Abstract
Purpose
Sofosbuvir, a nucleotide antiviral drug, is a Biopharmaceutics Classification System (BCS) class III prodrug suffering from limited intestinal absorption due to its high hydrophilicity and low intestinal permeability. This research aims to investigate the luminal stability of Sofosbuvir, the influence of anatomical site on its intestinal absorption and the effects of verapamil on such absorption.
Method
The study utilized in situ rabbit intestinal perfusion technique to examine absorption of Sofosbuvir from duodenum, jejunum, ileum and ascending colon. This was conducted both with and without verapamil.
Results
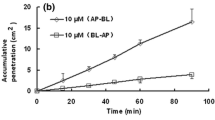
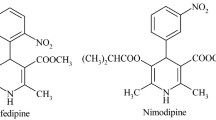
The luminal stability study showed that Sofosbuvir was subjected to premature degradation with varying fractions degraded from the different intestinal segments. The in situ perfusion data showed incomplete absorption of Sofosbuvir from small and large intestinal segments. The recorded values of the absorptive clearance per unit length (Pe.A/L) of Sofosbuvir were 0.026, 0.0075, 0.0026, & 0.054 ml/min.cm for duodenum, jejunum, ileum, and ascending colon, respectively. The Pe.A/L values were ordered as colon > duodenum > jejunum > ileum. This is the opposite rank of P-gp content in the different intestinal segments. The recorded values of the length required for complete Sofosbuvir absorption (L95%) were 29.58, 128.47, 949.2 and, 13.63 cm for duodenum, jejunum, ileum, and ascending colon, respectively. Co-perfusion with verapamil significantly increased Pe.A/L and reduced the L95% of Sofosbuvir from both jejunum and ileum (P-value < 0.05).
Conclusion
The results indicated that the absorptive clearance of Sofosbuvir was site dependent and associated with the content of P-glycoprotein, in addition to the expected drug interactions that can occur in polymedicated hepatitis C virus (HCV) infected patients.
Graphical abstract





Similar content being viewed by others
Data availability
All authors are sure that all data and materials support our published claims and comply with field standards. And all listed authors have approved the manuscript before submission, including the names and order of authors.
Ethical approval.
Animal handling and the study treatments were performed according to the permission of the Ethical Committee of College of Pharmacy, Tanta University (Approval number, 108017).
References
Asselah T. Sofosbuvir for the treatment of hepatitis C virus. Expert Opin Pharmacother. 2014;15(1):121–30.
Mehmood Y, Khan IU, Shahzad Y, Khan RU, Khalid SH, Yousaf AM, et al. Amino-decorated mesoporous silica nanoparticles for controlled sofosbuvir delivery. Eur J Pharm Sci [Internet]. 2020;143:105184. Available from: https://doi.org/10.1016/j.ejps.2019.105184
Kirby BJ, Symonds WT, Kearney BP, Mathias AA. Pharmacokinetic, Pharmacodynamic, and Drug-Interaction Profile of the Hepatitis C Virus NS5B Polymerase Inhibitor Sofosbuvir. Clin Pharmacokinet [Internet]. 2015 54(7):677–90. Available from: https://doi.org/10.1007/s40262-015-0261-7
Murakami E, Tolstykh T, Bao H, Niu C, Micolochick Steuer HM, Bao D, et al. Mechanism of activation of PSI-7851 and its diastereoisomer PSI-7977. J Biol Chem. 2010;285(45):34337–47.
Cada DJ, Cong J, Baker DE. Formulary drug reviews: Sofosbuvir. Hosp Pharm. 2014;49(5):466–78.
Gritsenko D, Hughes G. Ledipasvir/Sofosbuvir (harvoni): improving options for hepatitis C virus infection. P T. 2015 40(4):256-76
Takano M, Yumoto R, Murakami T. Expression and function of efflux drug transporters in the intestine. Pharmacol Ther. 2006;109(1–2):137–61.
Zhang H, Ya G, Rui H. Inhibitory Effects of Triptolide on Human Liver Cytochrome P450 Enzymes and P-Glycoprotein. Eur J Drug Metab Pharmacokinet. 2017;42(1):89–98.
Dahlgren D, Lennernäs H. Intestinal permeability and drug absorption: predictive experimental, computational and in vivo approaches. Vol. 11, Pharmaceutics. MDPI AG; 2019.
Mollazadeh S, Sahebkar A, Hadizadeh F, Behravan J, Arabzadeh S. Structural and functional aspects of P-glycoprotein and its inhibitors. Vol. 214, Life Sciences. Elsevier Inc.; 2018. 118–23.
Lozoya-Agullo I, González-Álvarez I, González-Álvarez M, Merino-Sanjuán M, Bermejo M. In Situ Perfusion Model in Rat Colon for Drug Absorption Studies: Comparison with Small Intestine and Caco-2 Cell Model. J Pharm Sci. 2015;104(9):3136–45.
Zhang Y, Bachmeier C, Miller DW. In vitro and in vivo models for assessing drug efflux transporter activity. Adv Drug Deliv Rev. 2003;55(1):31–51. https://doi.org/10.1016/s0169-409x(02)00170-9.
Ashmawy SM, Osman MA, El-Gizawy SA, El Maghraby GM. D-glucose elicits significant increase in the oral bioavailability of model BCS class III drugs in the rabbit. J Drug Deliv Sci Technol [Internet]. 2019;49(November 2018):521–6. Available from: https://doi.org/10.1016/j.jddst.2018.12.025
Stephens RH, Tanianis-Hughes J, Higgs NB, Humphrey M, Warhurst G. Region-dependent modulation of intestinal permeability by drug efflux transporters: In vitro studies in mdr1a(-/-) mouse intestine. J Pharmacol Exp Ther. 2002;303(3):1095–101.
Mouly S, Paine MF. P-Glycoprotein Increases from Proximal to Distal Regions of Human Small Intestine. Pharm Res. 2003;20(10):1595–9.
Ashmawy SM, El-Gizawy SA, El Maghraby GM, Osman MA. Regional difference in intestinal drug absorption as a measure for the potential effect of P-glycoprotein efflux transporters. J Pharm Pharmacol. 2019;71(3):362–70.
Liu CH, Su TH, Liu CJ, Hong CM, Yang HC, Tseng TC, et al. Sofosbuvir-based direct acting antiviral therapies for patients with hepatitis C virus genotype 2 infection. J Gastroenterol Hepatol. 2019;34(9):1620–5.
Tang H, Pak Y, Mayersohn M. Protein expression pattern of P-glycoprotein along the gastrointestinal tract of the Yucatan micropig. J Biochem Mol Toxicol. 2004;18(1):18–22.
Riad L, Sawchuk R. Absorptive clearance of carbamazepine and selected metabolites in rabbit intes-tine. Pharm Res. 1991;8:1050–5.
Osman MA, El Maghraby GM, Hedaya MA. Intestinal absorption and presystemic disposition of sildenafil citrate in the rabbit: Evidence for site-dependent absorptive clearance. Biopharm Drug Dispos. 2006;27(2):93–102.
Sultan AA, El-Gizawy SA, Osman MA, El Maghraby GM. Colloidal carriers for extended absorption window of furosemide. J Pharm Pharmacol. 2016;68(3):324–32.
Amidon GE, Ho NF, French AB, Higuchi WI. Predicted absorption rates with simultaneous bulk fluid flow in the intestinal tract. J Theor Biol. 1981;89(2):195–210. https://doi.org/10.1016/0022-5193(81)90306-4.
Komiya I, Park JY, Kamani A, Ho NFH, Higuchi WI. Quantitative mechanistic studies in simultaneous fluid flow and intestinal absorption using steroids as model solutes. Int J Pharm [Internet]. 1980 4(3):249–62. Available from: https://linkinghub.elsevier.com/retrieve/pii/0378517380901404. Accessed Oct 2021.
Osman M., El Maghraby GM, Hedaya MA. Intestinal absorption and presystemic disposition of sildenafil citrate in the rabbit: evidence for site-dependent absorptive clearance. Biopharm Drug Dispos [Internet]. 2006 27(2):93–102. Available from: http://doi.wiley.com/https://doi.org/10.1002/bdd.487
Lifson N, Gruman L, Levitt D. Diffusive-convective models for intestinal absorption of D2O. Am J Physiol Content [Internet]. 1968 215(2):444–54. Available from: https://www.physiology.org/doi/https://doi.org/10.1152/ajplegacy.1968.215.2.444
Lifson N, Hakim A. Simple diffusive-convective model for intestinal absorption of a nonelectrolyte (urea). Am J Physiol Content [Internet]. 1966 211(5):1137–46. Available from: https://www.physiology.org/doi/https://doi.org/10.1152/ajplegacy.1966.211.5.1137
Loehry CA, Kingham J, Baker J. Small intestinal permeability in animals and man. Gut. 1973;14(9):683–8.
Maeda T, Takenaka H, Yamahira Y, Noguchi T. Use of rabbits for GI drug absorption studies. J Pharm Sci. 1977;66(1):69–73.
Shen Y. CES Involved Inhibition and Regulation. Open Access Dissertations. 2017. Available from: https://digitalcommons.uri.edu/oa_diss/656. Accessed June 2021.
Amin ML. P-glycoprotein Inhibition for Optimal Drug Delivery. Drug Target Insights. 2013;7:27–34. https://doi.org/10.4137/DTI.S12519.
Brooks KM, Castillo-Mancilla JR, Blum J, Huntley R, MaWhinney S, Alexander K, et al. Increased tenofovir monoester concentrations in patients receiving tenofovir disoproxil fumarate with ledipasvir/sofosbuvir. J Antimicrob Chemother. 2019;74(8):2360–4.
Ishimine M, Yokomizo T, Lee-Okada H-C. Carboxylesterase 2: A Key Enzyme in Drug and Prodrug Metabolism. Juntendo Med J. 2020;66(2):120–4.
Taketani M, Shii M, Ohura K, Ninomiya S, Imai T. Carboxylesterase in the liver and small intestine of experimental animals and human. Life Sci. 2007;81(11):924–32.
Liu D, Gao J, Zhang C, Ren X, Liu Y, Xu Y. Identification of carboxylesterases expressed in rat intestine and effects of their hydrolyzing activity in predicting first-pass metabolism of ester prodrugs. Pharmazie. 2011;66(11):888–93.
Ishizaki Y, Furihata T, Oyama Y, Ohura K, Imai T, Hosokawa M, et al. Development of a Caco-2 cell line carrying the human intestine-type ces expression profile as a promising tool for ester-containing drug permeability studies. Biol Pharm Bull. 2018;41(5):697–706.
Satoh T, Hosokawa M. Structure, function and regulation of carboxylesterases. Chem Biol Interact. 2006;162(3):195–211.
Imai T. Human carboxylesterase isozymes: catalytic properties and rational drug design. Drug Metab Pharmacokinet. 2006;21(3):173–85.
Khanna R, Morton CL, Danks MK, Potter PM. Proficient metabolism of irinotecan by a human intestinal carboxylesterase. Cancer Res. 2000;60(17):4725–8.
Satoh T, Taylor P, Bosron WF, Sanghani SP, Hosokawa M, La Du BN. Current progress on esterases: From molecular structure to function. Drug Metab Dispos. 2002;30(5):488–93.
Mudie DM, Murray K, Hoad CL, Pritchard SE, Garnett MC, Amidon GL, et al. Quantification of gastrointestinal liquid volumes and distribution following a 240 mL dose of water in the fasted state. Mol Pharm. 2014;11(9):3039–47.
Tanaka Y, Goto T, Kataoka M, Sakuma S, Yamashita S. Impact of Luminal Fluid Volume on the Drug Absorption After Oral Administration: Analysis Based on In Vivo Drug Concentration-Time Profile in the Gastrointestinal Tract. J Pharm Sci. 2015;104(9):3120–7. https://doi.org/10.1002/jps.24433.
Schiller C, Fröhlich CP, Giessmann T, Siegmund W, Mönnikes H, Hosten N, et al. Intestinal fluid volumes and transit of dosage forms as assessed by magnetic resonance imaging. Aliment Pharmacol Ther. 2005;15;22(10):971–9. doi: https://doi.org/10.1111/j.1365-2036.2005.02683.x.
Magee DF, Dally II. Digestion and the Structure and Function of The Gut. Karger Continuing Education Series. 1986;Vol. 8. ISBN: 978–3–8055–4204–3.
Pang KS. Modeling of intestinal drug absorption: Roles of transporters and metabolic enzymes (for the gillette review series). Drug Metab Dispos. 2003;31(12):1507–19.
Levitan R, Fordtran JS, Burrows BA, Ingelfinger FJ. Water and salt absorption in the human colon. J Clin Invest. 1962;41(9):1754–9.
Lückhoff A, Horster M. Hormonal regulation of electrolyte and water transport in the Colon. Klin Wochenschr. 1984;62(12):555–63.
Sandle GI. Salt and water absorption in the human colon: A modern appraisal. Gut. 1998;43(2):294–9.
Kunzelmann K, Mall M. Electrolyte transport in the mammalian colon: Mechanisms and implications for disease. Physiol Rev. 2002;82(1):245–89.
Ayrton A, Morgan P. Role of transport proteins in drug absorption, distribution and excretion. Xenobiotica. 2001;31(8–9):469–97.
Bergson P, Lipkind G, Lee SP, Duban ME, Hanck DA. Verapamil block of T-type calcium channels. Mol Pharmacol. 2011;79(3):411–9.
Jouan E, Le Vée M, Mayati A, Denizot C, Parmentier Y, Fardel O. Evaluation of P-Glycoprotein Inhibitory Potential Using a Rhodamine 123 Accumulation Assay. Pharmaceutics. 2016;8(2):12. https://doi.org/10.3390/pharmaceutics8020012.
Zhu T, Howieson C, Wojtkowski T, Garg JP, Han D, Fisniku O, et al. The Effect of Verapamil, a P-Glycoprotein Inhibitor, on the Pharmacokinetics of Peficitinib, an Orally Administered, Once-Daily JAK Inhibitor. Clin Pharmacol Drug Dev. 2017;6(6):548–55.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Nada M. Mohsen: Investigation, Data curation and Writing drafted manuscript. Esmat E. Zein El-Din: Visualization, Supervision, Writing, Reviewing and Editing. Mohamed A. Osman: Conceptualization, Methodology, Data curation, Visualization and Supervision. Shimaa M. Ashmawy: Data Curation, Visualization, Writing, Reviewing and Editing.
Corresponding author
Ethics declarations
Conflicts of interest/Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mohsen, N.M., El-Din, E.E.Z., Osman, M.A. et al. Investigation of the effect of verapamil on the regional absorption of sofosbuvir from rabbit intestine in situ. DARU J Pharm Sci 30, 49–58 (2022). https://doi.org/10.1007/s40199-021-00429-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40199-021-00429-1