Abstract
Introduction
Graves’ ophthalmopathy (GO) is an autoimmune inflammatory disorder observed in a substantial proportion of patients with Graves’ disease (GD), with debilitating symptoms of disfiguring, periorbital pain, dry eyes, diplopia, and even visual disturbances. Previous studies involving Western populations have noted discrepancies in risk factors for GO. Therefore, this study aimed to determine the risk factors for GO development and the protective effect of statins in newly diagnosed patients with GD in Taiwan.
Methods
This retrospective case–control study was based on a tertiary center cohort involving patients with GD diagnosed between 2010 and 2019 at the National Taiwan University Hospital (n = 11,035). Patients who were diagnosed or treated elsewhere, had been followed up for less than 6 months or were with a diagnosis of orbital tumor were excluded. Overall, 3578 patients with GD met the inclusion criteria. Univariate and multivariate logistic regression analyses were used to ascertain the odds ratio (OR) of developing GO, with adjustment for sociodemographic factors, interventions for managing GD and thyroid hormone levels, to determine protective and risk factors for GO.
Results
In our multivariate model, the use of statins reduced the risk of GO development (OR 0.2; 95% confidence interval [CI] 0.08–0.50; p < 0.001). Thyroid dysfunction including hyperthyroidism (OR 4.2; 95% CI 2.97–5.88; p < 0.001) and hypothyroidism (OR 4.7; 95% CI 3.02–7.19; p < 0.001) was associated with an increased risk of developing GO. Smoking status and lipid profile were not risk factors in our cohort.
Conclusion
In newly diagnosed patients with GD, the use of statins decreased the risk of developing GO by 80%, whereas serum lipid levels were not considered risk factors. Further nationwide population-based studies may help clarify the differences in risk factors between various ethnic groups.
Trail Registration
This trial was approved by the Research Ethics Committee of National Taiwan University Hospital (202202066RINC), retrospectively registered from January 1, 2010 to December 31, 2019.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Graves’ disease (GD) can lead to Graves’ ophthalmopathy (GO) in a substantial proportion of patients, resulting in varying symptoms such as periorbital pain, dry eyes, diplopia, and even visual impairment. However, the previously identified risk factors were primarily derived from Western populations, with inconsistencies observed among various studies. |
In a cohort of patients with newly diagnosed GD in Taiwan, we determined the endogenous and exogenous risk factors for GO development and examined the possible beneficial effects of statins on GO prevention. |
What was learned from the study? |
Older age at diagnosis, higher body mass index, and hyper- or hypothyroidism were associated with a higher risk of developing GO, whereas high levels of high-density lipoprotein cholesterol were reported to be a protective factor. |
Other lipid profiles (low-density lipoprotein cholesterol, total cholesterol, and triglyceride), smoking status, and radioactive iodine or surgical treatments were not significantly correlated with the risk of developing GO. |
In our multivariate model, statins significantly decreased the risk of developing GO by 80% via their effects other than lowering lipids. |
Introduction
Graves’ disease (GD) is the most common cause of hyperthyroidism, with an annual incidence of 20 cases per 100,000 persons and a female to male ratio ranging from 4:1 to 5:1 [1, 2]. GD pathogenesis occurs via the stimulation of thyrotropin (thyroid-stimulating hormone [TSH]) receptors on thyroid follicular cells by thyrotropin receptor antibodies [3]. Approximately 25–50% of patients with GD develop Graves’ ophthalmopathy (GO), which may manifest as exophthalmos, periorbital edema, lid lag and retraction, and exposure keratitis [4]. Visual impairment due to optic neuropathy or corneal ulceration is a rare but severe manifestation of GO [3, 5]. GO features mainly result from inflammation and increased production of glycosaminoglycans, causing enlarged extraocular muscles and increased adipose tissue deposition within the orbit [6].
GO is a multifactorial disease with environmental, genetic, and immune factors [7]. It has a female to male ratio ranging from 2:1 to 10:1, although men tend to experience a more severe form [7, 8]. A previous study revealed that although the prevalence of GO does not differ among various ethnic groups, Asian patients develop milder forms of GO than Caucasian patients [9]. Other endogenous risk factors include genetics, with immune regulatory and response genes such as human leukocyte antigen (HLA)-DR3, cytotoxic T lymphocyte antigen (CTLA)-4, and thyroid-related genes thyroid-stimulating hormone receptor (TSHR) and thyroglobulin (TG) as candidates. A recent study showed that the allele and genotype frequencies were similar between patients with GO and those with GD [10].
Different GD treatments and smoking have been identified as exogenous risk factors for GO [11]. A recent study revealed that thyroidectomy and statin use can reduce GO risk, whereas radioactive iodine (RAI) exposure can increase the risk [12]. Thyroid dysfunction, including hyper- and hypothyroidism, is associated with an increased risk of GO development or deterioration [11]. However, the findings of previous studies investigating the role of TSHR antibodies by measuring the levels of thyrotropin-binding inhibitory immunoglobulin (TBII) or thyroid-stimulating immunoglobulin (TSI) are inconsistent. The studies also revealed that triiodothyronine (T3) and tetraiodothyronine (T4) levels are not predictors of GO risk [11, 13].
GO treatment depends on the severity of the disease. It includes artificial tears and topical glucocorticoids for mild disease and systemic steroids and orbital irradiation for moderate or severe disease [2]. Moreover, recent studies have shown the effectiveness of immunomodulatory drugs [2, 14, 15]. Clinical cohorts and in vitro studies have recently demonstrated that statins may play an active role in GO prevention [12, 16].
A retrospective study involving 34,894 newly diagnosed patients with GD in Sweden demonstrated that statin users are less likely to develop GO [6]. A phase 2 randomized clinical trial of statins for Graves’ orbitopathy (STAGO), which investigated the use of intravenous glucocorticoids with or without atorvastatin for patients with hypercholesterolemia and moderate-to-severe GO, showed that atorvastatin improved the response to intravenous glucocorticoids. Phase 3 studies are warranted to confirm this finding in patients without hypercholesterolemia [17]. The mechanisms by which statins reduce the risk of GO are not fully understood. Statins may inhibit adipogenesis, tumor necrosis factor alpha (TNFα)-induced inflammation, and transforming growth factor beta (TGFβ)-induced tissue remodeling that underlie GO symptoms [16, 18, 19].
Our study recruited a cohort of newly diagnosed patients with GD in a tertiary referral hospital. This study aimed to determine the protective and risk factors for GO in newly diagnosed patients with GD and examine the protective effect of statins, potentially developing future preventive strategies for GO.
Methods
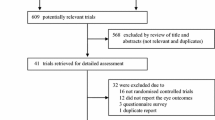
This single-center, retrospective case–control study was approved by the Research Ethics Committee of National Taiwan University Hospital (202202066RINC). This study adhered to the tenets of the Declaration of Helsinki. Research and analysis were conducted on deidentified data provided by National Taiwan University Hospital-integrative Medical Database (NTUH-iMD) under formal agreement. As a result of the nature of retrospective database research, individual consent to participate and to publish was waived. We enrolled newly diagnosed patients with GD (ICD-9-CM, 242.00; ICD-10-CM/PCS, E05.00) who were aged 20 years or more at diagnosis in National Taiwan University Hospital between 2010 and 2019. Patients diagnosed before 2010 or those who presented with GO manifestations during their first consultation were excluded, along with patients with benign or malignant orbital tumors. Individuals without documented GD treatment in our center who were possibly treated at other faculties were also excluded. Patients were followed up from the first GD diagnosis until GO development or end of the study on December 31, 2019. Patients who were followed up for less than 6 months were excluded. After the aforementioned patients were excluded, 3578 patients with GD were enrolled for further analysis (Fig. 1).
Excluding patients with orbital tumors in advance, we made a GO diagnosis if the patient had at least one of the billing codes for eyelid retraction, restrictive strabismus, exophthalmos, exposure keratopathy, or compressive optic neuropathy. Patients who underwent GO-related surgery, such as orbital decompression, mullerectomy, levator muscle recession, lower lid retraction correction, or strabismus surgery, were also included as patients with GO. Since the billing code for specific surgeries, such as mullerectomy, is exclusively designated for GO-related procedures in the National Health Insurance surgical reporting code system of Taiwan, and all enrolled cases had the order code of Hertel exophthalmometry, we can infer that patients recruited on the basis of the aforementioned criteria likely had GO.
A statin user was defined as a patient who received statin prescriptions for more than 60 days (1) within a year before GO diagnosis or (2) any time during follow-up for a patient without GO. The same criteria were applied to the users of other cholesterol-lowering agents, hydroxychloroquine, and cyclooxygenase-2 (COX-2) inhibitors.
Patient baseline demographics and clinical characteristics are summarized using means and standard deviations for normally distributed continuous variables, whereas other continuous numerical data are presented as median and interquartile range. Categorical variables are presented as frequencies and percentages. Potential risk factors were determined using the chi-squared test for nominal factors or Mann–Whitney U test for ordinal factors. Multivariate logistic regression was used to determine the odds ratio (OR) for developing GO, adjusted for age at GD diagnosis, body mass index (BMI), thyroid status, TBII levels, and statin usage. In the regression model, other antithyroid treatments (RAI exposure and thyroidectomy) were compared using treatment with antithyroid medication alone as the reference.
An exploratory subgroup analysis of patients with dyslipidemia was performed. Dyslipidemia was defined according to the 2019 European Society of Cardiology and the European Atherosclerosis Society (ESC/EAS) guidelines with the following criteria: low-density lipoprotein (LDL) cholesterol level greater than 115 mg/dL, high-density lipoprotein (HDL) cholesterol level less than 40 mg/dL in men or less than 45 mg/dL in women, total cholesterol (T-CHO) level greater than 190 mg/dL, or triglyceride (TG) level greater than 150 mg/dL [20]. We also included patients who administered statins for more than 60 days in our subgroup. Statistical analyses were performed using SAS, 9.4 software (SAS Institute, Cary, NC, USA). For all analyses, two-sided p values of less than 0.05 were considered to indicate statistical significance, and 95% CI was calculated.
Results
Of the 3578 patients with GD, 372 (10.4%) developed GO during follow-up. The mean follow-up time was 62.6 (standard deviation [SD] 37.4) months for the non-GO group and 9.9 (SD 16.2) months for the GO group. The mean age at GD diagnosis was significantly higher in the GO group than in the non-GO group (mean [SD] 46.2 [13.8] vs. 43.7 [15.0] years; p = 0.001), consistent with a previous study [21]. No sex difference was noted, and a higher proportion of women were observed in both groups. Higher BMI levels were associated with an increased risk of GO development (OR 1.06; 95% CI 1.02–1.10; p = 0.003) in the multivariate model. No statistical difference was noted in GO development between nonsmokers and smokers. Overall, 3326 (93%) patients received antithyroid medications in the study cohort. No significant difference was noted in medical or other treatments (including RAI or surgery) between GO and non-GO groups (Tables 1 and 2).
Statins significantly decreased the risk of developing GO in the univariate model (OR 0.19; 95% CI 0.10–0.39; p < 0.001). After adjustment for age, BMI, thyroid status, and TBII level, statins significantly decreased the risk of developing GO by 80% in the multivariate model (OR 0.2; 95% CI 0.08–0.50; p < 0.001). No significant difference was noted between the two groups regarding the use of hydroxychloroquine, COX-2 inhibitors, or other cholesterol-lowering agents such as fenofibrate, ezetimibe, gemfibrozil, and cholestyramine resin.
Compared with the euthyroid status, both hyperthyroidism (OR 4.2; 95% CI 2.97–5.88; p < 0.001) and hypothyroidism (OR 4.7; 95% CI 3.02–7.19; p < 0.001) increased the risk of developing GO in the multivariate model. Elevated levels of TSHR antibody (OR 1.02; 95% CI 1.01–1.02; p < 0.001) also increased the risk of developing GO. HDL cholesterol showed a protective effect against GO development in the univariate model, although with an OR of 0.97 (95% CI 0.94–0.99; p = 0.007). LDL cholesterol, T-CHO, TG, or dyslipidemia status showed no significant correlations and were not included in our multivariate model.
We conducted a subgroup analysis of patients with dyslipidemia to determine whether statin’s lipid-lowering effect or other pleiotropic mechanisms decreased the risk of GO development (Table 3). Statin use decreased the risk of developing GO by 86% (OR 0.14; 95% CI 0.05–0.35; p < 0.001) in the multivariate model. HDL and LDL cholesterol did not affect GO development (OR 0.97; 95% CI 0.93–1.00; p = 0.06 and OR 0.99; 95% CI 0.98–1.00; p = 0.12 respectively), suggesting that statins exert their influence via a pleiotropic effect.
Discussion
Our study demonstrated that statins play a significant role in decreasing the risk of GO development by 80%. This finding was independent of the patient’s lipid profile or dyslipidemia status, suggesting the presence of mechanisms other than lipid-lowering effects. There exists increasing evidence that the administration of statins by patients with GD may reduce GO risk. Stein et al. demonstrated that statin use decreased the risk of GO development by 40% in a nationwide cohort in the USA in 2015 [12]. Nilsson et al. also revealed that statin users were less likely to develop GO (hazard ratio [HR] 0.87, p = 0.04) [6]. A recent Korean study compared the effects of statins according to sex, showing that higher doses of statins were associated with a higher risk of GO in men (HR 1.27, p = 0.05) and lower risk of GO in women (HR 0.37, p < 0.001) [22]. The STAGO phase II randomized clinical trial demonstrated that orally administered atorvastatin improved the treatment response of patients with GO to intravenous glucocorticoids [17]. However, the mechanism by which statins or cholesterol levels influence GO development is not yet fully understood. A previous longitudinal study demonstrated that nonstatin cholesterol-lowering drugs or other anti-inflammatory drugs have no protective effect against GO [12]. In addition to its hypolipidemic role, statins exert pleiotropic anti-inflammatory, immunomodulatory, and antifibrotic effects [23]. Simvastatin has been demonstrated to inhibit the expression of TNFα-induced proinflammatory factor cysteine-rich protein 61, which is noted in many inflammatory diseases, including GO [19, 24]. In addition, simvastatin reportedly downregulated adipogenesis and inhibited TGFβ-induced myofibroblast differentiation in cultured orbital fibroblasts from patients with GO [16, 25].
Our research discovered that statin use was associated with an 80% reduction in the risk of developing GO, which is greater than that reported in previous studies in Western populations [6, 12]. Consistent with our findings, Lee et al. [22] found that a high dose of statins was associated with a 63% reduction in the risk of developing GO (95% CI 0.22–0.62, p < 0.001) in Korean women. Racial differences in the efficacy of statins should be considered. Prior work has shown that Western populations require three to four times higher doses of statins and a significantly longer duration of statin administration to achieve a certain LDL reduction compared to Asian populations, denoting higher statin potency in Asian subjects [26, 27]. Aside from the hypolipidemic effect, the protective effect of statins against GO may also exhibit racial differences. Further cross-ethnic research or analysis would be required to validate the racial difference of the pleiotropic effects of statins and elucidate the potent genetic factors.
Recent studies have suggested that increased cholesterol levels are a risk factor for or a predictor of higher clinical activity scores (CAS) in GO [21, 28]. A retrospective study involving 86 patients with GD showed higher LDL cholesterol (135 vs. 107 mg/dL) and T-CHO (212 vs. 176 mg/dL) levels in the GO group than in the non-GO group. No differences in HDL cholesterol or TG levels were noted between the two groups [28]. A cross-sectional study involving 250 patients with GD revealed that T-CHO levels greater than 191 mg/dL or LDL cholesterol levels greater than 118 mg/dL were associated with an increased risk of developing GO. Furthermore, higher T-CHO levels were indicative of higher CAS [21]. Baseline LDL cholesterol levels greater than 190 mg/dL reportedly predict a poorer response to parenteral corticosteroids [29]. In the Korean study, higher T-CHO levels increased the risk of developing GO in women (HR 1.04, p = 0.003); however, this was not observed in men (HR 1.04, p = 0.117) [22]. In our study, although serum lipid profiles had no significant influence on GO development, some findings are notable. The overall average LDL cholesterol level was 104 mg/dL, whereas the average levels in GO and non-GO groups were 99 and 105 mg/dL, respectively. These LDL cholesterol levels in our cohort were considerably lower than those reported in previous cohorts [21, 30]. Similarly, both GO and non-GO groups in our study showed lower T-CHO levels (183 and 180 mg/dL, respectively) than those reported in the Caucasian cohort mentioned above [21, 30]. In the Korean study, the median T-CHO levels were 173.5 mg/dL in men and 179 mg/dL in women. Only T-CHO level in women showed a significant association with GO development [22]. Our cohort did not demonstrate significant effects of serum lipid levels, possibly because of the overall lower cholesterol levels in our ethnicity. This should be considered when determining risk factors in different populations. Further studies are warranted to clarify the role of serum lipid profiles in GO development in the Asian population.
Contrary to previous studies, elevated HDL cholesterol levels were shown to be a protective factor for the development of GO in our cohort [28, 31]. HDL cholesterol plays anti-inflammatory and antioxidant roles by removing oxidized lipids from cell membranes and other lipoproteins with their antioxidant enzymes and protein components [32]. Prior work showed the interactions between the protein components of HDLs and the immune cells inhibit the production of interleukin-1β and TNFα, both of which are implicated in GO pathogenesis [33]. Another study indicated that HDLs inhibit the expression of proinflammatory cytokines, especially TNFα, at the transcriptional level [34]. Elevated HDL levels, in addition to their peripheral lipid-removing effects, may act as a protective factor for GO development through systemic anti-inflammatory regulation.
A previous study revealed that thyroid dysfunction is associated with an increased risk of developing GO and more severe diseases, consistent with our study finding [35]. In another study, a positive correlation was found between TSHR antibody levels and the activity and severity of GO [36]. Additionally, elevated levels of TSI can also serve as a predictive indicator for the development of GO in newly diagnosed patients with GD [37]. However, a recent systematic review showed that the role of antithyroid peroxidase (anti-TPO) antibodies in GO remains unclear, and our study did not observe statistical significance in this regard [38]. Therefore, according to the findings of previous studies, patients with GD should undergo close monitoring of TSHR antibodies levels, as elevated levels of TSHR antibodies indicate an increased risk of developing GO.
Prior studies reported that about 25–50% of patients with GD develop GO; however, recent research has shown a lower incidence [4, 9, 37]. Stein et al. found that only 8.8% of newly diagnosed patients with GD developed GO during a 6-year follow-up [12]. A Korean study showed a low incidence of GO with no significant gender difference, with a ratio of 6.2% in men and 5.8% in women [22]. Similarly, our study revealed a GO incidence of 10.4% in patients with GD. The discrepancies among the reported incidence may result from the variation of study design and recruiting strategies. Our study recruited patients with GD at a tertiary center and excluded those treated elsewhere, potentially lowering the recorded incidence of GO. Furthermore, as the diagnosis of GO in our study was based upon billing codes for eyelid retraction, restrictive strabismus, exophthalmos, exposure keratopathy, compressive optic neuropathy, as well as the related surgeries, the recruitment may omit patients with milder manifestation of GO, underrating the incidence.
In our study, both GO and non-GO groups predominantly consisted of female patients, with no sex predilection toward GO development. This finding is consistent with that of studies involving different ethnicities. Lanzolla et al. reported no significant sex difference between GO and non-GO groups in an Italian population (n = 86) [28]. Stein et al. also showed no risk difference between the two sexes in a larger American population (n = 8404) [12].
Although smoking has been widely recognized as a risk factor for developing GO, our study revealed no significant association. Our results were comparable to those of the Korean study [22]. In both cohorts, approximately 6% of women were smokers or ex-smokers. As the cohorts consisted mostly of women, the number of smokers may have been extremely low, hindering the accurate estimation of the impact of smoking on GO development. Furthermore, the lack of documentation regarding the intensity and duration of smoking as well as secondhand smoke exposure (a recognized risk) may be crucial factors [35]. Among women, secondhand smoke exposure may be more prevalent than active smoking.
This study had some limitations. First, patients in a tertiary center were likely to have a more severe form of GO, which requires surgical intervention. Patients who had received prior treatment elsewhere were excluded, which lowered the rate of GO in the cohort. Second, patients with GO were identified according to the billing codes of eyelid retraction, strabismus, exophthalmos, or thyroid eye surgery. However, in clinical practice, patients with mild GO may not have such billing codes assigned to them, particularly if they have not visited an ophthalmologist. Consequently, the identified GO group may have more severe manifestations. Third, our study did not differentiate between types of statins or consider the dosages used. Another study revealed different results for atorvastatin and simvastatin before dosage adjustment [6]. Additionally, the number of patients prescribed with other cholesterol-lowering agents was extremely low; therefore, they could not be included in the multivariate analysis. These limitations should be considered when interpreting our study findings. Future research should aim to address these limitations to improve the understanding of the relationship between statin use and GO development.
Conclusion
This hospital-based cohort study demonstrated a significant reduction in the risk of developing GO associated with statin use. Thyroid dysfunction was also associated with an increased risk of developing GO. It is important to consider population differences, including variations in smoking prevalence or average serum lipid levels, when determining risk factors for GO in different ethnic groups.
Our research suggests that regular lipid profile assessments are recommended for patients with GD. Elevated lipid levels require treatment, with statins being the preferred choice. Further studies should explore the use of oral statins as a preventive treatment for GO through specific randomized controlled trials. These study findings may guide clinical approaches and inspire further studies in this field.
Data Availability
The datasets used and/or analyzed during the present study are available from the corresponding author upon reasonable request.
References
Hussain YS, Hookham JC, Allahabadia A, Balasubramanian SP. Epidemiology, management and outcomes of Graves’ disease-real life data. Endocrine. 2017;56(3):568–78.
Smith TJ, Hegedus L. Graves’ disease. N Engl J Med. 2016;375(16):1552–65.
Bahn RS, Heufelder AE. Pathogenesis of Graves’ ophthalmopathy. N Engl J Med. 1993;329(20):1468–75.
San MI, Arenas M, Carmona R, Rutllan J, Medina-Rivero F, Lara P. Review of the treatment of Graves’ ophthalmopathy: the role of the new radiation techniques. Saudi J Ophthalmol. 2018;32(2):139–45.
Bartalena L, Tanda ML. Clinical practice. Graves’ ophthalmopathy. N Engl J Med. 2009;360(10):994–1001.
Nilsson A, Tsoumani K, Planck T. Statins decrease the risk of orbitopathy in newly diagnosed patients with Graves disease. J Clin Endocrinol Metab. 2021;106(5):1325–32.
Bahn RS. Current insights into the pathogenesis of Graves’ ophthalmopathy. Horm Metab Res. 2015;47(10):773–8.
Ofira Z, Oded S, Ayelet P, et al. Gender differences in clinical presentation and prognosis of thyroid eye disease. Eur J Ophthalmol. 2021;31(5):2717–23.
Hiromatsu Y, Eguchi H, Tani J, Kasaoka M, Teshima Y. Graves’ ophthalmopathy: epidemiology and natural history. Intern Med. 2014;53(5):353–60.
Yin X, Latif R, Bahn R, Davies TF. Genetic profiling in Graves’ disease: further evidence for lack of a distinct genetic contribution to Graves’ ophthalmopathy. Thyroid. 2012;22(7):730–6.
Stan MN, Bahn RS. Risk factors for development or deterioration of Graves’ ophthalmopathy. Thyroid. 2010;20(7):777–83.
Stein JD, Childers D, Gupta S, et al. Risk factors for developing thyroid-associated ophthalmopathy among individuals with Graves disease. JAMA Ophthalmol. 2015;133(3):290–6.
Noh JY, Hamada N, Inoue Y, Abe Y, Ito K, Ito K. Thyroid-stimulating antibody is related to Graves’ ophthalmopathy, but thyrotropin-binding inhibitor immunoglobulin is related to hyperthyroidism in patients with Graves’ disease. Thyroid. 2000;10(9):809–13.
Perez-Moreiras JV, Gomez-Reino JJ, Maneiro JR, et al. Efficacy of tocilizumab in patients with moderate-to-severe corticosteroid-resistant Graves orbitopathy: a randomized clinical trial. Am J Ophthalmol. 2018;195:181–90.
Paridaens D, van den Bosch WA, van der Loos TL, Krenning EP, van Hagen PM. The effect of etanercept on Graves’ ophthalmopathy: a pilot study. Eye (Lond). 2005;19(12):1286–9.
Shahida B, Johnson PS, Jain R, et al. Simvastatin downregulates adipogenesis in 3T3-L1 preadipocytes and orbital fibroblasts from Graves’ ophthalmopathy patients. Endocr Connect. 2019;8(9):1230–9.
Lanzolla G, Sabini E, Leo M, et al. Statins for Graves’ orbitopathy (STAGO): a phase 2, open-label, adaptive, single centre, randomised clinical trial. Lancet Diabetes Endocrinol. 2021;9(11):733–42.
Bifulco M, Ciaglia E. Statin reduces orbitopathy risk in patients with Graves’ disease by modulating apoptosis and autophagy activities. Endocrine. 2016;53(3):649–50.
Wei YH, Liao SL, Wang CC, Wang SH, Tang WC, Yang CH. Simvastatin inhibits CYR61 expression in orbital fibroblasts in Graves’ ophthalmopathy through the regulation of FoxO3a signaling. Mediators Inflamm. 2021;2021:8888913.
Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Atherosclerosis. 2019;290:140–205.
Sabini E, Mazzi B, Profilo MA, et al. High serum cholesterol is a novel risk factor for Graves’ orbitopathy: results of a cross-sectional study. Thyroid. 2018;28(3):386–94.
Lee J, Kang J, Ahn HY, Lee JK. Sex-specific risk factors associated with Graves' orbitopathy in Korean patients with newly diagnosed Graves' disease. Eye (Lond). 2023;37(16):33–91.
Greenwood J, Steinman L, Zamvil SS. Statin therapy and autoimmune disease: from protein prenylation to immunomodulation. Nat Rev Immunol. 2006;6(5):358–70.
Lantz M, Vondrichova T, Parikh H, et al. Overexpression of immediate early genes in active Graves’ ophthalmopathy. J Clin Endocrinol Metab. 2005;90(8):4784–91.
Wei YH, Liao SL, Wang SH, Wang CC, Yang CH. Simvastatin and ROCK inhibitor Y-27632 inhibit myofibroblast differentiation of Graves’ ophthalmopathy-derived orbital fibroblasts via RhoA-mediated ERK and p38 signaling pathways. Front Endocrinol (Lausanne). 2020;11: 607968.
Ryo N, Katsumi M, Hiroyuki D. Racial differences in the cholesterol-lowering effect of statin. J Atheroscler Thromb. 2017;24(1):19–25.
Kalra Dinesh K. Bridging the racial disparity gap in lipid-lowering therapy. Am Heart Assoc. 2021;10:e019533.
Lanzolla G, Sabini E, Profilo MA, et al. Relationship between serum cholesterol and Graves’ orbitopathy (GO): a confirmatory study. J Endocrinol Invest. 2018;41(12):1417–23.
Naselli A, Moretti D, Regalbuto C, et al. Evidence that baseline levels of low-density lipoproteins cholesterol affect the clinical response of Graves’ ophthalmopathy to parenteral corticosteroids. Front Endocrinol (Lausanne). 2020;11:609895.
Lanzolla G, Sabini E, Profilo MA, et al. Relationship between serum cholesterol and Graves’ orbitopathy (GO): a confirmatory study. J Endocrinol Investig. 2018;41:1417–23.
Sulu C, Dedeoglu SE, Gonen B, et al. Serum lipoprotein(a) is not associated with Graves’ ophthalmopathy. Metab Syndrome Related Disord. 2023. https://doi.org/10.1530/endoabs.90.P792.
Massimiliano R, Margherita B, Nicola F, et al. High density lipoproteins inhibit oxidative stress-induced prostate cancer cell proliferation. Sci Rep. 2018;8(1):2236.
Nevila H, Jean-Michel D, Christine M, et al. Apolipoprotein AI inhibits the production of interleukin-1β and tumor necrosis factor-α by blocking contact-mediated activation of monocytes by T lymphocytes. Blood. 2001;97(8):2381–9.
Manabu I, Mamiko N, Yuriko O, et al. High-density lipoprotein suppresses tumor necrosis factor alpha production by mycobacteria-infected human macrophages. Sci Rep. 2018;8(1):6736.
Gontarz-Nowak K, Szychlinska M, Matuszewski W, Stefanowicz-Rutkowska M, Bandurska-Stankiewicz E. Current knowledge on Graves’ orbitopathy. J Clin Med. 2020;10(1):16.
Roos JCP, Paulpandian V, Murthy R. Serial TSH-receptor antibody levels to guide the management of thyroid eye disease: the impact of smoking, immunosuppression, radio-iodine, and thyroidectomy. Eye (Lond). 2019;33(2):212–7.
Takakura A, Kirkeby K, Earle K, Silkiss RZ. Predicting the development of orbitopathy in Graves thyroidopathy patients: the potential role of TSI testing. Ophthalmic Plast Reconstruct Surg. 2015;31(5):369–72.
Kyriakos G, Patsouras A, Voutyritsa E, et al. The role of TPOAb in thyroid-associated orbitopathy: a systematic review. Ocul Immunol Inflamm. 2022;30(7–8):1740–6.
Acknowledgements
We express our gratitude to all individuals participating in the study. The research would not have been completed without their valuable contributions and cooperation, and we are thankful for their involvement.
Medical Writing, Editorial, and Other Assistance
Clinical data were acquired from National Taiwan University Hospital-integrative Medical Database (NTUH-iMD) with the assistance from National Taiwan University Hospital Department of Medical Research. Statistical consultation and analyses were supported by National Taiwan University Hospital-Statistical Consulting Unit (NTUH-SCU). Editorial assistance for this article was provided by Hobert from Enago Inc., and was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship, agreed to be accountable for all aspects of the work, and have given their approval for this version to be published.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
Yi-Hsuan Wei proposed the study concept and design and contributed to manuscript revision. Shyang-Rong Shih proposed the study concept and design and contributed to manuscript revision. Shu-Lang Liao proposed the study concept and design. Grace Chia-Yen Hsu proposed the study design, performed statistical analysis, and drafted the manuscript. Fang-Yu Chang drafted the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Grace Chia-Yen Hsu, Shyang-Rong Shih, Fang-Yu Chang, Shu-Lang Liao, and Yi-Hsuan Wei have no competing interests to disclose.
Ethical Approval
This study was approved by the Research Ethics Committee of National Taiwan University Hospital (No. 202202066RINC) and adhered to the tenets of the Declaration of Helsinki. Research and analysis were conducted on deidentified data provided by National Taiwan University Hospital-integrative Medical Database (NTUH-iMD) under formal agreement. As a result of the nature of retrospective database research, individual consent to participate and to publish was waived.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hsu, G.CY., Shih, SR., Chang, FY. et al. An Appraisal of the Preventive Effect of Statins on the Development of Graves’ Ophthalmopathy: A Hospital-Based Cohort Study. Ophthalmol Ther 13, 1499–1511 (2024). https://doi.org/10.1007/s40123-024-00930-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-024-00930-1