Abstract
Purpose
Campylobacter bloodstream infection (C-BSI) is uncommon, and its clinical significance is unclear. The aim of the study was to determine risk factors and clinical outcomes associated with Campylobacter BSI.
Methods
We performed a single center retrospective case–control study comparing patients with C-BSI (cases) and patients with nonbacteremic Campylobacter enteritis (controls), from January 2007 through June 2020. Case and control patients were matched by age and sex at a ratio of 1:2. Demographic, clinical, and microbiological characteristics were compared between groups.
Results
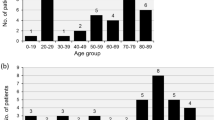
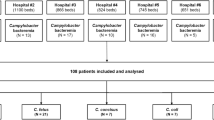
We identified 76 patients with C-BSI and matched them with 149 nonbacteremic patients with Campylobacter enteritis. Rates of C-BSI increased tenfold in 2014 following the introduction of BacTAlert FA/FN Plus blood culture bottles. Baseline variables significantly associated with C-BSI on multivariable logistic regression were fever, absence of diarrhea and recent exposure to antibiotics. Compared with controls, C-BSI was associated with higher 30-day mortality (12% vs. 2%, P = 0.003), more frequent need for intensive care (6.6% vs. 1.2%, P = 0.032) and longer hospital stay (median, 5 days vs. 3 days, P = 0.003). There was a high proportion of immunocompromised patients in both groups (55%).
Conclusions
C-BSI is identified with increasing frequency, reflecting both changes in epidemiology and improved sensitivity of blood culture systems. Our findings indicate that detection of Campylobacter spp. in blood culture is associated with significantly higher rates of death and other adverse outcomes.



Similar content being viewed by others
References
Skirrow MB, Jones DM, Sutcliffe E, Benjamin J. Campylobacter bacteraemia in England and Wales, 1981–91. Epidemiol Infect. 1993;110:567–73.
Nielsen H, Hansen KK, Gradel KO, et al. Bacteraemia as a result of Campylobacter species: a population-based study of epidemiology and clinical risk factors. Clin Microbiol Infect. 2010;16:57–61.
Feodoroff B, Lauhio A, Ellstrom P, Rautelin H. A nationwide study of Campylobacter jejuni and Campylobacter coli bacteremia in Finland over a 10-year period, 1998–2007, with special reference to clinical characteristics and antimicrobial susceptibility. Clin Infect Dis. 2011;53:e99–106.
Guerrant RL, Lahita RG, Winn WC Jr, Roberts RB. Campylobacteriosis in man: pathogenic mechanisms and review of 91 bloodstream infections. Am J Med. 1978;65:584–92.
Montero A, Corbella X, Lopez JA, Santin M, Ballon IH. Campylobacter fetus-associated aneurysms: report of a case involving the popliteal artery and review of the literature. Clin Infect Dis. 1997;24:1019–21.
Farrugia DC, Eykyn SJ, Smyth EG. Campylobacter fetus endocarditis: two case reports and review. Clin Infect Dis. 1994;18:443–6.
Hussein K, Raz-Pasteur A, Shachor-Meyouhas Y, et al. Campylobacter bacteraemia: 16 years of experience in a single centre. Infect Dis (Lond). 2016;48:796–9.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Clinical Laboratory Standards Institute. Methods for antimicrobial dilution and disk susceptibility testing of infrequently isolated or fastidious bacteria. 3rd edition. CLSI guideline M45. Wayne: Clinical Laboratory Standards Institute; 2016.
Health Mo. Central laboratory report (Hebrew). Jerusalem: Ministry of Health, 2021.
Harvala H, Ydring E, Brytting M, et al. Increased number of Campylobacter bacteraemia cases in Sweden, 2014. Clin Microbiol Infect. 2016;22:391–3.
Lovern D, Katzin B, Johnson K, et al. Antimicrobial binding and growth kinetics in BacT/ALERT® FA Plus and BACTEC® Aerobic/F Plus blood culture media. Eur J Clin Microbiol Infect Dis. 2016;35:2033–6.
BacT/Alert. http://www.biomerieux-usa.com. Accessed 4 Aug 2021.
Wang WL, Blaser MJ. Detection of pathogenic Campylobacter species in blood culture systems. J Clin Microbiol. 1986;23:709–14.
Tee W, Mijch A. Campylobacter jejuni bacteremia in human immunodeficiency virus (HIV)-infected and non-HIV-infected patients: comparison of clinical features and review. Clin Infect Dis. 1998;26:91–6.
Zhou SJ, Wang SQ, Ma YY, et al. Association of proton pump inhibitors with the occurrence of gut-derived bacteraemia in patients with haematological malignancy after chemotherapy. Hematology. 2016;21:332–7.
Pigrau C, Bartolome R, Almirante B, Planes AM, Gavalda J, Pahissa A. Bacteremia due to Campylobacter species: clinical findings and antimicrobial susceptibility patterns. Clin Infect Dis. 1997;25:1414–20.
Rokney A, Valinsky L, Vranckx K, et al. WGS-based prediction and analysis of antimicrobial resistance in Campylobacter jejuni isolates from Israel. Front Cell Infect Microbiol. 2020;10:365.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Tau, L., Adler, A., Shalom, O. et al. Clinical features and outcomes of bacteremic and non-bacteremic Campylobacteriosis: a case–control study. Infection 50, 1225–1231 (2022). https://doi.org/10.1007/s15010-022-01798-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-022-01798-8