Abstract
Objectives
In this study, we examined whether epilepsy and drug-resistant epilepsy are associated with neuroimaging findings in children with cerebral palsy (CP).
Methods
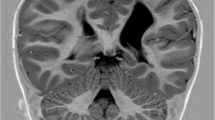
Magnetic resonance imaging classification system (MRICS) proposed by Surveillance of Cerebral Palsy in Europe (SCPE) was used for classification of different MRI patterns in patients with cerebral palsy. We reviewed the brain MRI scans and medical records of children with CP who were followed-up in our clinic between 2019 and 2023. Patients were divided into three categories: CP without epilepsy, CP with controlled epilepsy and CP with DRE. MRI patterns were grouped as maldevelopments, predominant white matter injury, predominant gray matter injury, miscellaneous (delayed myelination, cerebral atrophy, cerebellar atrophy, brainstem lesions and calcifications, lesions that were not classified under any other group) and normal according to MRICS of the SCPE.
Results
There were 325 CP patients. The most common MRI patterns were predominant white matter injury (47.6%) and gray matter injury (23.8%). There was a 1.5-fold reduction in the risk of epilepsy in patients with predominant white matter injury (OR = 1.54, 95% CI 1.23–1.94). In contrast, children in the miscellaneous group had significantly higher risks of epilepsy (p < 0.001), and we were able to determine that miscellaneous findings increased the risk by 1.8 times (OR = 1.77, 95% CI 1.47–2.12).
Conclusion
In conclusion, more than half of the children with CP had epilepsy, 40.7% of whom had DRE. On MRI, miscellaneous findings may indicate a poor prognosis for epilepsy, while predominant white matter injury may indicate a good outcome. Children with CP, especially those with miscellaneous findings on MRI, should be closely monitored for epilepsy development.

Similar content being viewed by others
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Michael-Asalu A, Taylor G, Cmpbell H, Lelea LL, Kirby RS (2019) Cerebral palsy: diagnosis, epidemiology, genetics, and clinical update. Adv Pediatr 334:189–208
Sadowska M, Sarecka-Hujar B, Kopyta I (2020) Cerebral palsy: current opinions on definition, epidemiology, risk factors, classification and treatment options. Neuropsychiatr Dis Treat 16:1505–1518
Ashwal S, Russman BS, Blasco PA, Miller G, Sandler A, Shevell M et al (2004) Practice parameter: diagnostic assessment of the child with cerebral palsy: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology 62:851–863
Graham HK, Rosenbaum P, Paneth N, Dan B, Lin JP, Damiano DL et al (2016) Cerebral palsy. Nat Rev Dis Primers 2:15082
Hadjipanayis A, Hadjichristodoulou C, Youroukos S (1997) Epilepsy in patients with cerebral palsy. Dev Med Child Neurol 39(10):659–663
Hollung SJ, Bakken IJ, Vik T, Lydersen S, Wiik R, Aaberg KM et al (2020) Comorbidities in cerebral palsy: a patient registry study. Dev Med Child Neurol 62(1):97–103
Kwong KL, Wong SN, So KT (1998) Epilepsy in children with cerebral palsy. Pediatr Neurol 19(1):31–36
Pahlman M, Gillberg C, Himmelmann K (2019) One-third of school-aged children with cerebral palsy have neuropsychiatric impairments in a population-based study. Acta Paediatr 108(11):2048–2055
Sellier E, Uldall P, Calado E, Sigurdardottir S, Torrioli MG, Platt MJ et al (2012) Epilepsy and cerebral palsy: characteristics and trends in children born in 1976–1998. Eur J Paediatr Neurol 16(1):48–55
Sadowska M, Sarecka-Hujar B, Kopyta I (2020) Evaluation of risk factors for epilepsy in pediatric patients with cerebral palsy. Brain Sci 10(8):481
Mert GG, Incecik F, Altunbasak S, Herguner O, Mert MK, Kiris N et al (2011) Factors affecting epilepsy development and epilepsy prognosis in cerebral palsy. Pediatr Neurol 45:89–94
Kulak W, Sobaniec W (2003) Risk factors and prognosis of epilepsy in children with cerebral palsy in north-eastern Poland. Brain Dev 27:499–506
Mohammadzadeh P, Nazarbaghi S (2022) The prevalence of drug-resistant-epilepsy and its associated factors in patients with epilepsy. Clin Neurol and Neurosurg 213:107086
Carlsson M, Olsson I, Hagberg G, Beckung E (2008) Behavior in children with cerebral palsy with and without epilepsy. Dev Med Child Neurol 50:784–789
Sander JW (2005) Ultimate success in epilepsy–the patient’s perspective. Eur J Neurol 12(Suppl 4):3–11
Himmelmann K, Horber V, De La Cruz J, Horridge K, Mejaski-Bosnjak V, Hollody K et al (2017) MRI classification system (MRICS) for children with cerebral palsy: development, reliability, and recommendations. Dev Med Child Neurol 59(1):57–64
Krägeloh-Mann I, Horber V (2007) The role of magnetic resonance imaging in elucidating the pathogenesis of cerebral palsy: a systematic review. Dev Med Child Neurol 49(2):144–151
Towsley K, Shevell MI, Dagenais L, REPACQ Consortium (2011) Population-based study of neuroimaging findings in children with cerebral palsy. Eur J Paediatr Neurol 15:29–35
Korzeniewski SJ, Birbeck G, DeLano MC, Potchen MJ, Paneth N (2008) A systematic review of neuroimaging for cerebral palsy. J Child Neurol 23:216–227
Novak I, Morgan C, Adde L, Blackman J, Boyd RN, Brunstrom-Hernandez J et al (2017) Early, accurate diagnosis and early intervention in cerebral palsy: advances in diagnosis and treatment. JAMA Pediatr 171:897–907
Liptak GS, Murphy NA (2011) Providing a primary care medical home for children and youth with cerebral palsy. Pediatrics 128:e1321–e1329
Korzeniewski SJ, Slaughter J, Lenski M, Haak P, Paneth N et al (2018) The complex aetiology of cerebral palsy. Nat Rev Neurol 14:528–543
Reid SM, Dagia CD, Ditchfield MR, Carlin JB, Meehan EM, Reddihough DS (2013) An Australian population study of factors associated with MRI patterns in cerebral palsy. Dev Med Child Neurol 56:178–184
Numata Y, Onuma A, Kobayashi Y, Sato-Shirai I, Tanaka S, Kobayashi S et al (2012) Brain magnetic resonance imaging and motor and intellectual functioning in 86 patients born at term with spastic diplegia. Dev Med Child Neurol 55:167–172
Horber V, Sellier E, Horridge K, Rackauskaite G, Andersen GL, Virella D (2020) The origin of the cerebral palsies: contribution of population-based neuroimaging data. Neuropediatrics 51(2):113–119
Fisher RS, Acevedo C, Arzimanoglou A, Bogacz A, Cross JH, Elger CHE et al (2014) ILAE official report: a practical clinical definition of epilepsy. Epilepsia 55:475–482
Kwan P, Arzimanoglou A, Berg AT, Brodie MJ, Allen Hauser W, Mathern G et al (2010) Definition of drug resistant epilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia 51(6):1069–1077
Téllez-Zenteno JF, Hernández-Ronquillo L, Buckley S, Zahagun R, Rizvi S (2014) A validation of the new dfinition of drug-resistant epilepsy by the International League Against Epilepsy. Epilepsia 55(6):829–834
Laxer KD, Trinka E, Hirsch LJ, Cendes F, Langfitt J, Delanty N et al (2014) The consequences of refractory epilepsy and its treatment. Epilepsy Behav 37:59–70
Löscher W, Potschka H, Sisodiya SM, Vezzani A (2020) Drug resistance in epilepsy: clinical impact, potential mechanisms, and new innovative treatment options. Pharmacol Rev 72(3):606–638
Zafeiriou DI, Kontopoulos EE, Tsikoulas I (1999) Characteristics and prognosis of epilepsy in children with cerebral palsy. J Child Neurol 14:289–294
Hanci F, Türay S, Dilek M, Kabakuş N (2020) Epilepsy and drug-resistant epilepsy in children with cerebral palsy: a retrospective observational study. Epilepsy Behav 112:107357
Tokatly Latzer I, Blumovich A, Sagi L, Uliel-Sibony S, Fattal-Valevski A (2020) Prediction of drug-resistant eilepsy in children with cerebral palsy. J Child Neurol 35(3):187–194
Nagy E, Herbert Z, Péter I, Csorba E, Skobrák A, Farkas N et al (2020) The usefulness of MRI classification system (MRICS) in a cerebral palsy cohort. Acta Paediatr 109(12):2783–2788
Himmelmann K, Horber V, Sellier E, De la Cruz J, Papavasiliou A, Krägeloh-Mann I, Surveillance of Cerebral Palsy in Europe (SCPE) Collaboration (2021) Neuroimaging patterns and function in cerebral palsy-application of an MRI classification. Front Neurol 11:617740
Carlsson M, Hagberg G, Olsson I (2003) Clinical and aetiological aspects of epilepsy in children with cerebral palsy. Dev Med Child Neurol 45(6):371–376
Horber V, Grasshoff U, Sellier E, Arnaud C, Krägeloh-Mann I, Himmelmann K (2021) The role of neuroimaging and genetic analysis in the diagnosis of children with cerebral palsy. Front Neurol 11:628075
Nolan D, Fink J (2018) Genetics of epilepsy. Handb Clin Neurol 148:467–491
Perucca P, Bahlo M, Berkovic SF (2020) The genetics of epilepsy. Annu Rev Genomics Hum Genet 21:205–230
Author information
Authors and Affiliations
Contributions
All authors have seen and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No author has a potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kilic, M.A., Yildiz, E.P., Kurekci, F. et al. Association of epilepsy with neuroimaging patterns in children with cerebral palsy. Acta Neurol Belg 124, 567–572 (2024). https://doi.org/10.1007/s13760-023-02385-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-023-02385-w