body of clinical evidence shows that the adoption of biosimilars can provide high-quality and affordable treatment to a greater number of patients with rheumatic disease than is currently possible without increasing the financial burden on the healthcare system [12, 58]. The proposed overarching principles and consensus recommendations are the first regional consensus recommendations for the Gulf region based on an SLR and PRISMA guidelines, integrating clinical evidence with clinical expertise to optimize decision making for the use of biosimilars in patients with rheumatic diseases. Though these principles and recommendations are intended to raise awareness on best practices for the use of biosimilars in the treatment of adult patients with rheumatic disease in the region, they also provide a framework for future educational and research initiatives in the Gulf region. While the overarching principles and consensus recommendations were developed specifically for the Gulf region, they were predominantly based on international data because of the lack of robust regional data. These statements offer a transferrable framework that can be adapted to serve as a clinical reference for healthcare professionals beyond the Gulf region, thereby facilitating the effective adoption of biosimilars for the treatment of rheumatic disease in patients worldwide. This can be particularly valuable in regions that are unfamiliar with biosimilars or are relatively new to the concept of biosimilars. These guidelines can also prove beneficial for patients, offering biosimilars as an affordable alternative, when access to biologics is limited because of the associated costs. Furthermore, the agenda for future research mirrors key gaps and challenges pertaining to the adoption of biosimilars that are also common to many other parts of the world.
References
National Academies of Sciences Engineering and Medicine, Health and Medicine Division, Board on Health Care Services. Selected health conditions and likelihood of improvement with treatment. 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559512/. Accessed 17 Jan 2024.
Prasad P, Verma S, Surbhi, Ganguly NK, Chaturvedi V, Mittal SA. Rheumatoid arthritis: advances in treatment strategies. Mol Cell Biochem. 2023;478(1):69–88. https://doi.org/10.1007/s11010-022-04492-3.
Alzahrani H, Alshehri MA, Alotaibi M, Alhowimel A, Alodaibi F, Alamam D, et al. Burden of musculoskeletal disorders in the Gulf Cooperation Council countries, 1990–2019: findings from the Global Burden of Disease study 2019. Front Med (Lausanne). 2022;9: 855414. https://doi.org/10.3389/fmed.2022.855414.
Mousavi SE, Nejadghaderi SA, Khabbazi A, Alizadeh M, Sullman MJM, Kaufman JS, et al. The burden of rheumatoid arthritis in the Middle East and North Africa region, 1990–2019. Sci Rep. 2022;12(1):19297. https://doi.org/10.1038/s41598-022-22310-0.
Benavent D, Capelusnik D, van der Heijde D, Landewe R, Poddubnyy D, van Tubergen A, et al. How is early spondyloarthritis defined in the literature? Results from a systematic review. Semin Arthritis Rheum. 2022;55: 152032. https://doi.org/10.1016/j.semarthrit.2022.152032.
Bedaiwi MK, AlRasheed RF, Bin Zuair A, Alqurtas EM, Baeshen MO, Omair MA. A cross-sectional study on clinical characteristics of Saudi axial spondylarthritis: preliminary results. Eur Rev Med Pharmacol Sci. 2021;25(16):5241–7. https://doi.org/10.26355/eurrev_202108_26538.
Quraishi MK, Badsha H, Khan B, Shahzeb M, Hegde S, Mofti A, et al. Interethnic variations and clinical features of spondyloarthropathies in a Middle Eastern country. Open Rheumatol J. 2018;12:10–8. https://doi.org/10.2174/1874312901812010010.
Bedaiwi M, Al-Homood IA, El-Garf A, Uthman I, Sunna N, Nassier R, et al. Disease burden and treatment challenges of psoriatic arthritis in Africa and the Middle East. Rheumatol Int. 2019;39(8):1321–9. https://doi.org/10.1007/s00296-019-04319-3.
Poddubnyy D, Sieper J, Akar S, Munoz-Fernandez S, Haibel H, Hojnik M, et al. Characteristics of patients with axial spondyloarthritis by geographic regions: PROOF multicountry observational study baseline results. Rheumatology (Oxford). 2022;61(8):3299–308. https://doi.org/10.1093/rheumatology/keab901.
El Zorkany B, Ali YM, Namas R, Bedaiwi M, Husain W, Ahmed HM, et al. The treatment journey for patients with axial spondyloarthritis in North Africa and the Middle East: from diagnosis to management. Int J Rheum Dis. 2020;23(11):1574–80. https://doi.org/10.1111/1756-185X.13961.
Benjamin O, Goyal A, Lappin SL. Disease-modifying antirheumatic drugs (DMARD). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507863/.
Kay J, Schoels MM, Dorner T, Emery P, Kvien TK, Smolen JS, et al. Consensus-based recommendations for the use of biosimilars to treat rheumatological diseases. Ann Rheum Dis. 2018;77(2):165–74. https://doi.org/10.1136/annrheumdis-2017-211937.
El Zorkany B, Al Ani N, Al Emadi S, Al Saleh J, Uthman I, El Dershaby Y, et al. Biosimilars in rheumatology: recommendations for regulation and use in Middle Eastern countries. Clin Rheumatol. 2018;37(5):1143–52. https://doi.org/10.1007/s10067-018-3982-9.
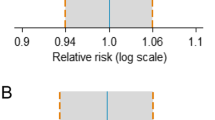
Ascef BO, Almeida MO, Medeiros-Ribeiro AC, Oliveira de Andrade DC, Oliveira Junior HA, de Soarez PC. Therapeutic equivalence of biosimilar and reference biologic drugs in rheumatoid arthritis: a systematic review and meta-analysis. JAMA Netw Open. 2023;6(5): e2315872. https://doi.org/10.1001/jamanetworkopen.2023.15872.
Moorkens E, Vulto AG, Huys I. An overview of patents on therapeutic monoclonal antibodies in Europe: are they a hurdle to biosimilar market entry? MAbs. 2020;12(1):1743517. https://doi.org/10.1080/19420862.2020.1743517.
Troin P, Newton M, Stoddart K, Arias A. The impact of biosimilar competition in Europe. IQVIA; 2022. Available from: https://www.iqvia.com/-/media/iqvia/pdfs/library/white-papers/the-impact-of-biosimilar-competition-in-europe-2022.pdf. Accessed 17 Jan 2024.
Kvien TK, Patel K, Strand V. The cost savings of biosimilars can help increase patient access and lift the financial burden of health care systems. Semin Arthritis Rheum. 2022;52: 151939. https://doi.org/10.1016/j.semarthrit.2021.11.009.
Tanaka E, Kawahito Y, Kohno M, Hirata S, Kishimoto M, Kaneko Y, et al. Systematic review and meta-analysis of biosimilar for the treatment of rheumatoid arthritis informing the 2020 update of the Japan College of Rheumatology clinical practice guidelines for the management of rheumatoid arthritis. Mod Rheumatol. 2022;32(1):74–86. https://doi.org/10.1080/14397595.2021.1899591.
Carrascosa JM, Jacobs I, Petersel D, Strohal R. Biosimilar drugs for psoriasis: principles, present, and near future. Dermatol Ther (Heidelb). 2018;8(2):173–94. https://doi.org/10.1007/s13555-018-0230-9.
Mysler E, Omair MA, Zayed M, Al Balushi F, Al Saleh J, Al Wahshi H, et al. Perception toward biosimilars and nonmedical switching: a cross-sectional survey among Arab rheumatologists. Dr Sulaiman Al Habib Med J. 2020;2(4):179–85. https://doi.org/10.2991/dsahmj.k.200727.001.
Halabi H, Al Zahrani Z, Al Swailem R, Husain W, Al Rayes H, Al Osaimi H, et al. Biosimilars in rheumatic diseases: regulatory guidelines, efficacy and safety implications in Saudi Arabia. Open Rheumatol J. 2018;12(1):313–22. https://doi.org/10.2174/1874312901812010313.
Al-Hazzaa HM. Physical Activity research in the gulf cooperation council countries: progress made but work still to do. J Phys Act Health. 2022;19(11):769–70. https://doi.org/10.1123/jpah.2022-0484.
Niazi SK. A proposed Global Medicines Agency (GMA) to make biological drugs accessible: starting with the League of Arab States. Healthcare. 2023;11(14):2075. https://doi.org/10.3390/healthcare11142075.
Laslop A, Wang J, Thorpe R. 2nd MENA stakeholder meeting on biosimilars 2018: report. GaBI J. 2019;8:76–87. https://doi.org/10.5639/gabij.2019.0802.009.
Leonard E, Wascovich M, Oskouei S, Gurz P, Carpenter D. Factors affecting health care provider knowledge and acceptance of biosimilar medicines: a systematic review. J Manag Care Spec Pharm. 2019;25(1):102–12. https://doi.org/10.18553/jmcp.2019.25.1.102.
Smeeding J, Malone DC, Ramchandani M, Stolshek B, Green L, Schneider P. Biosimilars: considerations for payers. P T. 2019;44(2):54–63.
Omair MA, Alhawassi T, Alwaihibi M, Aldrees G, Mosli M, Asser WM, et al. Improving the understanding of originator and biosimilar biologics among healthcare providers in Saudi Arabia. Saudi Pharm J. 2020;28(12):1827–9. https://doi.org/10.1016/j.jsps.2020.11.008.
Farhat F, Othman A, El Karak F, Kattan J. Review and results of a survey about biosimilars prescription and challenges in the Middle East and North Africa region. Springerplus. 2016;5(1):2113. https://doi.org/10.1186/s40064-016-3779-8.
Fonseca JE, Goncalves J, Araujo F, Cordeiro I, Teixeira F, Canhao H, et al. The Portuguese Society of Rheumatology position paper on the use of biosimilars. Acta Reumatol Port. 2014;39(1):60–71.
Araujo FC, Sepriano A, Teixeira F, Jesus D, Rocha TM, Martins P, et al. The Portuguese Society of Rheumatology position paper on the use of biosimilars: 2017 update. Acta Reumatol Port. 2017;42(3):219–28.
Kowalski SC, Benavides JA, Roa PAB, Galarza-Maldonado C, Caballero-Uribe CV, Soriano ER, et al. PANLAR consensus statement on biosimilars. Clin Rheumatol. 2019;38(5):1485–96. https://doi.org/10.1007/s10067-019-04496-3.
Hegde M. Unlocking the promising opportunities of biosimilars in the Middle East and Africa Market. Iqvia; 2023. Available from: https://www.iqvia.com/locations/middle-east-and-africa/blogs/2023/06/unlocking-the-promising-opportunities-of-biosimilars-in-the-middle-east-and-africa-market. Accessed 17 Jan 2024.
BIOMAPAS. Biosimilars in the MENA region: Regulatory landscape. 2023. Available from: https://www.biomapas.com/biosimilars-mena-regulatory-affairs/. Accessed 17 Jan 2024.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71. https://doi.org/10.1136/bmj.n71.
van der Heijde D, Aletaha D, Carmona L, Edwards CJ, Kvien TK, Kouloumas M, et al. 2014 Update of the EULAR standardised operating procedures for EULAR-endorsed recommendations. Ann Rheum Dis. 2015;74(1):8–13. https://doi.org/10.1136/annrheumdis-2014-206350.
Ismailov R, Simoens S, Khasanova Z. Greater awareness of biosimilars and shared decision-making among patients attending rheumatology practices in Colorado, United States: real-world data. World J Rheumatol. 2020;10(1):1–10. https://doi.org/10.5499/wjr.v10.i1.1.
Mazzoni D, Vener C, Mazzocco K, Monzani D, Pravettoni G. The psychological risks associated with the non-medical switch from biologics to biosimilars. Front Psychol. 2021;12: 605643. https://doi.org/10.3389/fpsyg.2021.605643.
Beck M, Michel B, Rybarczyk-Vigouret MC, Leveque D, Sordet C, Sibilia J, et al. Knowledge, behaviors and practices of community and hospital pharmacists towards biosimilar medicines: results of a French web-based survey. MAbs. 2017;9(2):383–90. https://doi.org/10.1080/19420862.2016.1267087.
Oqal M, Hijazi B, Alqudah A, Al-Smadi A, Almomani BA, Alnajjar R, et al. Awareness and knowledge of pharmacists toward biosimilar medicines: a survey in Jordan. Int J Clin Pract. 2022;2022:8080308. https://doi.org/10.1155/2022/8080308.
Gasteiger C, Lobo M, Dalbeth N, Petrie KJ. Patients’ beliefs and behaviours are associated with perceptions of safety and concerns in a hypothetical biosimilar switch. Rheumatol Int. 2021;41(1):163–71. https://doi.org/10.1007/s00296-020-04576-7.
Petit J, Antignac M, Poilverd RM, Baratto R, Darthout S, Desouches S, et al. Multidisciplinary team intervention to reduce the nocebo effect when switching from the originator infliximab to a biosimilar. RMD Open. 2021;7(1): e001396. https://doi.org/10.1136/rmdopen-2020-001396.
Batran RA, Elmoshneb M, Hussein AS, Hussien OM, Adel F, Elgarhy R, et al. Biosimilars: science, implications, and potential outlooks in the Middle East and Africa. Biologics. 2022;16:161–71. https://doi.org/10.2147/BTT.S376959.
Vandenplas Y, Simoens S, Van Wilder P, Vulto AG, Huys I. Informing patients about biosimilar medicines: the role of European patient associations. Pharmaceuticals. 2021;14(2):117. https://doi.org/10.3390/ph14020117.
Singh A, Kalaivani M, Srivastava S, Goyal RK, Gupta SK. Postmarketing safety of biosimilars: current status, challenges, and opportunities in the spontaneous reporting system. Ther Innov Regul Sci. 2020;54(3):667–80. https://doi.org/10.1007/s43441-019-00101-6.
Alnaqbi KA, Bellanger A, Brill A, Castaneda-Hernandez G, Clopes Estela A, Delgado Sanchez O, et al. An international comparative analysis and roadmap to sustainable biosimilar markets. Front Pharmacol. 2023;14:1188368. https://doi.org/10.3389/fphar.2023.1188368.
García-Goñi M, Río-Álvarez I, Carcedo D, Villacampa A. Budget impact analysis of biosimilar products in Spain in the period 2009–2019. Pharmaceuticals (Basel). 2021;14(4):348. https://doi.org/10.3390/ph14040348.
ERIC (The Erisa Industry Committee). Biosimilars at 10 years. 2020. Available from: https://www.eric.org/wp-content/uploads/2020/03/FINAL-ERICBiosimilarsAtTenYearsInfographic.pdf. Accessed 17 Jan 2024.
Tesar T, Golias P, Kobliskova Z, Wawruch M, Kawalec P, Inotai A. Potential cost-savings from the use of the biosimilars in Slovakia. Front Public Health. 2020;8:431. https://doi.org/10.3389/fpubh.2020.00431.
Barszczewska O, Piechota A. The impact of introducing successive biosimilars on changes in prices of adalimumab, infliximab, and trastuzumab: Polish experiences. Int J Environ Res Public Health. 2021;18(13):6952. https://doi.org/10.3390/ijerph18136952.
Thomas D, Vibeke S, Paul C, João G, László G, Jonathan K, et al. The changing landscape of biosimilars in rheumatology. Ann Rheum Dis. 2016;75(6):974. https://doi.org/10.1136/annrheumdis-2016-209166.
Bae SC, Lee YH. Comparative efficacy and safety of biosimilar adalimumab and originator adalimumab in combination with methotrexate in patients with active rheumatoid arthritis: a Bayesian network meta-analysis of randomized controlled trials. Clin Rheumatol. 2018;37(5):1199–205. https://doi.org/10.1007/s10067-018-4002-9.
Bae SC, Lee YH. Comparative efficacy and safety of biosimilar rituximab and originator rituximab in combination with methotrexate in patients with active rheumatoid arthritis: a Bayesian network meta-analysis. Int J Clin Pharmacol Ther. 2019;57(4):188–96. https://doi.org/10.5414/CP203360.
Kurki P, Barry S, Bourges I, Tsantili P, Wolff-Holz E. Safety, immunogenicity and interchangeability of biosimilar monoclonal antibodies and fusion proteins: a regulatory perspective. Drugs. 2021;81(16):1881–96. https://doi.org/10.1007/s40265-021-01601-2.
Niazi SK. Biosimilars: harmonizing the approval guidelines. Biologics. 2022;2(3):171–95. https://doi.org/10.3390/biologics2030014.
Colloca L, Panaccione R, Murphy TK. The clinical implications of nocebo effects for biosimilar therapy. Front Pharmacol. 2019;10:1372. https://doi.org/10.3389/fphar.2019.01372.
Fleischmann R, Jairath V, Mysler E, Nicholls D, Declerck P. Nonmedical switching from originators to biosimilars: does the nocebo effect explain treatment failures and adverse events in rheumatology and gastroenterology? Rheumatol Ther. 2020;7(1):35–64. https://doi.org/10.1007/s40744-019-00190-7.
Tweehuysen L, Huiskes VJB, van den Bemt BJF, Vriezekolk JE, Teerenstra S, van den Hoogen FHJ, et al. Open-label, non-mandatory transitioning from originator etanercept to biosimilar SB4: six-month results from a controlled cohort study. Arthritis Rheumatol. 2018;70(9):1408–18. https://doi.org/10.1002/art.40516.
Cross RK, Stewart AL, Edgerton CC, Shah B, Welz JA, Kay J. Implementation strategies of biosimilars in healthcare systems: the path forward. Am Health Drug Benefits. 2022;15(2):45–53.
Kristensen LE, Alten R, Puig L, Philipp S, Kvien TK, Mangues MA, et al. Non-pharmacological effects in switching medication: the nocebo effect in switching from originator to biosimilar agent. BioDrugs. 2018;32(5):397–404. https://doi.org/10.1007/s40259-018-0306-1.
Weeda ER, Nguyen E, Martin S, Ingham M, Sobieraj DM, Bookhart BK, et al. The impact of non-medical switching among ambulatory patients: an updated systematic literature review. J Mark Access Health Policy. 2019;7(1):1678563. https://doi.org/10.1080/20016689.2019.1678563.
Jorgensen KK, Olsen IC, Goll GL, Lorentzen M, Bolstad N, Haavardsholm EA, et al. Switching from originator infliximab to biosimilar CT-P13 compared with maintained treatment with originator infliximab (NOR-SWITCH): a 52-week, randomised, double-blind, non-inferiority trial. Lancet. 2017;389(10086):2304–16. https://doi.org/10.1016/S0140-6736(17)30068-5.
Goll GL, Jorgensen KK, Sexton J, Olsen IC, Bolstad N, Haavardsholm EA, et al. Long-term efficacy and safety of biosimilar infliximab (CT-P13) after switching from originator infliximab: open-label extension of the NOR-SWITCH trial. J Intern Med. 2019;285(6):653–69. https://doi.org/10.1111/joim.12880.
Cohen HP, Hachaichi S, Bodenmueller W, Kvien TK, Danese S, Blauvelt A. Switching from one biosimilar to another biosimilar of the same reference biologic: a systematic review of studies. BioDrugs. 2022;36(5):625–37. https://doi.org/10.1007/s40259-022-00546-6.
Barbier L, Ebbers HC, Declerck P, Simoens S, Vulto AG, Huys I. The efficacy, safety, and immunogenicity of switching between reference biopharmaceuticals and biosimilars: a systematic review. Clin Pharmacol Ther. 2020;108(4):734–55. https://doi.org/10.1002/cpt.1836.
Herndon TM, Ausin C, Brahme NN, Schrieber SJ, Luo M, Andrada FC, et al. Safety outcomes when switching between biosimilars and reference biologics: a systematic review and meta-analysis. PLoS ONE. 2023;18(10): e0292231. https://doi.org/10.1371/journal.pone.0292231.
Allocati E, Godman B, Gobbi M, Garattini S, Banzi R. Switching among biosimilars: a review of clinical evidence. Front Pharmacol. 2022;13: 917814. https://doi.org/10.3389/fphar.2022.917814.
European Medicines Agency. Information guide for healthcare professionals. 2017. Available from: https://www.ema.europa.eu/en/documents/leaflet/biosimilars-eu-information-guide-healthcare-professionals_en.pdf. Accessed 17 Jan 2024.
Krendyukov A, Schiestl M. Extrapolation concept at work with biosimilar: a decade of experience in oncology. ESMO Open. 2018;3(2): e000319. https://doi.org/10.1136/esmoopen-2017-000319.
European Medicines Agency. Guideline on similar biological medicinal products containing biotechnology-derived proteins as active substance: non-clinical and clinical issues. 2014. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2015/01/WC500180219.pdf. Accessed 17 Jan 2024.
Zalcberg J. Biosimilars are coming: ready or not. Intern Med J. 2018;48(9):1027–34. https://doi.org/10.1111/imj.14033.
Alameddine M, AlGurg R, Otaki F, Alsheikh-Ali AA. Physicians’ perspective on shared decision-making in Dubai: a cross-sectional study. Hum Resour Health. 2020;18(1):33. https://doi.org/10.1186/s12960-020-00475-x.
European Medicines Agency, European Commission. Biosimilars in the EU. 2017. Available from: https://www.ema.europa.eu/en/documents/leaflet/biosimilars-eu-information-guide-healthcare-professionals_en.pdf. Accessed 17 Jan 2024.
Windisch J. Biosimilars versus original biologics: similarities and differences from development to approval. Z Rheumatol. 2015;74(8):672–81. https://doi.org/10.1007/s00393-014-1486-9.
Kirchhoff CF, Wang XM, Conlon HD, Anderson S, Ryan AM, Bose A. Biosimilars: key regulatory considerations and similarity assessment tools. Biotechnol Bioeng. 2017;114(12):2696–705. https://doi.org/10.1002/bit.26438.
Kim H, Alten R, Avedano L, Dignass A, Gomollon F, Greveson K, et al. The future of biosimilars: maximizing benefits across immune-mediated inflammatory diseases. Drugs. 2020;80(2):99–113. https://doi.org/10.1007/s40265-020-01256-5.
Kurki P, van Aerts L, Wolff-Holz E, Giezen T, Skibeli V, Weise M. Interchangeability of biosimilars: a European perspective. BioDrugs. 2017;31(2):83–91. https://doi.org/10.1007/s40259-017-0210-0.
Alshammari TM, Mendi N, Alenzi KA, Alsowaida Y. Pharmacovigilance systems in Arab countries: overview of 22 Arab countries. Drug Saf. 2019;42(7):849–68. https://doi.org/10.1007/s40264-019-00807-4.
Jassim NA, Humadi YA. The use of biosimilars in the middle east: review article. Curr Rheumatol Rep. 2018;20(7):45. https://doi.org/10.1007/s11926-018-0740-6.
GaBI Online - Generics and Biosimilars Initiative. Biosimilars approved in Europe. 2023 [updated 12 May 2023].Available from: https://gabionline.net/biosimilars/general/biosimilars-approved-in-europe. Accessed 17 Jan 2024.
GaBI Online - Generics and Biosimilars Initiative. Biosimilars approved in the US. 2023 [updated 19 May 2023]. Available from: https://www.gabionline.net/biosimilars/general/biosimilars-approved-in-the-us]. Accessed 17 Jan 2024.
Edgar BS, Cheifetz AS, Helfgott SM, Smith GP, Bandekar T, Hoye-Simek A, et al. Overcoming barriers to biosimilar adoption: real-world perspectives from a national payer and provider initiative. J Manag Care Spec Pharm. 2021;27(8):1129–35. https://doi.org/10.18553/jmcp.2021.27.8.1129.
Rathore AS, Stevenson JG, Chhabra H, Maharana C. The global landscape on interchangeability of biosimilars. Expert Opin Biol Ther. 2022;22(2):133–48. https://doi.org/10.1080/14712598.2021.1889511.
Malekinejad M, Horvath H, Snyder H, Brindis CD. The discordance between evidence and health policy in the United States: the science of translational research and the critical role of diverse stakeholders. Health Res Policy Syst. 2018;16(1):81. https://doi.org/10.1186/s12961-018-0336-7.
Al-Herz A, Saleh K, Al-Awadhi A, Al-Kandari W, Hasan E, Ghanem A, et al. Accessibility to biologics and its impact on disease activity and quality of life in patients with rheumatoid arthritis in Kuwait. Clin Rheumatol. 2021;40(5):1759–65. https://doi.org/10.1007/s10067-020-05444-2.
Acknowledgments
Medical writing support was provided by Eric Mario, Connect Communications, Dubai, UAE. We are grateful to Dr. Lina Wahba (Clinical Pharmacist, Department of Oncology/Hematology at Tawam Hospital, Al Ain, UAE) for her insights into the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
Relevant data and materials are provided as supplementary information.
Code Availability
Not applicable.
Conflicts of Interest/Competing Interests
Samar Al Emadi reported consulting service fees from AbbVie, Pfizer, and Johnson & Johnson. Amin El Shamy reported research grants and consulting service fees from AbbVie, AstraZeneca, Viatris, and Janssen. Mohammed A. Omair reported consulting service fees from AbbVie, Pfizer, Amgen, Roche, Janssen, Hikma, Sandoz, Novartis, and BMS. Tore K. Kvien reported fees for speaking and/or consulting from AbbVie, Amgen, Celltrion, Egis, Evapharma, Ewopharma, Gilead, Hikma, Janssen, Mylan, Novartis, Oktal, Pfizer, Sandoz, and UCB; and research funding to Diakonhjemmet Hospital from AbbVie, Amgen, BMS, MSD, Novartis, Pfizer, and UCB. Khalid A. Alnaqbi, Nasra Al Adhoubi, Sara Aldallal, Adeeba Al-Herz, Suad Hannawi, and Sahar A. Saad have no conflicts of interest that are directly relevant to the content of this article.
Funding
This work was funded by an unrestricted educational grant from Sandoz to the Emirates Health Economics Society (non-profit organization).
Authors’ Contributions
All authors contributed towards the conception and design of the manuscript and were involved in the analysis and interpretation of the data and in the development of the recommendations. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Alnaqbi, K.A., Al Adhoubi, N., Aldallal, S. et al. Consensus-Based Overarching Principles and Recommendations on the Use of Biosimilars in the Treatment of Inflammatory Arthritis in the Gulf Region. BioDrugs 38, 449–463 (2024). https://doi.org/10.1007/s40259-023-00642-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40259-023-00642-1