Abstract
Introduction
oral anticoagulant (DOAC) agents are becoming the anticoagulation strategy of choice for most clinical risks for which they are indicated. However, residual uncertainty remains regarding their use in preventing stroke in patients with low bodyweight [< 60 kg or body mass index (BMI) < 18 kg/m2]. We have carried out pooled systematic analyses of published studies to determine the efficacy and safety of these agents compared with warfarin in stroke prevention in patients with low bodyweight.
Methods
We carried out a comprehensive search of electronic databases from inception to June 2023 for eligible studies reporting on the efficacy and safety of direct oral anticoagulants versus warfarin in patients with atrial fibrillation who had low bodyweight. These include PubMed, EMBASE, the Cochrane Database of Systematic Reviews, the Science Citation Index, and the Database of Abstracts of Reviews of Effectiveness. Using the random effects model, derived pooled odd ratios (with their corresponding confidence intervals) of mortality outcomes in patient cohorts exposed to direct oral anticoagulants versus warfarin in patients with atrial fibrillation who had low bodyweight.
Results
Nine studies (n = 159,514 patients) were included in our meta-analysis. DOAC analogs were associated with lower stroke recurrence compared with warfarin [odds ratio (OR) 0.66, 95% confidence interval (CI) 0.49–0.9]; however, there was no significant difference in the composite outcome (OR 0.81, 95% CI 0.59–1.09) and mortality (OR 0.82, 95% CI 0.48–1.41). Additionally, DOAC analogs showed a significant reduction in major bleeding events by 30% compared with warfarin (OR 0.70, 95% CI 0.62–0.80).
Conclusion
In this pooled meta-analytical synthesis of studies comprising both real-world and randomized controlled data, the use of DOAC analogs in patients with atrial fibrillation and low bodyweight (< 60 kg or BMI < 18 kg/m2) was associated with a significant reduction in risks of stroke and major bleeding compared with patient cohorts stabilized on warfarin-based therapy. There was uncertainty regarding the composite outcome and mortality point estimate between these two anticoagulation strategies. This finding helps to resolve the uncertainty associated with the use of DOACs in this cohort. Additionally, it suggests the need for confirmatory non-inferiority randomized controlled trials evaluating DOACs versus warfarin in this cohort of patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Direct oral anticoagulant (DOAC) agents are the preferred approach for stroke prevention in patients with atrial fibrillation. |
Uncertainty remains regarding their use in patients with low bodyweight (LBW). |
Our comprehensive analysis revealed that DOACs usage in stroke prevention for patients with LBW significantly lowers the risk of stroke and major bleeding compared with warfarin. |
1 Introduction
Atrial fibrillation (AF) is the most common type of cardiac arrhythmia [1]. AF could present as persistent, permanent, or paroxysmal AF [1]. Ischemic stroke represents the most morbidity-prone consequence in patients with AF. Strokes related to AF are more severe and have worse outcomes than those due to other cardiovascular risks [2]. Consequently, stroke prevention represents the fundamental therapeutic objective of AF management. National and international clinical guidelines have long established that anticoagulation (AC) is mandatory (where indicated and in the absence of contraindications) to prevent ischemic stroke. Until a few years ago, initial bridging with low-molecular-weight heparin (LMWH) followed by oral anticoagulation (OAC) with vitamin K antagonists (VKA) has been considered the mainstay of therapy [3]. However, as reported in multiple studies, warfarin-based anticoagulation strategy is fraught with many clinical, therapeutic, and logistical issues. These range from potential drug–drug and drug–food interactions to inter- and intra-individual variability in both responses to treatment and risk of side effects [4,5,6,7]. Others include the logistics involved in organizing a reliable and robust international normalizing ratio (INR) monitoring regimen (with its additional cost to the overall cost of healthcare) [4,5,6]. Consequent upon these well-reported shortcomings, direct oral anticoagulants (DOACs) have been developed (including factor IIa (thrombin) and factor Xa inhibitors) and have received marketing authorization for various indications for which their efficacy and safety have been proven. For example, they have been approved by the Food and Drug Administration (FDA) for stroke prevention in patients with AF [7,8,9,10]. A steady stream of randomized controlled clinical trials (RCTs) has demonstrated the non-inferiority of these agents when compared with VKA with regard to both efficacy and safety for systemic embolism and stroke risk reduction in patients with AF [11,12,13,14,15]. This has resulted in their incorporation into therapeutic national/society guidelines [16, 17]. Since introducing DOACs to the market, OAC management has witnessed a significant paradigm shift [18].
Among the favorable pharmacokinetic and pharmacodynamics of DOACs is their wider therapeutic window at fixed dosing regimens and minimal and manageable food and drug interactions without requiring routine monitoring [19]. However, the low representation of patients with low bodyweight (LBW; < 60 kg) in the main DOACs trials has raised questions about the efficacy, adequacy of fixed dosing, and safety in these cohorts of patients.
There is a paucity of evidence examining the efficacy and safety of DOACs in patients with LBW. Patients with LBW usually exert an inaccurate estimated renal function due to lower muscle mass, affecting DOACs use and their optimum dosing [20]. Additionally, initial RCTs evaluating DOACs in AF or venous thromboembolism (VTE) did not incorporate weight as an exclusion criterion; however, extreme-body-weight cohorts have hardly been reasonably represented in clinical trials. [21, 22].
Owing to this demonstrable lack of robust data, DOACs pharmacokinetic studies have attempted to suggest prescriptive recommendations in patients with LBW exposed to DOACs [21]. Chen et al. recommend adjusted doses of apixaban and edoxaban and avoiding dabigatran and rivaroxaban. [20]. Covert et al. recommend unadjusted doses for rivaroxaban, apixaban, and edoxaban and cautiously using dabigatran [23].
A real-world Asian population study showed that using DOACs (apixaban, rivaroxaban, dabigatran, and edoxaban) with an unadjusted dose in LBW was safer and more effective than warfarin. [23]. Similarly, Barakat et al. found that DOACs have a 30% significant reduction in the risk of ischemic stroke and a 60% reduction in the risk of bleeding events; however, the bleeding outcome did not reach statistical significance. [24].
Therefore, there is an unresolved uncertainty regarding the utility of DOAC analogs as a stroke prevention strategy in patients with LBW [body mass index (BMI) < 18 kg/m2 or weight < 60 kg]. It will be valuable to demonstrate that DOACs are at least non-inferior to VKA with regard to efficacy and safety in this patient population.
In this meta-analysis, we aim to evaluate the effectiveness (rates of stroke events, composite outcome, mortality) and safety (major bleeding) of DOAC analogs compared with warfarin in patients with AF and extremely LBW.
2 Methods
This review followed PRISMA guidelines.
2.1 Study Eligibility Criteria
This systematic review and meta-analysis was conducted adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Additionally, the study was registered with PROSPERO under the registration number CRD42023456605. We included real-world observational data and randomized controlled trials comparing DOAC analogs versus warfarin in patients with LBW (BMI < 18 or weight < 60 Kg). Ethical clearance was not necessary, as this research involved already published data accessible in the public domain.
2.2 Search Strategy
We conducted a literature search of PubMed, Medline, and EMBASE since their inception till 01/06/2023. No language, date, or article type restrictions were adopted in our search strategy. Example of a database search strategy is: ((((((((((((((direct oral anticoagulants) OR (new oral anticoagulants)) OR (rivaroxaban)) OR (Dabigatran)) OR (Apixaban)) OR (Edoxaban)) OR (DOACs)) OR (NOACs)) OR (DOACs [Title/Abstract])) OR (direct oral anticoagulants[Title/Abstract])) OR (new oral anticoagulants[Title/Abstract])) OR (anticoagulant agents[MeSH Terms]) AND (2022/5/31:2023/5/10[pdat])) AND (((((((warfarin[MeSH Terms]) OR (warfarin)) OR (vitamin K antagonist)) OR (Coumadin)) OR (Warfarin Sodium)) OR (warfarin[Title/Abstract])) OR (vitamin k antagonist[Title/Abstract]) AND (2022/5/31:2023/5/10[pdat]))) AND (((((atrial fibrillation[Title/Abstract]) OR (Atrial Fibrillations)) OR (A. Fib)) OR (atrial fibrillation[MeSH Terms])) OR (atrial fibrillations[MeSH Terms]) AND (2022/5/31:2023/5/10[pdat]))) AND (((((((low weight) OR (low bodyweight)) OR (underweight)) OR (low weight[Title/Abstract])) OR (low bodyweight[Title/Abstract])) OR (underweight[MeSH Terms])) OR (low weight[MeSH Terms]) AND (2022/5/31:2023/5/10[pdat])). Additionally, we attempted a manual reference search of retrieved studies.
2.3 Inclusion and Exclusion Criteria
Inclusion criteria were as follows: (1) The study had to be either a randomized controlled trial (RCT) or an observational (prospective or retrospective cohort) study; (2) it should have involved patients diagnosed with atrial fibrillation (AF) and exhibiting LBW (defined as a BMI < 18 or weight < 60 kg) who were prescribed warfarin or DOACs (dabigatran, rivaroxaban, apixaban, or edoxaban); and (3) the study needed to provide quantitative estimates of hazard ratios (HRs) and 95% confidence intervals (CIs), specifically addressing safety and effectiveness outcomes among these patients. At a minimum, the studies were required to report on stroke recurrence or major bleeding events to be considered for inclusion in the review.
We excluded studies that focused on patients with AF but did not include a LBW cohort. Additionally, certain types of publications (e.g., reviews, case reports, case series, letters, and conference abstracts) were excluded due to insufficient data or lack of detailed study information. Pediatric patient cohorts (< 18 years old) and studies that did not meet the inclusion criteria were also excluded.
2.4 Screening and Data Extraction
The title and abstract were screened initially. Eligible articles were retrieved for full-text review and assessment for inclusion in our review. Two reviewers (ME and MS) performed the search and screening. In the case of disagreement between the reviewers, this was resolved by consensus, or a third reviewer (AE) adjudicated the disagreement following the protocol. We utilized a predetermined template for retrieving the data. The extracted information encompasses general article information, such as authorship, publication year, study methodology, intervention and control specifics, outcomes, weight, and more.
2.5 Outcomes
The primary outcome in our review is the rate of ischemic stroke recurrence, composite outcome (combined ischemic stroke, systemic embolism, and myocardial infarction), and all-cause mortality. Major bleeding events served as our secondary outcome (as defined by the primary study authors). We would look at these outcomes at 6 months of follow-up whenever specified in the study; otherwise, we would consider the extended observation period when the exposure duration was not specified.
2.6 Study Quality and Risk of Bias Assessment
Using the Cochrane Risk of Bias Tool for Randomized Controlled Trials, reviewers evaluated the risk of bias (ROB) in the included studies [25]. The six bias domains addressed by the risk of bias tool are selection bias, performance bias, detection bias, attrition bias, reporting bias, and other biases. Cohort study quality was evaluated using the Newcastle Ottawa Scale (NOS) [26]. Eight fundamental factors were measured using the NOS scale, broken into three major categories: Comparability, exposure, and research quality selection. In the case of post hoc analysis, we also took a distinct strategy to evaluate the risks of bias in each of the original trials while using data from the research [27]. The Review Manager (RevMan) software version 5.4 and the Risk-of-Bias Visualization (robvis) tools were used to create the visualization of the ROBs numbers.
2.7 Statistical Analysis
The odds ratios (OR) were computed as measures of effect size. The Forest plot was generated to summarize the results. Additionally, we conducted a sensitivity analysis to screen for consistency and small-study effects. The I2 statistic was used to report heterogeneity. An I2 > 50% is suggestive of marked heterogeneity in our review. The random-effects model was used as our meta-analytical technique. All statistical analyses were performed with STATA software (Stata MP 15 (StataCorp, College Station, TX).
3 Results
Our exhaustive search strategy retrieved 241 titles. After screening these records, we selected 120 titles. After reviewing the abstracts, 19 remaining studies were potentially available, which were then subjected to full-text screenings. Following our predefined inclusion and exclusion criteria, we excluded 10 studies for various reasons: (1) wrong outcome (n = 1); (2) wrong study design (n = 1); (3) foreign language (n = 1); (4) review articles, meta-analyses, or opinions (n = 5); and (5) wrong population (n = 2). The total number of patients evaluated in these studies is 159,514 patients. The included studies were five observational and four randomized controlled studies [29,30,31,32,33,34,35,36,37] meeting our eligibility criteria (Fig. 1 shows the PRISMA flow diagram; Table 1 summary of studies included in the meta-analysis).
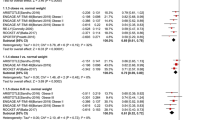
3.1 Recurrent stroke
Only four studies evaluated stroke recurrent events in patients with LBW [31, 32, 34, 35]. These studies showed that DOAC analogs were associated with a 34% reduction of stroke events compared with warfarin (OR 0.66, 95% CI 0.49–0.9, Q = 3.70, I2 = 30.58%). The low I2 suggested the homogeneity of the results (Fig. 2). We conducted subgroup analysis of the primary efficacy end point based on ethnicity and study type (Fig. 3). The funnel plot revealed no marked asymmetry (Fig. 8).
A Depicting a forest plot of stroke recurrence rates in DOAC analogs compared with warfarin in patients with LBW. B Depicting a forest plot of composite outcomes in DOAC analogs compared with warfarin in patients with LBW. C Depicting a forest plot of mortality in DOAC analogs compared with warfarin in patients with LBW. D Depicting a forest plot of major bleeding events in DOAC analogs compared with warfarin in patients with LBW. REML random-effects model
3.2 Composite Outcome
Six studies reported composite outcomes in patients with LBW [28,29,30,31, 33, 36]. Prescribing DOACs in patients with LBW with atrial fibrillation had a consistent non-significant trend toward an overall reduced composite outcome by 19% (OR 0.81, 95% CI 0.59–1.09, Q = 7.67, I2 = 42.24%; Fig 2). Among all DOACs, only dabigatran demonstrated a significant reduction in composite outcomes compared with warfarin (Fig. 4).
3.3 Mortality
Six studies evaluated mortality outcomes in patients with LBW [31,32,33,34,35,36]. These studies showed no significant difference in mortality associated with DOACs compared with warfarin. In the pooled analysis of the six studies, patients with LBW with AF who received DOACs had no significant mortality difference versus warfarin (OR 0.82, 95% CI 0.48–1.41; Fig. 5; Q = 1.78, I2 = 0%) (Fig. 6).(see Fig. 6).
3.4 Major Bleeding
Nine studies evaluated and reported the risk of major bleeding events [28,29,30,31,32,33,34,35,36]. DOAC analogs had a consistent significant trend toward an overall reduced risk of major bleeding events by 30% (OR 0.70, 95% CI 0.62–0.80, Q = 6.69, I2 = 0%; Fig. 2). Among all DOACs, only apixaban significantly reduced major bleeding events compared with warfarin (Fig. 7). The funnel plot showed no marked asymmetry (Fig. 8).
A Funnel plot to assess the publication bias for studies assessing stroke recurrence in DOAC analogs versus warfarin displaying no marked asymmetry. B Funnel plot to assess the publication bias for studies assessing major bleeding events in DOAC analogs versus warfarin showing no marked asymmetry. C Regression-based Egger test for small-study effects denoting a negligible degree of publication bias. REML random-effects model
3.5 Risk of Bias Assessment
Three clinical trials and one post hoc analysis showed a low risk of bias, while Bayer AG et al. 2010 showed an overall unclear risk of bias (Fig. 9). The main domain of high risk among the four studies was allocation concealment (selection bias). The overall quality assessment of cohort studies revealed a low risk of bias among all included studies (Fig. 8), and the “adequacy of follow-up of cohort” item was the leading cause of the high risk of bias (Fig. 9).
4 Discussion
From this pooled meta-analytical synthesis of studies exploring the efficacy and safety of DOACs versus warfarin in patients with LBW who have nonvalvular AF (NVAF), we found those exposed to DOACs had about 34% relative risk reduction in stroke-related outcomes compared with those on warfarin. Conversely, we found instability in the final point estimates of DOACs versus warfarin in mortality reduction and the composite outcomes. Among the DOAC analogs, only dabigatran demonstrated a significant reduction in composite outcomes compared with warfarin. Other DOACs showed a reduction trend in hard clinical endpoints but with unstable point estimates. The significant reduction in composite-related outcomes in cohorts of patients on dabigatran, in particular, is a novelty given that its pivotal primary trials in both NVAF and VTE [28, 37,38,39], recruited very few patients with LBW, which therefore meant that these studies failed to provide any actionable insight into its effect on patients with LBW. The RELY trial, in particular, only recruited 376 (about 2% of the total population) patients with NVAF and was not powered ab initio to detect efficacy and safety differences in patients weighing < 50 kg. Our pooled synthesis provided the requisite numerical scaffold and statistical power crucial to testing the weighted effect of LBW on hard clinical endpoints in these cohorts of patients. Patients with LBW represent an essential proportion of the general population, and the outcome of this review will provide an additional layer of therapeutic reassurance to this demography, at least in NVAF-related stroke risk reduction.
The advent of DOACs did herald understandable excitement and genuine expectation, especially in their ability to reduce hard clinical endpoints effectively and safely without the associated inconvenience of traditional VKAs (such as the need for therapeutic drug monitoring and drug–drug interactions, among others). Reported clinical outcomes from extremes-of-weight patient cohort studies, especially in observational patient databases, appear to negate these benefits. Despite combining RCTs and observational studies in the total pool of studies evaluated in this review, we found modest heterogeneity (I2 = 30%), further emphasizing the stability of our estimates, especially those relating to reduced stroke-related outcomes.
The dearth of robust, specific pharmacokinetic studies exploring dose-related hard clinical outcomes in these patients’ cohorts meant that estimates from our pooled synthesis would provide the very first robust data to guide decision-making at the guideline evaluation stage and the patient level. Although previous reviews, as well as some international guidelines, have suggested the avoidance of DOACs in patients with LBW [23, 40], our recommendation, especially with regard to stroke patients, is prescriptive and explicit; they should be considered reliable and safe in this cohort of patients (except in situations where explicit contraindications for the use of DOACs exists). Notably, within the studies analyzed in our meta-analysis, individuals with LBW predominantly received reduced doses rather than the standard dosage. The direct impact of this disparity on safety and effectiveness outcomes is not immediately clear. Determining whether this factor should prompt recommendations to initiate patients with low bodyweight on standard doses requires further investigation. Current guidelines suggest the utilization of DOACs, particularly apixaban and edoxaban, in patients weighing between 40 and 60 kg. For those weighing less than 40 kg, guidelines recommend either the use of vitamin K antagonists (VKAs) or conducting plasma level measurements of DOACs [41]. However, there is presently no guidance available regarding dose reduction in instances of supra-therapeutic levels [42]. This highlights an area necessitating additional guidance and research to establish optimal dosing strategies for individuals with LBW.
Pivotal trials of DOACs such as ROCKET-AF [29] did report data for underweight patients, but they constitute an insignificant proportion of the entire trial population (4.25% of the study population had a BMI of ≤ 25 kg/m2). Of all the pivotal trials of DOACs leading to their marketing authorization, only ARISTOTLE [43], exploring the efficacy and safety of apixaban for prevention risk reduction in patients with NVAF, recruited what could be considered a relatively “reasonable” number of patients with LBW [11% (n = 1985) of the study cohort]. A pre-specified analysis of this LBW cohort, as reported elsewhere [28], showed no difference in efficacy and safety outcomes between them and patients with normal bodyweight. This perhaps explains the lack of uncertainty regarding apixaban’s efficacy and safety outcomes in patients with LBW. There is, however, a caveat regarding the absence of additional information on the exact proportion of patients with LBW in this trial that had apixaban dose reduction.
Additionally, our pooled meta-analytical synthesis showed an overall reduced risk of major bleeding episodes (30%) with DOACs compared with warfarin. Among the spectrum of DOACs, our subgroup analysis unveiled a significant reduction in major bleeding events with apixaban compared with warfarin. Our findings align with the conclusions drawn by Ballestri et al. and Lopez et al., both asserting that apixaban demonstrated the most favorable safety profile among oral anticoagulants (OACs) [42, 44]. This consistency in results reinforces the safety advantages of apixaban. Similar affirmations regarding apixaban’s safety benefits were evident in real-world observational trials, systematic reviews, and meta-analyses conducted by Li G et al. and Zhang J et al. and their research teams, who also found apixaban to be the most preferred OAC [45, 46].
One often reported flaw of previous studies that compared bleeding risks associated with DOACs was the lack of head-to-head comparison between individual DOACs with VKA; rather, bleeding risks were reported as an aggregate of all DOACs combined. As alluded to earlier, no such uncertainty regarding bleeding risks subsists for apixaban [40]. The ENGAGE-AF TIMI 48 trial [30] examining the efficacy and safety of two doses of edoxaban in patients with NVAF did not report any focused analyses in patients with LBW. Therefore, no robust prescriptive recommendation regarding its use has been forthcoming from international clinical guidelines. However, because ENGAGE-AF TIMI 48 [30] data showed a significantly higher risk of ischemic strokes among patients randomized to the 30 mg edoxaban dose, it is unlikely any dose other than the alternative 60 mg will suffice in any cohort of patients (including those with LBW). This concern also extends to its bleeding risks.
Our meta-analysis results are consistent with Grymonprez et al.’s meta-analysis, which demonstrated a significant reduction in the risks of stroke/systemic embolism and major bleeding in patients treated with DOACs compared with those treated with warfarin, with no significant difference in all-cause mortality [47]. Additionally, we examined the composite outcomes between the two anticoagulation strategies, and our findings did not show any statistically significant differences. In contrast, a meta-analysis conducted by Boonyawat et al. included a diverse cohort of patients with AF and acute venous thromboembolism (VTE), receiving DOACs or warfarin for stroke prevention or VTE treatment. Their analysis revealed higher incidence of thromboembolic events in patients with LBW (4.28%) compared with patients who do not have LBW (2.74%), suggesting that patients with LBW may indeed pose a higher risk of thromboembolic events in anticoagulated patients, but with no significant difference in bleeding outcomes between LBW group and non-LBW group (5.96% versus 6.08). [48]
The recent meta-analysis exploring the effectiveness and safety of warfarin and DOACs in individuals with AF or VTE across different BMI categories revealed noteworthy findings. It showed a higher incidence of major bleeding events among underweight patients using DOACs compared with patients with normal weight. However, there was no significant difference in VTE or stroke recurrence rates between these groups. Additionally, when comparing DOACs to warfarin across various BMI categories (normal weight, overweight, and obese), the analysis revealed a significant increase of major bleeding events among patients on warfarin compared with DOACs. However, the rates of VTE recurrence or stroke did not significantly differ between the two therapies within the same weight categories. However, it is crucial to note that this analysis did not specifically examine or report on the comparison between DOACs and warfarin in the LBW category [49].
4.1 Strengths and Limitations
This meta-analytical review represents the first robust purposeful examination of published reports examining the efficacy and safety of DOACs versus warfarin among patients with LBW who have NVAF. Our finding of a significant reduction in systemic stroke risk reduction and reduced risks of major bleeding among patients with LBW on DOACs versus warfarin is seminal. It provides more clarity in the management of these patients. It has the prescriptive potential to necessitate national and international guidelines review to give a more explicit recommendation of DOACs for reducing systemic stroke risks in these cohorts of patients. Including data from pivotal Marche clinical trials responsible for acquiring the various DOACs marketing authorization [29, 31, 43] in our analyses adds rigor to our analyses and inferences drawn from them.
The combination of RCTs and real-world data in our analyses may have accounted for the lack of certainty regarding the point estimates of some of our evaluated outcomes, especially composite outcomes and subgroup analyses.
5 Conclusion
In a pooled examination of studies evaluating therapeutic anticoagulation strategies, patient cohorts with LBW who received DOACs had a significant reduction in stroke and major bleeding risks compared with those receiving warfarin. There was uncertainty regarding mortality and composite outcomes between the two strategies. This will suggest the need to revisit current clinical guidelines, especially on updating recommendations regarding the safety of DOACs in LBW patients with stroke.
References
Healey JS, Connolly SJ, Gold MR, Israel CW, Van Gelder IC, Capucci A, Lau C, Fain E, Yang S, Bailleul C, et al. Subclinical atrial fibrillation and the risk of stroke. N Engl J Med. 2012;366:120–9.
Lip GY. Anticoagulation therapy and the risk of stroke in patients with atrial fibrillation at ‘moderate risk’ [CHADS2 score=1]: simplifying stroke risk assessment and thromboprophylaxis in real-life clinical practice. Thromb Haemost. 2010;103:683–5.
Stevens SM, Woller SC, Kreuziger LB, Bounameaux H, Doerschug K, Geersing GJ, Huisman MV, Kearon C, King CS, Knighton AJ, Lake E, Murin S, Vintch JRE, Wells PS, Moores LK. Antithrombotic therapy for VTE disease: second update of the CHEST Guideline and Expert Panel Report. Chest. 2021;160(6):e545–608. https://doi.org/10.1016/j.chest.2021.07.055. (Epub 2021 Aug 2. Erratum in: Chest. 2022;162(1):269. PMID: 34352278).
Andreu, V. and J., Pérez- Roldán V, López-Fernández MF. Pharmacogenetics of acenocoumarol in patients with extreme dose requirements. J Thromb Haemost. 1012, 2010. 8 SRC - BaiduScholar.
Holbrook AM, et al. Systematic overview of warfarin and its drug and food interactions. Arch Intern Med. 2005;165(10):1095–106.
Sconce E, et al. Vitamin K supplementation can improve stability of anticoagulation for patients with unexplained variability in response to warfarin. Blood. 2007;109(6):2419–23.
Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bounameaux H, Huisman M, King CS, Morris TA, Sood N, Stevens SM, Vintch JRE, Wells P, Woller SC, Moores L. Antithrombotic therapy for VTE Disease: CHEST Guideline and Expert Panel Report. Chest. 2016;149(2):315–52. https://doi.org/10.1016/j.chest.2015.11.026. (Epub 2016 Jan 7. Erratum in: Chest. 2016;150(4):988. PMID: 26867832.).
https://www.accessdata.fda.gov/drugsatfda_docs/nda/2010/022512orig1s000toc.cfm#:~:text=Approval%20Date%3A%2010%2F19%2F2010. Accessed 25 Jul 2023.
https://www.accessdata.fda.gov/drugsatfda_docs/nda/2011/022406Orig1s000TOC.cfm. Accessed 25 July 2023.
https://www.accessdata.fda.gov/drugsatfda_docs/nda/2015/206316orig1orig2s000toc.cfm. Accessed 25 July 2023.
https://www.accessdata.fda.gov/drugsatfda_docs/nda/2012/202155orig1s000toc.cfm. Accessed 25 July 2023.
Agnelli G, et al. Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med. 2013;369(9):799–808.
Hokusai VTEI, et al. Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. N Engl J Med. 2013;369(15):1406–15.
Investigators E, et al. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med. 2010;363(26):2499–510.
Investigators EP, et al. Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med. 2012;366(14):1287–97.
Schulman S, et al. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009;361(24):2342–52.
Kearon C, et al. Antithrombotic therapy for VTE Disease: CHEST Guideline and Expert Panel Report. Chest. 2016;149(2):315–52.
Phillippe HM, et al. Pharmacist interventions regarding the appropriateness of apixaban, rivaroxaban, dabigatran, and warfarin in a university-affiliated outpatient clinic. J Pharm Technol. 2016;32(6):245–52.
Bauer KA. Pros and cons of new oral anticoagulants. Hematology Am Soc Hematol Educ Program. 2013;2013:464–70. https://doi.org/10.1182/asheducation-2013.1.464.
Steffel J, Verhamme P, Potpara TS, Albaladejo P, Antz M, Desteghe L, Haeusler KG, Oldgren J, Reinecke H, Roldan-Schilling V, et al. The 2018 European Heart Rhythm Association practical guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur Heart J. 2018;39:1330–93.
Chen A, Stecker E, Warden AB. Direct oral anticoagulant use: a practical guide to common clinical challenges. J Am Heart Assoc. 2020;9(13):e017559.
Boonyawat K, Caron F, Li A, Chai-Adisaksopha C, Lim W, Iorio A, Lopes RD, Garcia D, Crowther MA. Association of body weight with efficacy and safety outcomes in phase III randomized controlled trials of direct oral anticoagulants: a systematic review and meta-analysis. J Thromb Haemost. 2017;15:1322–33.
Lee SR, Choi EK, Park CS, Han KD, Jung JH, Oh S, Lip GYH. Direct oral anticoagulants in patients with nonvalvular atrial fibrillation and low body weight. J Am Coll Cardiol. 2019;73:919–31.
Covert K, Branam DL. Direct-acting oral anticoagulant use at extremes of body weight: literature review and recommendations. Am J Health Syst Pharm. 2020;77(11):865–76. https://doi.org/10.1093/ajhp/zxaa059. (PMID: 32426845).
Barakat AF, Jain S, Masri A, Alkukhun L, Senussi M, Sezer A, Wang Y, Thoma F, Bhonsale A, Saba S, Mulukutla S. Outcomes of direct oral anticoagulants in atrial fibrillation patients across different body mass index categories. JACC Clin Electrophysiol. 2021;7(5):649–58. https://doi.org/10.1016/j.jacep.2021.02.002. (Epub 2021 Mar 31 PMID: 33812834).
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Br Med J. 2011;18(343): d5928.
Wells GA, Shea B, O’Connel D. et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. Department of Epidemiology and Community Medicine, University of Ottawa, Canada; 2009; ohri.ca/programs/clinical_epidemiology/oxford.htm
Koval N, Alves M, Plácido R, et al. Direct oral anticoagulants versus vitamin K antagonists in patients with antiphospholipid syndrome: systematic review and meta-analysis. RMD Open. 2021;7: e001678. https://doi.org/10.1136/rmdopen-2021-001678.
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, Pogue J, Reilly PA, Themeles E, Varrone J, Wang S, Alings M, Xavier D, Zhu J, Diaz R, Lewis BS, Darius H, Diener HC, Joyner CD, Wallentin L. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–51. https://doi.org/10.1056/NEJMoa0905561. (Epub 2009 Aug 30. Erratum in: N Engl J Med. 2010;363(19):1877).
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, Breithardt G, Halperin JL, Hankey GJ, Piccini JP, Becker RC, Nessel CC, Paolini JF, Berkowitz SD, Fox KA, Califf RM, ROCKET AF Investigators. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–91. https://doi.org/10.1056/NEJMoa1009638. (Epub 2011 Aug 10).
Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, Waldo AL, Ezekowitz MD, Weitz JI, Špinar J, Ruzyllo W, Ruda M, Koretsune Y, Betcher J, Shi M, Grip LT, Patel SP, Patel I, Hanyok JJ, Mercuri M, Antman EM, ENGAGE AF-TIMI 48 Investigators. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093–104. https://doi.org/10.1056/NEJMoa1310907.
Berglund E, Wallentin L, Oldgren J, Renlund H, Alexander JH, Granger CB, Hohnloser SH, Hylek EM, Lopes RD, McMurray JJ, Lytsy P. Effects of apixaban compared with warfarin as gain in event-free time—a novel assessment of the results of the ARISTOTLE trial. Eur J Prev Cardiol. 2020;27(12):1311–9.
Lee SR, Choi EK, Park CS, Han KD, Jung JH, Oh S, Lip GYH. Direct oral anticoagulants in patients with nonvalvular atrial fibrillation and low body weight. J Am Coll Cardiol. 2019;73(8):919–31.
Russo V, Attena E, Di Maio M, Carbone A, Parisi V, Rago A, Grieco FV, Buonauro A, Golino P, Nigro G. Non-vitamin K vs vitamin K oral anticoagulants in patients aged > 80 year with atrial fibrillation and low body weight. Eur J Clin Invest. 2020;50(11):e13335.
Lee SR, Choi EK, Jung JH, Park SH, Han KD, Oh S, Lip GYH. Body mass index and clinical outcomes in Asian patients with atrial fibrillation receiving oral anticoagulation. Stroke. 2021;52(2):521–30.
Nakao YM, Nakao K, Wu J, Nadarajah R, Camm AJ, Gale CP. Risks and benefits of oral anticoagulants for stroke prophylaxis in atrial fibrillation according to body mass index: nationwide cohort study of primary care records in England. EClinicalMedicine. 2022;31(54): 101709.
Russo V, Attena E, Baroni M, Trotta R, Manu MC, Kirchhof P, De Caterina R. Clinical performance of oral anticoagulants in elderly with atrial fibrillation and low body weight: insight into Italian cohort of PREFER-AF and PREFER-AF prolongation registries. J Clin Med. 2022;11(13):3751.
Schulman S, Kearon C, Kakkar AK, Mismetti P, Schellong S, Eriksson H, Baanstra D, Schnee J, Goldhaber SZ. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009;361(24):2342–52.
Schulman S, Kakkar AK, Schellong SM, Goldhaber SZ, Henry E, Mismetti P, Christiansen AV, Schnee J, Kearon C. A randomized trial of dabigatran versus warfarin in the treatment of acute venous thromboembolism (RE-COVER II). Blood. 2011;118(21):205.
Schulman S, Kearon C, Kakkar AK, Schellong S, Eriksson H, Baanstra D, Kvamme AM, Friedman J, Mismetti P, Goldhaber SZ. Extended use of dabigatran, warfarin, or placebo in venous thromboembolism. N Engl J Med. 2013;368(8):709–18.
Burnett AE, Mahan CE, Vazquez SR, Oertel LB, Garcia DA, Ansell J. Guidance for the practical management of the direct oral anticoagulants (DOACs) in VTE treatment. J Thromb Thrombolysis. 2016;41(1):206–32. https://doi.org/10.1007/s11239-015-1310-7.
Steffel J, Collins R, Antz M, Cornu P, Desteghe L, Haeusler KG, Oldgren J, Reinecke H, Roldan-Schilling V, Rowell N, Sinnaeve P, Vanassche T, Potpara T, Camm AJ, Heidbüchel H, Lip GY, Deneke T, Dagres N, Boriani G, Field M. 2021 European Heart Rhythm Association practical guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Europace. 2021;23(10):1612–76. https://doi.org/10.1093/europace/euab065.
Ballestri S, Romagnoli E, Arioli D, Coluccio V, Marrazzo A, Athanasiou A, Di Girolamo M, Cappi C, Marietta M, Capitelli M. Risk and management of bleeding complications with direct oral anticoagulants in patients with atrial fibrillation and venous thromboembolism: a narrative review. Adv Ther. 2023;40(1):41–66. https://doi.org/10.1007/s12325-022-02333-9. (Epub 2022 Oct 16. PMID: 36244055; PMCID: PMC9569921).
Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, Al-Khalidi HR, Ansell J, Atar D, Avezum A, Bahit MC. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–92.
López-López JA, Sterne JAC, Thom HHZ, et al. Oral anticoagulants for prevention of stroke in atrial fibrillation: systematic review, network meta-analysis and cost effectiveness analysis. Br Med J. 2017;359:j5058.
Li G, Lip GYH, Holbrook A, et al. Direct comparative effectiveness and safety between non-vitamin K antagonist oral anticoagulants for stroke prevention in nonvalvular atrial fibrillation: a systematic review and meta-analysis of observational studies. Eur J Epidemiol. 2019;34:173–90.
Zhang J, Wang X, Liu X, et al. Comparative effectiveness and safety of direct acting oral anticoagulants in nonvalvular atrial fibrillation for stroke prevention: a systematic review and meta-analysis. Eur J Epidemiol. 2021;36:793–812. https://doi.org/10.1007/s10654-021-00751-7.
Grymonprez M, De Backer TL, Steurbaut S, Boussery K, Lahousse L. Non-vitamin K antagonist oral anticoagulants (NOACs) versus warfarin in patients with atrial fibrillation and (morbid) obesity or low body weight: a systematic review and meta-analysis. Cardiovasc Drugs Ther. 2022;36(4):749–61. https://doi.org/10.1007/s10557-020-07122-6IF:3.4Q2.
Boonyawat K, Caron F, Li A, et al. Association of body weight with efficacy and safety outcomes in phase III randomized controlled trials of direct oral anticoagulants: a systematic review and meta-analysis. J Thromb Haemost. 2017;15(7):1322–33. https://doi.org/10.1111/jth.13701.
Almas T, Muhammad F, Siddiqui L, et al. Safety and efficacy of direct oral anticoagulants in comparison with warfarin across different BMI ranges: a systematic review and meta-analysis. Ann Med Surg (Lond). 2022;77:103610. https://doi.org/10.1016/j.amsu.2022.103610.
Acknowledgment
The Qatar National Library (QNL) provides the Open-access funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open Access funding provided by the Qatar National Library. Apart from the publication fund provided by QNL, no other funding was sought for the conduction of this review.
Conflict of Interest
Mohamed Nabil Elshafei, Muhammad Salem, Ahmed El-Bardissy, Mohamed S Abdelmoneim, Ahmed Khalil, Sherine Elhadad, and Mohammed Danjuma declare no conflicts of interest relevant to this review or its publication.
Ethics Approval
None is sought or required, as this is a secondary synthesis of already available data.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Author’s Contributions
ME, MAM, and AE agreed on the review idea. ME and MS performed the initial search, screening, and data extraction. MA, AE, MS, and ME extracted data. ME and MID constructed the tables. ME and MD analyzed the data. ME produced the figures. ME, AE, MD, and MA wrote the initial manuscript. The manuscript was then critically revised by ME, MID, and AE. All the authors approved the final version of the manuscript for publication.
Data Availability Statement
All the data generated or analyzed during this study are included in the publication article.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Elshafei, M.N., El-Bardissy, A., Salem, M. et al. Comparative Effectiveness and Safety of Direct Oral Anticoagulants Compared with Warfarin in Patients with Low Bodyweight who have Atrial Fibrillation: A Systematic Review and Meta-analysis. Am J Cardiovasc Drugs 24, 255–271 (2024). https://doi.org/10.1007/s40256-024-00628-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-024-00628-6