Abstract
Introduction
Myopia is recognized as a progressive eye disease. The aim of this study was to evaluate the frequency and associated factors of clinically significant axial length (AL) shortening among myopic children following repeated low-level red light (RLRL) therapy.
Methods
The clinical data that were collected for the myopic children aged 3–17 years who received an RLRL therapy delivered by home-use desktop light device that emitted light at 650 nm for at least 1 year, were reviewed. The clinical data included AL, spherical equivalent refraction (SER), and visual acuity measured at baseline and follow-up. The primary outcomes were frequency of AL shortening of > 0.05 mm, > 0.10 mm, and > 0.20 mm per year, and associated factors of AL shortening per year.
Results
A total of 434 myopic children with at least 12 months of follow-up data were included. The mean age of participants was 9.7 (2.6) years with SER of −3.74 (2.60) diopters. There were 115 (26.50%), 76 (17.51%), and 20 (4.61%) children with AL shortening based on cutoffs of 0.05 mm/year, 0.10 mm/year, and 0.20 mm/year, respectively. In the multivariable model, AL shortening was significantly associated with older baseline age, female gender, and longer baseline AL or greater spherical equivalent refraction (all P < 0.05). Among AL shortened eyes, the mean AL difference (standard deviation, SD) was −0.142 (0.094) mm/year. Greater AL shortening was observed among children who were younger and had longer baseline AL (all P < 0.05).
Conclusions
More than a quarter of children had AL shortening > 0.05 mm following RLRL therapy, and the overall mean AL change was −0.142 mm/year. Further studies should explore the mechanisms underlying AL shortening.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Repeated low-level red light (RLRL) therapy has emerged as a novel therapy for myopia control with unexpected efficacy in axial shortening. |
The effect of RLRL therapy in controlling myopia and shortening axial length in clinical settings remains unclear. |
What was learned from the study? |
In a retrospective study of 434 myopic children, more than a quarter of children had axial shortening > 0.05 mm following RLRL therapy. |
The axial shortening effect of RLRL is confirmed in a real-world setting. |
Introduction
Myopia is characterized by progressive axial elongation and loss of distance vision. It is estimated that it will affect half of the world’s population by 2050, 40% of whom are projected to be high myopia [1, 2]. Axial length (AL) elongation is associated with structural and functional alterations in the eye, which increases the risk of vision-threatening conditions such as macular hemorrhage, retinal detachment, cataracts, and glaucoma [3]. Therefore, AL control is an underlying principle for myopia treatment and preventing vision loss [4, 5].
In infant rhesus monkeys, it has been observed that ocular shape is able to recover, to some extent, from experimentally induced myopia once the myopic stimulus is removed [6,7,8,9,10]. After removing the form deprivation and hyperopic defocus stimulus, elongation of the vitreous chamber would slow down, resulting in AL comparable with that of the contralateral eye [7]. This is consolidated by a meta-analysis, suggesting eye shortening also takes place in non-human primates following myopic defocus, mainly through modulations in vitreous chamber depth [11]. The eyes of tree shrews had a greater proportion of AL recovery compared with other species in response to myopic defocus [11,12,13,14,15,16,17,18]. This reduces the severity of myopia by increasing spherical equivalent of myopia, and therefore reduces the chances of vision-threatening complications.
In humans, the presence of AL shortening following myopia therapies has only rarely been observed [19, 20]. Repeated low-level red light (RLRL) therapy has emerged as an innovative and promising approach for the control of myopia progression [21]. We recently reported the efficacy and safety of RLRL for controlling AL in Chinese children with myopia in a multicenter randomized control trial (RCT), where exposure to RLRL twice daily markedly reduced myopia progression and AL elongation over 1 year [22]. Unexpectedly, a certain proportion of children exhibited AL shortening following RLRL therapy, which is a novel and important finding. Given that the RCT was conducted under strict inclusion and exclusion criteria, the effect of RLRL on AL shortening in real clinical settings with significant population heterogeneity remains unknown. Therefore, a retrospective analysis of RLRL users from 11 hospitals located in six provinces in China were analyzed, with the aim of investigating the frequency and associated factors of AL shortening, as well as its associated factors in clinical settings.
Methods
Study Population
Eleven hospitals that initiated RLRL treatment in 2018 across six Chinese provinces (Fig. 1) were included into the study. These hospitals included one hospital in Henan (Anyang Beiguan Tongtong Ophthalmology Clinic), three in Anhui (the First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China, University Hospital of Science and Technology of China, Huishi Eye Hospital in Hefei City), two in Jiangsu (Li Xiang Eye Hopital Soochow University, Children’s Hospital of Soochow University Ophthalmology), three in Shanghai (Shanghai Aier eye hospital, Shanghai Xinshijie Zhongxing Eye Hospital, Shanghai Heping Eye Hospital), and one in both Hubei (Yichang Huaxia Eye Hospital) and Guangdong provinces (Shenzhen Children’s Hospital).
Myopic children underwent RLRL treatments for at least 12 months, had clinical data available at both baseline and at least one follow-up visit at 12 months onward, aged between 3 and 17 years were included for this study. The myopia was defined as a spherical equivalent refraction (SER) of at least −0.50 diopters (D), and had complete axial length (AL) data. Participants were excluded if they had strabismus, binocular vision abnormalities, other ocular abnormalities or systemic diseases, and history of ocular surgeries (such as laser surgery, high myopia-related surgery, and others). Children who had myopia control treatments other than single-vision spectacles (SVS) in the past such as atropine, orthokeratology, and progressive lens, were also excluded.
Statement of Ethics
This retrospective analysis was approved by the institutional ethics committee of Zhongshan Ophthalmic Centre (2020KYPJ107) and adhered to the Declaration of Helsinki for experimentation on human subjects.
RLRL Therapy
RLRL was purchased/provided free of charge for the duration of the study period and delivered through a desktop light therapy device (Eyerising, Suzhou Xuanjia Optoelectronics Technology, Jiangsu, China) and is widely used in China for amblyopia in children and teenagers [22,23,24,25]. Details of the device are published elsewhere. In brief, the device contained class IIa semiconductor laser diodes that emit low-level red light at a wavelength of 650 ± 10 nm at approximately 100 lux from the pupil to the fundus. The light power going through the pupil is 0.29 mW, which is classified as a class 1 light, safe for direct ocular exposure and would not cause retinal thermic hazard (International electrotechnical commission, 60,825–1:2014 standard) [26]. Myopic children and teenagers and their parents/guardians were instructed to use the RLRL therapy at home under strict supervision by parents or guardians. Children used the device for five days per week, with two treatment sessions per day and 3 min per session. There was an interval of at least 4 h between sessions. During the school semester, Chinese students had the first session of RLRL after getting up (around 6:00–8:00 am) and had the second session of RLRL after school (around 18:00–21:00 pm). During the summer and winter holidays, the RLRL therapy was conducted at morning and afternoon with an interval of at least 4 h. The device was connected to the internet with an automated diary function to record treatment sessions and to monitor patient compliance. Data on the date and time of each login were used to build an online automated diary function, thus providing an accurate measure of compliance with the treatment. If a child was completing fewer than eight sessions per week, the system would alert the trial manager and automatically send the parent or legal guardian a short mobile reminder message to facilitate improvements in treatment compliance. Treatment compliance was calculated based on data from the automated diary function in the device system. Treatment compliance was calculated as a percentage of completed sessions divided by the total number of assigned treatment sessions (two sessions per day, 5 days per week) during the entire treatment period.
Ophthalmic Examinations
Measures of AL were conducted on each eye prior to cycloplegia using an IOL-Master (Carl Zeiss 500/700, Meditec, Oberkochen, Germany), Lenstar (Lenstar LS-900, Haag-Streit AG, Koeniz, Switzerland), or Nidek AL-Scan (Nidek Co., LTD., Tokyo, Japan) depending on the biometry devices that were available and used in each specific hospital. It was mandated that the same device used at baseline for each participant was to be used at follow-up. Cycloplegia was conducted using two drops of 0.5% tropicamide 5 min apart, three times before autorefraction. A pupil size of more than 6 mm and/or the light reflex being absent was considered fully dilated. Autorefraction was measured in each eye using Topcon KR-8800 (Topcon, Tokyo, Japan) or Nidek ARK-900 (Nidek Co., LTD., Tokyo, Japan), and three readings in each eye were taken and averaged until the desired precision (0.25 D for spherical and cylinder power, 5° for axis) was achieved. Cycloplegic spherical equivalent refraction (SER) was defined as the spherical degree plus half of the cylindrical degree.
Definition of Variables
The frequency of significant AL shortening that could not be attributed to measurement error, defined as > 0.05 mm/year (criterion 1), > 0.10 mm/year (criterion 2), and > 0.20 mm/year (criterion 3) was the primary outcome. The secondary outcome was the magnitude of change in AL per year among those with AL shortening based on criteria 1. Baseline age was categorized into seven groups as follows: 3–4, 5–6, 7–8, 9–10, 11–12, 13–14, and 15–17 years. Myopia was classified according to SER, which was categorized as mild (−3.0 < SER ≤ −0.5 D), moderate (−6.0 < SER ≤ −3.0 D), or high (SER ≤ −6.0 D). Axial high myopia was defined when AL ≥26.0 mm.
Statistical Analysis
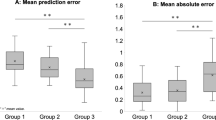
Changes in AL and SER were calculated as the difference between baseline and each follow-up visit. Analyses was performed based on data from each participant’s right eye to exclude intra-individual correlations. Continuous and categorical variables were presented as mean [standard deviation (SD)] or number [percentage (%)], respectively. Frequency of AL shortening under three criteria stratified by age, sex, baseline SER, and baseline AL group were compared with Chi-square or Kruskal–Wallis rank sum tests when appropriate. Scatter plots and box plots described the distribution of AL rate of change, per year over age, sex, baseline AL, and baseline SER groups. Multivariable logistic and linear regression models investigated the relationships between frequency of AL shortening across the three criterion or magnitude of AL change, with baseline factors. Because AL and SER are highly correlated, they were separately included in multivariable models. All statistical analyses were performed using Stata Software 17.0 (StataCorp, College Station, TX, USA). A P value < 0.05 was considered statistically significant.
Results
Baseline Characteristics of Included Subjects
Between 1 January 2018 and 30 July 2020, 477 children received RLRL therapy for at least 1 year, and 43 participants were excluded due to missing data on age or AL (Fig. 1). Finally, 434 subjects were available for inclusion in the present analysis. Table 1 summarizes the baseline demographics and clinical features of the participants included for analysis. There were 234 boys (53.9%) and the mean age at baseline (SD) was 9.7 (2.6) years. The mean (SD) treatment duration was 22.4 (6.0) months. Mean baseline AL and SER were 24.9 (1.20) mm and −3.74 (2.60) D, respectively, and treatment compliance was 81.7% (Table 1).
Frequency of AL Shortening After RLRL Therapy
Following RLRL therapy, 115 (26.50%), 76 (17.51%), and 20 (4.61%) children recorded AL shortening based on cutoffs of 0.05 mm/year, 0.10 mm/year, and 0.20 mm/year, respectively. Table 2 shows the frequency of AL shortening per year stratified by baseline age, sex, SER, and AL. There was a significant increase in the frequency of AL shortening with increasing baseline age, AL, and SER (all P < 0.05). AL shortening was not statistically significant under 0.50 mm/year and 0.10 mm/year cutoffs; however, this was significant in girls under the 0.20 mm/year cutoff (P = 0.028).
Factors Associated with the Presence of AL Shortening
After adjusting for other confounding factors, female gender and longer baseline AL were significantly associated with greater odds of AL shortening in the multivariable model including AL across all three cutoffs (Table 3). Each 1 year increase in age was also significantly associated with AL shortening of 0.05 mm/year, but not for other cutoffs. For the multivariable model including SER, only age and SER at baseline were significantly associated with odds of AL shortening under cutoffs of 0.05 mm/year and 0.10 mm/year (P < 0.05).
Magnitude of AL Shortening after RLRL Therapy
Among those with AL shortening under the 0.05 mm/year cutoff, the mean (SD) magnitude was −0.142 (0.095) mm/year (eTable 1). Younger age was associated with greater magnitude of AL shortening (coefficient = −0.020; 95% CI −0.025 to −0.014; P = 0.003) (eFigure 1), with the magnitude of AL shortening being −0.137 (0.056) mm/year among children aged 15–17 years and −0.271 (0.261) mm/year among children aged 3–5 years (P = 0.010). Figure 2 shows the relationship between AL changes after RLRL therapy and AL at baseline. A significant increase in the magnitude of AL shortening per year was noted with increasing AL at baseline, with a coefficient of −0.044 (95% CI −0.056 to −0.032; P = 0.006). Subgroup analysis based on refractive status showed a greater magnitude of AL shortening among children with high myopia and younger age (eTable 1). The magnitudes of AL shortening per year among those experiencing AL shortening were similar across sex (P = 0.164). The AL parameters were closely correlated to SER parameters (eTable 2).
Factors Associated with the Magnitude of AL Shortening
Greater AL shortening per year was significantly associated with younger age and longer baseline AL in the multivariable model including AL (Table 4). For the multivariable model including SER, younger baseline age and severe myopic refraction were significantly associated with greater AL shortening after adjusting for other factors. Age, sex, AL, and SER could only explain 7.0–9.4% of AL changes. No adverse events have been noted.
Discussion
In this retrospective analysis of a multicenter database, 26.50% of myopic children underwent AL shortening > 0.05 mm per year following over 12 months of RLRL therapy. In addition, 4.61% of participants had AL shortening > 0.20 mm per year. Those who underwent AL shortening had a mean change of −0.142 mm per year, a magnitude that cannot be explained by measurement error produced by optical biometry (< 0.05 mm) [27, 28]. Younger children with longer AL (higher myopia) tended to achieve greater AL shortening from the RLRL therapy. Considering these findings, further studies should investigate the mechanisms underlying the AL shortening following RLRL treatment.
Reports on AL shortening in clinical studies have been considered anomalies in the past due to their uncommon incidence and insignificance in analysis. Of the 37 patients in the retardation of myopia in orthokeratology (ROMIO) study who used orthokeratology (OK) lenses, one patient (2.7%) had an AL shortening of more than 0.10 mm [19], and in the Low-Concentration Atropine for Myopia Progression (LAMP) study, approximately 6% of children who used 0.05% atropine drops over 2 years had an AL shortening of 0.025 mm, although this was too small to exclude measurement error [20]. It is considered AL shortening ≤ 0.05 mm could be attributed to optical biometry measurement errors, which has been the basis for refuting these few cases of AL shortening in the past [27, 28]. Our previous RCT was the first to show consistent AL shortening that was also too large in magnitude to be attributed to measurement error, and 39.8%, 29.2%, 32.9%, and 21.6% myopic children in the RLRL group underwent AL shortening > 0.05 mm at the 1-, 3-, 6-, and 12-month follow-ups, respectively [22]. The current study reinforces findings of the previous RCT in the clinical setting, and reports even higher frequency of AL shortening when treatment duration was more than 12 months (> 0.05 mm in 26.5% of subjects). It appears the inclusion of higher myopes (−3.74 versus −2.49 diopters) in the current study may explain the larger frequency of AL shortening than in the RCT, where high myopes were restricted from study inclusion previously.
Older age was significantly correlated with frequency of AL shortening, whilst magnitude of AL shortening was greater in younger children. In both the LAMP study and Defocus Incorporated Multiple Segments (DIMS) study using spectacle lenses, younger age was identified as a determinant for worse treatment efficacy, and had more volatile treatment response [20, 29]. The DIMS study included children of ages 8–13 years, and reported younger children had greater incidence of progression, with 80% of children aged 8–9 years using DIMS lens experiencing rapid myopia progression [29]. In the LAMP study, younger age was the only factor associated with SE and AL progression with 6 year olds requiring five times the dose of 8 year olds to achieve a similar SE [20]. We speculate that older children have higher degrees of myopia [30], making them more likely to undergo AL shortening with RLRL. Meanwhile, younger children likely have greater scleral plasticity throughout eye development that responds with greater magnitudes to RLRL via AL shortening [31].
Interestingly, we found females experienced AL shortening more frequently, although this was only statistically significant for the > 0.20 mm/year cutoff. The LAMP first-year results found that the natural course of myopia progression was 0.18 D/year faster in females than in males [18]. The girls in Sydney and Guangzhou are more likely to be myopic than boys [32,33,34]. In this study, the girls had trend of greater myopia at baseline than boys (−3.98 ± 2.80 versus −3.53 ± 2.39; P = 0.085), and a greater proportion of high myopia than boys (22.00% versus 17.52%; P = 0.581) (eTable 3). Gender differences may be influenced by the different participation of the sexes in outdoor activities and near work [32]. Further studies with larger sample sizes and behavior data are needed to confirm whether sex influences RLRL efficacy.
A higher frequency and greater magnitude of axial shortening was observed among those with longer baseline AL, suggesting RLRL is efficacious for high myopes. This is a significant finding as the previous study on RLRL prohibited myopes with a SER < −5.0 D from enrolling for treatment, and our analysis observed high myopes were more likely to undergo AL changes > 0.10 and > 0.20 mm.
In addition, with the median AL magnitude among AL-shortened myopes being −0.142 mm, it is difficult to hypothesize whether AL shortening may occur in a dose-dependent manner such that AL eventually returns to an emmetropic range with greater durations of use. Another consideration is the possibility of AL instability among participants, considering they were not closely followed in this study compared with the RCT. While it is possible that AL may fluctuate with RLRL therapy, our previous trial indicates this does not occur. Considering the many questions surrounding efficacy yet to be addressed, future trials with longer treatment durations should confirm whether RLRL has a dose-dependent response, and whether these changes are permanent throughout and after use.
It is unknown how RLRL shortens AL; however, animal models suggest axial shortening is commonly observed if a myopic stimulus is removed [6,7,8, 10,11,12, 14, 15, 18, 35,36,37,38]. Currently, the strongest hypothesis for AL shortening involves the modulation of scleral and choroidal mRNA expression leading to thickening [18, 35, 36, 39]. The choroid is a key structure contributing to myopia onset and progression, with refractive errors from visual signals known to produce changes in choroidal thickness [18, 37]. In our previous RCT, optical coherence tomorapgy (OCT) data proves RLRL is associated with significant CT thickening and likely increases metabolism and choroidal blood flow, which improves scleral hypoxia and restores scleral collagen levels in myopic individuals [22, 24, 40, 41]. Further experimental studies are needed to clarify the key molecular mechanisms of AL shortening from RLRL, which may lead to more effective targets for AL modulation.
Our research highlights RLRL as a promising and novel therapy that can shorten myopic AL in more than 25% of eyes by 0.142 ± 0.095 mm/year. With this level of myopia reversal or AL shortening, RLRL may revert mild myopes to emmetropia, although the frequency and magnitude of AL shortening in mild myopes was not as dramatic as in more severe counterparts. Certainly, RLRL has the propensity to reduce vision-threatening complications of myopia considering its aptitude for treating high myopes, and the choice of treating younger myopes with longer AL may effectively prevent high myopia in children where it was once destined to develop [42]. It should be noted that RLRL in studies outside of control for myopia have found benefits with modulating duration, light pulse or flicker, and energy fluence [43,44,45]. Considering the infancy of RLRL for myopia control, the effect of these factors is yet to be explored but should be considered by future studies wishing to develop RLRL to its full potential.
The strengths of this study include its large sample size, inclusion of study participants with 12 months or greater follow-up data for analysis, and standardized measurements across each study site. Some limitations must also be acknowledged. First, the children included in this study were only of Chinese ethnicity, which is known to have differing rates of myopia and ocular characteristics [46]. Further studies should seek to iterate these findings in multiethnic populations and differing geographic regions. Second, this study design did not allow for the longer-term follow-up of RLRL users, and understanding the long-term impacts of RLRL on axial shortening over time will require a longer follow-up study with thoughtfulness towards the dose, duration, and cessation of therapy. Third, AL was measured by optical biometric devices, which defined AL as the distance from cornea to the retinal pigment epithelium (RPE). AL measurements may be affected by changes in choroidal thickness; however, the consistent results indicate that while choroidal thickness could still be a confounding factor, the reliability and robustness of our findings are clear without this supporting data. Fourth, data on outdoor activities was not available in this retrospective study, but given that time spent outdoor varies greatly across different seasons, it would lead to significant bias to get outdoor activities information in real settings with questionnaires at one timepoint. Future studies are needed to evaluate the combined effect of time spent outdoors and RLRL for myopia controlling. Fifth, there is a lack of OCT data in this study since the data was collected in clinical settings where OCT is not a routine practice.
Finally, the per year reduction estimates are based on 1 year of follow-up information, and so it is not appropriate to view this as an estimate of reduction that will take place in subsequent years.
Conclusions
More than a quarter of children experienced AL shortening following at least 12 months of RLRL therapy in this multicenter cohort. Younger age and longer baseline AL had greater associated benefits that resulted in greater AL shortening following RLRL use. Therefore, RLRL therapy is a proven practical and effective treatment for managing AL elongation and preventing vision-threatening complications that has applications to clinical practice. Future studies should confirm the effect of RLRL in non-Chinese populations and clarify the mechanisms underlying AL shortening.
References:
Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–42.
Baird PN, Saw SM, Lanca C, et al. Myopia. Nat Rev Dis Primers. 2020;6(1):99.
Haarman A, Enthoven CA, Tideman J, et al. The complications of myopia: a review and meta-analysis. Invest Ophthalmol Vis Sci. 2020;61(4):49.
Walline JJ. Myopia control: a review. Eye Contact Lens. 2016;42(1):3–8.
Bullimore MA, Ritchey ER, Shah S, et al. The risks and benefits of myopia control. Ophthalmology. 2021;128(11):1561–79.
Huang J, Hung LF, Smith ER. Recovery of peripheral refractive errors and ocular shape in rhesus monkeys (Macaca mulatta) with experimentally induced myopia. Vis Res. 2012;73:30–9.
Qiao-Grider Y, Hung LF, Kee CS, et al. Recovery from form-deprivation myopia in rhesus monkeys. Invest Ophthalmol Vis Sci. 2004;45(10):3361–72.
Troilo D, Nickla DL. The response to visual form deprivation differs with age in marmosets. Invest Ophthalmol Vis Sci. 2005;46(6):1873–81.
Smith ER, Kee CS, Ramamirtham R, et al. Peripheral vision can influence eye growth and refractive development in infant monkeys. Invest Ophthalmol Vis Sci. 2005;46(11):3965–72.
She Z, Hung LF, Arumugam B, et al. The development of and recovery from form-deprivation myopia in infant rhesus monkeys reared under reduced ambient lighting. Vis Res. 2021;183:106–17.
Zhu X, McBrien NA, Smith ER, et al. Eyes in various species can shorten to compensate for myopic defocus. Invest Ophthalmol Vis Sci. 2013;54(4):2634–44.
Lu F, Zhou X, Jiang L, et al. Axial myopia induced by hyperopic defocus in guinea pigs: a detailed assessment on susceptibility and recovery. Exp Eye Res. 2009;89(1):101–8.
Zhou X, Ye J, Willcox MD, et al. Changes in protein profiles of guinea pig sclera during development of form deprivation myopia and recovery. Mol Vis. 2010;16:2163–74.
Zhou X, Lu F, Xie R, et al. Recovery from axial myopia induced by a monocularly deprived facemask in adolescent (7-week-old) guinea pigs. Vis Res. 2007;47(8):1103–11.
Siegwart JJ, Norton TT. Steady state mRNA levels in tree shrew sclera with form-deprivation myopia and during recovery. Invest Ophthalmol Vis Sci. 2001;42(6):1153–9.
Frost MR, Norton TT. Alterations in protein expression in tree shrew sclera during development of lens-induced myopia and recovery. Invest Ophthalmol Vis Sci. 2012;53(1):322–36.
Grytz R, Siegwart JJ. Changing material properties of the tree shrew sclera during minus lens compensation and recovery. Invest Ophthalmol Vis Sci. 2015;56(3):2065–78.
McBrien NA, Lawlor P, Gentle A. Scleral remodeling during the development of and recovery from axial myopia in the tree shrew. Invest Ophthalmol Vis Sci. 2000;41(12):3713–9.
Cheung SW, Cho P. Validity of axial length measurements for monitoring myopic progression in orthokeratology. Invest Ophthalmol Vis Sci. 2013;54(3):1613–5.
Li FF, Zhang Y, Zhang X, et al. Age effect on treatment responses to 0.05%, 0.025%, and 0.01% atropine: low-concentration atropine for myopia progression study. Ophthalmology. 2021;128(8):1180–7.
Xiong F, Mao T, Liao H, et al. Orthokeratology and low-intensity laser therapy for slowing the progression of myopia in children. Biomed Res Int. 2021;2021:8915867.
Jiang Y, Zhu Z, Tan X, et al. Effect of repeated low-level red-light therapy for myopia control in children: a multicenter randomized controlled trial. Ophthalmology. 2022;129(5):509–19.
Dong J, Zhu Z, Xu H, He M. Myopia control effect of repeated low-level red-light therapy in chinese children: a randomized, double-blind. Control Clin Trial Ophthalmol. 2022. https://doi.org/10.1016/j.ophtha.2022.08.024.
Xiong R, Zhu Z, Jiang Y, et al. Longitudinal changes and predictive value of choroidal thickness for myopia control following repeated low-level red-light therapy. Ophthalmology. 2022. https://doi.org/10.1016/j.ophtha.2022.10.002.
Xiong R, Zhu Z, Jiang Y, et al. Sustained and rebound effect of repeated low-level red-light therapy on myopia control: a 2-year post-trial follow-up study. Clin Exp Ophthalmol. 2022. https://doi.org/10.1111/ceo.14149.
International Electrotechnical Commission %J 3IEC G. IEC 60825-1: 2014 Safety of laser products-Part 1: Equipment classification and requirements. 2014.
Montes-Mico R, Pastor-Pascual F, Ruiz-Mesa R, Tana-Rivero P. Ocular biometry with swept-source optical coherence tomography. J Cataract Refract Surg. 2021;47(6):802–14.
Lee AC, Qazi MA, Pepose JS. Biometry and intraocular lens power calculation. Curr Opin Ophthalmol. 2008;19(1):13–7.
Lam C, Tang WC, Tse DY, et al. Defocus Incorporated Multiple Segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial. Br J Ophthalmol. 2020;104(3):363–8.
He X, Sankaridurg P, Xiong S, et al. Prevalence of myopia and high myopia, and the association with education: Shanghai Child and Adolescent Large-scale Eye Study (SCALE): a cross-sectional study. BMJ Open. 2021;11(12): e48450.
Tano Y. Pathologic myopia: where are we now? Am J Ophthalmol. 2002;134(5):645–60.
Morgan IG, Wu PC, Ostrin LA, et al. IMI risk factors for myopia. Invest Ophthalmol Vis Sci. 2021;62(5):3.
Murthy GV, Gupta SK, Ellwein LB, et al. Refractive error in children in an urban population in New Delhi. Invest Ophthalmol Vis Sci. 2002;43(3):623–31.
Ip JM, Huynh SC, Robaei D, et al. Ethnic differences in refraction and ocular biometry in a population-based sample of 11–15-year-old Australian children. Eye (Lond). 2008;22(5):649–56.
Siegwart JJ, Norton TT. The time course of changes in mRNA levels in tree shrew sclera during induced myopia and recovery. Invest Ophthalmol Vis Sci. 2002;43(7):2067–75.
He L, Frost MR, Siegwart JJ, Norton TT. Gene expression signatures in tree shrew choroid during lens-induced myopia and recovery. Exp Eye Res. 2014;123:56–71.
Gentle A, McBrien NA. Modulation of scleral DNA synthesis in development of and recovery from induced axial myopia in the tree shrew. Exp Eye Res. 1999;68(2):155–63.
Gao H, Frost MR, Siegwart JJ, Norton TT. Patterns of mRNA and protein expression during minus-lens compensation and recovery in tree shrew sclera. Mol Vis. 2011;17:903–19.
Guo L, Frost MR, Siegwart JJ, Norton TT. Gene expression signatures in tree shrew sclera during recovery from minus-lens wear and during plus-lens wear. Mol Vis. 2019;25:311–28.
Zhao F, Zhang D, Zhou Q, et al. Scleral HIF-1alpha is a prominent regulatory candidate for genetic and environmental interactions in human myopia pathogenesis. EBioMedicine. 2020;57: 102878.
Wu H, Chen W, Zhao F, et al. Scleral hypoxia is a target for myopia control. Proc Natl Acad Sci USA. 2018;115(30):E7091–100.
Bullimore MA, Brennan NA. Myopia control: why each diopter matters. Optom Vis Sci. 2019;96(6):463–5.
Gupta AK, Bamimore MA. Factors influencing the effect of photobiomodulation in the treatment of androgenetic alopecia: a systematic review and analyses of summary-level data. Dermatol Ther. 2020;33(6): e14191.
Hashmi JT, Huang YY, Sharma SK, et al. Effect of pulsing in low-level light therapy. Lasers Surg Med. 2010;42(6):450–66.
Muralidharan AR, Lanca C, Biswas S, et al. Light and myopia: from epidemiological studies to neurobiological mechanisms. Ther Adv Ophthalmol. 2021;13:970355154.
Morgan IG, French AN, Ashby RS, et al. The epidemics of myopia: aetiology and prevention. Prog Retin Eye Res. 2017;62:134.
Acknowledgements
We are indebted to the participants who were involved in this trial, without whom the trial would not have been possible.
Funding
This research was supported in part by a grant from the Fundamental Research Funds of the State key Laboratory of 0phthalmology (3030901010058). The journal's Rapid Service fee was funded by grant from the Fundamental Research Funds of the State key Laboratory of 0phthalmology (3030901010058).
Author Contributions
Dr He had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Wang, Jiang, Zhu, Xuan, Zeng, Morgan, He. Acquisition, analysis, or interpretation of data: Wang, Jiang, Zhu, Xuan, Morgan, He. Drafting of the manuscript: Wang, Jiang, Zhu, Zhang, Xuan, Zeng, Morgan, He. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: Wang, Jiang, Zhang, Morgan, He. Obtained funding: He. Administrative, technical, or material support: Jiang, Zhu, Zhang, Tan, Kong, Zhong, Bulloch, Xiong, Yuan, Zhao, Chen, Shi, Jiao, Yan, Feng, Liu, Yan, Jiang, Zeng, He. Study supervision: Morgan, He.
Disclosures
Minguang He and Zhuoting Zhu are inventors on the patents and patent applications related to the study (CN201910490186.6). Minguang He is Director and shareholder in Eyerising Ltd., and Eyerising International Pty Ltd. All other named authors have no conflicts of interest to declare.
Compliance with Ethics Guidelines
This retrospective study was approved by the institutional ethics committee of Zhongshan Ophthalmic Centre (2020KYPJ107) and adhered to the Declaration of Helsinki for experimentation on human subjects.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wang, W., Jiang, Y., Zhu, Z. et al. Clinically Significant Axial Shortening in Myopic Children After Repeated Low-Level Red Light Therapy: A Retrospective Multicenter Analysis. Ophthalmol Ther 12, 999–1011 (2023). https://doi.org/10.1007/s40123-022-00644-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00644-2