Abstract
Objective
Previous studies showed that offering BRCA mutation testing to population subgroups at high risk of harbouring the mutation may be cost effective, yet no evidence is available for low- or middle-income countries (LMIC) and in Asia. We estimated the cost effectiveness of BRCA mutation testing in early-stage breast cancer patients with high pre-test probability of harbouring the mutation in Malaysia, an LMIC in Asia.
Methods
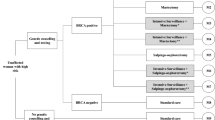
We developed a decision analytic model to estimate the lifetime costs and quality-adjusted life-years (QALYs) accrued through BRCA mutation testing or routine clinical surveillance (RCS) for a hypothetical cohort of 1000 early-stage breast cancer patients aged 40 years. In the model, patients would decide whether to accept testing and to undertake risk-reducing mastectomy, oophorectomy, tamoxifen, combinations or neither. We calculated the incremental cost-effectiveness ratio (ICER) from the health system perspective. A series of sensitivity analyses were performed.
Results
In the base case, testing generated 11.2 QALYs over the lifetime and cost US$4815 per patient whereas RCS generated 11.1 QALYs and cost US$4574 per patient. The ICER of US$2725/QALY was below the cost-effective thresholds. The ICER was sensitive to the discounting of cost, cost of BRCA mutation testing and utility of being risk-free, but the ICERs remained below the thresholds. Probabilistic sensitivity analysis showed that at a threshold of US$9500/QALY, 99.9% of simulations favoured BRCA mutation testing over RCS.
Conclusions
Offering BRCA mutation testing to early-stage breast cancer patients identified using a locally-validated risk-assessment tool may be cost effective compared to RCS in Malaysia.



Similar content being viewed by others
References
Valachis A, Nearchou AD, Lind P. Surgical management of breast cancer in BRCA-mutation carriers: a systematic review and meta-analysis. Breast Cancer Res Treat. 2014;144(3):443–55.
Mavaddat N, et al. Cancer risks for BRCA1 and BRCA2 mutation carriers: results from prospective analysis of EMBRACE. J Natl Cancer Inst. 2013;105(11):812–22.
Ingham SL, et al. Ovarian cancer among 8,005 women from a breast cancer family history clinic: no increased risk of invasive ovarian cancer in families testing negative for BRCA1 and BRCA2. J Med Genet. 2013;50(6):368–72.
Guo F, et al. Use of BRCA Mutation Test in the US, 2004–2014. Am J Prev Med. 2017;52(6):702–9.
Evans DGR, et al. A new scoring system for the chances of identifying a BRCA1/2 mutation outperforms existing models including BRCAPRO. J Med Genet. 2004;41(6):474.
D’Andrea E, et al. Which BRCA genetic testing programs are ready for implementation in health care? A systematic review of economic evaluations. Genet Med. 2016;18(12):1171–80.
Oosterhoff M, van der Maas ME, Steuten LMG. A systematic review of health economic evaluations of diagnostic biomarkers. Appl Health Econ Health Policy. 2016;14(1):51–65.
Tengs TO, Berry DA. The cost effectiveness of testing for the BRCA1 and BRCA2 breast-ovarian cancer susceptibility genes. Dis Manag Clin Outcomes. 2000;1:15–24.
Manchanda R, et al. Cost-effectiveness of population screening for BRCA mutations in Ashkenazi jewish women compared with family history-based testing. J Natl Cancer Inst. 2015;107(1):380.
Holland ML, Huston A, Noyes K. Cost-effectiveness of testing for breast cancer susceptibility genes. Value Health. 2009;12(2):207–16.
Antoniou AC, et al. Predicting the likelihood of carrying a BRCA1 or BRCA2 mutation: validation of BOADICEA, BRCAPRO, IBIS, Myriad and the Manchester scoring system using data from UK genetics clinics. J Med Genet. 2008;45(7):425–31.
Ministry of Health Malaysia and Academy of Medicines Malaysia. Management of Breast Cancer, 2nd Ed. Ministry of Health Malaysia: Putrajaya; 2010. http://www.moh.gov.my/penerbitan/CPG2017/6915.pdf.
Thirthagiri E, et al. Evaluation of BRCA1 and BRCA2 mutations and risk-prediction models in a typical Asian country (Malaysia) with a relatively low incidence of breast cancer. Breast Cancer Res. 2008;10(4):R59.
Yoon SY, et al. Genetic counseling for patients and families with hereditary breast and ovarian cancer in a developing Asian country: an observational descriptive study. Fam Cancer. 2011;10(2):199–205.
Cancer Research Malaysia. Breast Cancer Current Research and Programme: MyBrCa and MyMammo. 2016 05/06/2016]. http://www.cancerresearch.my/our-research/breast-cancer-research/more-than-a-mammo-programme/. Accessed 20 June 2017.
Husereau D et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. BMJ Br Med J 2013;346:f1049.
Kwon JS, et al. Expanding the criteria for BRCA mutation testing in breast cancer survivors. J Clin Oncol. 2010;28(27):4214–20.
Toh GT, et al. BRCA1 and BRCA2 germline mutations in Malaysian women with early-onset breast cancer without a family history. PLoS One. 2008;3(4):e2024.
Allemani C, et al. Global surveillance of cancer survival 1995–2009: analysis of individual data for 25 676 887 patients from 279 population-based registries in 67 countries (CONCORD-2). The Lancet. 2015;385(9972):977–1010.
Tan X-Y, et al. Assessment of preference for hormonal treatment-related health states among patients with breast cancer. Value Health Reg Issues. 2014;3:27–32.
Havrilesky LJ, et al. Determination of quality of life-related utilities for health states relevant to ovarian cancer diagnosis and treatment. Gynecol Oncol. 2009;113(2):216–20.
Peasgood T, Ward SE, Brazier J. Health-state utility values in breast cancer. Expert Rev Pharmacoecon Outcomes Res. 2010;10(5):553–66.
Grann VR, et al. The quality of life associated with prophylactic treatments for women with BRCA1/2 mutations. Cancer J Sci Am. 1999;5(5):283–92.
Cappelli M, et al. Measuring women’s preferences for breast cancer treatments and BRCA1/BRCA2 testing. Qual Life Res. 2001;10(7):595–607.
Metcalfe KA, et al. The risk of ovarian cancer after breast cancer in BRCA1 and BRCA2 carriers. Gynecol Oncol. 2005;96(1):222–6.
Metcalfe K, et al. Predictors of contralateral breast cancer in BRCA1 and BRCA2 mutation carriers. Br J Cancer. 2011;104(9):1384–92.
Metcalfe K, et al. Risk of ipsilateral breast cancer in BRCA1 and BRCA2 mutation carriers. Breast Cancer Res Treat. 2011;127(1):287–96.
Nelson HD, et al. Genetic risk assessment and brca mutation testing for breast and ovarian cancer susceptibility: systematic evidence review for the US preventive services task force. Ann Intern Med. 2005;143(5):362–79.
Department of Statistics Malaysia. Malaysia economics statistics—time series 2015. 2015 30/12/2015 10/05/2016]. https://www.statistics.gov.my/index.php?r=column/ctimeseries&menu_id=NHJlaGc2Rlg4ZXlGTjh1SU1kaWY5UT09. Accessed 20 June 2017.
Central Bank of Malaysia. Kuala Lumpur US$/MYR Reference Rate. 2016 20/06/2017]. http://www.bnm.gov.my/index.php?ch=statistic&pg=kualalumpurusdmyrreferencerate. Accessed 20 June 2017.
Attorney General’s Chambers of Malaysia. Fees (Medical Cost of Services) Order 2014. Putrajaya: Attorney General’s Chambers of Malaysia; 2014.
Clinical Research Centre (CRC). National Healthcare Establishment and Workforce Statistics (Hospital) 2011. Kuala Lumpur: Clinical Research Centre, Ministry of Health Malaysia; 2013.
Lim GCC, et al. Closing the global cancer divide—performance of breast cancer care services in a middle income developing country. BMC Cancer. 2014;14:212.
Ministry of Health Malaysia. Pharmacoeconomic guideline for Malaysia. Kuala Lumpur: Pharmaceutical Services Division; 2012.
Hutubessy R, et al. Generalized cost-effectiveness analysis for national-level priority-setting in the health sector. Cost Effect Resour Alloc C/E. 2003;1:8.
Malaysian Health Technology Assessment Section. Establishing a cost-effectiveness threshold value for health technologies Newsletter, Vol 17. Putrajaya: Malaysian Health Technology Assessment Section (MaHTAS) Medical Development Division Ministry of Health Malaysia; 2015.
Shafie AA, et al. Exploring the willingness to pay for a quality-adjusted life-year in the state of Penang, Malaysia. ClinicoEcono Outcomes Res CEOR. 2014;6:473–81.
Lim YW, et al. PHP201—Determination of cost-effectiveness threshold for Malaysia. Value Health. 2014;17(7):A438.
Briggs A, Claxton K, Sculpher M. Chapter 4: making decision model probabilistic. In: Grey A, Briggs A, editors. Decision modelling for health economic evaluation. Oxford: Oxford University Press; 2011.
Heimdal K, Maehle L, Moller P. Costs and benefits of diagnosing familial breast cancer. Dis Mark. 1999;15(1–3):167–73.
Balmana J, et al. Genetic counseling program in familial breast cancer: analysis of its effectiveness, cost and cost-effectiveness ratio. Int J Cancer. 2004;112(4):647–52.
Kwon JS, et al. Preventing future cancers by testing women with ovarian cancer for BRCA mutations. J Clin Oncol. 2010;28(4):675–82.
International Agency for Research on Cancer (IARC). GLOBOCAN 2012: Estimated cancer incidence, mortality and prevalence worldwide in 2012: Malaysia. 2012 20/12/2016]. http://globocan.iarc.fr/Pages/fact_sheets_population.aspx. Accessed 20 June 2017.
Data Availability Statement
All data used in the analyses are referenced and described in the text and listed in Supplementary File 2. All other information is available from the corresponding authors on reasonable request.
Author information
Authors and Affiliations
Contributions
SYY, SHT and NC conceptualized the research idea; KKL and NC formulated the research questions, and designed and performed the analysis; NAMT, YLW and MKT assisted in model building by providing their clinical inputs, FHS and MD provided secondary data on resource consumption, and assisted in data analysis and interpretation of findings. KKL prepared the first draft of the manuscript. All authors were responsible for critically revising the manuscript and agreed on the final content before submission.
Corresponding author
Ethics declarations
Funding
No funding was involved for this study.
Human or animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
All authors (KKL, SYY, NAMT, FHS, MD, YLW, MKT, SHT, NC) declare no conflicts of interest related to BRCA mutation testing.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lim, K.K., Yoon, S.Y., Mohd Taib, N.A. et al. Is BRCA Mutation Testing Cost Effective for Early Stage Breast Cancer Patients Compared to Routine Clinical Surveillance? The Case of an Upper Middle-Income Country in Asia. Appl Health Econ Health Policy 16, 395–406 (2018). https://doi.org/10.1007/s40258-018-0384-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-018-0384-8