Abstract
Monitoring the level of consciousness during general anesthesia with processed electroencephalogram (EEG) monitors has become an almost routine practice in the operating room, despite ambiguous research results regarding its potential benefits. For the patient as well as the anesthesiologist, the primary concern with respect to general anesthesia is that there will be a lack of awareness and recall during surgery. Using EEG signals to monitor the depth of anesthesia should reduce the incidence of intraoperative awareness, lead to a reduction in drug consumption, prevent anesthesia-related adverse events, and enable faster recovery. These benefits have been associated with depth-of-anesthesia monitoring in small clinical trials, but larger studies of EEG-based monitoring have failed to confirm the results of the smaller studies. The results of recent studies that investigated the emergence of consciousness after general anesthesia and the mechanism of action of anesthetic drugs on the central nervous system may help us to understand the limitations of EEG-based monitors and why they do not perform better in large clinical trials. In this article, we review the current status of monitoring the hypnotic component of general anesthesia and discuss the results of recent studies and guidelines that pertain to depth-of-anesthesia monitoring.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There are four main components to general anesthesia (GA): unconsciousness (hypnosis and amnesia), antinociception, immobility with muscle paralysis, and hemodynamic stability. Electroencephalogram (EEG) patterns are known to change with the patient’s depth of anesthesia, and assessment of hypnosis requires measurements of electrical activity in the central nervous system (CNS). Anesthetics act on the brain; thus, this organ should be monitored in addition to the patient’s spinal cord reflexes and cardiovascular system signs such as blood pressure and heart rate. EEG-based depth-of-anesthesia (DoA) monitors use algorithms to continuously analyze EEG signals and translate any changes into simple numerical indices that correspond to the level of consciousness. Monitoring the level of consciousness is complex, and despite rapid developments in this area, the benefits of EEG-based anesthesia monitoring are still controversial [1, 2•]. The problem lies in the fact that our understanding of human consciousness is incomplete, and we do not yet entirely understand the effects of GA on the brain [3]. The depth of anesthesia is neither stable nor constant; rather, it is a dynamic condition that depends upon the balance between the dosage of anesthesia and the pain caused by surgery. A primary concern related to GA is the occurrence of awareness with recall (AWR) during surgery. To prevent AWR, unnecessarily deep levels of anesthesia are commonly used; this is a risk factor for intraoperative hypotension. Moreover, associations between too-deep states of anesthesia and poor postoperative, long-term outcomes have been reported [4]. Monitoring of the depth of anesthesia should accomplish certain goals: it should show changes in the level of anesthesia resulting from changes in the concentration of anesthetics in the blood, yield similar results even when different anesthetic agents are used, show changes corresponding to surgical stimulation, and indicate awareness with no more than a short delay. The use of monitors should reduce drug consumption, prevent anesthesia-related complications, enable faster recovery, and reduce intraoperative awareness. It should also be cost-effective. In this review, we will discuss current studies and guidelines for monitoring the hypnotic component of anesthesia.
General Anesthesia and the Mechanism of Unconsciousness
Anesthesia causes a global reduction in cerebral blood flow (CBF) and brain metabolism; these causes arise from the hyperpolarization of neuronal pathways to the cortex [5, 6]. In a positron emission tomography (PET) study with propofol and sevoflurane performed by Kaisti et al. [5], both anesthetic agents reduced the relative CBF in the cuneus, precuneus, posterior limbic system, thalamus, and midbrain. In addition, propofol reduced the relative CBF in the parietal and frontal cortices.
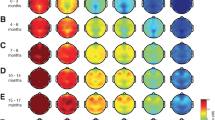
During the preoperative visit, anesthesiologists usually talk to patients about “being put to sleep” instead of being put into coma; however, GA is actually a reversible drug-induced coma [3]. In a deep coma state, patient responsiveness to pain stimulation disappears, just as it does during surgical anesthesia. The EEG pattern during a deep coma is similar to that of deep anesthesia, with high-amplitude, low frequency activity [7]. On the molecular level, stimulation of postsynaptic inhibitory ligand-gated ion channels is a potential side effect of anesthetic drug activity. The inhibitory synaptic receptors, such as gamma-aminobutyric acid subtype A (GABA2), are the site of action for propofol and volatile anesthetics [8]. It was previously thought that unconsciousness and amnesia during GA were brain cortical structure phenomena [9]. However, according to a study by Långsjö et al. [10••], during the emergence of consciousness from anesthesia, the subcortical structures of the brain are also involved. In this study, arousal-induced brain activation after propofol and dexmedetomidine anesthesia were administered was visualized with PET. The emergence of consciousness, as assessed by the motor response to a spoken command, was associated with the activation of deep brain structures, involving subcortical and limbic regions that are functionally connected with parts of the frontal and inferior parietal cortices (Fig. 1). Lee et al., [11••] investigated the mechanism of action of ketamine during GA and compared it with sevoflurane and propofol. They used EEG and normalized symbolic transfer entropy (NSTE) to measure directional connectivity across the frontal and parietal regions of the brain. Disruptions in frontal–parietal communication during GA are part of the mechanism by which ketamine, propofol, and sevoflurane induce unconsciousness. They concluded that measurement of frontal–parietal feedback connectivity during GA could provide a common metric of anesthesia-induced unconsciousness.
Neural correlates associated with the return of consciousness following propofol anesthesia, as assessed by the motor response to a spoken command, were associated with the activation of deep brain structures, involving subcortical and limbic regions that are functionally connected with parts of the frontal and inferior parietal cortices. Sagittal (top) and axial (bottom) sections of PET scan showing activation in the anterior cingulate cortex (i), thalamus (ii), and the brainstem (iii). Cortical renderings showing minimal occipital, parietal, and frontal activations at this threshold. From [10••], with permission from The Society of Neuroscience
EEG-Based Monitors of Depth of Anesthesia
There are many different EEG-based DoA monitors, including the Bispectral Index System Monitor (BIS Monitor; Covidien, USA); E-Entropy Module (GE Healthcare, USA); Narcotrend Compact M (MonitorTechnik, Germany); AEP A-line Monitor, Cerebral State Monitor (Danmeter, Denmark); Patient State Index Monitor, SEDLine (Masimo, USA); and SNAPII (Stryker, USA). However, not all of them have been thoroughly well validated by clinical studies. Auditory evoked potentials (AEPs) reflect the response in the EEG to auditory stimulation, usually as a click through headphones. AEPs were first used in studies of anesthesia depth, and they show dose-dependent changes with general anesthetics that are similar among different drugs. Decreases in amplitudes and increases in latencies of AEPs were detected during progressive stages of sedation and anesthesia [12]. An anesthesia depth monitor that uses AEP, the AEP A-line Monitor/2 (Danmeter, Denmark), employs a composite AEP/EEG A-line autoregressive index (AAI) [13–15]. To our knowledge, the AEP monitor is no longer available commercially as a DoA monitor. Thus, in this article, we will focus on only three EEG-based monitors: the BIS Monitor, E-Entropy and Narcotrend Compact M.
The BIS Monitor was the first commercially available monitor to measure the hypnotic component of anesthesia and thus monitor the pharmacodynamic effects of anesthetic agents on the brain [16–18]. The United States Food and Drug Administration (FDA) accepted the BIS monitor as a measure of hypnotic levels of anesthesia in 1996. BIS technology combines multiple processed EEG signal analyses: bispectral, power spectral, and time domain analyses [16].
In BIS monitoring validation studies, most intravenous anesthetics (e.g., propofol and thiopental) and volatile anesthetics (e.g., isoflurane, sevoflurane, and desflurane) cause gradual changes in BIS values with increased drug concentration. In a multicenter BIS evaluation study [19] with propofol, isoflurane, and midazolam, the researchers found a good correlation between BIS values and the observer’s assessment of alertness and sedation (OAAS) scale, with a very high predictive performance for correctly indicating the probability of loss of consciousness (LOC). Another multicenter study [20], which monitored the effects of anesthesia on BIS values, demonstrated that dosing anesthetic drugs with the goal of lowering BIS values is associated with a lower probability of movement in response to surgical stimulation.
The Narcotrend-Compact M (MonitorTechnik, Germany) monitors EEG signals continuously and uses an algorithm to predict which of the six hypnotic stages patients are currently in: A, awake; B, sedated; C, light anesthesia; D, general anesthesia; E, deep hypnosis; and F, burst suppression or electrical silence (there are also 15 substages). For surgical anesthesia, anesthetics are administered so that patients are maintained in the D and E stages [21]. In addition, the Narcotrend index can be used for calculations: the index is 100–0, and general anesthesia is within the range of 64–0. Validation studies that compared Narcotrend values with BIS values are available for propofol anesthesia [22–24] and also for inhalation anesthesia with desflurane and isoflurane [25, 26]. High prediction probability for loss of verbal response and eyelash reflex and for opens eyes spontaneously was detected with Narcotrend monitor [27].
Spectral entropy, which is a measure of the hypnotic level of anesthesia, was conceptualized in Finland in 1999 by Datex-Ohmeda. Spectral entropy estimates the complexity and irregularity of the signal and quantifies the amount of disorder in the EEG frequency domain [28]. Two components of spectral entropy are calculated: response entropy (RE) and state entropy (SE). RE is computed from EEG and electromyography (EMG) frequencies in the range of 0.8–47 Hz. An increase in the EMG frequency is an indicator of patient arousal, for example, in response to nociception stimulation. The shortest sampling window for RE is 1.92 s, which allows the monitor to respond quickly to EMG activation. SE is computed from the range of 0.8–32 Hz, and its time window for sampling is 15–60 s. Vakkuri et al. [29] validated SE as an accurate assessment of anesthesia depth with sevoflurane, propofol, and thiopental. RE and SE can distinguish between conscious and unconscious states and show high sensitivity and specificity in the detection of LOC. Moreover, Ellerkmann et al. [30] found that SE and RE were useful EEG-based measures of the effect of sevoflurane and propofol. Rinaldi et al. [31] evaluated BIS monitoring and SE in terms of their correlations with different end-tidal concentrations of sevoflurane, and found a good correlation between SE and end-tidal sevoflurane.
Reductions in Drug Consumption and Postoperative Adverse Events
In BIS utility studies [32, 33], BIS monitoring enabled a reduction in propofol use, faster emergence from anesthesia, and reduced recovery time. BIS monitoring is also reported to improve recovery from anesthesia and reduce the amount of propofol (29 %) and isoflurane (40 %) used [34], as well as the amount of sevoflurane [35]. SE-guided induction of GA with propofol reduced the amount of propofol needed [36, 37] and allowed for better cardiovascular stability in elderly patients [37]. In a study [38] that compared standard anesthesia practices and entropy-guided propofol-remifentanil anesthesia, the standard-anesthesia group of patients received more propofol and less remifentanil. A reduction in sevoflurane administration was also reported with the use of entropy-guided monitoring [35, 39], as well as with desflurane with Narcotrend monitoring [25].
BIS monitoring may help to reduce the incidence of postoperative nausea and vomiting [33, 40, 41]. In a meta-analysis [42] of BIS trials of ambulatory anesthesia in 1,390 patients across 11 randomized trials, BIS-guided anesthesia reduced anesthetic consumption by 19 %, reduced the occurrence of nausea/vomiting from 38 to 32 % in all patients, and reduced recovery time. There was no time difference between the groups with respect to discharge from the ambulatory surgery unit, and the total cost of patient stay was higher in the BIS group. Overall, in a Cochrane review [43] that included 31 randomized studies, BIS monitoring was not associated with an overall reduction in the amount of propofol or volatile anesthetics used. Moreover, Avidan and colleagues [44, 45] could not confirm that BIS monitoring was more likely to lead to a reduction in the administration of volatile anesthetics during GA compared to end-tidal anesthetic-agent concentration (ETAC). In a large study to prevent AWR with BIS monitoring [46••], there was no difference between the BIS group and an ETAC group with respect to the postoperative incidence of nausea/vomiting or discharge time from the recovery room. Therefore, one could question the benefits of this type of monitoring compared to traditional ETAC monitoring with respect to reducing recovery time and anesthetic consumption. In the study [47•] with automatic anesthesia system for closed-loop administration of anesthesia drugs with target BIS values, an adequate level of anesthesia was better achieved in the closed-loop group compared to the manual control group. Emergency time was shorter in the closed-loop group, but there was no significant difference in propofol consumption between groups.
EEG-Based Monitoring to Prevent Intraoperative Awareness During General Anesthesia
The first clinical trial to demonstrate that BIS monitoring reduces intraoperative awareness was the Ekman study [48]. This study compared 4,945 patients under GA with intubation, muscle relaxation, and BIS monitoring with 7,826 control patients for whom BIS monitoring was not used. There was a 77 % reduction in the incidence of awareness in the BIS-monitored group. The incidence of awareness in the BIS group was 0.04 % compared to 0.18 % in the control group from previous study. In the B-Aware trial [49], 2,463 patients who were at high risk of awareness during anesthesia were randomly allocated to either the BIS group or to the routine-practice group. BIS-guided anesthesia reduced the risk of awareness by 82 %. With the cost of routine BIS monitoring at 16 US dollars per use and a number needed to treat of 138, the cost of preventing one case of awareness in high-risk patients was about 2,200 US dollars in this study. By contrast, Avidan et al. [44] were unable to confirm the ability of BIS monitoring to prevent awareness during GA in patients with a higher risk of awareness. Two thousand patients were assigned to BIS-guided anesthesia (BIS values in the range of 40–60) or to ETAC, the latter of which was administered within a range of minimum alveolar concentration (MAC) of 0.7–1.3. Two cases of definite awareness occurred in each group (absolute difference 0 %). The investigators concluded that these results did not support routine BIS monitoring as part of standard anesthesia practice.
In a large, multicenter, randomized study [45] of 6,041 patients at high risk of awareness who were randomly assigned to BIS-guided anesthesia (BIS values in the range of 40–60) or ETAC-guided anesthesia (MAC 0.7–1.3), seven patients in the BIS group had definite intraoperative awareness, whereas two patients had definite intraoperative awareness in the ETAC group. Possible awareness was ascribed to 19 patients and eight patients, respectively, in the BIS and ETAC groups. Total definite and possible awareness was 0.47 % in all patients. Thus, BIS-guided anesthesia was not superior to ETAC-guided anesthesia with respect to awareness. However, 41 % of cases of awareness occurred when ETAC and BIS were within the study protocol’s target ranges; therefore, intraoperative awareness was not preventable with either monitoring method. ETAC is a measure of volatile drug concentration and does not measure the response of the brain to the anesthetic dose. Volatile anesthetics were used in the control group, but quite often, such as during cardiac surgery, anesthesia had been maintained by total intravenous anesthesia (TIVA). Under these circumstances, one cannot use ETAC for anesthesia depth control, and TIVA alone can be a risk for AWR [50, 51]. In 5,000 surgical patients who underwent TIVA [52], BIS monitoring reduced the incidence of awareness compared to the control group (0.14 % vs. 0.65 %, respectively). In an unselected population of 21,000 patients [46••] subjects were randomized to a BIS-guided group or a MAC-guided group. There was no difference between the BIS-guided and MAC-guided groups with respect to incidences of definite awareness. However, according to post hoc analyses, BIS monitoring was associated with a 4.7-fold reduction in definite or possible awareness events compared to routine care. All of the published studies of BIS monitoring to prevent AWR are shown in Table 1.
The clinical and cost effectiveness of the three monitors of general anesthetic depth, the BIS Monitor, E-Entropy, and Narcotrend, were evaluated in a recent report [2•], which compared these technologies with standard clinical monitoring during GA. Twenty-two randomized controlled trials were included in this systematic review of patients’ risk of short-term anesthesia-related complications and the risk of experiencing intraoperative awareness. Evidence of the impact of the monitors on reducing intraoperative awareness was limited, due to the lack of clinical effectiveness data for the E-Entropy and Narcotrend monitors. However, reductions in anesthetic consumption and recovery time were associated with the use of these monitors. For the BIS Monitor, six studies in which patients were classified as having risk factors for intraoperative awareness were included, and the overall pooled odds ratio for BIS monitoring to reduce awareness was 0.45 (95 % confidence interval, 0.25–0.81). The cost effectiveness of DoA monitors as measured by quality-adjusted life-years ranged from 8,033 to 44,198 British pounds sterling for the Narcotrend and BIS monitors, respectively, and appeared to be highly dependent upon a number of factors, in particular, the probability of awareness.
In conclusion, the results of various studies that measured the ability of BIS monitoring to guide the level of anesthesia and to prevent awareness are contradictory. BIS monitoring appears to be useful for patients who have a high risk of awareness and under TIVA [49, 52], but a study that used ETAC-guided anesthesia with volatile anesthetics did not support the utility of BIS monitoring [44, 45, 46••]. In addition, all studies of BIS monitoring thus far have been underpowered. If the incidence of awareness is 0.01 % and BIS monitoring produces a 50 % reduction in incidence, almost 41,000 patients would need to be included in a prospective randomized trial. The Långsjö et al. [10••] study was the first to reveal that not only cortical brain structures, but also deep subcortical structures, are involved in human consciousness and arousal. This may be one reason why BIS monitoring, which is based on cortex EEG signals, fails in the prevention of awareness during anesthesia.
Guidelines to Prevent AWR
The incidence of AWR is estimated to be approximately 0.1–0.4 % [53, 54] or 1–2 per 1,000 GA administered. During a recent national survey to estimate the incidence of AWR [55••], the estimated incidence of awareness was lower with this methodology (1:15,000) than previously reported in prospective clinical trials. In the recent study [56••] by Aranake et al., surgical patients with a history of AWR were five times more likely to experience AWR than similar patients without a history of AWR. The American Society of Anesthesiologists (ASA) has published descriptions of conditions that increase the risk of awareness during GA and guidelines to prevent intraoperative recall [50]. They recommend the use of EEG-based monitors of hypnosis (e.g., the BIS Monitor and E-Entropy) to reduce intraoperative awareness in high-risk patients (Table 2). The recent healthcare guidelines released by the National Institute for Health and Care Excellence (NICE) in the United Kingdom recommended the use of EEG-based DoA monitors during general anesthesia [57••, 58]. They recommended the BIS, E-Entropy, and Narcotrend monitors as options for patients receiving TIVA and for patients who are considered at higher risk of adverse outcomes during any type of GA. This includes patients who are at higher risk of unintended awareness and patients who are at higher risk of excessively deep anesthesia, including older patients, patients with liver disease, patients with a high body mass index, and patients with poor cardiovascular function.
BIS Monitoring and Postoperative Outcomes
A couple of studies have reported an association between a too-deep state of anesthesia and poor postoperative, long-term outcomes. In a study by Monk et al. [59], an association between deep cumulative anesthesia and increased 1-y mortality was reported for non-cardiac surgery patients. In that study, 1-year mortality was 5.5 % in all patients (n = 1,064) and 10.3 % in patients ≥65 years (n = 243). Significant, independent predictors of mortality were patient comorbidity, intraoperative systolic hypotension, and cumulative deep hypnotic time (BIS values of <45). In 4,086 patients with malignant disease who were monitored by BIS during surgery, 2-year mortality was associated with low BIS values (BIS values of <45); low BIS values were also a significant predictor of 1-year and 2-year mortality in this patient group [60]. In this study, when the initial multivariate regression analysis was repeated using pre-existing malignancy status among the covariates in the model, the previously significant relationship between 1-year and 2-year mortality and BIS values of <45 did not reach statistical significance. An association between the duration of low BIS values (BIS values of <45) and intermediate-term mortality was also found in 460 cardiac surgery patients [61]. The effect of BIS monitoring on long-term survival in the 2,463 patients included in the B-Aware trial was published by Leslie et al. [62]. The median follow-up time was 4.1 years, and the primary endpoint of the study was survival. The secondary objectives were incidences of myocardial infarction and stroke. There was no difference between the BIS group and the standard anesthesia care group with respect to risk of death. However, the hazard ratio for death was higher in patients with deep anesthesia (BIS values of <40 for more than 5 min) compared to other BIS-monitored patients. In addition, the odds ratios for myocardial infarction and stroke were higher in this patient group. The results of these studies [59–62] suggest that anesthesia management may have an effect on morbidity and mortality; however, these were observational studies, and the relationship between the level of anesthesia and patient outcome remains an open question [4].
Limitations of EEG-Based Monitoring of Hypnosis
Artifacts from the operating room environment, where there are other electrical devices, such as diathermy instruments and pacemakers, can contaminate EEG signals. Artifacts and poor signal quality may be sources of unreliable BIS values. During BIS monitoring for the assessment of hypnosis, various conditions, such as hypothermia, hypovolemia, and neurological disorders, could cause changes in the EEG signal such that it would indicate an incorrect hypnotic state [63]. The level of muscular block and EMG activity should also be taken into account during monitoring. Many studies have shown that the level of muscular block can interfere with the values of EEG-based monitoring [64, 65].
BIS monitoring may not perform reliably with all anesthetics. The use of nitrous oxide has no impact on BIS values [66] and entropy indices [67]. In addition, ketamine use does not change the bispectral index [68] and poor performance of spectral entropy monitoring during S-ketamine anesthesia was detected [69]. In the large group of 1,100 patients who participated in the B-Unaware trial, the relationship between ETAC and BIS values during maintenance of anesthesia was examined [70]. In this study, BIS values frequently correlated poorly with ETAC values and were often insensitive to changes in inhalation anesthetic concentrations. In a study by Kaskinoro et al. [71], spectral entropy and BIS values were tested to differentiate consciousness from unconsciousness during increasing doses of three different anesthetic agents: dexmedetomidine, propofol, and sevoflurane. Because of wide inter-individual variability, BIS and entropy monitoring were not able to reliably differentiate consciousness from unconsciousness during and after stepwise increasing concentrations of these anesthetics. The dose–response curve of anesthetic drugs and depth-of-anesthesia indices are sigmoidal, with a pharmacodynamic plateau near the value of 40; this means that below this value, BIS monitoring is not sensitive to changes in anesthetic drug concentrations [72].
Conclusions and Future Perspectives
In large clinical studies, BIS monitoring failed to prevent AWR during general anesthesia and also failed to reduce intraoperative drug consumption compared to ETAC monitoring [44, 45, 46••]. According to recent studies [10••, 11••] of the mechanism of consciousness during general anesthesia, the subcortical structure of the human brain and information connectivity between the frontal and parietal cortices are involved during emergence from anesthesia. EEG-based DoA monitors that use only a frontal EEG montage for signal analyses are probably unable to detect these changes; thus, they may fail to reduce intraoperative awareness. In spite of some remaining ambiguity, the results of a few studies, as well as the existing literature as a whole, suggest that the level of hypnosis during general anesthesia, at least in patients with a high risk of awareness and adverse outcomes during any type of GA, and during TIVA, should be monitored by EEG-based systems [50, 57••].
In the future, EEG-based monitors should include more EEG channels, such as those in the occipital area and both brain hemispheres. Algorithms that include the blood concentration of anesthetics should also be incorporated into DoA monitors, as well as better EMG filtering. The development of monitors that use a combination of information from EEG and, for example, AEPs, should be considered, because BIS monitoring only measures cortical function, (hypnotic state), whereas AEPs monitoring provides information about the function of the brainstem as well as the subcortical and cortical components [73–75]. In daily clinical practice, by using EEG-based monitoring to measure the hypnotic level of anesthesia, anesthesiologists should be able improve patient care, recovery, and outcome by keeping the depth of anesthesia stable, avoiding excessively deep levels of hypnosis, and reducing the incidence of perioperative awareness. The anesthetists who assess the depth of hypnosis should analyze information not only from EEG-based monitors, but also from hemodynamic signs like blood pressure and pulse frequency, and should also interpret the raw EEG waveform seen on the anesthesia monitor to check for signs such as the easy-to-interpret burst-suppression pattern in the EEG. EEG-based monitoring will also help clinicians and anesthesiology residents to understand more fully the effect of anesthetic activity on patients and the relationship between different aspects of anesthesia (e.g., hypnosis, antinociception, and immobility).
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ellerkmann RK, Soehle M, Kreuer S. Brain monitoring revisited: what is it all about? Best Pract Res Clin Anaesthesiol. 2013;2:225–33.
• Shepherd J, Jones J, Frampton G, et al. Clinical effectiveness and cost-effectiveness of depth of anaesthesia monitoring (E-Entropy, Bispectral Index and Narcotrend): a systematic review and economic evaluation. Health Technol Assess. 2013;17:1–264. The available evidence on the impact of the technologies on reducing the likelihood of intraoperative awareness is limited. However, there were reductions in general anesthetic consumption and anesthetic recovery times. The cost-effectiveness of depth of anesthesia monitoring appears to be highly dependent on a number of factors, including probability of awareness.
Brown EN, Lydic R, Schiff ND. General anesthesia, sleep, and coma. N Engl J Med. 2010;363:2638–50.
Monk TG, Weldon BC. Does depth of anesthesia monitoring improve postoperative outcomes? Curr Opin Anaesthesiol. 2011;24:665–9.
Kaisti KK, Metsähonkala L, Teräs M, et al. Effects of surgical levels of propofol and sevoflurane anesthesia on cerebral blood flow in healthy subjects studied with positron emission tomography. Anesthesiology. 2002;96:1358–70.
Schlünzen L, Juul N, Hansen KV, et al. Regional cerebral glucose metabolism during sevoflurane anaesthesia in healthy subjects studied with positron emission tomography. Acta Anaesthesiol Scand. 2010;54:603–9.
Young GB. The EEG in coma. J Clin Neurophysiol. 2000;17:473–85.
John ER, Prichep LS. The anesthetic cascade: a theory of how anesthesia suppresses consciousness. Anesthesiology. 2005;102:447–71.
Jameson LC, Sloan TB. Using EEG to monitor anesthesia drug effects during surgery. J Clin Monit Comput. 2006;20:445–72.
•• Långsjö JW, Alkire MT, Kaskinoro K, et al. Returning from oblivion: imaging the neural core of consciousness. J Neurosci. 2012;32:4935–43. The emergence of consciousness, as assessed with a motor response to a spoken command, was associated with the activation of a core network involving subcortical and limbic regions that become functionally coupled with parts of frontal and inferior parietal cortices upon awakening from unconsciousness.
•• Lee U, Ku S, Noh G, et al. Disruption of frontal-parietal communication by ketamine, propofol, and sevoflurane. Anesthesiology. 2013;118:1264–75. Diverse anesthetics disrupt frontal-parietal communication, despite molecular and neurophysiologic differences. Analysis of directional connectivity in frontal-parietal networks could provide a common metric of general anesthesia and insight into the cognitive neuroscience of anesthetic-induced unconsciousness.
Thornton C. Evoked potentials in anaesthesia. Eur J Anaesthesiol. 1991;8:89–107.
Struys MM, Jensen EW, Smith W, et al. Performance of the ARX-derived auditory evoked potential index as an indicator of anesthetic depth: a comparison with bispectral index and hemodynamic measures during propofol administration. Anesthesiology. 2002;96:803–16.
Recart A, Gasanova I, White PF, et al. The effect of cerebral monitoring on recovery after general anesthesia: a comparison of the auditory evoked potential and bispectral index devices with standard clinical practice. Anesth Analog. 2003;97:1667–74.
Recart A, White PF, Wang A, et al. Effect of auditory evoked potential index monitoring on anesthetic drug requirements and recovery profile after laparoscopic surgery: a clinical utility study. Anesthesiology. 2003;99:813–8.
Rampil IJ. A primer for EEG signal processing in anesthesia. Anesthesiology. 1998;89:980–1002.
Johansen JW. Update on Bispectral Index monitoring. Best Pract Research Clin Anaesth. 2006;1:81–99.
Punjasawadwong Y, Boonjeungmonkol N, Phongchiewboon A. Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Library. 2010;1-70.
Glass PS, Bloom M, Kearse L, et al. Bispectral analysis measures sedation and memory effects of propofol, midazolam, isoflurane, and alfentanil in healthy volunteers. Anesthesiology. 1997;86:836–47.
Sebel PS, Lang E, Rampil IJ, et al. A multicenter study of bispectral electroencephalogram analysis for monitoring anesthetic effect. Anesth Analg. 1997;84:891–9.
Kreuer S, Wilhelm W. The Narcotrend monitor. Best Pract Res Clin Anaesthesiol. 2006;20:111–9.
Kreuer S, Wilhelm W, Grundmann U, et al. Narcotrend index versus bispectral index as electroencephalogram measures of anesthetic drug effect during propofol anesthesia. Anesth Analog. 2004;98:692–7.
Kreuer S, Bruhn J, Larsen R, et al. Comparability of Narcotrend index and bispectral index during propofol anaesthesia. Br J Anaesth. 2004;93:235–40.
Schmidt GN, Bischoff P, Standl T, et al. Comparative evaluation of Narcotrend, Bispectral Index, and classical electroencephalographic variables during induction, maintenance, and emergence of a propofol/remifentanil anesthesia. Anesth Analog. 2004;98:1346–53.
Kreuer S, Bruhn J, Stracke C, et al. Narcotrend or bispectral index monitoring during desflurane-remifentanil anesthesia: a comparison with a standard practice protocol. Anesth Analg. 2005;101:427–34.
Kreuer S, Bruhn J, Larsen R, et al. Application of Bispectral Index and Narcotrend index to the measurement of the electroencephalographic effects of isoflurane with and without burst suppression. Anesthesiology. 2004;101:847–54.
Schmidt GN, Bischoff P, Standl T, et al. Narcotrend and Bispectral Index monitor are superior to classic electroencephalographic parameters for the assessment of anesthetic states during propofol-remifentanil anesthesia. Anesthesiology. 2003;99:1072–7.
Viertiö-Oja H, Maja V, Särkelä M, et al. Description of the Entropy™ algorithm as applied in the Datex-Ohmeda S/5™ Entropy Module. Acta Anaesthesiol Scand. 2004;48:154–61.
Vakkuri A, Yli-Hankala A, Talja P, et al. Time–frequency balanced spectral entropy as a measure of anesthetic drug effect in central nervous system during sevoflurane, propofol, and thiopental anesthesia. Acta Anaesthesiol Scand. 2004;48:145–53.
Ellerkmann RK, Soehle M, Alves TM, et al. Spectral entropy and bispectral index as measures of the electroencephalographic effects of propofol. Anesth Analog. 2006;102:1456–62.
Rinaldi S, Consales G, De Gaudio AR. State entropy and bispectral index: correlation with end tidal sevoflurane concentrations. Minerva Anestesiol. 2007;73:39–48.
Gan TJ, Glass PS, Windsor A, et al. Bispectral index monitoring allows faster emergence and improved recovery from propofol, alfentanil, and nitrous oxide anesthesia. BIS Utility Study Group. Anesthesiology. 1997;87:808–15.
Luginbühl M, Wüthrich S, Petersen-Felix S, et al. Different benefit of bispectal index (BIS) in desflurane and propofol anesthesia. Acta Anaesthesiol Scand. 2003;47:165–73.
Yli-Hankala A, Vakkuri A, Annila P, et al. EEG bispectral index monitoring in sevoflurane or propofol anaesthesia: analysis of direct costs and immediate recovery. Acta Anaesthesiol Scand. 1999;43:545–9.
Aimé I, Verroust N, Masson-Lefoll C, et al. Does monitoring bispectral index or spectral entropy reduce sevoflurane use? Anesth Analog. 2006;103:1469–77.
Vakkuri A, Yli-Hankala A, Sandin R, et al. Spectral entropy monitoring is associated with reduced propofol use and faster emergence in propofol-nitrous oxide-alfentanil anesthesia. Anesthesiology. 2005;103:274–9.
Riad W, Schreiber M, Saeed AB. Monitoring with EEG entropy decreases propofol requirement and maintains cardiovascular stability during induction of anaesthesia in elderly patients. Eur J Anaesthesiol. 2007;24:684–8.
Gruenewald M, Zhou J, Schloemerkemper N, et al. M-Entropy guidance vs standard practice during propofol-remifentanil anaesthesia: a randomised controlled trial. Anaesthesia. 2007;62:1224–9.
El Hor T, Van Der Linden P, De Hert S, et al. Impact of entropy monitoring on volatile anesthetic uptake. Anesthesiology. 2013;118:868–73.
Nelskylä KA, Yli-Hankala AM, Puro PH, et al. Sevoflurane titration using bispectral index decreases postoperative vomiting in phase II recovery after ambulatory surgery. Anesth Analog. 2001;93:1165–9.
Pavlin JD, Souter KJ, Hong JY, et al. Effects of bispectral index monitoring on recovery from surgical anesthesia in 1,580 inpatients from an academic medical center. Anesthesiology. 2005;102:566–73.
Liu SS. Effects of Bispectral Index monitoring on ambulatory anesthesia: a meta-analysis of randomized controlled trials and a cost analysis. Anesthesiology. 2004;101:311–5.
Punjasawadwong Y, Boonjeungmonkol N, Phongchiewboon A. Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Library. 2010;1–70.
Avidan MS, Zhang L, Burnside BA, et al. Anesthesia awareness and the bispectral index. N Engl J Med. 2008;358:1097–108.
Avidan MS, Jacobsohn E, Glick D, et al. BAG-RECALL Research Group. Prevention of intraoperative awareness in a high-risk surgical population. N Engl J Med. 2011;365:591–600.
•• Mashour GA, Shanks A, Tremper KK, et al. Prevention of intraoperative awareness with explicit recall in an unselected surgical population: a randomized comparative effectiveness trial. Anesthesiology. 2012;117:717–25. This negative trial could not detect a difference in the incidence of definite awareness or recovery variables between monitoring protocols based on either BIS values or anesthetic concentration. By post hoc secondary analysis, the BIS protocol was associated with a 4.7-fold reduction in definite or possible awareness events compared with a cohort receiving no intervention.
• Hemmerling TM, Arbeid E, Wehbe M, et al. Evaluation of a novel closed-loop total intravenous anaesthesia drug delivery system: a randomized controlled trial. Br J Anaesth. 2013;110:1031–9. The closed-loop system was better at maintaining BIS and Analgoscore than manual administration.
Ekman A, Lindholm ML, Lennmarken C, Sandin R. Reduction in the incidence of awareness using BIS monitoring. Acta Anaesthesiol Scand. 2004;48:20–6.
Myles PS, Leslie K, McNeil J, et al. Bispectral index monitoring to prevent awareness during anaesthesia: the B-Aware randomised controlled trial. Lancet. 2004;29:1757–63.
Apfelbaum JL, James F. Arens JF, et al. American Society of Anesthesiologists Task Force on Intraoperative Awarenes. Practice advisory for intraoperative awareness and brain function monitoring: a report by the American Society of Anesthesiologists task force on intraoperative awareness. Anesthesiology. 2006;104:847–64.
Xu L, Wu AS, Yue Y. The incidence of intra-operative awareness during general anesthesia in China: a multi-center observational study. Acta Anaesthesiol Scand. 2009;53:873–82.
Zhang C, Xu L, Ma YQ, et al. Bispectral index monitoring prevent awareness during total intravenous anesthesia: a prospective, randomized, double-blinded, multi-center controlled trial. Chin Med J (Engl). 2011;124:3664–9.
Sandin RH, Enlund G, Samuelsson P, Lennmarken C. Awareness during anaesthesia: a prospective case study. Lancet. 2000;26:707–11.
Sebel PS, Bowdle TA, Ghoneim MM, et al. The incidence of awareness during anesthesia: a multicenter United States study. Anesth Analog. 2004;99:833–9.
•• Pandit JJ, Cook TM, Jonker WR, O’Sullivan E. A national survey of anaesthetists (NAP5 Baseline) to estimate an annual incidence of accidental awareness during general anaesthesia in the UK. 5th National Audit Project (NAP5) of the Royal College of Anaesthetists and the Association of Anaesthetists of Great Britain and Ireland. Anaesthesia. 2013;68:343–53. The estimated incidence of awareness with this methodology of 1:15,000 was lower than the 1–2:1000 previously reported in prospective clinical trials.
•• Aranake A, Gradwohl S, Ben-Abdallah A, et al. Increased risk of intraoperative awareness in patients with a history of awareness. Anesthesiology. 2013;119:1275–83. Surgical patients with a history of AWR are five times more likely to experience AWR than similar patients without a history of AWR. Further consideration should be given to modifying perioperative care and postoperative evaluation of patients with a history of AWR.
•• National Institute for Clinical Excellence. NICE Diagnostics Guidance: Depth of anaesthesia monitors—Bispectral index (BIS), E-Entropy and Narcotrend Compact M. 2012. www.nice.org.uk. Recommendations for the use the BIS, E-Entropy, and Narcotrend monitors as options for patients receiving TIVA and for patients who are considered at higher risk of adverse outcomes during any type of GA.
Pandit JJ, Cook TM. National Institute for Clinical Excellence guidance on measuring depth of anaesthesia: limitations of EEG-based technology. Br J Anaesth. 2013;110:325–8.
Monk TG, Saini V, Weldon BC, et al. Anesthetic management and one-year mortality after noncardiac surgery. Anesth Analog. 2005;100:4–10.
Lindholm ML, Träff S, Granath F, et al. Mortality within 2 years after surgery in relation to low intraoperative bispectral index values and preexisting malignant disease. Anesth Analog. 2009;108:508–12.
Kertai MD, Pal N, Palanca BJ, et al. B-Unaware Study Group Association of perioperative risk factors and cumulative duration of low bispectral index with intermediate-term mortality after cardiac surgery in the B-Unaware Trial. Anesthesiology. 2010;112:1116–27.
Leslie K, Myles PS, Forbes A, et al. The effect of bispectral index monitoring on long-term survival in the B-aware trial. Anesth Analog. 2010;110:816–22.
Dahaba AA. Different conditions that could result in the bispectral index indicating an incorrect hypnotic state. Anesth Analog. 2005;101:765–73.
Hans P, Giwer J, Brichant JF, et al. Effect of an intubation dose of rocuronium on Spectral Entropy and Bispectral Index™ responses to laryngoscopy during propofol anaesthesia. Br J Anaesth. 2006;97:842–7.
Aho AJ, Lyytikäinen LP, Yli-Hankala A, et al. Explaining Entropy responses after a noxious stimulus, with or without neuromuscular blocking agents, by means of the raw electroencephalographic and electromyographic characteristics. Br J Anaesth. 2011;106:69–76.
Rampil IJ, Kim JS, Lenhardt R, et al. Bispectral EEG index during nitrous oxide administration. Anesthesiology. 1998;89:671–7.
Anderson RE, Jakobsson JG. Entropy of EEG during anaesthetic induction: a comparative study with propofol or nitrous oxide as sole agent. Br J Anaesth. 2004;92:167–70.
Sakai T, Singh H, Mi WD, et al. The effect of ketamine on clinical endpoints of hypnosis and EEG variables during propofol infusion. Acta Anaesthesiol Scand. 1999;43:212–6.
Maksimow A, Särkelä M, Långsjö JW, et al. Increase in high frequency EEG activity explains the poor performance of EEG spectral entropy monitor during S-ketamine anesthesia. Clin Neurophysiol. 2006;117:1660–8.
Whitlock EL, Villafranca AJ, Lin N, et al. Relationship between bispectral index values and volatile anesthetic concentrations during the maintenance phase of anesthesia in the B-Unaware trial. Anesthesiology. 2011;115:1209–18.
Kaskinoro K, Maksimow A, Långsjö J, et al. Wide inter-individual variability of bispectral index and spectral entropy at loss of consciousness during increasing concentrations of dexmedetomidine, propofol, and sevoflurane. Br J Anaesth. 2011;107:573–80.
Palanca BJ, Mashour GA, Avidan MS. Processed electroencephalogram in depth of anesthesia monitoring. Curr Opin Anaesthesiol. 2009;22:553–9.
Nishiyama T, Hanaoka K. The A-line ARX index may be a more sensitive detector of arousal than the bispectral index during propofol-fentanyl-nitrous oxide anesthesia: a preliminary investigation. Can J Anaesth. 2004;51:539–44.
Bonhomme V, Llabres V, Dewandre PY, et al. Combined use of Bispectral Index and A-Line Autoregressive Index to assess anti-nociceptive component of balanced anaesthesia during lumbar arthrodesis. Br J Anaesth. 2006;96:353–60.
Musialowicz T, Niskanen M, Yppärilä-Wolters H, et al. Auditory evoked potentials in bispectral index-guided anaesthesia for cardiac surgery. Eur J Anaesthesiol. 2007;24:571–9.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Musialowicz, T., Lahtinen, P. Current Status of EEG-Based Depth-of-Consciousness Monitoring During General Anesthesia. Curr Anesthesiol Rep 4, 251–260 (2014). https://doi.org/10.1007/s40140-014-0061-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-014-0061-x