Abstract
Purpose of Review
Massive blood loss secondary to major trauma is a leading cause of death worldwide. In recent years, multiple different strategies have evolved to counteract this life-threatening condition. In this review, we will review our understanding of trauma-induced coagulopathy and summarize current clinical transfusion regimes utilized in military and civilian settings. We will review currently available blood products used to rectify the coherent disturbances of haemostasis by outlining the characteristics of the different products.
Recent Findings
Current evidence suggests that fresh frozen plasma and fibrinogen components play a fundamental role in trauma resuscitation with recent studies suggesting pre-hospital plasma and fibrinogen administration might also be beneficial in counteracting trauma-induced coagulopathy. Based on experience out of combat zones, whole blood transfusion might experience a renaissance in the future.
Summary
Multiple different plasma-based products are available to treat and prevent trauma-induced coagulation disturbances. As randomized controlled trials in trauma population are difficult to conduct, most of the evidence is currently based on relatively small studies. While the overarching result of our review suggests the early use of plasma and fibrinogen products in combination with packed red blood cells will prevent trauma-induced coagulopathy, large, multi-centre studies are warranted to evaluate the long-term effects on patients’ outcome.

Similar content being viewed by others
Abbreviations
- aPC:
-
Activated protein C
- aPTT:
-
Activated partial thromboplastin time
- ARC:
-
American Red Cross
- ATC:
-
Acute traumatic coagulopathy
- FC:
-
Fibrinogen concentrate
- FDA:
-
US Food and Drug Administration
- FDP:
-
Freeze-dried human plasma
- FFP:
-
Fresh frozen plasma
- FLyP:
-
French lyophilised plasma
- FVIII:
-
Coagulation factor VIII
- FWB:
-
Fresh whole blood
- ISS:
-
Injury severity score
- LP:
-
Lyophilised plasma
- LTOWB:
-
Low-titre group O whole blood
- PCC:
-
Prothrombin complex concentrate
- PRBC:
-
Packed red blood cell
- PT:
-
Prothrombin time
- PT:
-
prothrombin time
- tPA:
-
Tissue plasminogen activator
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Borgman MA, Spinella PC, Perkins JG, Grathwohl KW, Repine T, Beekley AC, et al. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. J Trauma. 2007;63:805–13.
Spinella PC, Perkins JG, Grathwohl KW, Beekley AC, Niles SE, McLaughlin DF, et al. Effect of plasma and red blood cell transfusions on survival in patients with combat related traumatic injuries. J Trauma. 2008;64:S69–77 discussion S77.
Holcomb JB, Wade CE, Michalek JE, Chisholm GB, Zarzabal LA, Schreiber MA, et al. Increased plasma and platelet to red blood cell ratios improves outcome in 466 massively transfused civilian trauma patients. Ann Surg. 2008;248:447–58.
Shackelford SA, Del Junco DJ, Powell-Dunford N, Mazuchowski EL, Howard JT, Kotwal RS, et al. Association of pPrehospital bBlood pProduct tTransfusion dDuring mMedical eEvacuation of cCombat cCasualties in Afghanistan wWith aAcute and 30-dDay sSurvival. JAMA. 2017;318:1581–91.
Holcomb JB, Tilley BC, Baraniuk S, Fox EE, Wade CE, Podbielski JM, et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA. 2015;313:471–82.
• Spahn DR, Bouillon B, Cerny V, Duranteau J, Filipescu D, Hunt BJ, et al. The European guideline on management of major bleeding and coagulopathy following trauma: fifth edition. Crit Care. 2019;23:98 This manuscript summarized the current guidelines for resuscitation and provides a clear overview of the state-of-the-art treatment strategies.
Cannon JW, Khan MA, Raja AS, Cohen MJ, Como JJ, Cotton BA, et al. Damage control resuscitation in patients with severe traumatic hemorrhage: aA practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2017;82:605–17.
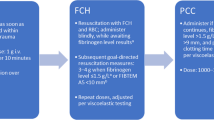
Innerhofer P, Fries D, Mittermayr M, Innerhofer N, von Langen D, Hell T, et al. Reversal of trauma-induced coagulopathy using first-line coagulation factor concentrates or fresh frozen plasma (RETIC): a single-centre, parallel-group, open-label, randomised trial. Lancet Haematol. 2017;4:e258–71.
McQuilten ZK, Wood EM, Bailey M, Cameron PA, Cooper DJ. Fibrinogen is an independent predictor of mortality in major trauma patients: aA five-year statewide cohort study. Injury. 2017;48:1074–81.
Rourke C, Curry N, Khan S, Taylor R, Raza I, Davenport R, et al. Fibrinogen levels during trauma hemorrhage, response to replacement therapy, and association with patient outcomes. J Thromb Haemost. 2012;10:1342–51.
Nardi G, Agostini V, Rondinelli B, Russo E, Bastianini B, Bini G, et al. Trauma induced coagulopathy: impact of the early coagulation support protocol on blood product consumption, mortality and costs. Crit Care. 2015;19:817.
Leeper CM, Strotmeyer SJ, Neal MD, Gaines BA. Window of oOpportunity to mMitigate tTrauma-induced cCoagulopathy: fFibrinolysis sShutdown not pPrevalent uUntil 1 hHour pPost-injury. Ann Surg. 2019;270:528–34.
Gall LS, Davenport RA. Fibrinolysis and antifibrinolytic treatment in the trauma patient. Curr Opin Anaesthesiol. 2018;31:227–33.
Gando S, Mayumi T, Ukai T. The roles of activated protein C in experimental trauma models. Chin J Traumatol. 2018;21:311–5.
Davenport R. Pathogenesis of acute traumatic coagulopathy. Transfusion. 2013;53(Suppl 1):23S–7S.
van Zyl N, Milford EM, Diab S, Dunster K, McGiffin P, Rayner SG, et al. Activation of the protein C pathway and endothelial glycocalyx shedding is associated with coagulopathy in an ovine model of trauma and hemorrhage. J Trauma Acute Care Surg. 2016;81:674–84.
Spinella PC, Cap AP. Whole blood: back to the future. Curr Opin Hematol. 2016;23:536–42.
Roberts I, Shakur H, Coats T, Hunt B, Balogun E, Barnetson L, et al. The CRASH-2 trial: a randomised controlled trial and economic evaluation of the effects of tranexamic acid on death, vascular occlusive events and transfusion requirement in bleeding trauma patients. Health Technol Assess. 2013;17:1–79.
Simmons RL, Collins JA, Heisterkamp CA, Mills DE, Andren R, Phillips LL. Coagulation disorders in combat casualties. I. Acute changes after wounding. II. Effects of massive transfusion. 3. Post-resuscitative changes. Ann. Surg. 1969;169:455–82.
Kushimoto S, Kudo D, Kawazoe Y. Acute traumatic coagulopathy and trauma-induced coagulopathy: an overview. J Intensive Care. 2017;5:6.
Brohi K, Singh J, Heron M, Coats T. Acute traumatic coagulopathy. J Trauma. 2003;54:1127–30.
MacLeod JBA, Lynn M, McKenney MG, Cohn SM, Murtha M. Early coagulopathy predicts mortality in trauma. J Trauma. 2003;55:39–44.
Maegele M, Lefering R, Yucel N, Tjardes T, Rixen D, Paffrath T, et al. Early coagulopathy in multiple injury: an analysis from the German Trauma Registry on 8724 patients. Injury. 2007;38:298–304.
Plotkin AJ, Wade CE, Jenkins DH, Smith KA, Noe JC, Park MS, et al. A reduction in clot formation rate and strength assessed by thrombelastography is indicative of transfusion requirements in patients with penetrating injuries. J Trauma. 2008;64:S64–8.
Carroll RC, Craft RM, Langdon RJ, Clanton CR, Snider CC, Wellons DD, et al. Early evaluation of acute traumatic coagulopathy by thrombelastography. Transl Res. 2009;154:34–9.
Doran CM, Woolley T, Midwinter MJ. Feasibility of using rotational thromboelastometry to assess coagulation status of combat casualties in a deployed setting. J Trauma. 2010;69(Suppl 1):S40–8.
Thorn S, Lefering R, Maegele M, Gruen RL, Mitra B. Early prediction of acute traumatic coagulopathy: a validation of the COAST score using the German Trauma Registry. Eur J Trauma Emerg Surg. 2019.
Curry NS, Davenport RA, Hunt BJ, Stanworth SJ. Transfusion strategies for traumatic coagulopathy. Blood Rev. 2012;26:223–32.
Rizoli SB, Scarpelini S, Callum J, Nascimento B, Mann KG, Pinto R, et al. Clotting factor deficiency in early trauma-associated coagulopathy. J Trauma. 2011;71:S427–34.
Floccard B, Rugeri L, Faure A, Saint Denis M, Boyle EM, Peguet O, et al. Early coagulopathy in trauma patients: an on-scene and hospital admission study. Injury. 2012;43:26–32.
Brohi K, Cohen MJ, Ganter MT, Schultz MJ, Levi M, Mackersie RC, et al. Acute coagulopathy of trauma: hypoperfusion induces systemic anticoagulation and hyperfibrinolysis. J Trauma. 2008;64:1211–7 discussion 1217.
Gruen RL, Brohi K, Schreiber M, Balogh ZJ, Pitt V, Narayan M, et al. Haemorrhage control in severely injured patients. Lancet. 2012;380:1099–108.
Johansson PI, Stensballe J, Rasmussen LS, Ostrowski SR. A high admission syndecan-1 level, a marker of endothelial glycocalyx degradation, is associated with inflammation, protein C depletion, fibrinolysis, and increased mortality in trauma patients. Ann Surg. 2011;254:194–200.
Brohi K, Cohen MJ, Ganter MT, Matthay MA, Mackersie RC, Pittet J-F. Acute traumatic coagulopathy: initiated by hypoperfusion: modulated through the protein C pathway? Ann Surg. 2007;245:812–8.
Niles SE, McLaughlin DF, Perkins JG, Wade CE, Li Y, Spinella PC, et al. Increased mortality associated with the early coagulopathy of trauma in combat casualties. J Trauma. 2008;64:1459–63 discussion 1463.
Frith D, Cohen MJ, Brohi K. Animal models of trauma-induced coagulopathy. Thromb Res. 2012;129:551–6.
Frith D, Brohi K. The pathophysiology of trauma-induced coagulopathy. Curr Opin Crit Care. 2012;18:631–6.
Cohen MJ, Kutcher M, Redick B, Nelson M, Call M, Knudson MM, et al. Clinical and mechanistic drivers of acute traumatic coagulopathy. J Trauma Acute Care Surg. 2013;75:S40–7.
Cohen MJ, Call M, Nelson M, Calfee CS, Esmon CT, Brohi K, et al. Critical role of activated protein C in early coagulopathy and later organ failure, infection and death in trauma patients. Ann Surg. 2012;255:379–85.
Chesebro BB, Rahn P, Carles M, Esmon CT, Xu J, Brohi K, et al. Increase in activated protein C mediates acute traumatic coagulopathy in mice. Shock. 2009;32:659–65.
Reitsma S, Slaaf DW, Vink H, van Zandvoort MAMJ. oude Egbrink MGA. The endothelial glycocalyx: composition, functions, and visualization. Pflugers Arch. 2007;454:345–59.
Pati S, Potter DR, Baimukanova G, Farrel DH, Holcomb JB, Schreiber MA. Modulating the endotheliopathy of trauma: fFactor concentrate versus fresh frozen plasma. J Trauma Acute Care Surg. 2016;80:576–84 discussion 584.
Naumann DN, Hazeldine J, Dinsdale RJ, Bishop JR, Midwinter MJ, Harrison P, et al. Endotheliopathy is associated with higher levels of cell-free DNA following major trauma: aA prospective observational study. PLoS One. 2017;12:e0189870.
Naumann DN, Hazeldine J, Davies DJ, Bishop J, Midwinter MJ, Belli A, et al. Endotheliopathy of tTrauma is an on-sScene pPhenomenon, and is aAssociated with mMultiple oOrgan dDysfunction sSyndrome: aA pProspective oObservational sStudy. Shock. 2018;49:420–8.
Johansson PI, Stensballe J, Ostrowski SR. Shock induced endotheliopathy (SHINE) in acute critical illness - a unifying pathophysiologic mechanism. Crit Care. 2017;21:25.
Annecke T, Fischer J, Hartmann H, Tschoep J, Rehm M, Conzen P, et al. Shedding of the coronary endothelial glycocalyx: effects of hypoxia/reoxygenation vs ischaemia/reperfusion. Br J Anaesth. 2011;107:679–86.
Nieuwdorp M, Meuwese MC, Mooij HL, van Lieshout MHP, Hayden A, Levi M, et al. Tumor necrosis factor-alpha inhibition protects against endotoxin-induced endothelial glycocalyx perturbation. Atherosclerosis. 2009;202:296–303.
Ostrowski SR, Henriksen HH, Stensballe J, Gybel-Brask M, Cardenas JC, Baer LA, et al. Sympathoadrenal activation and endotheliopathy are drivers of hypocoagulability and hyperfibrinolysis in trauma: aA prospective observational study of 404 severely injured patients. J Trauma Acute Care Surg. 2017;82:293–301.
•• Henriksen HH, McGarrity S, SigurÐardóttir RS, Nemkov T, D’Alessandro A, Palsson BO, et al. Metabolic sSystems aAnalysis of sShock-iInduced eEndotheliopathy (SHINE) in tTrauma: aA nNew rResearch pParadigm. Ann Surg. 2019; In this manuscript, the authors clearly describe 4 different, trauma- induced endotheliopathy phenotypes. This manuscript clearly suggests that trauma response is most likely driven by genetic components.
O’Shaughnessy DF, Atterbury C, Bolton Maggs P, Murphy M, Thomas D, Yates S, et al. Guidelines for the use of fresh-frozen plasma, cryoprecipitate and cryosupernatant. Br J Haematol. 2004;126:11–28.
Tholpady A, Monson J, Radovancevic R, Klein K, Bracey A. Analysis of prolonged storage on coagulation fFactor (F)V, FVII, and FVIII in thawed plasma: is it time to extend the expiration date beyond 5 days? Transfusion. 2013;53:645–50.
Chapman JF, Elliott C, Knowles SM, Milkins CE, Poole GD, Working Party of the British Committee for Standards in Haematology Blood Transfusion Task Force. Guidelines for compatibility procedures in blood transfusion laboratories. Transfus Med. 2004;14:59–73.
O’Brien SF, Yi Q-L, Fan W, Scalia V, Kleinman SH, Vamvakas EC. Current incidence and estimated residual risk of transfusion-transmitted infections in donations made to Canadian Blood Services. Transfusion. 2007;47:316–25.
Semple JW, Rebetz J, Kapur R. Transfusion-associated circulatory overload and transfusion-related acute lung injury. Blood. 2019;133:1840–53.
Maskens C, Downie H, Wendt A, Lima A, Merkley L, Lin Y, et al. Hospital-based transfusion error tracking from 2005 to 2010: identifying the key errors threatening patient transfusion safety. Transfusion. 2014;54:66–73 quiz 65.
Popovsky MA. Pulmonary consequences of transfusion: TRALI and TACO. Transfus Apher Sci. 2006;34:243–4.
Emerson CP, Ebert RV. A study of shock in battle casualties: measurements of the blood volume changes occurring in response to therapy. Ann Surg. 1945;122:745–72.
Stanworth SJ, Brunskill SJ, Hyde CJ, McClelland DBL, Murphy MF. Is fresh frozen plasma clinically effective? A systematic review of randomized controlled trials. Br J Haematol. 2004;126:139–52.
Watson GA, Sperry JL, Rosengart MR, Minei JP, Harbrecht BG, Moore EE, et al. Fresh frozen plasma is independently associated with a higher risk of multiple organ failure and acute respiratory distress syndrome. J Trauma. 2009;67:221–7 discussion 228.
Norda R, Knutson F, Berseus O, Akerblom O, Nilsson-Ekdahl K, Stegmayr B, et al. Unexpected effects of donor gender on the storage of liquid plasma. Vox Sang. 2007;93:223–8.
Rossaint R, Bouillon B, Cerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, et al. Management of bleeding following major trauma: an updated European guideline. Crit Care. 2010;14:R52.
British Committee for Standards in Haematology, Stainsby D, MacLennan S, Thomas D, Isaac J, Hamilton PJ. Guidelines on the management of massive blood loss. Br J Haematol. 2006;135:634–41.
Padhi S, Kemmis-Betty S, Rajesh S, Hill J, Murphy MF. Guideline Development Group. Blood Transfus: summary of NICE guidance BMJ. 2015;351:h5832.
Kanani AN, Hartshorn S. NICE clinical guideline NG39: Major trauma: assessment and initial management. Arch Dis Child Educ Pract Ed. 2017;102:20–3.
Iorio A, Basileo M, Marchesini E, Materazzi M, Marchesi M, Esposito A, et al. The good use of plasma. A critical analysis of five international guidelines. Blood Transfus. 2008;6:18–24.
American Society of Anesthesiologists Task Force on Perioperative Blood Transfusion and Adjuvant Therapies. Practice guidelines for perioperative blood transfusion and adjuvant therapies: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Blood Transfusion and Adjuvant Therapies. Anesthesiology. 2006;105:198–208.
Rossaint R, Bouillon B, Cerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, et al. The European guideline on management of major bleeding and coagulopathy following trauma: fourth edition. Crit Care. 2016;20:100.
Inaba K. Freeze-dried plasma. J Trauma. 2011;70:S57–8.
Oktavec WA, Smetana EJ. Lyophilized normal human plasma control in the prothrombin-time clotting test. Am J Clin Pathol. 1954;24:250.
Spoerke N, Zink K, Cho SD, Differding J, Muller P, Karahan A, et al. Lyophilized plasma for resuscitation in a swine model of severe injury. Arch Surg. 2009;144:829–34.
Shuja F, Shults C, Duggan M, Tabbara M, Butt MU, Fischer TH, et al. Development and testing of freeze-dried plasma for the treatment of trauma-associated coagulopathy. J Trauma. 2008;65:975–85.
Lee TH, Van PY, Spoerke NJ, Hamilton GJ, Cho SD, Watson K, et al. The use of lyophilized plasma in a severe multi-injury pig model. Transfusion. 2013;53(Suppl 1):72S–9S.
Hamilton GJ, Van PY, Differding JA, Kremenevskiy IV, Spoerke NJ, Sambasivan C, et al. Lyophilized plasma with ascorbic acid decreases inflammation in hemorrhagic shock. J Trauma. 2011;71:292–7 discussion 297.
Bux J, Dickhörner D, Scheel E. Quality of freeze-dried (lyophilized) quarantined single-donor plasma. Transfusion. 2013;53:3203–9.
Daban JL, Clapson P, Ausset S, Deshayes AV, Sailliol A. Freeze dried plasma: a French army specialty. Crit Care. 2010;14:412.
Martinaud C, Ausset S, Deshayes AV, Cauet A, Demazeau N, Sailliol A. Use of freeze-dried plasma in French intensive care unit in Afghanistan. J Trauma. 2011;71:1761–4 discussion 1764.
Patrick J, Cauet A, Deshayes AV, Demazeau N, Sailliol A, Ausset S. Clinical use of freeze dried plasma (FDP) in deployed operations: aAnalysis of 72 episodes of transfusion (ET): 6AP5-2. Eur J Anaesthesiol (EJA). 2011;28.
Shlaifer A, Siman-Tov M, Radomislensky I, Peleg K, Shina A, Baruch EN, et al. Prehospital administration of freeze-dried plasma, is it the solution for trauma casualties? J Trauma Acute Care Surg. 2017;83:675–82.
Nguyen C, Bordes J, Cungi P-J, Esnault P, Cardinale M, Mathais Q, et al. Use of French lyophilized plasma transfusion in severe trauma patients is associated with an early plasma transfusion and early transfusion ratio improvement. J Trauma Acute Care Surg. 2018;84:780–5.
Sunde GA, Vikenes B, Strandenes G, Flo K-C, Hervig TA, Kristoffersen EK, et al. Freeze dried plasma and fresh red blood cells for civilian prehospital hemorrhagic shock resuscitation. J Trauma Acute Care Surg. 2015;78:S26–30.
• Garrigue D, Godier A, Glacet A, Labreuche J, Kipnis E, Paris C, et al. French lyophilized plasma versus fresh frozen plasma for the initial management of trauma-induced coagulopathy: a randomized open-label trial. J Thromb Haemost. 2018;16:481–9 This study describes a comparison of the military- manufactured French lyophilized plasma (FLyP) with conventional fresh frozen plasma during early trauma resuscitation in a civilian patient population. Although only 47 patients were enrolled in this single-centre, open-label trial, the data clearly suggest that early transfusion of FLyP was more effective in correcting trauma- induced coagulopathy.
Schlimp CJ, Voelckel W, Inaba K, Maegele M, Ponschab M, Schöchl H. Estimation of plasma fibrinogen levels based on hemoglobin, base excess and Injury Severity Score upon emergency room admission. Crit Care. 2013;17:R137.
Rahe-Meyer N, Sørensen B. For: Fibrinogen concentrate for management of bleeding. J Thromb Haemost. 2011;9:1–5.
Fenger-Eriksen C, Jensen TM, Kristensen BS, Jensen KM, Tønnesen E, Ingerslev J, et al. Fibrinogen substitution improves whole blood clot firmness after dilution with hydroxyethyl starch in bleeding patients undergoing radical cystectomy: a randomized, placebo-controlled clinical trial. J Thromb Haemost. 2009;7:795–802.
Pereira A. Cryoprecipitate versus commercial fibrinogen concentrate in patients who occasionally require a therapeutic supply of fibrinogen: risk comparison in the case of an emerging transfusion-transmitted infection. Haematologica. 2007;92:846–9.
Theodoulou A, Berryman J, Nathwani A, Scully M. Comparison of cryoprecipitate with fibrinogen concentrate for acquired hypofibrinogenaemia. Transfus Apher Sci. 2012;46:159–62.
Danés AF, Cuenca LG, Bueno SR, Mendarte Barrenechea L, Ronsano JBM. Efficacy and tolerability of human fibrinogen concentrate administration to patients with acquired fibrinogen deficiency and active or in high-risk severe bleeding. Vox Sang. 2008;94:221–6.
Fenger-Eriksen C, Lindberg-Larsen M, Christensen AQ, Ingerslev J, Sørensen B. Fibrinogen concentrate substitution therapy in patients with massive haemorrhage and low plasma fibrinogen concentrations. Br J Anaesth. 2008;101:769–73.
Thorarinsdottir HR, Sigurbjornsson FT, Hreinsson K, Onundarson PT, Gudbjartsson T, Sigurdsson GH. Effects of fibrinogen concentrate administration during severe hemorrhage. Acta Anaesthesiol Scand. 2010;54:1077–82.
Schöchl H, Nienaber U, Hofer G, Voelckel W, Jambor C, Scharbert G, et al. Goal-directed coagulation management of major trauma patients using thromboelastometry (ROTEM)-guided administration of fibrinogen concentrate and prothrombin complex concentrate. Crit Care. 2010;14:R55.
Mengoli C, Franchini M, Marano G, Pupella S, Vaglio S, Marietta M, et al. The use of fibrinogen concentrate for the management of trauma-related bleeding: a systematic review and meta-analysis. Blood Transfus. 2017;15:318–24.
Nascimento B, Callum J, Tien H, Peng H, Rizoli S, Karanicolas P, et al. Fibrinogen in the initial resuscitation of severe trauma (FiiRST): a randomized feasibility trial. Br J Anaesth. 2016;117:775–82.
Yamamoto K, Yamaguchi A, Sawano M, Matsuda M, Anan M, Inokuchi K, et al. Pre-emptive administration of fibrinogen concentrate contributes to improved prognosis in patients with severe trauma. Trauma Surg Acute Care Open. 2016;1:e000037.
Itagaki Y, Hayakawa M, Maekawa K, Saito T, Kodate A, Honma Y, et al. Early administration of fibrinogen concentrate is associated with improved survival among severe trauma patients: a single-centre propensity score-matched analysis. World J Emerg Surg. 2020;15:7.
Hellstern P, Halbmayer WM, Köhler M, Seitz R, Müller-Berghaus G. Prothrombin complex concentrates: indications, contraindications, and risks: a task force summary. Thromb Res. 1999;95:S3–6.
Hellstern P. Production and composition of prothrombin complex concentrates: correlation between composition and therapeutic efficiency. Thromb Res. 1999;95:S7–12.
Schulman S, Bijsterveld NR. Anticoagulants and their reversal. Transfus Med Rev. 2007;21:37–48.
Dickneite G, Pragst I. Prothrombin complex concentrate vs fresh frozen plasma for reversal of dilutional coagulopathy in a porcine trauma model. Br J Anaesth. 2009;102:345–54.
Joseph B, Aziz H, Pandit V, Hays D, Kulvatunyou N, Yousuf Z, et al. Prothrombin complex concentrate versus fresh-frozen plasma for reversal of coagulopathy of trauma: is there a difference? World J Surg. 2014;38:1875–81.
Jehan F, Aziz H, Oʼ Keeffe T, Khan M, Zakaria ER, Hamidi M, et al. The role of four-factor prothrombin complex concentrate in coagulopathy of trauma: aA propensity matched analysis. J Trauma Acute Care Surg. 2018;85:18–24.
Stansbury LG, Hess JR. The 100th anniversary of the first blood bank. Transfusion. 2017;57:2562–3.
Haddaway K, Bloch EM, Tobian AAR, Frank SM, Sikorski R, Cho BC, et al. Hemostatic properties of cold-stored whole blood leukoreduced using a platelet-sparing versus a non-platelet-sparing filter. Transfusion. 2019;59:1809–17.
Sivertsen J, Braathen H, Lunde THF, Kristoffersen EK, Hervig T, Strandenes G, et al. Cold-stored leukoreduced CPDA-1 whole blood: in vitro quality and hemostatic properties. Transfusion. 2020;
Huish S, Green L, Curnow E, Wiltshire M, Cardigan R. Effect of storage of plasma in the presence of red blood cells and platelets: re-evaluating the shelf life of whole blood. Transfusion. 2019;59:3468–77.
Meledeo MA, Peltier GC, McIntosh CS, Bynum JA, Cap AP. Optimizing whole blood storage: hemostatic function of 35-day stored product in CPD, CP2D, and CPDA-1 anticoagulants. Transfusion. 2019;59:1549–59.
Magnotti LJ, Zarzaur BL, Fischer PE, Williams RF, Myers AL, Bradburn EH, et al. Improved survival after hemostatic resuscitation: does the emperor have no clothes? J Trauma. 2011;70:97–102.
Koch CG, Li L, Sessler DI, Figueroa P, Hoeltge GA, Mihaljevic T, et al. Duration of red-cell storage and complications after cardiac surgery. N Engl J Med. 2008;358:1229–39.
Cartotto R, Taylor SL, Holmes JH, Peck M, Cochran A, King BT, et al. The effects of storage age of blood in massively transfused burn patients: a secondary analysis of the randomized transfusion requirement in burn care evaluation study. Crit Care Med. 2018;46:e1097–104.
• Bautista A, Wright TB, Meany J, Kandadai SK, Brown B, Khalafalla K, et al. Red cell storage duration does not affect outcome after massive blood transfusion in trauma and nontrauma patients: a retrospective analysis of 305 patients. Biomed Res Int. 2017;2017:3718615 This single-centre, retrospective study analysed the impact of storage time on trauma resuscitation outcome in severe injured patients. Despite limitations based on the design, the trial clearly demonstrates that the so- called “storage” effect, does not apply in patients undergoing massive blood transfusion in the trauma setting.
Cotton BA, Au BK, Nunez TC, Gunter OL, Robertson AM, Young PP. Predefined massive transfusion protocols are associated with a reduction in organ failure and postinjury complications. J Trauma. 2009;66:41–8 discussion 48.
Gunter OL, Au BK, Isbell JM, Mowery NT, Young PP, Cotton BA. Optimizing outcomes in damage control resuscitation: identifying blood product ratios associated with improved survival. J Trauma. 2008;65:527–34.
Maegele M, Lefering R, Paffrath T, Tjardes T, Simanski C, Bouillon B, et al. Red-blood-cell to plasma ratios transfused during massive transfusion are associated with mortality in severe multiple injury: a retrospective analysis from the Trauma Registry of the Deutsche Gesellschaft für Unfallchirurgie. Vox Sang. 2008;95:112–9.
Savage SA, Zarzaur BL, Croce MA, Fabian TC. Time matters in 1: 1 resuscitations: concurrent administration of blood: plasma and risk of death. J Trauma Acute Care Surg. 2014;77:833–7 discussion 837.
Dente CJ, Shaz BH, Nicholas JM, Harris RS, Wyrzykowski AD, Patel S, et al. Improvements in early mortality and coagulopathy are sustained better in patients with blunt trauma after institution of a massive transfusion protocol in a civilian level I trauma center. J Trauma. 2009;66:1616–24.
Teixeira PGR, Inaba K, Shulman I, Salim A, Demetriades D, Brown C, et al. Impact of plasma transfusion in massively transfused trauma patients. J Trauma. 2009;66:693–7.
Zink KA, Sambasivan CN, Holcomb JB, Chisholm G, Schreiber MA. A high ratio of plasma and platelets to packed red blood cells in the first 6 hours of massive transfusion improves outcomes in a large multicenter study. Am J Surg. 2009;197:565–70 discussion 570.
Snyder CW, Weinberg JA, McGwin G, Melton SM, George RL, Reiff DA, et al. The relationship of blood product ratio to mortality: survival benefit or survival bias? J Trauma. 2009;66:358–62 discussion 362.
Sim ES, Guyette FX, Brown JB, Daley BJ, Miller RS, Harbrecht BG, et al. Massive transfusion and the response to prehospital plasma: it is all in how you define it. J Trauma Acute Care Surg. 2020.
•• Nederpelt CJ, El Hechi MW, Kongkaewpaisan N, Kokoroskos N, Mendoza AE, Saillant NN, et al. Fresh frozen plasma-to-packed red blood cell ratio and mortality in traumatic hemorrhage: nationwide analysis of 4,427 patients. J Am Coll Surg. 2019;230(6):893–901 This large retrospective nationwide cohort study analysed the effect of different FFP to PRBC ratios in trauma patients. The trial confirmed in a much larger setting previous findings, which suggested that a 1:1 FFP to PRBC ration is associated with the lowest mortality in haemorrhaging trauma patients.
Roquet F, Neuschwander A, Hamada S, Favé G, Follin A, Marrache D, et al. Association of eEarly, hHigh pPlasma-to-rRed bBlood cCell tTransfusion rRatio wWith mMortality in aAdults wWith sSevere bBleeding aAfter tTrauma. JAMA Netw Open. 2019;2:e1912076.
Haywood-Watson RJ, Holcomb JB, Gonzalez EA, Peng Z, Pati S, Park PW, et al. Modulation of syndecan-1 shedding after hemorrhagic shock and resuscitation. PLoS One. 2011;6:e23530.
•• Sperry JL, Guyette FX, Brown JB, Yazer MH, Triulzi DJ, Early-Young BJ, et al. Prehospital plasma during air medical transport in trauma patients at risk for hemorrhagic shock. N Engl J Med. 2018;379:315–26 The “PAMPER” trial is a multi-centre, cluster-randomized, phase 3 superiority study comparing pre-hospital administration of thawed plasma with standard-care resuscitation during air medical transport. With a total of 501 patients, this trail clearly demonstrates a 9.8% reduction in mortality in patients who received pre-hospital FFP. Interestingly, the authors did not find any difference in respect to multi-organ failure, acute lung injury, nosocomial infections, or allergic or transfusion-related reactions. The trial opens the discussion whether pre-hospital FFP should be limited to air -ambulance services only.
Guyette FX, Sperry JL, Peitzman AB, Billiar TR, Daley BJ, Miller RS, et al. Prehospital blood product and crystalloid resuscitation in the severely injured patient: aA secondary analysis of the prehospital air medical plasma trial. Ann Surg. 2019.
Spinella PC, Perkins JG, Grathwohl KW, Beekley AC, Holcomb JB. Warm fresh whole blood is independently associated with improved survival for patients with combat-related traumatic injuries. J Trauma. 2009;66:S69–76.
Nessen SC, Eastridge BJ, Cronk D, Craig RM, Berséus O, Ellison R, et al. Fresh whole blood use by forward surgical teams in Afghanistan is associated with improved survival compared to component therapy without platelets. Transfusion. 2013;53(Suppl 1):107S–13S.
Cap AP, Beckett A, Benov A, Borgman M, Chen J, Corley JB, et al. Whole bBlood tTransfusion. Mil Med. 2018;183:44–51.
Gilstad C, Roschewski M, Wells J, Delmas A, Lackey J, Uribe P, et al. Fatal transfusion-associated graft-versus-host disease with concomitant immune hemolysis in a group A combat trauma patient resuscitated with group O fresh whole blood. Transfusion. 2012;52:930–5.
Yazer MH, Spinella PC. The use of low-titer group O whole blood for the resuscitation of civilian trauma patients in 2018. Transfusion. 2018;58:2744–6.
•• Young PP, Borge PD. Making whole blood for trauma available (again): the AMERICAN Red Cross experience. Transfusion. 2019;59:1439–45 This review by the American Red Cross emphasis their efforts to implement the usage of whole blood for trauma resuscitation. According to their survey, 93% of trauma surgeons would prefer whole blood transfusion instead of component therapy; despite the lack of clinical evidence. While the article points out some of the challenges related to preparing whole blood to immediate use for hospitals, the authors point out that the simplicity of transfusion might reign its limitations.
Ley EJ, Clond MA, Srour MK, Barnajian M, Mirocha J, Margulies DR, et al. Emergency department crystalloid resuscitation of 1.5 L or more is associated with increased mortality in elderly and nonelderly trauma patients. J Trauma. 2011;70:398–400.
Perel P, Roberts I, Ker K. Colloids versus crystalloids for fluid resuscitation in critically ill patients. Cochrane Database Syst. Rev. 2013;CD000567.
Condron M, Scanlan M, Schreiber M. Massive transfusion of low-titer cold-stored O-positive whole blood in a civilian trauma setting. Transfusion. 2019;59:927–30.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Anesthesia for Trauma
Rights and permissions
About this article
Cite this article
Nordmann, G.R., Obal, D. Is Fresh Frozen Plasma Still Necessary for Management of Acute Traumatic Coagulopathy?. Curr Anesthesiol Rep 10, 297–307 (2020). https://doi.org/10.1007/s40140-020-00397-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-020-00397-3