Abstract
Introduction
This work aimed to determine the potential link between white matter hyperintensity (WMH) burden and serum amyloid A (SAA) level in patients with acute ischemic stroke.
Methods
Consecutive patients with acute large artery atherosclerosis (LAA) stroke between April 2021 and May 2022 were included. WMH volumes (periventricular, deep, and total) were measured using the Fazekas score and a semiautomated volumetric analysis on fluid-attenuated inversion recovery–magnetic resonance imaging. The burdens of WMH were scored to assess the dose-dependent association between SAA and WMH volume. Multivariate regression and a two-piecewise linear regression model were used to evaluate whether SAA levels are an independent predictor of WMH, and to discover the threshold effect or saturation effect of SAA levels with respect to WMH volume.
Results
The mean age of patients was 63.2 ± 11.5 years, with 65.9% men. The median SAA level was 3.93 mg/L and the total WMH volume of 6.86 cm3. In the multivariable analysis, SAA remained an independent predictor of total WMH volume [β = 0.82, 95% confidence interval (CI) = 0.49–1.07, p < 0.001], periventricular WMH volume (adjusted β = 0.76, 95% CI = 0.46–1.07, p < 0.001), and deep WMH volume (adjusted β = 0.26, 95% CI = 0.06–0.45, p = 0.011) after controlling for confounders. Furthermore, SAA levels were associated with periventricular Fazekas score, deep Fazekas score, and Fazekas grades. Threshold effect and saturation effect analyses demonstrated a nonlinear relationship between SAA levels and periventricular white matter hyperintensity (PVWMH) volumes, with SAA levels (2.12–19.89 mg/L) having significant dose-dependent relationships with periventricular WMH volumes (adjusted β = 1.98, 95% CI = 1.12–2.84, p < 0.001).
Conclusion
SAA level ranging from 2.12 to 19.89 mg/L is dose-dependently associated with periventricular WMH development. These findings point the way forward for future research into the pathophysiology of WMH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Traditional vascular risk factors explain only up to 2% of the white matter hyperintensity (WMH) variance; therefore, elucidating the associated risk factors is important. |
We hypothesized that serum amyloid A (SAA) with pro-inflammatory and pro-atherosclerosis activity is associated with the formation and development of WMH. |
SAA is a predictor of WMH, and the level ranging from 2.12 to 19.89 mg/L is dose-dependently associated with periventricular WMH development. |
These findings point the way forward for future research into the pathophysiology of WMH. |
Introduction
White matter hyperintensity (WMH)—areas of high intensity in the periventricular and deep cerebral white matter on T2-weighted (T2W) or T2 fluid-attenuated inversion recovery images is a common feature of brain magnetic resonance imaging (MRI), particularly in the elderly with vascular risk factors and cerebrovascular disease [1]. Although the pathophysiological mechanism of WMH is not fully understood and may be complex, several researchers have attempted to explain the above phenomenon using data such as atherosclerosis, widespread hypoperfusion, and endothelial dysfunction [1,2,3,4]. Nevertheless, the mechanism underlying the above finding is unknown. Evidence indicates that hypertension, diabetes, smoking, and homocysteine levels are major risk factors for WMH [5]. However, WMH has a significant “non-vascular” component, and standard vascular risk factors explain only up to 2% of the WMH variance [6]. Moreover, restricted randomized control trial data on the influence of traditional risk factors reduction on WMH progression have yielded inconsistent results [7,8,9]. As a result, there is an urgent need to identify additional variables that will add to our understanding of WMH etiology.
Serum amyloid A (SAA) is a small protein family (103–104 amino acids) with significant sequence homology that is increased in acute-phase response and persistently elevated in chronic inflammatory situations [10, 11]. In a recently published study, SAA was revealed as a novel independent predictor of infection after stroke [12]. Epidemiologic studies have demonstrated robust associations of elevated SAA with increased risk of atherosclerosis, rheumatoid arthritis, chronic obstructive pulmonary disease, and tumor [13,14,15,16]. Studies have further linked higher SAA levels to Alzheimer’s dementia and cardiovascular disease, implying that endothelial dysfunction is a primary cause of disease [17,18,19,20]. Endothelial dysfunction has been investigated as a potential cause of WMH [1, 3]. Thus, increased SAA levels may be linked to the formation and development of WMH. However, most previous studies only looked at the relationships between SAA levels and cardiovascular disease in individuals with varying characteristics [17,18,19], and epidemiological data showed that higher SAA is associated with cerebrovascular disease mortality [21]. Few studies have investigated the possible link between SAA levels and cerebrovascular diseases, particularly in WMH of suspected vascular origin.
The purpose of this study was to determine the potential link between the SAA level and WMH in patients with acute ischemic stroke. The SAA levels among individuals with WMH were also analyzed based on their burden to find out more about the underlying pathomechanisms of WMH.
Methods
Patients and Population
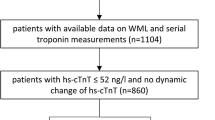
SAA levels may vary in participants with different types of ischemic stroke. To eliminate the impact of this confounding factor, we took it into account and limited the study population to patients with large artery atherosclerosis (LAA) stroke. Consecutive patients with LAA stroke within 72 h after symptom onset between April 2021 and May 2022 were recorded from the electronic medical record in our center (n = 544). Registry discharge diagnoses of acute LAA stroke are > 99% correct, while diagnoses of acute LAA stroke were individually validated by two independent neurologists reviewing medical records. Inclusion criteria were as follows: (1) clinical symptoms, signs, and cranial MRI + brain magnetic resonance angiography (MRA) examination confirmed acute LAA stroke; (2) without intravenous thrombolysis and endovascular treatment due to exceeding the therapeutic time window; and (3) age of the patients ranged from 30 to 80 years. Exclusion criteria were as follows: (1) those with a previous history of Alzheimer’s disease, Parkinson’s disease, psychiatric illness, cerebral amyloid angiopathy, chronic obstructive pulmonary disease, or head injury; (2) complicated with functional failure of heart, kidney, lung, liver, or other important organs; (3) complicated with neoplastic, inflammatory, or autoimmune diseases; (4) complicated with stroke-associated infection; and (5) clinical data collection was incomplete. Finally, participants with stroke-associated infection (n = 53), tumor or autoimmune disease (n = 4), and insufficient MRI image (n = 21) or SAA missing (n = 287) were excluded from the trial. The final analysis included 179 acute LAA stroke subjects having data on brain MRI and SAA inspection findings (Fig. 1). The admission screenings included broad evaluations, including SSA level, brain MRI, brain magnetic resonance angiography (MRA), and laboratory examinations.
Standard Protocol Approvals, Registrations, and Patient Consent
Ethics approval was obtained from the Scientific Research Ethics Committee of the Affiliated Hospital of Jining Medical University (Jining, China) (approval no. 2022C075). All participants provided written informed consent regarding the use of their clinical data and biological samples for scientific research. This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Clinical Assessment
Patient demographics and clinical variables, major vascular risk factors, and laboratory factors were all obtained retrospectively. Laboratory examinations including fasting plasma glucose level, lipid profile, creatinine, homocysteine, and SAA level were also evaluated after 12 h of fasting. To detect SAA levels, venous samples were taken from patients within 24–72 h of onset and were immediately separated by centrifugation (1920g for 15 min). The levels of SAA in serum were then determined using an immunofluorescent antibody method within 2 h of collection. The minimal detection concentration of SAA is 2.0 mg/L, and concentrations less than 2.0 mg/L were statistically analyzed using half of the lower limit values. All clinical and laboratory factors of all participants were comprehensively assessed.
Imaging Assessment
All image acquisitions were performed on 3.0-T magnetic resonance scanners (Philips Ingenia CX, Best, the Netherlands). The following broad MRI acquisitions were acquired: T1-weighted images [repetition time (TR)/echo time (TE) = 250/2.3 ms (ms)], T2-weighted images (TR/TE = 4000/102 ms), T2 fluid-attenuated inversion recovery images (TR/TE = 4800/310 ms), and three-dimensional time-of-flight MRA images (TR/TE = 20/3.45 ms, slice thickness = 1.0 mm). With the exception of the time-of-flight MRA images, the basic slice thickness was 5 mm in the axial plane.
WMHs were identified as variable-sized signal abnormalities in the white matter of the brain that produce a hyperintense signal on FLAIR images [1]. A MIPAV software package (NIH, Bethesda, MD, USA) was used to quantitatively measure the total white matter hyperintensity (TWMH), deep white matter hyperintensity (DWMH), and periventricular white matter hyperintensity (PVWMH) volumes using a previously described semiautomated volumetric analysis method [22]. The deep and periventricular sub-segmentation of WMH was based on the discontinuity of the DWMH, which is not touching the PVWMH, as opposed to the PVWMH, which is in direct contact with the ventricles. PVWMH was defined as WMH in contact with the ventricles that could be followed on two slices above the ventricles. Above this level, WMH was confirmed as DWMH [23]. To avoid the confounding effect caused by the presence of focal white matter damage owing to ischemic stroke, we measured only WMH from the unaffected hemisphere and doubled it to determine the final WMH volume in all patients, which was a validated procedure with strong interhemispheric correlation in WMH severity [24]. We also used a manual rating method based on the Fazekas scale to rate WMH volume [25]. All clinical data, as well as other metrics, were kept hidden from the image analysts. All imaging assessments were reviewed by two well-trained neurologists, and disagreements were settled through consensus.
Statistical Analysis
Continuous variables with normal distributions were expressed as mean ± SD; those with abnormal distributions were presented as median [interquartile range (IQR)]. Continuous variables with skewed distributions were transformed into a log scale or squared root scale. In univariable analyses, we used simple regression analyses for TWMH, DWMH, and PVWMH volume to assess whether SAA is a potential predictor of WMH. In the univariable analyses, variables with p-values < 0.10, as well as for creatinine and homocysteine, were included in the multivariable regression analyses. Next, relationships between TWMH, PVWMH, and DWMH volumes and SAA levels were investigated using multivariable regression models with crude and adjusted β-values and 95% CI in multivariable regression models.
To assess the dose-dependence of the relationships between SAA and WMH volumes, we compared mean SAA levels among individuals with varying loads of TWMH, PVWMH, and DWMH volumes assessed using both the Fazekas score and a semiautomated volumetric analysis. Next, we used a smoothing function and a two-piecewise linear regression model to examine the threshold effect or saturation effect of the log SAA on TWMH, PVWMH, and DWMH volumes. The threshold level or saturation level (e.g., turning point) was confirmed using trial and error, which included selecting turning points along a predefined interval and then selecting turning points that produced the highest model likelihood. This step is relevant to R programming, an additional file shows this in more detail (see the appendix in the electronic supplementary material).
To examine the characteristics of groups with high and low SAA levels, we used the median value to divide the whole cohort into a higher SAA group and a lower SAA group. Next, the Student’s t-test or the Mann–Whitney U test was used to evaluate continuous variables, and the chi-square test or Fisher exact test were used to analyze categorical variables.
SAA level is likely to be affected by the size of infarction volume and the severity of ischemic stroke. To avoid bias caused by differences in the size of infarction volume and the severity of ischemic stroke, we also conducted the following two sensitivity analyses of the study population. Given that all of the participants suffered mild-to-moderate ischemic stroke, patients with a National Institutes of Health Stroke Scale (NIHSS) score > 3 were selected as the study population for sensitivity analysis. Similarly, patients with cerebral infarct volume > 0.9 cm3 were also included in another sensitivity analysis using a median infarct volume of 0.9 cm3 as the cut-off point.
We used multiple imputation, based on five replications and a chained equation approach method in the R MI procedure, to account for missing data. The results of data interpolation were consistent with that of the original data.
All statistical analyses in the study were performed using EmpowerStats version 4.0 (X&Y Solutions, inc. Boston, MA, USA) and R software. Values of p < 0.05 were considered statistically significant.
Results
The final study population included 179 participants (mean age, 63.2 ± 11.5 years; male sex, 65.9%). The median SAA level was 3.93 (2.63–7.29) mg/L. The median volume of TWMH, PVWMH, and DWMH lesions were 6.86 (0.73–16.98) cm3, 6.01 (0.60–12.72) cm3, and 0.80 (0–4.02) cm3, respectively. The baseline characteristics of the cohort are displayed in Table 1. The higher SAA group did not vary from the lower SAA group base on male sex, hypertension, diabetes, current smoking, or a history of a previous stroke, but had higher levels of TWMH, PVWMH, and DWMH volume (Table 2).
After controlling for relevant confounders (age, sex, hypertension, diabetes, hyperlipidemia, history of previous stroke, current smoking, antiplatelet medication, statins, total cholesterol, creatinine, and homocysteine), SAA remained an independent predictor of total WMH volume [β = 0.82; 95% confidence interval (CI) = 0.49–1.16, p < 0.001], periventricular WMH volume (adjusted β = 0.76; 95% CI = 0.46–1.07, p < 0.001), and deep WMH volume ( adjusted β = 0.26; 95% CI = 0.06–0.45, p = 0.011; Tables 3 and 4).
The link between SAA levels and WMH loads was also examined, and correlations were found between SAA levels and the modified Fazekas score in both periventricular (p = 0.004, p for trend < 0.023) and deep (p = 0.001, p for trend = 0.008) areas. A similar trend was demonstrated between SAA levels and the Fazekas grade in total WMH burden (p = 0.001, p for trend < 0.008; Fig. 2).
Distribution of mean values according to the burdens of white matter hyperintensity volume. SAA had positive dose-dependent associations with periventricular Fazekas score (p = 0.001, p for trend < 0.008), deep Fazekas score (p = 0.004, p for trend = 0.023), and Fazekas grade (p = 0.001, p for trend = 0.008). PVWMH periventricular white matter hyperintensity, DWMH deep white matter hyperintensity, TWMH total white matter hyperintensity
Adjusted smoothed plots suggested nonlinear relationships between SAA and TWMH, PVWMH, and DWMH volumes. There were two inflection points between SAA levels and PVWMH volume. With a log SAA < 0.75 (SAA < 2.12 mg/L) and a log SAA ≥ 1.99 (SAA ≥ 19.89 mg/L), the predicted dose-response curve was consistent with a horizontal line. In other words, the relationships between the SAA levels and PVWMH volumes were not statistically significant (p = 0.074 and 0.612, respectively). However, SAA levels ranging from 2.12 to 19.89 mg/L demonstrated a significant correlation between SAA and the PVWMH volume in a dose-dependent manner (adjusted β = 1.98; 95% CI = 1.12–2.84, p < 0.001). Additionally, the TWMH volume increased with the SAA level up to the turning point log SAA < 2.25 (SAA < 9.49 mg/L) (adjusted β = 1.14; 95% CI = 0.70–1.58, p < 0.001). When the log SAA level was ≥ 2.25 (SAA ≥ 9.49) mg/L, the level of SAA was not associated with the TWMH volume (adjusted β = −0.10; 95% CI = −0.98 to 0.78, p = 0.825). Our two-piecewise linear regression model also revealed a significant correlation between SAA and the DWMH volume (adjusted β = 0.46; 95% CI = 0.19–0.74, p = 0.001) at log SAA level < 2.00 (SAA < 7.39 mg/L) (Fig. 3, Table 5).
SAA levels and WMH volumes dose-response relationship. The area between two dotted lines is expressed as a 95% CI. Each point represents the magnitude of the SAA level and is connected to form a continuous line. A SAA and TWMH volumes; B SAA and PWMH volumes; C SAA and DWMH volumes. a: These variables were transformed to square root scale. b: Adjusted for sex, age, hypertension, diabetes, hyperlipidemia, stroke, current smoking, antiplatelet medication, statins, total cholesterol, creatinine, homocysteine. PVWMH periventricular white matter hyperintensity, DWMH deep white matter hyperintensity, TWMH total white matter hyperintensity
In two sensitivity analyses, SAA remained an independent predictor of TWMH volume and PWMH volume in patients with NIHSS scores > 3 or ≤ 3. Similarly, SAA level was still associated with TWMH volume in both the study population with infarct volume > 0.9 cm3 or ≤ 0.9 cm3. In general, SAA level was hardly affected by the severity of ischemic stroke or the size of infarct volume (see Table S1 in the electronic supplementary material for details).
Discussion
In this population-based study, we evaluated the potential association of SAA levels with WMH in an acute ischemic stroke group. These relationships were consistent in dose-dependent studies of WMH volumes within a particular range. As a result, these findings may provide useful information for future research into the pathophysiology of WMH.
The current investigation found that higher SAA levels were independently associated with total WMH, implying that dysregulated SAA may play a role in the etiology of overall WMH. However, the bulk of prior investigations has focused on the association of other plasma inflammatory markers [including, total homocysteine (tHcy), hypersensitive-C reactive protein (hs-CRP), vascular cell adhesion molecule-1 (VCAM-1), E-selection, and P-selection] with total WMH burden [26,27,28]. Few researchers have focused on the impact of different variables on PVWHM and DWMH. Also, the possible mechanisms by which this occurs are unclear. In this view, we are unsure whether SAA levels differentiate between PVWMH and DWMH. Moreover, academic circles have not agreed on a unified standard of the definition of PVWMH and DWMH lesions, or on the WMH rating scaling procedure, which may explain the past inconsistency. One widely accepted theory is that PVWMH and DWMH have unique histopathological and etiological features [1, 29, 30]. PVWMH is related to changes in the short penetrating microvessels that end close to larger arterial blood vessels [1, 31,32,33]. They are thought to be more directly influenced by hypertension and traditional risk factors for stroke [33,34,35]. DWMH lesion occurs in the subcortical areas, which are primarily supplied by long microvessels, and may be damaged as a result of hypertension and the possibility of subsequent hypoperfusion, which is ischemic in nature [33,34,35,36]. In our study, we found that higher SAA levels were associated with higher PVWMH and DWMH volumes. The relationships between SAA levels and DWMH volumes were slightly weakened after controlling for covariates but remained statistically significant. Unlike previous genetic studies that found PVWMH and DWMH to have distinct genetic foundations, implying separate etiologies [37], our findings show that there is no difference in the location of the effect of SAA levels on WMH development. An increasing body of evidence that SAA has many pro-inflammatory and pro-atherogenic activities may explain this phenomenon [13].
Postmortem testing indicates that PVWMH has a nonischemic discontinuous ependymal loss, loosening of the white matter fibers, and loss of myelin [4, 29, 31], implying that microvascular dysfunction is important in the formation and development of PVWMH. A growing body of research suggests that high SAA levels are both directly and indirectly linked to endothelial dysfunction by stimulating endothelial cell migration and proliferation [38]. To understand the strong association between the SAA level and PVWMH, we proposed different endothelial dysfunction-related theories. One widely accepted cause is the loss of blood–brain barrier (BBB) function. It was shown that increased SAA levels induced the expression of adhesion molecules such as intercellular adhesion molecule-1 (ICAM1), VCAM1, and E-selectin in human endothelial cells, as well as stimulated endothelial cell migration and proliferation, resulting in functional suppression of the BBB [38,39,40]. The functional collapse of the BBB may result in the perivascular infiltration of hazardous elements (e.g., protease, immunoglobulin, and complement components) into brain tissues. These events would lead to the formation and development of PVWMH [3, 41].
In contrast, postmortem examination of the DWMH reveals more multiple tiny vacuolations, varied axonal loss, and increased tissue loss in more severe lesions, indicating potential arteriosclerosis and microcystic infarction in addition to demyelination and gliosis [4, 29, 31]. Although the particular processes are unknown, there is substantial evidence that SAA plays a causal role in atherosclerosis [13]. Initially, SAA can activate the NOD-like receptor pyrin domain-containing 3 (NLRP3) inflammasome in macrophages, which may explain its range of effects [42]. Furthermore, we discovered that the presence of SAA on apoB-lipoproteins increased their proteoglycan binding affinity [43], which is an important step in the start of atherosclerosis [44]. A retrospective clinical study found that SAA levels were highly linked to blood coagulability and thrombosis [45]. In summary, subcortical areas hypoperfusion caused by atherosclerosis would eventually result in DWMH. It can be concluded that higher SAA levels have different impacts on PVWMH and DWMH via various mechanisms, which is consistent with the findings of our multivariate regression analysis.
A recent cross-sectional investigation revealed that the WMH volume, particularly PVWMH, follows a nonlinear quadratic polynomial model with a remarkable elevation between the ages of 50 and 60 years [46]. In women, the relationship between serum-free hemoglobin level and PVWMH volume was U-shaped [47]. These findings imply that there is no simple linear relationship between WMH volume and its associated risk factors. As far as we know, our study also found a consistent and independent relationship between the SAA level and PVWMH volume, which is also a nonlinear relationship. According to the two-piecewise linear regression model, SAA levels ranging from 2.12 to 19.82 mg/L demonstrated a significant correlation with PVWMH volume. This highlights the idea that comparing SAA levels to standard WMH risk factors screening could give a more accurate means of identifying patients at risk for WMH.
Although our research incorporates several novel discoveries, we acknowledge that our study has some limitations. First, SAA, as an inflammatory marker, may drive the neuroinflammatory response after acute ischemic stroke. In a group of 1176 stroke-free subjects drawn from the same underlying population as part of a prospective cohort study among stroke patients, the mean log (SAA) was not higher among stroke patients than stroke-free participants. Moreover, there was no evidence of a time trend in levels of SAA during the 28 days of follow-up. The random effect model has demonstrated that SAA level was not associated with stroke severity, which was also consistent with the results of our sensitivity analysis [48]. In summary, first, the SAA level was hardly affected by acute ischemic stroke. In comparison, we acknowledge that the evaluation of SAA level in healthy individuals with WMH burden should have provided a better interpretation of the presumed association. Second, while we have described relationships between SAA levels and cerebral WMHs, we lack conclusive evidence that increased SAA is a risk factor for WMH burden. Also, because our study is cross-sectional and does not infer causation, future prospective studies are needed to address this issue. Third, our sample size of 179 participants was rather smaller in comparison to previous research on WMH volume and other risk variables. Therefore, after we reached our conclusion, we used the simulated statistical efficiency module of the EmpowerStats software to calculate whether the sample size was reasonable. The results of statistical analysis demonstrated that the sample size of the current study may not be optimal, but should be sufficient to draw a conclusion that may guide clinical practice (see Fig. S1 in the electronic supplementary material for details). Fourth, our study was absence of a control arm, which cannot eliminate the influence of relevant confounding factors. Next, we will conduct a 3-year prospective cohort study in a healthy population to assess whether SAA level is an independent risk factor for WMH burden. Fifth, we cannot rule out the possibility that high SAA levels are an epiphenomenon of other pathologic conditions such as possible infection or a chronic inflammatory state. Although individuals with suspicious clinical infections or inflammatory diseases were excluded, the selection bias remains. Finally, it may also have affected the concentration that the collection time point of SAA was different for different patients. To remove this effect, we attempted to minimize the difference in collection time point. However, this factor should be considered.
Conclusion
We demonstrated that a higher SAA level is independently associated with the development of WMH in an acute ischemic stroke group. Furthermore, these correlations were detected in a dose-dependent manner within a limited range of SAA levels. These findings, therefore, point the way forward for future research into the pathophysiology of WMH and potentially cerebrovascular diseases. Nevertheless, our conclusions must be confirmed in larger prospective studies in the future.
References
Wardlaw JM, Smith C, Dichgans M. Mechanisms of sporadic cerebral small vessel disease: insights from neuroimaging. Lancet Neurol. 2013;12(5):483–97.
Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 2010;9(7):689–701.
Wardlaw JM. Blood–brain barrier and cerebral small vessel disease. J Neurol Sci. 2010;299(1–2):66–71.
Schmidt R, Schmidt H, Haybaeck J, Loitfelder M, Weis S, Cavalieri M, et al. Heterogeneity in age-related white matter changes. Acta Neuropathol. 2011;122(2):171–85.
Launer LJ. Epidemiology of white matter lesions. Top Magn Reson Imaging. 2004;15(6):365–7.
Wardlaw JM, Allerhand M, Doubal FN, Valdes Hernandez M, Morris Z, Gow AJ, et al. Vascular risk factors, large-artery atheroma, and brain white matter hyperintensities. Neurology. 2014;82(15):1331–8.
Dufouil C, Chalmers J, Coskun O, Besancon V, Bousser MG, Guillon P, et al. Effects of blood pressure lowering on cerebral white matter hyperintensities in patients with stroke: the PROGRESS (Perindopril Protection Against Recurrent Stroke Study) magnetic resonance imaging substudy. Circulation. 2005;112(11):1644–50.
Weber R, Weimar C, Blatchford J, Hermansson K, Wanke I, Moller-Hartmann C, et al. Telmisartan on top of antihypertensive treatment does not prevent progression of cerebral white matter lesions in the prevention regimen for effectively avoiding second strokes (PRoFESS) MRI substudy. Stroke. 2012;43(9):2336–42.
Launer LJ, Miller ME, Williamson JD, Lazar RM, Gerstein HC, Murray AM, et al. Effects of intensive glucose lowering on brain structure and function in people with type 2 diabetes (ACCORD MIND): a randomised open-label substudy. Lancet Neurol. 2011;10(11):969–77.
Tannock LR, De Beer MC, Ji A, Shridas P, Noffsinger VP, den Hartigh L, et al. Serum amyloid A3 is a high density lipoprotein-associated acute-phase protein. J Lipid Res. 2018;59(2):339–47.
Kisilevsky R, Manley PN. Acute-phase serum amyloid A: perspectives on its physiological and pathological roles. Amyloid. 2012;19(1):5–14.
Schweizer J, Bustamante A, Lapierre-Fetaud V, Faura J, Scherrer N, Azurmendi Gil L, et al. SAA (serum amyloid A): a novel predictor of stroke-associated infections. Stroke. 2020;51(12):3523–30.
Shridas P, Tannock LR. Role of serum amyloid A in atherosclerosis. Curr Opin Lipidol. 2019;30(4):320–5.
Ciregia F, Nys G, Cobraiville G, Badot V, Di Romana S, Sidiras P, et al. A cross-sectional and longitudinal study to define alarmins and A-SAA variants as companion markers in early rheumatoid arthritis. Front Immunol. 2021;12: 638814.
Lin TL, Chen WW, Ding ZR, Wei SC, Huang ML, Li CH. Correlations between serum amyloid A, C-reactive protein and clinical indices of patients with acutely exacerbated chronic obstructive pulmonary disease. J Clin Lab Anal. 2019;33(4): e22831.
He LN, Fu S, Zhang X, Hu Q, Du W, Li H, et al. Baseline and early changes in circulating serum amyloid A (SAA) predict survival outcomes in advanced non-small cell lung cancer patients treated with anti-PD-1/PD-L1 monotherapy. Lung Cancer. 2021;158:1–8.
Johnson BD, Kip KE, Marroquin OC, Ridker PM, Kelsey SF, Shaw LJ, et al. Serum amyloid A as a predictor of coronary artery disease and cardiovascular outcome in women: the national heart, lung, and blood institute-sponsored women’s ischemia syndrome evaluation (WISE). Circulation. 2004;109(6):726–32.
Hua S, Song C, Geczy CL, Freedman SB, Witting PK. A role for acute-phase serum amyloid A and high-density lipoprotein in oxidative stress, endothelial dysfunction and atherosclerosis. Redox Rep. 2009;14(5):187–96.
Ridker PM, Hennekens CH, Buring JE, Rifai N. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med. 2000;342(12):836–43.
Cao X, Chen P. Changes in serum amyloid A (SAA) and 8-OHdG in patients with senile early cognitive impairment. Med Sci Monit. 2020;26: e919586.
Mayer FJ, Binder CJ, Krychtiuk KA, Schillinger M, Minar E, Hoke M. The prognostic value of serum amyloid A for long-term mortality among patients with subclinical carotid atherosclerosis. Eur J Clin Invest. 2019;49: e13095.
Rost NS, Rahman RM, Biffi A, Smith EE, Kanakis A, Fitzpatrick K, et al. White matter hyperintensity volume is increased in small vessel stroke subtypes. Neurology. 2010;75(19):1670–7.
Charidimou A, Boulouis G, Haley K, Auriel E, van Etten ES, Fotiadis P, et al. White matter hyperintensity patterns in cerebral amyloid angiopathy and hypertensive arteriopathy. Neurology. 2016;86(6):505–11.
Gurol ME, Irizarry MC, Smith EE, Raju S, Diaz-Arrastia R, Bottiglieri T, et al. Plasma beta-amyloid and white matter lesions in AD, MCI, and cerebral amyloid angiopathy. Neurology. 2006;66(1):23–9.
Nam KW, Kwon HM, Jeong HY, Park JH, Kim SH, Jeong SM, et al. Cerebral white matter hyperintensity is associated with intracranial atherosclerosis in a healthy population. Atherosclerosis. 2017;265:179–83.
Zhang DD, Cao Y, Mu JY, Liu YM, Gao F, Han F, et al. Inflammatory biomarkers and cerebral small vessel disease: a community-based cohort study. Stroke Vasc Neurol. 2022;7:302–4.
Nam KW, Kwon HM, Jeong HY, Park JH, Kwon H, Jeong SM. Serum homocysteine level is related to cerebral small vessel disease in a healthy population. Neurology. 2019;92(4):e317–25.
Avci AY, Lakadamyali H, Arikan S, Benli US, Kilinc M. High sensitivity C-reactive protein and cerebral white matter hyperintensities on magnetic resonance imaging in migraine patients. J Headache Pain. 2015;16:9.
Kim KW, MacFall JR, Payne ME. Classification of white matter lesions on magnetic resonance imaging in elderly persons. Biol Psychiatry. 2008;64(4):273–80.
Vermeer SE, van Dijk EJ, Koudstaal PJ, Oudkerk M, Hofman A, Clarke R, et al. Homocysteine, silent brain infarcts, and white matter lesions: The Rotterdam Scan Study. Ann Neurol. 2002;51(3):285–9.
Wardlaw JM, Valdes Hernandez MC, Munoz-Maniega S. What are white matter hyperintensities made of? Relevance to vascular cognitive impairment. J Am Heart Assoc. 2015;4(6): 001140.
Griffanti L, Jenkinson M, Suri S, Zsoldos E, Mahmood A, Filippini N, et al. Classification and characterization of periventricular and deep white matter hyperintensities on MRI: a study in older adults. Neuroimage. 2018;170:174–81.
Wardlaw JM, Smith EE, Biessels GJ, Cordonnier C, Fazekas F, Frayne R, et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 2013;12(8):822–38.
Blanco PJ, Muller LO, Spence JD. Blood pressure gradients in cerebral arteries: a clue to pathogenesis of cerebral small vessel disease. Stroke Vasc Neurol. 2017;2(3):108–17.
Fernando MS, Simpson JE, Matthews F, Brayne C, Lewis CE, Barber R, et al. White matter lesions in an unselected cohort of the elderly: molecular pathology suggests origin from chronic hypoperfusion injury. Stroke. 2006;37(6):1391–8.
De Reuck J. The human periventricular arterial blood supply and the anatomy of cerebral infarctions. Eur Neurol. 1971;5(6):321–34.
Armstrong NJ, Mather KA, Sargurupremraj M, Knol MJ, Malik R, Satizabal CL, et al. Common genetic variation indicates separate causes for periventricular and deep white matter hyperintensities. Stroke. 2020;51(7):2111–21.
Cai X, Freedman SB, Witting PK. Serum amyloid A stimulates cultured endothelial cells to migrate and proliferate: inhibition by the multikinase inhibitor BIBF1120. Clin Exp Pharmacol Physiol. 2013;40(9):662–70.
Nishida E, Aino M, Kobayashi SI, Okada K, Ohno T, Kikuchi T, et al. Serum amyloid A promotes E-selectin expression via toll-like receptor 2 in human aortic endothelial cells. Mediators Inflamm. 2016;2016:7150509.
Bowman GL, Dayon L, Kirkland R, Wojcik J, Peyratout G, Severin IC, et al. Blood–brain barrier breakdown, neuroinflammation, and cognitive decline in older adults. Alzheimers Dement. 2018;14(12):1640–50.
Hassan A, Hunt BJ, O’Sullivan M, Parmar K, Bamford JM, Briley D, et al. Markers of endothelial dysfunction in lacunar infarction and ischaemic leukoaraiosis. Brain. 2003;126(Pt 2):424–32.
Shridas P, De Beer MC, Webb NR. High-density lipoprotein inhibits serum amyloid A-mediated reactive oxygen species generation and NLRP3 inflammasome activation. J Biol Chem. 2018;293(34):13257–69.
Wilson PG, Thompson JC, Shridas P, McNamara PJ, de Beer MC, de Beer FC, et al. Serum amyloid A is an exchangeable apolipoprotein. Arterioscler Thromb Vasc Biol. 2018;38(8):1890–900.
Thompson JC, Jayne C, Thompson J, Wilson PG, Yoder MH, Webb N, et al. A brief elevation of serum amyloid A is sufficient to increase atherosclerosis. J Lipid Res. 2015;56(2):286–93.
Deguchi H, Elias DJ, Navarro S, Espana F, Griffin JH. Elevated serum amyloid A is associated with venous thromboembolism. Thromb Haemost. 2013;109(2):358–9.
Huang CC, Yang AC, Chou KH, Liu ME, Fang SC, Chen CC, et al. Nonlinear pattern of the emergence of white matter hyperintensity in healthy Han Chinese: an adult lifespan study. Neurobiol Aging. 2018;67:99–107.
Oh DJ, Kim JS, Lee S, Yang HW, Bae JB, Han JW, et al. Association between serum free hemoglobin level and cerebral white matter hyperintensity volume in older adults. Sci Rep. 2022;12(1):3296.
Elkind MS, Coates K, Tai W, Paik MC, Boden-Albala B, Sacco RL. Levels of acute phase proteins remain stable after ischemic stroke. BMC Neurol. 2006;16:6–37.
Acknowledgements
The magnetic resonance parameter information was collected by Yanting Wang, from the department of radiology, Affiliated Hospital of Jining Medical University.
Funding
Funding for this study, including funding the journal’s Rapid Service, was provided by a grant from the National Nature Science Foundation of China (grant number: 81901228) and a grant from the Health Commission of Shandong Province (grant number: 2021-QLJQ-003), and a grant from the Jining Science and Technology Bureau (2019SMNS002). The funding source had no role in the study design, data collection, data analysis, data interpretation, writing of the manuscript, or decision to submit it for publication.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Daojing Li revised the content of the manuscript and took responsibility for the integrity of the data and the accuracy of the data analysis; Peng Zhang and Rongrong Han drafted the manuscript and formulated the research protocols and plans; Aimei Zhang, Hao Yu, and Ziheng Zhang were responsible for the analysis of imaging data; Xiaohong Zhang, Hongfang Li, Peng Xu, and Ziyou Qi took charge in the acquisition of clinical data; Peng Yang made statistical analysis of all available data.
Disclosures
Peng Zhang, Rongrong Han, Aimei Zhang, Xiaohong Zhang, Ziheng Zhang, HaoYu, Hongfang Li, Ziyou Qi, Peng Xu, Peng Yang, and Daojing Li declare that they have nothing to disclose regarding the content of this article.
Compliance with Ethics Guidelines
This study was performed in compliance with the Helsinki Declaration of 1964 and its later amendments. Ethics approval was obtained from the Scientific Research Ethics Committee of the Affiliated Hospital of Jining Medical University (Jining, China) (approval no. 2022C075). All participants provided written informed consent regarding the use of their clinical data and biological samples for scientific research.
Data Availability
Data supporting the findings of this study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Zhang, P., Han, R., Zhang, A. et al. Association between Serum Amyloid A Level and White Matter Hyperintensity Burden: a Cross-Sectional Analysis in Patients with Acute Ischemic Stroke. Neurol Ther 12, 161–175 (2023). https://doi.org/10.1007/s40120-022-00415-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-022-00415-y