Abstract
Purpose of Review
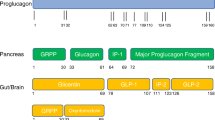
Although Glucagon-like peptide (GLP)-1 receptor agonists have been used for almost two decades in the treatment of diabetes mellitus type 2 and, lately, in obesity, recent years have seen an increasing interest in the pharmacological agonism of other proglucagon-derived peptides, including GLP-2. Herein, we aimed to review the available evidence on the effects of GLP-2 agonism from animal and clinical studies. Furthermore, we summarize the current clinical applications of GLP-2 agonists among patients with intestinal failure associated with short bowel syndrome (SBS-IF) as well as potential future expansion of their indications to other intestinal disorders.
Recent Findings
Evidence from preclinical studies has highlighted the cellular trophic and functional beneficial actions of GLP-2 on small intestinal and colonic mucosa. Subsequently, pharmacologic agonism of GLP-2 has gathered interest for the treatment of patients with conditions pertaining to the loss of intestinal anatomical and/or functional integrity to a degree requiring parenteral support, collectively referred to as intestinal failure. GLP-2 analogs positively influence nutrient absorption in animal models and humans, although continued therapy is likely needed for sustained effects. The degradation-resistant GLP-2-analog teduglutide has received approval for the treatment of SBS-IF, in which it may decisively reduce patient dependency on parenteral support and improve quality of life. Another two longer-acting analogs, glepaglutide and apraglutide, are currently undergoing phase III clinical trials.
Summary
The use of GLP-2 analogs is effective in the management of SBS-IF and may show promise in the treatment of other severe gastrointestinal disorders associated with loss of effective intestinal resorptive surface area.


Similar content being viewed by others
Abbreviations
- Anti-TNFα:
-
Anti-tumor necrosis factor-α
- Anti-IL12 and anti-IL23:
-
Anti-interleukin-12 and anti-interleukin-23
- c-AMP:
-
Cyclic adenosine monophosphate
- CD:
-
Crohn’s disease
- CDAI:
-
Crohn’s Disease Activity Index
- DNA:
-
Deoxy-ribonucleic acid
- DPP-4:
-
Dipeptidyl peptidase-4
- EGF:
-
Epidermal growth factor
- ESPEN:
-
European Society for Clinical Nutrition and Metabolism
- GE:
-
Gastric emptying
- GI:
-
Gastrointestinal
- GLP-2:
-
Glucagon-like peptide-2
- GLP-2R:
-
Glucagon-like peptide 2 receptor
- GIP:
-
Glucose-dependent insulinotropic polypeptide
- GRPP:
-
Glicentin-related pancreatic peptide
- IBD:
-
Inflammatory bowel disease
- IGF-1:
-
Insulin-like growth factor-1
- IVS:
-
Intravenous supplementation
- KGF:
-
Keratinocyte growth factor
- nNOS:
-
Neuronal nitric oxide synthase
- PC:
-
Pro-hormone convertase
- PGDP:
-
Pro-glucagon-derived peptide
- PKA:
-
Protein kinase A
- PS:
-
Parenteral support
- QoL:
-
Quality of life
- SBS-IF:
-
Short bowel syndrome-intestinal failure
- SC:
-
Subcutaneous
- SGLT-1:
-
Sodium-glucose transporter-1
- T2DM:
-
Diabetes mellitus type 2
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Seige K. Glucagon, its discovery and description and the work of Max Burger. Z Gesamte Inn Med. 1986;41:568–71.
Bromer WW, Sinn LG, Staub A, Behrens OK. The amino acid sequence of glucagon. Diabetes. 1957;6:234–8. https://doi.org/10.2337/diab.6.3.234.
Lafferty RA, O’Harte FPM, Irwin N, Gault VA, Flatt PR. Proglucagon-derived peptides as therapeutics. Front Endocrinol (Lausanne). 2021;12: 689678. https://doi.org/10.3389/fendo.2021.689678.
Heine RJ, Van Gaal LF, Johns D, Mihm MJ, Widel MH, Brodows RG, et al. Exenatide versus insulin glargine in patients with suboptimally controlled type 2 diabetes: a randomized trial. Ann Intern Med. 2005;143:559–69. https://doi.org/10.7326/0003-4819-143-8-200510180-00006.
Sjolund K, Sanden G, Hakanson R, Sundler F. Endocrine cells in human intestine: an immunocytochemical study. Gastroenterology. 1983;85:1120–30.
Baggio LL, Drucker DJ. Biology of incretins: GLP-1 and GIP. Gastroenterology. 2007;132:2131–57. https://doi.org/10.1053/j.gastro.2007.03.054.
Kuhre RE, Deacon CF, Holst JJ, Petersen N. What is an L-cell and how do we study the secretory mechanisms of the L-cell? Front Endocrinol (Lausanne). 2021;12: 694284. https://doi.org/10.3389/fendo.2021.694284.
Billiauws L, Joly F. Emerging treatments for short bowel syndrome in adult patients. Expert Rev Gastroenterol Hepatol. 2019;13:241–6. https://doi.org/10.1080/17474124.2019.1569514.
Austin K, Markovic MA, Brubaker PL. Current and potential therapeutic targets of glucagon-like peptide-2. Curr Opin Pharmacol. 2016;31:13–8. https://doi.org/10.1016/j.coph.2016.08.008.
Berkowitz DE, Steenbergen C, O’Rourke B. Hibernating squirrels: SIRTin clues for organ protection after ischemia-reperfusion. Anesthesiology. 2016;124:1215–7. https://doi.org/10.1097/ALN.0000000000001114.
Drucker DJ, Yusta B. Physiology and pharmacology of the enteroendocrine hormone glucagon-like peptide-2. Annu Rev Physiol. 2014;76:561–83. https://doi.org/10.1146/annurev-physiol-021113-170317.
Rowland KJ, Brubaker PL. The “cryptic” mechanism of action of glucagon-like peptide-2. Am J Physiol Gastrointest Liver Physiol. 2011;301:G1-8. https://doi.org/10.1152/ajpgi.00039.2011.
Yusta B, Holland D, Koehler JA, Maziarz M, Estall JL, Higgins R, et al. ErbB signaling is required for the proliferative actions of GLP-2 in the murine gut. Gastroenterology. 2009;137:986–96. https://doi.org/10.1053/j.gastro.2009.05.057.
Austin K, Imam NA, Pintar JE, Brubaker PL. IGF binding protein-4 is required for the growth effects of glucagon-like peptide-2 in murine intestine. Endocrinology. 2015;156:429–36. https://doi.org/10.1210/en.2014-1829.
Van Landeghem L, Santoro MA, Mah AT, Krebs AE, Dehmer JJ, McNaughton KK, et al. IGF1 stimulates crypt expansion via differential activation of 2 intestinal stem cell populations. FASEB J. 2015;29:2828–42. https://doi.org/10.1096/fj.14-264010.
Iturrino J, Camilleri M, Acosta A, O’Neill J, Burton D, Edakkanambeth Varayil J, et al. Acute effects of a glucagon-like peptide 2 analogue, teduglutide, on gastrointestinal motor function and permeability in adult patients with short bowel syndrome on home parenteral nutrition. JPEN J Parenter Enteral Nutr. 2016;40:1089–95. https://doi.org/10.1177/0148607115597644.
Bremholm L, Hornum M, Andersen UB, Hartmann B, Holst JJ, Jeppesen PB. The effect of glucagon-like peptide-2 on mesenteric blood flow and cardiac parameters in end-jejunostomy short bowel patients. Regul Pept. 2011;168:32–8. https://doi.org/10.1016/j.regpep.2011.03.003.
Berg JK, Kim EH, Li B, Joelsson B, Youssef NN. A randomized, double-blind, placebo-controlled, multiple-dose, parallel-group clinical trial to assess the effects of teduglutide on gastric emptying of liquids in healthy subjects. BMC Gastroenterol. 2014;14:25. https://doi.org/10.1186/1471-230X-14-25.
Cani PD, Possemiers S, Van de Wiele T, Guiot Y, Everard A, Rottier O, et al. Changes in gut microbiota control inflammation in obese mice through a mechanism involving GLP-2-driven improvement of gut permeability. Gut. 2009;58:1091–103. https://doi.org/10.1136/gut.2008.165886.
Dong CX, Zhao W, Solomon C, Rowland KJ, Ackerley C, Robine S, et al. The intestinal epithelial insulin-like growth factor-1 receptor links glucagon-like peptide-2 action to gut barrier function. Endocrinology. 2014;155:370–9. https://doi.org/10.1210/en.2013-1871.
Gonzalez-Mariscal L, Betanzos A, Nava P, Jaramillo BE. Tight junction proteins. Prog Biophys Mol Biol. 2003;81:1–44. https://doi.org/10.1016/s0079-6107(02)00037-8.
Hartmann B, Harr MB, Jeppesen PB, Wojdemann M, Deacon CF, Mortensen PB, et al. In vivo and in vitro degradation of glucagon-like peptide-2 in humans. J Clin Endocrinol Metab. 2000;85:2884–8. https://doi.org/10.1210/jcem.85.8.6717.
Drucker DJ, Shi Q, Crivici A, Sumner-Smith M, Tavares W, Hill M, et al. Regulation of the biological activity of glucagon-like peptide 2 in vivo by dipeptidyl peptidase IV. Nat Biotechnol. 1997;15:673–7. https://doi.org/10.1038/nbt0797-673.
Ferrone M, Scolapio JS. Teduglutide for the treatment of short bowel syndrome. Ann Pharmacother. 2006;40:1105–9. https://doi.org/10.1345/aph.1G419.
Naimi RM, Hvistendahl M, Enevoldsen LH, Madsen JL, Fuglsang S, Poulsen SS, et al. Glepaglutide, a novel long-acting glucagon-like peptide-2 analogue, for patients with short bowel syndrome: a randomised phase 2 trial. Lancet Gastroenterol Hepatol. 2019;4:354–63. https://doi.org/10.1016/S2468-1253(19)30077-9.
Eliasson J, Hvistendahl MK, Freund N, Bolognani F, Meyer C, Jeppesen PB. Apraglutide, a novel glucagon-like peptide-2 analog, improves fluid absorption in patients with short bowel syndrome intestinal failure: findings from a placebo-controlled, randomized phase 2 trial. JPEN J Parenter Enteral Nutr. 2021. https://doi.org/10.1002/jpen.2223.
Kocoshis SA, Merritt RJ, Hill S, Protheroe S, Carter BA, Horslen S, et al. Safety and efficacy of teduglutide in pediatric patients with intestinal failure due to short bowel syndrome: a 24-week, phase III study. JPEN J Parenter Enteral Nutr. 2020;44:621–31. https://doi.org/10.1002/jpen.1690.
Hvistendahl MK, Naimi RM, Enevoldsen LH, Madsen JL, Fuglsang S, Jeppesen PB. Effect of glepaglutide, a long-acting glucagon-like peptide-2 analog, on gastrointestinal transit time and motility in patients with short bowel syndrome: findings from a randomized trial. JPEN J Parenter Enteral Nutr. 2020;44:1535–44. https://doi.org/10.1002/jpen.1767.
Hargrove DM, Alagarsamy S, Croston G, Laporte R, Qi S, Srinivasan K, et al. Pharmacological characterization of apraglutide, a novel long-acting peptidic glucagon-like peptide-2 agonist, for the treatment of short bowel syndrome. J Pharmacol Exp Ther. 2020;373:193–203. https://doi.org/10.1124/jpet.119.262238.
Cheeseman CI, Tsang R. The effect of GIP and glucagon-like peptides on intestinal basolateral membrane hexose transport. Am J Physiol. 1996;271:G477–82. https://doi.org/10.1152/ajpgi.1996.271.3.G477.
Brubaker PL. Glucagon-like peptide-2 and the regulation of intestinal growth and function. Compr Physiol. 2018;8:1185–210. https://doi.org/10.1002/cphy.c170055.
Dahly EM, Gillingham MB, Guo Z, Murali SG, Nelson DW, Holst JJ, et al. Role of luminal nutrients and endogenous GLP-2 in intestinal adaptation to mid-small bowel resection. Am J Physiol Gastrointest Liver Physiol. 2003;284:G670–82. https://doi.org/10.1152/ajpgi.00293.2002.
Dash S, Xiao C, Morgantini C, Connelly PW, Patterson BW, Lewis GF. Glucagon-like peptide-2 regulates release of chylomicrons from the intestine. Gastroenterology. 2014;147:1275–84 e4. https://doi.org/10.1053/j.gastro.2014.08.037.
Schwartz LK, O’Keefe SJ, Fujioka K, Gabe SM, Lamprecht G, Pape UF, et al. Long-term teduglutide for the treatment of patients with intestinal failure associated with short bowel syndrome. Clin Transl Gastroenterol. 2016;7: e142. https://doi.org/10.1038/ctg.2015.69.
Lee SJ, Lee J, Li KK, Holland D, Maughan H, Guttman DS, et al. Disruption of the murine Glp2r impairs Paneth cell function and increases susceptibility to small bowel enteritis. Endocrinology. 2012;153:1141–51. https://doi.org/10.1210/en.2011-1954.
Benjamin MA, McKay DM, Yang PC, Cameron H, Perdue MH. Glucagon-like peptide-2 enhances intestinal epithelial barrier function of both transcellular and paracellular pathways in the mouse. Gut. 2000;47:112–9. https://doi.org/10.1136/gut.47.1.112.
Sigalet DL, de Heuvel E, Wallace L, Bulloch E, Turner J, Wales PW, et al. Effects of chronic glucagon-like peptide-2 therapy during weaning in neonatal pigs. Regul Pept. 2014;188:70–80. https://doi.org/10.1016/j.regpep.2013.12.006.
Zaczek Z, Jurczak-Kobus P, Panczyk M, Braszczynska-Sochacka J, Majewska K, Kunecki M, et al. Changes in parenteral nutrition requirements and BMI in patients with parenteral nutrition-dependent short bowel syndrome after stopping teduglutide-9 years of follow-up. Nutrients. 2022;14. https://doi.org/10.3390/nu14081634.
Pironi L, Arends J, Baxter J, Bozzetti F, Pelaez RB, Cuerda C, et al. ESPEN endorsed recommendations. Definition and classification of intestinal failure in adults. Clin Nutr. 2015;34:171–80. https://doi.org/10.1016/j.clnu.2014.08.017.
Billiauws L, Corcos O, Joly F. What’s new in short bowel syndrome? Curr Opin Clin Nutr Metab Care. 2018;21:313–8. https://doi.org/10.1097/MCO.0000000000000473.
Goulet O, Abi Nader E, Pigneur B, Lambe C. Short bowel syndrome as the leading cause of intestinal failure in early life: some insights into the management. Pediatr Gastroenterol Hepatol Nutr. 2019;22:303–29. https://doi.org/10.5223/pghn.2019.22.4.303.
Lim DW, Levesque CL, Vine DF, Muto M, Koepke JR, Nation PN, et al. Synergy of glucagon-like peptide-2 and epidermal growth factor coadministration on intestinal adaptation in neonatal piglets with short bowel syndrome. Am J Physiol Gastrointest Liver Physiol. 2017;312:G390–404. https://doi.org/10.1152/ajpgi.00281.2016.
Rowland KJ, Trivedi S, Lee D, Wan K, Kulkarni RN, Holzenberger M, et al. Loss of glucagon-like peptide-2-induced proliferation following intestinal epithelial insulin-like growth factor-1-receptor deletion. Gastroenterology. 2011;141:2166–75 e7. https://doi.org/10.1053/j.gastro.2011.09.014.
Burrin DG, Stoll B, Guan X, Cui L, Chang X, Hadsell D. GLP-2 rapidly activates divergent intracellular signaling pathways involved in intestinal cell survival and proliferation in neonatal piglets. Am J Physiol Endocrinol Metab. 2007;292:E281–91. https://doi.org/10.1152/ajpendo.00129.2006.
Jeppesen PB, Gilroy R, Pertkiewicz M, Allard JP, Messing B, O’Keefe SJ. Randomised placebo-controlled trial of teduglutide in reducing parenteral nutrition and/or intravenous fluid requirements in patients with short bowel syndrome. Gut. 2011;60:902–14. https://doi.org/10.1136/gut.2010.218271.
Reiner J, Berlin P, Wobar J, Schaffler H, Bannert K, Bastian M, et al. Teduglutide promotes epithelial tight junction pore function in murine short bowel syndrome to alleviate intestinal insufficiency. Dig Dis Sci. 2020;65:3521–37. https://doi.org/10.1007/s10620-020-06140-6.
Pauline ML, Nation PN, Wizzard PR, Hinchliffe T, Wu T, Dimitriadou V, et al. Comparing the intestinotrophic effects of 2 glucagon-like peptide-2 analogues in the treatment of short-bowel syndrome in neonatal piglets. JPEN J Parenter Enteral Nutr. 2021;45:538–45. https://doi.org/10.1002/jpen.1853.
Slim GM, Lansing M, Wizzard P, Nation PN, Wheeler SE, Brubaker PL, et al. Novel long-acting GLP-2 analogue, FE 203799 (apraglutide), enhances adaptation and linear intestinal growth in a neonatal piglet model of short bowel syndrome with total resection of the ileum. JPEN J Parenter Enteral Nutr. 2019;43:891–8. https://doi.org/10.1002/jpen.1500.
Suri M, Turner JM, Sigalet DL, Wizzard PR, Nation PN, Ball RO, et al. Exogenous glucagon-like peptide-2 improves outcomes of intestinal adaptation in a distal-intestinal resection neonatal piglet model of short bowel syndrome. Pediatr Res. 2014;76:370–7. https://doi.org/10.1038/pr.2014.97.
Burness CB, McCormack PL. Teduglutide: a review of its use in the treatment of patients with short bowel syndrome. Drugs. 2013;73:935–47. https://doi.org/10.1007/s40265-013-0070-y.
•• Rosete BE, Wendel D, Horslen SP. Teduglutide for pediatric short bowel syndrome patients. Expert Rev Gastroenterol Hepatol. 2021;15:727–33. https://doi.org/10.1080/17474124.2021.1913052. Expert review regarding the usefulness of teduglytide for short bowel syndrome in pediatric patients.
Seidner DL, Gabe SM, Lee HM, Olivier C, Jeppesen PB. Enteral autonomy and days off parenteral support with teduglutide treatment for short bowel syndrome in the STEPS trials. JPEN J Parenter Enteral Nutr. 2020;44:697–702. https://doi.org/10.1002/jpen.1687.
Chen K, Mu F, Xie J, Kelkar SS, Olivier C, Signorovitch J, et al. Impact of teduglutide on quality of life among patients with short bowel syndrome and intestinal failure. JPEN J Parenter Enteral Nutr. 2020;44:119–28. https://doi.org/10.1002/jpen.1588.
Pape UF, Iyer KR, Jeppesen PB, Kunecki M, Pironi L, Schneider SM, et al. Teduglutide for the treatment of adults with intestinal failure associated with short bowel syndrome: pooled safety data from four clinical trials. Therap Adv Gastroenterol. 2020;13:1756284820905766. https://doi.org/10.1177/1756284820905766.
Podolsky DK. Inflammatory bowel disease. N Engl J Med. 2002;347:417–29. https://doi.org/10.1056/NEJMra020831.
Buhner S, Buning C, Genschel J, Kling K, Herrmann D, Dignass A, et al. Genetic basis for increased intestinal permeability in families with Crohn’s disease: role of CARD15 3020insC mutation? Gut. 2006;55:342–7. https://doi.org/10.1136/gut.2005.065557.
D’Haens G, Baert F, van Assche G, Caenepeel P, Vergauwe P, Tuynman H, et al. Early combined immunosuppression or conventional management in patients with newly diagnosed Crohn’s disease: an open randomised trial. Lancet. 2008;371:660–7. https://doi.org/10.1016/S0140-6736(08)60304-9.
Blonski W, Buchner AM, Aberra F, Lichtenstein G. Teduglutide in Crohn’s disease. Expert Opin Biol Ther. 2013;13:1207–14. https://doi.org/10.1517/14712598.2013.815721.
Feagan BG, Sandborn WJ, Gasink C, Jacobstein D, Lang Y, Friedman JR, et al. Ustekinumab as induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2016;375:1946–60. https://doi.org/10.1056/NEJMoa1602773.
Sandborn WJ, Feagan BG, Rutgeerts P, Hanauer S, Colombel JF, Sands BE, et al. Vedolizumab as induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2013;369:711–21. https://doi.org/10.1056/NEJMoa1215739.
Fragkos KC, Forbes A. Citrulline as a marker of intestinal function and absorption in clinical settings: a systematic review and meta-analysis. United European Gastroenterol J. 2018;6:181–91. https://doi.org/10.1177/2050640617737632.
• Buchman AL, Katz S, Fang JC, Bernstein CN, Abou-Assi SG, Teduglutide Study G. Teduglutide, a novel mucosally active analog of glucagon-like peptide-2 (GLP-2) for the treatment of moderate to severe Crohn’s disease. Inflamm Bowel Dis. 2010;16:962–73. https://doi.org/10.1002/ibd.21117. This is the first manuscript regarding the therapeutic potential of GLP-2 analogs among patients with severe Crohn’s disease.
Tavakkolizadeh A, Shen R, Abraham P, Kormi N, Seifert P, Edelman ER, et al. Glucagon-like peptide 2: a new treatment for chemotherapy-induced enteritis. J Surg Res. 2000;91:77–82. https://doi.org/10.1006/jsre.2000.5917.
Pini A, Garella R, Idrizaj E, Calosi L, Baccari MC, Vannucchi MG. Glucagon-like peptide 2 counteracts the mucosal damage and the neuropathy induced by chronic treatment with cisplatin in the mouse gastric fundus. Neurogastroenterol Motil. 2016;28:206–16. https://doi.org/10.1111/nmo.12712.
•• Nardini P, Pini A, Bessard A, Duchalais E, Niccolai E, Neunlist M, et al. GLP-2 prevents neuronal and glial changes in the distal colon of mice chronically treated with cisplatin. Int J Mol Sci. 2020;21. https://doi.org/10.3390/ijms21228875. This report highlights the therapeutic potential of GLP-2 analogs in a rodent model of chemotherapy-induced gastrointestinal damage.
Zhang T, Shi L, Xu Y, Li Y, Li S, Guan B, et al. Purified PEGylated human glucagon-like peptide-2 reduces the severity of irradiation-induced acute radiation enteritis in rats. J Radiat Res. 2019;60:7–16. https://doi.org/10.1093/jrr/rry076.
Torres S, Thim L, Milliat F, Vozenin-Brotons MC, Olsen UB, Ahnfelt-Ronne I, et al. Glucagon-like peptide-2 improves both acute and late experimental radiation enteritis in the rat. Int J Radiat Oncol Biol Phys. 2007;69:1563–71. https://doi.org/10.1016/j.ijrobp.2007.08.051.
Tack J, Arts J, Caenepeel P, De Wulf D, Bisschops R. Pathophysiology, diagnosis and management of postoperative dumping syndrome. Nat Rev Gastroenterol Hepatol. 2009;6:583–90. https://doi.org/10.1038/nrgastro.2009.148.
Wauters L, Vanuytsel T. Applications of peptide hormone ligands for the treatment of dumping and short bowel syndrome. Curr Opin Pharmacol. 2018;43:118–23. https://doi.org/10.1016/j.coph.2018.09.005.
Scarpellini E, Arts J, Karamanolis G, Laurenius A, Siquini W, Suzuki H, et al. International consensus on the diagnosis and management of dumping syndrome. Nat Rev Endocrinol. 2020;16:448–66. https://doi.org/10.1038/s41574-020-0357-5.
van Furth AM, de Heide LJM, Emous M, Veeger N, van Beek AP. Dumping syndrome and postbariatric hypoglycemia: supporting evidence for a common etiology. Surg Obes Relat Dis. 2021;17:1912–8. https://doi.org/10.1016/j.soard.2021.05.020.
Abrahamsson N, Engstrom BE, Sundbom M, Karlsson FA. GLP1 analogs as treatment of postprandial hypoglycemia following gastric bypass surgery: a potential new indication? Eur J Endocrinol. 2013;169:885–9. https://doi.org/10.1530/EJE-13-0504.
Ding B, Hu Y, Yuan L, Yan RN, Ma JH. Effectiveness of beinaglutide in a patient with late dumping syndrome after gastrectomy: a case report. Medicine (Baltimore). 2021;100: e26086. https://doi.org/10.1097/MD.0000000000026086.
Marier JF, Beliveau M, Mouksassi MS, Shaw P, Cyran J, Kesavan J, et al. Pharmacokinetics, safety, and tolerability of teduglutide, a glucagon-like peptide-2 (GLP-2) analog, following multiple ascending subcutaneous administrations in healthy subjects. J Clin Pharmacol. 2008;48:1289–99. https://doi.org/10.1177/0091270008320605.
Jeppesen PB, Gabe SM, Seidner DL, Lee HM, Olivier C. Factors associated with response to teduglutide in patients with short-bowel syndrome and intestinal failure. Gastroenterology. 2018;154:874–85. https://doi.org/10.1053/j.gastro.2017.11.023.
Jeppesen PB, Pertkiewicz M, Messing B, Iyer K, Seidner DL, O'Keefe S J, et al. Teduglutide reduces need for parenteral support among patients with short bowel syndrome with intestinal failure. Gastroenterology. 2012;143:1473–81 e3. https://doi.org/10.1053/j.gastro.2012.09.007.
Hill S, Carter BA, Cohran V, Horslen S, Kaufman SS, Kocoshis SA, et al. Safety findings in pediatric patients during long-term treatment with teduglutide for short-bowel syndrome-associated intestinal failure: pooled analysis of 4 clinical studies. JPEN J Parenter Enteral Nutr. 2021;45:1456–65. https://doi.org/10.1002/jpen.2061.
Billiauws L, Bataille J, Boehm V, Corcos O, Joly F. Teduglutide for treatment of adult patients with short bowel syndrome. Expert Opin Biol Ther. 2017;17:623–32. https://doi.org/10.1080/14712598.2017.1304912.
Carroll RE, Benedetti E, Schowalter JP, Buchman AL. Management and complications of short bowel syndrome: an updated review. Curr Gastroenterol Rep. 2016;18:40. https://doi.org/10.1007/s11894-016-0511-3.
Jeppesen PB. The novel use of peptide analogs in short bowel syndrome. Expert Rev Gastroenterol Hepatol. 2013;7:197–9. https://doi.org/10.1586/egh.13.2.
Jeppesen PB, Pertkiewicz M, Forbes A, Pironi L, Gabe SM, Joly F, et al. Quality of life in patients with short bowel syndrome treated with the new glucagon-like peptide-2 analogue teduglutide–analyses from a randomised, placebo-controlled study. Clin Nutr. 2013;32:713–21. https://doi.org/10.1016/j.clnu.2013.03.016.
Bortvedt SF, Lund PK. Insulin-like growth factor 1: common mediator of multiple enterotrophic hormones and growth factors. Curr Opin Gastroenterol. 2012;28:89–98. https://doi.org/10.1097/MOG.0b013e32835004c6.
Tsai CH, Hill M, Drucker DJ. Biological determinants of intestinotrophic properties of GLP-2 in vivo. Am J Physiol. 1997;272:G662–8. https://doi.org/10.1152/ajpgi.1997.272.3.G662.
Brubaker PL, Izzo A, Hill M, Drucker DJ. Intestinal function in mice with small bowel growth induced by glucagon-like peptide-2. Am J Physiol. 1997;272:E1050–8. https://doi.org/10.1152/ajpendo.1997.272.6.E1050.
Litvak DA, Hellmich MR, Evers BM, Banker NA, Townsend CM Jr. Glucagon-like peptide 2 is a potent growth factor for small intestine and colon. J Gastrointest Surg. 1998;2:146–50. https://doi.org/10.1016/s1091-255x(98)80005-x.
Scott RB, Kirk D, MacNaughton WK, Meddings JB. GLP-2 augments the adaptive response to massive intestinal resection in rat. Am J Physiol. 1998;275:G911–21. https://doi.org/10.1152/ajpgi.1998.275.5.G911.
Burrin DG, Stoll B, Jiang R, Petersen Y, Elnif J, Buddington RK, et al. GLP-2 stimulates intestinal growth in premature TPN-fed pigs by suppressing proteolysis and apoptosis. Am J Physiol Gastrointest Liver Physiol. 2000;279:G1249–56. https://doi.org/10.1152/ajpgi.2000.279.6.G1249.
Guan X, Stoll B, Lu X, Tappenden KA, Holst JJ, Hartmann B, et al. GLP-2-mediated up-regulation of intestinal blood flow and glucose uptake is nitric oxide-dependent in TPN-fed piglets 1. Gastroenterology. 2003;125:136–47. https://doi.org/10.1016/s0016-5085(03)00667-x.
Martin GR, Wallace LE, Sigalet DL. Glucagon-like peptide-2 induces intestinal adaptation in parenterally fed rats with short bowel syndrome. Am J Physiol Gastrointest Liver Physiol. 2004;286:G964–72. https://doi.org/10.1152/ajpgi.00509.2003.
Washizawa N, Gu LH, Gu L, Openo KP, Jones DP, Ziegler TR. Comparative effects of glucagon-like peptide-2 (GLP-2), growth hormone (GH), and keratinocyte growth factor (KGF) on markers of gut adaptation after massive small bowel resection in rats. JPEN J Parenter Enteral Nutr. 2004;28:399–409. https://doi.org/10.1177/0148607104028006399.
Burrin DG, Stoll B, Guan X, Cui L, Chang X, Holst JJ. Glucagon-like peptide 2 dose-dependently activates intestinal cell survival and proliferation in neonatal piglets. Endocrinology. 2005;146:22–32. https://doi.org/10.1210/en.2004-1119.
Cottrell JJ, Stoll B, Buddington RK, Stephens JE, Cui L, Chang X, et al. Glucagon-like peptide-2 protects against TPN-induced intestinal hexose malabsorption in enterally refed piglets. Am J Physiol Gastrointest Liver Physiol. 2006;290:G293-300. https://doi.org/10.1152/ajpgi.00275.2005.
Sigalet DL, Bawazir O, Martin GR, Wallace LE, Zaharko G, Miller A, et al. Glucagon-like peptide-2 induces a specific pattern of adaptation in remnant jejunum. Dig Dis Sci. 2006;51:1557–66. https://doi.org/10.1007/s10620-006-9077-5.
Vegge A, Thymann T, Lund P, Stoll B, Bering SB, Hartmann B, et al. Glucagon-like peptide-2 induces rapid digestive adaptation following intestinal resection in preterm neonates. Am J Physiol Gastrointest Liver Physiol. 2013;305:G277–85. https://doi.org/10.1152/ajpgi.00064.2013.
Jeppesen PB, Sanguinetti EL, Buchman A, Howard L, Scolapio JS, Ziegler TR, et al. Teduglutide (ALX-0600), a dipeptidyl peptidase IV resistant glucagon-like peptide 2 analogue, improves intestinal function in short bowel syndrome patients. Gut. 2005;54:1224–31. https://doi.org/10.1136/gut.2004.061440.
O’Keefe SJ, Jeppesen PB, Gilroy R, Pertkiewicz M, Allard JP, Messing B. Safety and efficacy of teduglutide after 52 weeks of treatment in patients with short bowel intestinal failure. Clin Gastroenterol Hepatol. 2013;11(815–23):e1-3. https://doi.org/10.1016/j.cgh.2012.12.029.
Tappenden KA, Edelman J, Joelsson B. Teduglutide enhances structural adaptation of the small intestinal mucosa in patients with short bowel syndrome. J Clin Gastroenterol. 2013;47:602–7. https://doi.org/10.1097/MCG.0b013e3182828f57.
Carter BA, Cohran VC, Cole CR, Corkins MR, Dimmitt RA, Duggan C, et al. Outcomes from a 12-week, open-label, multicenter clinical trial of teduglutide in pediatric short bowel syndrome. J Pediatr. 2017;181:102–11 e5. https://doi.org/10.1016/j.jpeds.2016.10.027.
Naimi RM, Hvistendahl M, Nerup N, Ambrus R, Achiam MP, Svendsen LB, et al. Effects of glepaglutide, a novel long-acting glucagon-like peptide-2 analogue, on markers of liver status in patients with short bowel syndrome: findings from a randomised phase 2 trial. EBioMedicine. 2019;46:444–51. https://doi.org/10.1016/j.ebiom.2019.07.016.
Joly F, Seguy D, Nuzzo A, Chambrier C, Beau P, Poullenot F, et al. Six-month outcomes of teduglutide treatment in adult patients with short bowel syndrome with chronic intestinal failure: a real-world French observational cohort study. Clin Nutr. 2020;39:2856–62. https://doi.org/10.1016/j.clnu.2019.12.019.
Jeppesen PB, Gabe SM, Seidner DL, Lee HM, Olivier C. Citrulline correlations in short bowel syndrome-intestinal failure by patient stratification: analysis of 24 weeks of teduglutide treatment from a randomized controlled study. Clin Nutr. 2020;39:2479–86. https://doi.org/10.1016/j.clnu.2019.11.001.
Ramos Boluda E, Redecillas Ferreiro S, Manrique Moral O, Garcia Romero R, Irastorza Terradillos I, Nunez Ramos R, et al. Experience with teduglutide in pediatric short bowel syndrome: first real-life data. J Pediatr Gastroenterol Nutr. 2020;71:734–9. https://doi.org/10.1097/MPG.0000000000002899.
Hvistendahl MK, Naimi RM, Hansen SH, Rehfeld JF, Kissow H, Pedersen J, et al. Bile acid-farnesoid X receptor-fibroblast growth factor 19 axis in patients with short bowel syndrome: the randomized, glepaglutide phase 2 trial. JPEN J Parenter Enteral Nutr. 2021. https://doi.org/10.1002/jpen.2224.
Solar H, Doeyo M, Ortega M, De Barrio S, Olano E, Moreira E, et al. Postsurgical intestinal rehabilitation using semisynthetic glucagon-like peptide-2 analogue (sGLP-2) at a referral center: can patients achieve parenteral nutrition and sGLP-2 independency? JPEN J Parenter Enteral Nutr. 2021;45:1072–82. https://doi.org/10.1002/jpen.1983.
Author information
Authors and Affiliations
Contributions
All authors meet authorship criteria. N.G. Vallianou and M. Dalamaga developed the concept of the manuscript. Literature research was carried out by D. Kounatidis, N.G. Vallianou, and D. Tsilingiris. D. Kounatidis, N.G. Vallianou, D. Tsilingiris, G.S. Christodoulatos, and T. Stratigou wrote the draft. Artwork was prepared by G.S. Christodoulatos. E. Geladari, I. Karampela, and M. Dalamaga edited and reviewed the manuscript. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of Interest
All authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Diabetes and Obesity
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kounatidis, D., Vallianou, N.G., Tsilingiris, D. et al. Therapeutic Potential of GLP-2 Analogs in Gastrointestinal Disorders: Current Knowledge, Nutritional Aspects, and Future Perspectives. Curr Nutr Rep 11, 618–642 (2022). https://doi.org/10.1007/s13668-022-00433-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13668-022-00433-0