Abstract
Purpose
To examine factors of influence in diabetes management and their association with self-reported health outcomes in patients with type 2 diabetes treated at Federally Qualified Health Centers (FQHCs).
Methods
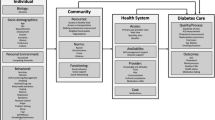
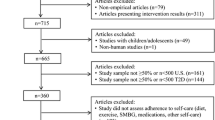
This cross-sectional study examined data from the 2014 Health Center Patient Survey (HCPS). Predictor variables were categorized across three levels of the National Institute on Minority Health and Health Disparities research framework. Outcome variables retrieved from HCPS included self-reports of blood glucose levels, and diabetes-related emergency department (ED)/hospital visits during past year.
Results
A total of 936 patients with diabetes were included. Most (65%) participants received a diabetes self-management plan. During the previous year, 72% received > = 2 A1C checks, 52% reported high blood glucose levels, and 12% visited an ED/hospital. Multivariable results showed that insulin use and receiving a self-management plan were associated with high blood glucose levels and ED/hospital visits. Community factors of being unable to get medications and receiving a specialist foot exam were respectively associated with high blood glucose levels and ED/hospital visits.
Conclusion
Different factors were associated with health outcomes in patients with diabetes treated at FQHCs. Identifying these factors can help with targeted screening and follow-up and assessing potential interventions to improve health outcomes.
Similar content being viewed by others
References
National Diabetes Statistics Report. In: Centers for Disease Control and Prevention. 2022. https://www.cdc.gov/diabetes/data/statistics-report/index.html. Accessed Jun 12 2023.
Cheng YJ, Kanaya AM, Araneta MRG, Saydah SH, Kahn HS, Gregg EW, et al. Prevalence of diabetes by race and ethnicity in the United States, 2011–2016. JAMA. 2019;322(24):2389–98.
American Diabetes Association. 6. Glycemic targets: Standards of Medical Care in diabetes-2021. Diabetes Care. 2021;44(Suppl 1):S73–84.
Yan JW, Gushulak KM, Columbus MP, van Aarsen K, Hamelin AL, Wells GA, et al. Risk factors for recurrent emergency department visits for hyperglycemia in patients with diabetes mellitus. Int J Emerg Med. 2017;10(1):23.
Kazemian P, Shebl FM, McCann N, Walensky RP, Wexler DJ. Evaluation of the cascade of diabetes care in the United States, 2005–2016. JAMA Intern Med. 2019;179(10):1376–85.
Kim S. Burden of hospitalizations primarily due to uncontrolled diabetes: implications of inadequate primary health care in the United States. Diabetes Care. 2007;30(5):1281–2.
Health Center Program Award Recipients. In: Helath Resources & Services Administration. https://www.hrsa.gov/opa/eligibility-and-registration/health-centers/fqhc/index.html. Accessed Jun 12 2023.
Health center program.: Impact and growth. In: Health Resources & Services Administration. https://bphc.hrsa.gov/about/healthcenterprogram/index.html. Accessed Jun 12 2023.
National Health Center Program uniform data system (UDS). awardee data. In: Health Resources and Services Administration. https://bphc.hrsa.gov/uds/datacenter.aspx. Accessed Jun 12 2023.
American Diabetes Association. 4. Comprehensive medical evaluation and assessment of comorbidities: standards of Medical Care in diabetes-2021. Diabetes Care. 2021;44(Suppl 1):40–52.
Oladele CRW, Barnett E. Racial/Ethnic and social class differences in preventive care practices among persons with diabetes. BMC Public Health. 2006;6(1):259.
Kamat S, Gousse Y, Muzumdar J, Gu A. Trends and disparities in quality of diabetes care in the US: the national health and nutrition examination survey, 1999–2016. Inov Pharm. 2019;10(4):17.
NIMHD Research Framework. In: National Instituite on Minority Health and Health Disparities. https://nimhd.nih.gov/researchFramework. Accessed Jun 13 2023.
Rivich J, Kosirog ER, Billups SJ, Petrie JL, Saseen JJ. Social and psychosocial determinants of health associated with uncontrolled diabetes in a federally qualified health center population. Diabetes Spectr. 2019;32(2):145–51.
Reichsman A, Werner J, Cella P, Bobiak S, Stange KC. Opportunities for improved diabetes care among patients of safety net practices: a safety net providers’ strategic alliance study. J Natl Med Assoc. 2009;101(1):4–11.
Reyes J, Tripp-Reimer T, Parker E, Muller B, Laroche H. Factors influencing diabetes self-management among medically underserved patients with type II diabetes. Glob Qual Nurs Res. 2017;4:2333393617713097.
Dao J, Spooner C, Lo W, Harris MF. Factors influencing self-management in patients with type 2 diabetes in general practice: a qualitative study. Aust J Prim Health. 2019;25(2):176–84.
Davis J, Fischl AH, Beck J, Browning L, Carter A, Condon JE, et al. 2022 national standards for diabetes self-management education and support. Diabetes Care. 2022;45(2):484–94.
Nagelkerk J, Reick K, Meengs L. Perceived barriers and effective strategies to diabetes self-management. J Adv Nurs. 2006;54(2):151–8.
Cooper HC, Booth K, Gill G. Patients’ perspectives on diabetes health care education. Health Educ Res. 2003;18(2):191–206.
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. Retinopathy, Neuropathy, and Foot Care: standards of Care in Diabetes-2023. Diabetes Care. 2023;12:203–15.
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 6. Glycemic targets: standards of care in diabetes-2023. Diabetes Care. 2023;46(Suppl 1):97–110.
Selvin E, Venkat Narayan KM, Huang ES. Quality of care in people with diabetes. National Institute of Diabetes and Digestive and Kidney Diseases; 2018.
Hill CV, Pérez-Stable EJ, Anderson NA, Bernard MA. The National Institute on aging Health disparities Research Framework. Ethn Dis. 2015;25(3):245–54.
Institute of Medicine (US). Committee on Monitoring Access to Personal Health Care Services, Millman M. A model for monitoring access. Washington, D.C., DC: National Academies Press; 1993.
National Academies of Sciences, Engineering, and, Medicine H, Division M, Board on Health Care Services, Committee on Ensuring Patient Access to Affordable Drug Therapies, Nass SJ, Madhavan G, et al. Factors influencing affordability. Washington, D.C., DC: National Academies Press; 2017.
Barros AJD, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3:21.
Bennett DA. How can I deal with missing data in my study? Aust N Z J Public Health. 2001;25(5):464–9.
Morkos M, Tahsin B, Fogelfeld L. Factors associated with diabetes control in predominately African American and hispanic population with newly diagnosed type 2 diabetes. J Racial Ethn Health Disparities. 2021;8(2):332–8.
American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: Standards of Medical Care in diabetes-2021. Diabetes Care. 2021;44(Suppl 1):S111–24.
Reaven PD, Emanuele NV, Wiitala WL, Bahn GD, Reda DJ, McCarren M, et al. Intensive glucose control in patients with type 2 diabetes– 15-year follow-up. N Engl J Med. 2019;380(23):2215–24.
Chapter 9: Sliding fee discount program. In: Health Resources & Services Administration. 2018. https://bphc.hrsa.gov/programrequirements/compliancemanual/chapter-9.html. Accessed Jun 24 2021.
Booth GL, Hux JE. Relationship between avoidable hospitalizations for diabetes mellitus and income level. Arch Intern Med. 2003;163(1):101–6.
Ji H, Chen R, Huang Y, Li W, Shi C, Zhou J. Effect of simulation education and case management on glycemic control in type 2 diabetes. Diabetes Metab Res Rev. 2019;35(3):e3112.
Powers MA, Bardsley JK, Cypress M. Diabetes self-management education and support in adults with type 2 diabetes: a consensus report of the American Diabetes Association, the Association of Diabetes, Care Education specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the. Diabetes Care. 2020;43(7). https://doi.org/10.2337/dci20-0023.
Strawbridge LM, Lloyd JT, Meadow A, Riley GF, Howell BL. One-year outcomes of diabetes self-management training among Medicare beneficiaries newly diagnosed with diabetes. Med Care. 2017 =;55(4):391–7.
Chrvala CA, Sherr D, Lipman RD. Diabetes self-management education for adults with type 2 diabetes mellitus: a systematic review of the effect on glycemic control. Patient Educ Couns. 2016;99(6):926–43.
Morgan JM, Mensa-Wilmot Y, Bowen S-A, Murphy M, Bonner T, Rutledge S, et al. Implementing key drivers for diabetes self-management education and support programs: early outcomes, activities, facilitators, and barriers. Prev Chronic Dis. 2018;15(170399). https://doi.org/10.5888/pcd15.170399.
Toulouse C, Kodadek M. Continuous access to medication and health outcomes in uninsured adults with type 2 diabetes. J Am Assoc Nurse Pract. 2016;28(6):327–34.
Shi L, Lee D-C, Haile GP, Liang H, Chung M, Sripipatana A. Access to care and satisfaction among health center patients with chronic conditions. J Ambul Care Manage. 2017;40(1):69–76.
Shepherd JG, Locke E, Zhang Q, Maihafer G. Health services use and prescription access among uninsured patients managing chronic diseases. J Community Health. 2014;39(3):572–83.
Goins RT, Williams KA, Carter MW, Spencer M, Solovieva T. Perceived barriers to health care access among rural older adults: a qualitative study. J Rural Health. 2005;21(3):206–13.
American Diabetes Association. 11. Microvascular complications and foot care: Standards of Medical Care in diabetes-2021. Diabetes Care. 2021;44(Suppl 1):S151–67.
Skrepnek GH, Mills JL, Sr, Lavery LA, Armstrong DG. Health care service and outcomes among an estimated 6.7 million ambulatory care diabetic foot cases in the U.S. Diabetes Care. 2017;40(7):936–42.
Dai M, Peabody MR, Peterson LE, Mainous AG III. Adherence to clinical guidelines for monitoring diabetes in primary care settings. Fam Med Community Health. 2018;6(4):161–7.
Imai C, Li L, Hardie R-A, Georgiou A. Adherence to guideline-recommended HbA1c testing frequency and better outcomes in patients with type 2 diabetes: a 5-year retrospective cohort study in Australian general practice. BMJ Qual Saf. 2021;30(9):706–14.
Lian J, Liang Y. Diabetes management in the real world and the impact of adherence to guideline recommendations. Curr Med Res Opin. 2014;30(11):2233–40.
Wasserman J, Boyce-Smith G, Hopkins DS, Schabert V, Davidson MB, Ozminkowski RJ, et al. A comparison of diabetes patient’s self-reported health status with hemoglobin A1c test results in 11 California health plans. Manag Care. 2001;10(3):58–62. 65–8, 70.
Short ME, Goetzel RZ, Pei X, Tabrizi MJ, Ozminkowski RJ, Gibson TB, et al. How accurate are self-reports? Analysis of self-reported health care utilization and absence when compared with administrative data. J Occup Environ Med. 2009;51(7):786–96.
Kjellsson G, Clarke P, Gerdtham U-G. Forgetting to remember or remembering to forget: a study of the recall period length in health care survey questions. J Health Econ. 2014;35:34–46.
Acknowledgements
Dr. Ali was supported by the University of Wisconsin Primary Care Research Fellowship, funded by grant T32HP10010 from the Health Resources and Services Administration.
The authors gratefully acknowledge Dr. Mindy Smith for the insightful comments of the manuscript.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
Drs. Ali and Young contributed to the conception and design of the study and data acquisition. Dr. Ali conducted the data cleaning, analysis, and interpretation, and wrote the initial draft of the manuscript. Drs. Young and Cobran provided statistical expertise and critically reviewed the manuscript for important intellectual content. All authors approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Deidentified publicly available data was used. So, no informed consent was needed or obtained.
Competing interests
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ali, A.M., Cobran, E.K. & Young, H.N. Individual, interpersonal, and community factors associated with health outcomes in patients with type 2 diabetes mellitus treated at federally qualified health centers. J Diabetes Metab Disord (2024). https://doi.org/10.1007/s40200-024-01388-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40200-024-01388-5