Abstract
Purpose of Review
This review summarizes the literature on intraoperative electroencephalography (EEG) monitoring in pediatric anesthesia from 2017 to 2022.
Recent Findings
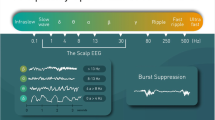
New developments to our understanding of EEG changes in the anesthetized brain, developing brain, emergence delirium, epileptiform activity, and EEG changes during spinal anesthesia will be discussed. Low voltage EEG (i.e., discontinuous or isoelectric EEG) and its association with changes in the alpha frequency (8–12 Hz) band, non-proprietary EEG to guide anesthetic dosing in young children, EEG-guided propofol anesthesia, and a summary of EEG studies to improve clinical outcomes will be covered.
Summary
Intraoperative EEG in children has gained significant interest over the past few years. Despite our improved understanding of EEG changes under anesthesia, and using EEG as a biomarker of anesthetic depth to titrate dosing in children, much remains to be discovered, particularly related to the optimal EEG parameters to use in infants and how EEG can be used to improve clinical outcomes.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hemmings HC, Riegelhaupt PM, Kelz MB, Solt K, Eckenhoff RG, Orser BA, et al. Towards a comprehensive understanding of anesthetic mechanisms of action: a decade of discovery. Trends Pharmacol Sci. 2019;40(7):464–81. This review article updates the reader on the mechanisms of general anesthetics at the molecular level and at the systems-neuroscience level. The paper includes a summary drug-specific EEG profiles, and an overview state-dependent functional connectivity profiles.
Lee U, Mashour GA. Role of network science in the study of anesthetic state transitions. Anesthesiology. 2018;129(5):1029–44.
Purdon PL, Sampson A, Pavone KJ, Brown EN. Clinical electroencephalography for anesthesiologists: part i: background and basic signatures. Anesthesiology. 2015;123(4):937–60.
Brandt SP, Walsh EC, Cornelissen L, Lee JM, Berde C, Shank ES, et al. Case studies using the electroencephalogram to monitor anesthesia-induced brain states in children. Anesth Analg. 2020;131(4):1043–56.
Ching S, Cimenser A, Purdon PL, Brown EN, Kopell NJ. Thalamocortical model for a propofol-induced α-rhythm associated with loss of consciousness. Proc Natl Acad Sci. 2010;107(52):22665–70.
Lee U, Oh G, Kim S, Noh G, Choi B, Mashour GA. Brain networks maintain a scale-free organization across consciousness, anesthesia, and recovery: evidence for adaptive reconfiguration. Anesthesiology. 2010;113(5):1081–91.
Duclos C, Nadin D, Mahdid Y, Tarnal V, Picton P, Vanini G, et al. Brain network motifs are markers of loss and recovery of consciousness. Sci Rep. 2021;11(1):3892.
Lee JM, Akeju O, Terzakis K, Pavone KJ, Deng H, Houle TT, et al. A prospective study of age-dependent changes in propofol-induced electroencephalogram oscillations in children. Anesthesiology. 2017;127(2):293–306.
Cornelissen L, Kim SE, Lee JM, Brown EN, Purdon PL, Berde CB. Electroencephalographic markers of brain development during sevoflurane anaesthesia in children up to 3 years old. Br J Anaesth. 2018;120(6):1274–86. A comprehensive study examining the spatial and temporal patterns of EEG activity in infants and children using power and coherence measures.
Rigouzzo A, Khoy-Ear L, Laude D, Louvet N, Moutard ML, Sabourdin N, et al. EEG profiles during general anesthesia in children: a comparative study between sevoflurane and propofol. Pediatr Anesth. 2019;29(3):250–7. A uniquely designed prospective study using step-wise dose escalation to examine relationship with anesthetic concentration, EEG properties and BIS output in older children aged 5 to 18 years.
Liang Z, Ren N, Wen X, Li H, Guo H, Ma Y, et al. Age-dependent cross frequency coupling features from children to adults during general anesthesia. Neuroimage. 2021;240:118372. A comprehensive study examining cross-frequency coupling properties across age in children and adults. The authors propose the use of coupling measures as a future tool for depth of anesthesia monitoring in the pediatric population.
Koch S, Stegherr AM, Mörgeli R, Kramer S, Toubekis E, Lichtner G, et al. Electroencephalogram dynamics in children during different levels of anaesthetic depth. Clin Neurophysiol. 2017;128(10):2014–21.
de Heer IJ, Bouman SJM, Weber F. Electroencephalographic (EEG) density spectral array monitoring in children during sevoflurane anaesthesia: a prospective observational study. Anaesthesia. 2019;74(1):45–50.
Cornelissen L, Donado C, Lee JM, Liang NE, Mills I, Tou A, et al. Clinical signs and electroencephalographic patterns of emergence from sevoflurane anaesthesia in children. Eur J Anaesthesiol. 2018;35(1):49–59.
Zakaria L, Desowska A, Berde CB, Cornelissen L. Electroencephalographic delta and alpha oscillations reveal phase-amplitude coupling in paediatric patients undergoing sevoflurane-based general anaesthesia. Br J Anaesth. 2023;130(5):595–602.
Bethlehem RAI, Seidlitz J, White SR, Vogel JW, Anderson KM, Adamson C, et al. Brain charts for the human lifespan. Nature. 2022;604(7906):525–33.
Grasso C, Marchesini V, Disma N. Applications and limitations of neuro-monitoring in paediatric anaesthesia and intravenous anaesthesia: a narrative review. J Clin Med. 2021;10(12):2639.
Kim J, Lee HC, Byun SH, Lim H, Lee M, Choung Y, et al. Frontal electroencephalogram activity during emergence from general anaesthesia in children with and without emergence delirium. Br J Anaesth. 2021;126(1):293–303.
Koch S, Rupp L, Prager C, Wernecke KD, Kramer S, Fahlenkamp A, et al. Emergence delirium in children is related to epileptiform discharges during anaesthesia induction: an observational study. Eur J Anaesthesiol EJA. 2018;35(12):929.
Koch S, Stegherr AM, Rupp L, Kruppa J, Prager C, Kramer S, et al. Emergence delirium in children is not related to intraoperative burst suppression – prospective, observational electrography study. BMC Anesthesiol. 2019;19(1):146.
Miao M, Han Y, Zhang Y, Xu Y, Zhang L, Yang Y, et al. Epileptiform EEG discharges during sevoflurane anesthesia in children: a meta-analysis. Clin Neurophysiol. 2022;143:48–55.
Chao JY, Tam M, Ferrera A, Ivenitsky D, Gizzo L, Schwartz R, et al. Epileptiform discharges, electrographic seizures, and electroclinical seizures during paediatric sevoflurane anaesthesia: a systematic review and proposal for standard definitions. Br J Anaesth. 2023;130(1):e18-21. This recent systematic review summarizes the prior literature reporting epileptiform changes during pediatric sevoflurane anesthesia and proposes a set of standard definitions to help increase the rigor and reproducibility of future research.
Whitaker EE, Chao JY, Holmes GL, Legatt AD, Yozawitz EG, Purdon PL, et al. Electroencephalographic assessment of infant spinal anesthesia: a pilot prospective observational study. Pediatr Anesth. 2021;31(11):1179–86. This study reported the finding of the development of sleep spindle complexes following spinal anesthesia in infants, suggesting that the commonly observed sedated state in this age group is associated with a normal, physiologic non-rapid eye movement NREM) sleep state.
Pawar N, Barreto Chang OL. Burst suppression during general anesthesia and postoperative outcomes: mini review. Front Syst Neurosci. 2022;15:767489.
Cornelissen L, Bergin AM, Lobo K, Donado C, Soul JS, Berde CB. Electroencephalographic discontinuity during sevoflurane anesthesia in infants and children. Kurth D, editor. Pediatr Anesth. 2017;27(3):251–62.
Agrawal U, Berde CB, Cornelissen L. Electroencephalographic features of discontinuous activity in anesthetized infants and children. Xie Z, editor. PLOS ONE. 2019;14(10):e0223324.
Yuan I, Landis WP, Topjian AA, Abend NS, Lang SS, Huh JW, et al. Prevalence of isoelectric electroencephalography events in infants and young children undergoing general anesthesia. Anesth Analg. 2020;130(2):462–71.
Yuan I, Xu T, Skowno J, Zhang B, Davidson A, von Ungern-Sternberg BS, et al. Isoelectric Electroencephalography in infants and toddlers during anesthesia for surgery: an international observational study. Anesthesiology. 2022;137(2):187–200. Large international prospective study determining the incidence of isoelectric EEG in children under 3 and the associated factors. There is a marginal difference of expired sevoflurane between infants with vs without isoelectric EEG, suggesting that traditional dosing may be “over-dosing” the brain.
Chao JY, Gutiérrez R, Legatt AD, Yozawitz EG, Lo Y, Adams DC, et al. Decreased electroencephalographic alpha power during anesthesia induction is associated with EEG discontinuity in human infants. Anesth Analg. 2022;135(6):1207–16. This study assessed the association of alpha power during sevoflurane induction with development of low voltage EEG patterns (i.e., EEG discontinuity), with findings suggesting that salient features in the EEG might serve as biomarkers that could be useful for clinical anesthetic titration/management to help avoid the development of discontinuous EEG.
Flores FJ, Hartnack KE, Fath AB, Kim SE, Wilson MA, Brown EN, et al. Thalamocortical synchronization during induction and emergence from propofol-induced unconsciousness. Proc Natl Acad Sci. 2017;114(32):E6660–8.
Cornelissen L, Kim SE, Purdon PL, Brown EN, Berde CB. Age-dependent electroencephalogram (EEG) patterns during sevoflurane general anesthesia in infants. Culham JC, editor. eLife. 2015;23(4):e06513.
Yuan I, Xu T, Kurth CD. Using electroencephalography (EEG) to guide propofol and sevoflurane dosing in pediatric anesthesia. Anesthesiol Clin. 2020;38(3):709–25.
Xu T, Kurth CD, Yuan I, Vutskits L, Zhu T. An approach to using pharmacokinetics and electroencephalography for propofol anesthesia for surgery in infants. Pediatr Anesth. 2020;30(12):1299–307. Provides practical guidance on using EEG parameters besides the proprietary EEG index to guide anesthesia.
Nimmo AF, Absalom AR, Bagshaw O, Biswas A, Cook TM, Costello A, et al. Guidelines for the safe practice of total intravenous anaesthesia (TIVA): joint guidelines from the association of anaesthetists and the society for intravenous anaesthesia. Anaesthesia. 2019;74(2):211–24.
Yuan I, Missett RM, Jones-Oguh S, Massa CB, Babus LW, Garcia-Marcinkiewicz AG, et al. Implementation of an electroencephalogram-guided propofol anesthesia education program in an academic pediatric anesthesia practice. Pediatr Anesth. 2022;32(11):1252–61.
Long MHY, Lim EHL, Balanza GA, Allen JC, Purdon PL, Bong CL. Sevoflurane requirements during electroencephalogram (EEG)-guided vs standard anesthesia care in children: a randomized controlled trial. J Clin Anesth. 2022;81:110913. One of few randomized trials investigating clinical outcomes of using EEG guided anesthesia in pediatrics.
Weber F, Walhout LC, Escher JC. The impact of Narcotrend™ EEG-guided propofol administration on the speed of recovery from pediatric procedural sedation-a randomized controlled trial. Pediatr Anesth. 2018;28(5):443–9.
Larsen LG, Wegger M, LéGreves S, Erngaard L, Hansen TG. Emergence agitation in paediatric day case surgery: a randomised, single-blinded study comparing narcotrend and heart rate variability with standard monitoring. Eur J Anaesthesiol. 2022;39(3):261–8. One of few randomized trials determining emergence agitation when using EEG to guide anesthesia.
Dennhardt N, Boethig D, Beck C, Heiderich S, Boehne M, Leffler A, et al. Optimization of initial propofol bolus dose for EEG Narcotrend Index-guided transition from sevoflurane induction to intravenous anesthesia in children. Anderson B, editor. Pediatr Anesth. 2017;27(4):425–32.
Cheung YM, Scoones G, Stolker RJ, Weber F. Use, applicability and reliability of depth of hypnosis monitors in children - a survey among members of the European Society for Paediatric Anaesthesiology. BMC Anesthesiol. 2018;18(1):40.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
IY has received speaker honorarium and consulting fees from Masimo Corp. JYC is supported by NIH/National Center for Advancing Translational Science (NCATS) Einstein-Montefiore CTSA Grant Numbers UL1 TR002556 andKL2 TR002558 (JC). CDK is a member of the Masimo Corp clinical leadership advisory board. LC is supported in part by the Boston Children’s Hospital Anesthesia Research Trailblazer Award and the Sara Page Mayo Endowment for Pediatric Pain Research, Education, and Treatment. The authors declare no other financial or conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yuan, I., Chao, J.Y., Kurth, C.D. et al. Intraoperative EEG Monitoring in Pediatric Anesthesia. Curr Anesthesiol Rep 13, 135–142 (2023). https://doi.org/10.1007/s40140-023-00562-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-023-00562-4