Abstract
Background
This study characterizes factors affecting glycemic control in a predominately African American and Hispanic population with newly diagnosed type 2 diabetes (T2DM).
Methods
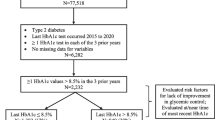
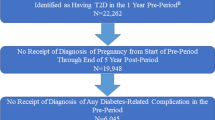
Retrospective longitudinal cohort study of 1638 patients with newly diagnosed T2DM to determine factors associated with improved HbA1c (ΔHbA1c ≤ − 0.5%) and achieving target HbA1c < 7%.
Results
At baseline, mean age 51.7 ± 11.5 years, males 52.9%, mean BMI 33.9 ± 7.8 kg/m2, median HbA1c 9.9 (7.6–12.1)%. At study end, median follow-up duration 27 (13–54) months, median HbA1c 7.0 (6.2–8.7)%, 69.6% with improved HbA1c, 48.3% achieved target HbA1c < 7%, 88.4% monitored blood glucose, 40.1% used insulin, and 72.4% reported not missing medications. In multivariate analysis, improved HbA1c significantly correlated with glucose monitoring (OR = 2.65), higher initial HbA1c (OR = 1.85), and medication adherence (OR = 1.66) and inversely correlated with insulin use (OR = 0.38) and follow-up duration (OR = 0.99). Achieving HbA1c < 7% significantly correlated with glucose monitoring (OR = 2.14), medication adherence (OR = 1.88), more provider visits (OR = 1.04), and older age (OR = 1.03). It inversely correlated with insulin use (OR = 0.47), initial HbA1c (OR = 0.93), and follow-up duration (OR = 0.98).
Conclusions
In those with newly diagnosed T2DM, achieving better glycemic control was mainly related to patient self-management behaviors and inversely related to insulin use. Emphasis on patients’ diabetes education and empowerment are critical to improved glycemic control.


Similar content being viewed by others
References
Centers for Disease Control and Prevention. National diabetes statistics report: estimates of diabetes and its burden in the United States, 2017. Atlanta: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2017.
Baicker K, Taubman SL, Allen HL, Bernstein M, Gruber JH, Newhouse JP, et al. The Oregon experiment—effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368:1713–22.
Berkowitz SA, Meigs JB, DeWalt D, Seligman HK, Barnard LS, Bright OJM, et al. Material need insecurities, control of diabetes mellitus, and use of health care resources: results of the Measuring Economic Insecurity in Diabetes study. JAMA Intern Med. 2015;175:257–65.
Golden SH, Brown A, Cauley JA, Chin MH, Gary-Webb TL, Kim C, et al. Health disparities in endocrine disorders: biological, clinical, and nonclinical factors—an Endocrine Society scientific statement. JCEM. 2012;97:E1579.
Philis-Tsimikas A, Walker C. Improved care for diabetes in underserved populations. J Ambul Care Manage. 2001;24:39–43.
Morkos M, Tahsin B, Fogg L, Fogelfeld L. Newly diagnosed type 2 diabetes in an ethnic minority population: clinical presentation and comparison to other populations. BMJ Open Diabetes Res Care. 2018 Oct 11;6(1):e000568.
UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352:837–53.
Diabetes Control and Complications Trial Research Group, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–86.
Action to Control Cardiovascular Risk in Diabetes Study Group, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545–59.
Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360:129–39.
Currie CJ, Peters JR, Tynan A, Evans M, Heine RJ, Bracco OL, et al. Survival as a function of HbA1c in people with type 2 diabetes: a retrospective cohort study. Lancet. 2010;375:481–9.
Dluhy RG, McMahon GT. Intensive glycemic control in the ACCORD and ADVANCE trials. N Engl J Med. 2008;358(24):2630–3.
American Diabetes Association. 6. Glycemic targets: standards of medical care in diabetes—2019. Diabetes Care. 2019;42(Suppl 1):S61–70.
American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes—2019. Diabetes Care. 2019;42(Suppl 1):S13–28.
Guerci B, Drouin P, Grange V, et al. Self-monitoring of blood glucose significantly improves metabolic control in patients with type 2 diabetes mellitus: the Auto-Surveillance Intervention Active (ASIA) study. Diabetes Metab. 2003;29:587–94.
Norris SL, Engelgau MM, Narayan KV. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. 2001;24:561–87.
Berikai P, Meyer PM, Kazlauskaite R, Savoy B, Kozik K, Fogelfeld L. Gain in patients' knowledge of diabetes management targets is associated with better glycemic control. Diabetes Care. 2007;30:1587–9.
Koro CE, Bowlin SJ, Bourgeois N, Fedder DO. Glycemic control from 1988 to 2000 among US adults diagnosed with type 2 diabetes: a preliminary report. Diabetes Care. 2004;27:17–20.
El-Kebbi IM, Cook CB, Ziemer DC, et al. Association of younger age with poor glycemic control and obesity in urban African Americans with type 2 diabetes. Arch Intern Med. 2003;163:69–75.
Halban PA, Polonsky KS, Bowden DW, Hawkins MA, Ling C, Mather KJ, et al. β-Cell failure in type 2 diabetes: postulated mechanisms and prospects for prevention and treatment. JCEM. 2014;99(6):1983–92.
Author information
Authors and Affiliations
Contributions
Michael Morkos: Conceptualization, methodology, formal analysis, investigation, writing—original draft, writing—review and editing, visualization. Bettina Tahsin: formal analysis, data curation, writing—review and editing, visualization. Leon Fogelfeld: conceptualization, methodology, formal analysis, data curation, writing—review and editing, visualization, supervision, project administration.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Morkos, M., Tahsin, B. & Fogelfeld, L. Factors Associated with Diabetes Control in Predominately African American and Hispanic Population with Newly Diagnosed Type 2 Diabetes. J. Racial and Ethnic Health Disparities 8, 332–338 (2021). https://doi.org/10.1007/s40615-020-00785-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-020-00785-9