Abstract
Purpose of the Review
Colorectal cancer is the second most common cause of cancer death in the world. The aim of this review is to provide an update on recent epidemiological studies, the molecular mechanisms involved, and ongoing clinical trials investigating the relationship between red meat consumption and colorectal cancer.
Recent Findings
Evidence in the literature proposes an association between red meat consumption and development of colorectal cancer, and there is some insight with regard to the mechanisms involved.
Summary
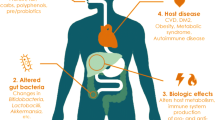
Twenty studies of the IARC report (1990–2015) showed that red meat is positively associated with colorectal cancer whereas 14 studies either supported no positive association or no statistically significant association between red meat consumption and risk for CRC. More recent epidemiological studies conducted from 2016 and onwards provided further evidence that adherence to diets low in red and/or processed meat reduces the risk of colorectal cancer. Evidence from recent studies supports that quantity, doneness, and preparation of red meat play a role in colorectal carcinogenesis. Red meat’s degradation products allow for the creation of a pro-inflammatory colonic microenvironment, and the gut microbiome plays a role in colorectal carcinogenesis. Heme, hydrogen sulfide, lipid peroxidation, nitroso compounds, and the bacterium Fusobacterium Nucleatum (as well as possibly other bacteria such as Akkermansia muciniphila, Eubacterium cylindroides, Eubacterium eligens 1 and 2, and Eubacterium rectale 1 and 2) also partake in the process of colorectal carcinogenesis. Several clinical trials are underway investigating the effects of different diets and red meat substitution products on colorectal cancer incidence as well as the underlying molecular mechanisms involved in the process.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Colorectal cancer. Gco.iarc.fr. 2020 [cited 19 July 2021]. Available from: https://gco.iarc.fr/today/data/factsheets/cancers/10_8_9-Colorectum-fact-sheet.pdf.
Dragovich T. Colon cancer clinical presentation: history, physical examination . In: medscape. 2020. https://emedicine.medscape.com/article/277496-clinical. Accessed 2 Nov 2020.
Nathional Health Services (NHS) Guidelines, UK. 2020. https://www.nhs.uk/conditions/rectal-examination/. Accessed 2 Nov 2020.
Li J, Yuan S. Fecal occult blood test in colorectal cancer screening. Journal of Digestive Diseases. 2019;20(2):62-4.
National Institute for Health and Care Excellence (NICE). 2020. Clinical Guidelines for Colorectal Cancer: The Diagnosis And Management Of Colorectal Cancer. In NICE.org.uk 2020. https://www.nice.org.uk/guidance/cg131/documents/colorectal-cancer-full-guideline2. Accessed 2 Nov 2020.
Matin K. Colon cancer treatment protocols: treatment protocols. In: Medscape. 2020. https://emedicine.medscape.com/article/2005487-overview. Accessed 2 Nov 2020.
Cancer Organisation. 2020. Colon Cancer Treatment, By Stage - How To Treat Colon Cancer. https://www.cancer.org/cancer/colon-rectal-cancer/treating/by-stage-colon.html. Accessed 2 Nov 2020.
Mármol I, Sánchez-de-Diego C, Pradilla Dieste A, Cerrada E, Rodriguez Yoldi M. Colorectal carcinoma: a general overview and future perspectives in colorectal cancer. Int J Mol Sci. 2017;18(1):197. https://doi.org/10.3390/ijms18010197.
Keum N, Giovannucci E. Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat Rev Gastroenterol Hepatol. 2019;16(12):713–32. https://doi.org/10.1038/s41575-019-0189-8. Epub 2019 Aug 27. PMID: 31455888.
Testa U, Pelosi E, Castelli G. Colorectal cancer: genetic abnormalities, tumor progression, tumor heterogeneity, clonal evolution and tumor-initiating cells. Med Sci (Basel). 2018;6(2):31. https://doi.org/10.3390/medsci6020031.
Thanikachalam K, Khan G. Colorectal cancer and nutrition. Nutrients. 2019;11(1):164. https://doi.org/10.3390/nu11010164.
Bouvard V, Loomis D, Guyton K, Grosse Y, Ghissassi F, Benbrahim-Tallaa L et al. Carcinogenicity of consumption of red and processed meat. Lancet Oncol. 2015;(16):1599–1600. https://doi.org/10.1016/S1470-2045(15)00444-1.
World Health Organisation (WHO). 2021. International Agency for Research on Cancer. IARC Monographs on teh evaluation of carcinogenic risks to humans. Red meat and processed meat;114. https://monographs.iarc.who.int/wp-content/uploads/2018/06/mono114.pdf. This report includes all relevant epidemiological evidence regarding the association of red and processed meat and colorectal cancer.
Willett WC, Stampfer MJ, Colditz GA, Rosner BA, Speizer FE. Relation of meat, fat, and fiber intake to the risk of colon cancer in a prospective study among women. N Engl J Med. 1990;323(24):1664–72. https://doi.org/10.1056/NEJM199012133232404. PMID: 2172820.
Larsson SC, Rafter J, Holmberg L, Bergkvist L, Wolk A. Red meat consumption and risk of cancers of the proximal colon, distal colon and rectum: the Swedish Mammography Cohort. Int J Cancer. 2005;113(5):829–34. https://doi.org/10.1002/ijc.20658. PMID: 15499619.
Takachi R, Tsubono Y, Baba K, Inoue M, Sasazuki S, Iwasaki M, Tsugane S; Japan Public Health Center-Based Prospective Study Group. Red meat intake may increase the risk of colon cancer in Japanese, a population with relatively low red meat consumption. Asia Pac J Clin Nutr. 2011;20(4):603–12. PMID: 22094846.
Giovannucci E, Rimm EB, Stampfer MJ, Colditz GA, Ascherio A, Willett WC. Intake of fat, meat, and fiber in relation to risk of colon cancer in men. Cancer Res. 1994;54(9):2390–7. PMID: 8162586.
Gaard M, Tretli S, Løken EB. Dietary factors and risk of colon cancer: a prospective study of 50,535 young Norwegian men and women. Eur J Cancer Prev. 1996;5(6):445–54. PMID: 9061275.
Singh P, Fraser G. Dietary risk factors for colon cancer in a low-risk population. Am J Epidemiol. 1998;148(8):761–74.
English DR, MacInnis RJ, Hodge AM, Hopper JL, Haydon AM, Giles GG. Red meat, chicken, and fish consumption and risk of colorectal cancer. Cancer Epidemiol Biomarkers Prev. 2004;13(9):1509–14. PMID: 15342453.
Norat T, Bingham S, Ferrari P, Slimani N, Jenab M, Mazuir M, Overvad K, Olsen A, Tjønneland A, Clavel F, Boutron-Ruault MC, Kesse E, Boeing H, Bergmann MM, Nieters A, Linseisen J, Trichopoulou A, Trichopoulos D, Tountas Y, Berrino F, Palli D, Panico S, Tumino R, Vineis P, Bueno-de-Mesquita HB, Peeters PH, Engeset D, Lund E, Skeie G, Ardanaz E, González C, Navarro C, Quirós JR, Sanchez MJ, Berglund G, Mattisson I, Hallmans G, Palmqvist R, Day NE, Khaw KT, Key TJ, San Joaquin M, Hémon B, Saracci R, Kaaks R, Riboli E. Meat, fish, and colorectal cancer risk: the European Prospective Investigation into cancer and nutrition. J Natl Cancer Inst. 2005;97(12):906–16. https://doi.org/10.1093/jnci/dji164. PMID: 15956652; PMCID: PMC1913932.
Sørensen M, Autrup H, Olsen A, Tjønneland A, Overvad K, Raaschou-Nielsen O. Prospective study of NAT1 and NAT2 polymorphisms, tobacco smoking and meat consumption and risk of colorectal cancer. Cancer Lett. 2008;266(2):186–93. https://doi.org/10.1016/j.canlet.2008.02.046. Epub 2008 Mar 26 PMID: 18372103.
Lee SA, Shu XO, Yang G, Li H, Gao YT, Zheng W. Animal origin foods and colorectal cancer risk: a report from the Shanghai Women’s Health Study. Nutr Cancer. 2009;61(2):194–205. https://doi.org/10.1080/01635580802419780. PMID: 19235035; PMCID: PMC2810117.
Bernstein AM, Song M, Zhang X, Pan A, Wang M, Fuchs CS, Le N, Chan AT, Willett WC, Ogino S, Giovannucci EL, Wu K. Processed and unprocessed red meat and risk of colorectal cancer: analysis by tumor location and modification by time. PLoS ONE. 2015;10(8): e0135959. https://doi.org/10.1371/journal.pone.0135959. PMID: 26305323; PMCID: PMC4549221.
Pietinen P, Malila N, Virtanen M, Hartman TJ, Tangrea JA, Albanes D, Virtamo J. Diet and risk of colorectal cancer in a cohort of Finnish men. Cancer Causes Control. 1999;10(5):387–96. https://doi.org/10.1023/a:1008962219408. PMID: 10530608.
Tiemersma EW, Kampman E, Bueno de Mesquita HB, Bunschoten A, van Schothorst EM, Kok FJ, Kromhout D. Meat consumption, cigarette smoking, and genetic susceptibility in the etiology of colorectal cancer: results from a Dutch prospective study. Cancer Causes Control. 2002;13(4):383–93. https://doi.org/10.1023/a:1015236701054. PMID: 12074508.
Chan AT, Tranah GJ, Giovannucci EL, Willett WC, Hunter DJ, Fuchs CS. Prospective study of N-acetyltransferase-2 genotypes, meat intake, smoking and risk of colorectal cancer. Int J Cancer. 2005;115(4):648–52. https://doi.org/10.1002/ijc.20890 PMID: 15700302.
Nöthlings U, Yamamoto JF, Wilkens LR, Murphy SP, Park SY, Henderson BE, Kolonel LN, Le Marchand L. Meat and heterocyclic amine intake, smoking, NAT1 and NAT2 polymorphisms, and colorectal cancer risk in the multiethnic cohort study. Cancer Epidemiol Biomarkers Prev. 2009;18(7):2098–106. https://doi.org/10.1158/1055-9965.EPI-08-1218. Epub 2009 Jun 23. PMID: 19549810; PMCID: PMC2771770.
Ananthakrishnan AN, Du M, Berndt SI, Brenner H, Caan BJ, Casey G, Chang-Claude J, Duggan D, Fuchs CS, Gallinger S, Giovannucci EL, Harrison TA, Hayes RB, Hoffmeister M, Hopper JL, Hou L, Hsu L, Jenkins MA, Kraft P, Ma J, Nan H, Newcomb PA, Ogino S, Potter JD, Seminara D, Slattery ML, Thornquist M, White E, Wu K, Peters U, Chan AT. Red meat intake, NAT2, and risk of colorectal cancer: a pooled analysis of 11 studies. Cancer Epidemiol Biomarkers Prev. 2015 Jan;24(1):198–205. doi: https://doi.org/10.1158/1055-9965.EPI-14-0897. Epub 2014 Oct 23. PMID: 25342387; PMCID: PMC4294960.
Lüchtenborg M, Weijenberg MP, de Goeij AF, Wark PA, Brink M, Roemen GM, Lentjes MH, de Bruïne AP, Goldbohm RA, van 't Veer P, van den Brandt PA. Meat and fish consumption, APC gene mutations and hMLH1 expression in colon and rectal cancer: a prospective cohort study (The Netherlands). Cancer Causes Control. 2005;16(9):1041–54. https://doi.org/10.1007/s10552-005-0239-0. PMID: 16184469.
Hansen RD, Sørensen M, Tjønneland A, Overvad K, Wallin H, Raaschou-Nielsen O, Vogel U. XPA A23G, XPC Lys939Gln, XPD Lys751Gln and XPD Asp312Asn polymorphisms, interactions with smoking, alcohol and dietary factors, and risk of colorectal cancer. Mutat Res. 2007;619(1–2):68–80. https://doi.org/10.1016/j.mrfmmm.2007.02.002. Epub 2007 Feb 12 PMID: 17363013.
Andersen V, Ostergaard M, Christensen J, Overvad K, Tjønneland A, Vogel U. Polymorphisms in the xenobiotic transporter Multidrug Resistance 1 (MDR1) and interaction with meat intake in relation to risk of colorectal cancer in a Danish prospective case-cohort study. BMC Cancer. 2009;21(9):407. https://doi.org/10.1186/1471-2407-9-407. PMID: 19930591; PMCID: PMC2797527.
Hutter CM, Chang-Claude J, Slattery ML, Pflugeisen BM, Lin Y, Duggan D, Nan H, Lemire M, Rangrej J, Figueiredo JC, Jiao S, Harrison TA, Liu Y, Chen LS, Stelling DL, Warnick GS, Hoffmeister M, Küry S, Fuchs CS, Giovannucci E, Hazra A, Kraft P, Hunter DJ, Gallinger S, Zanke BW, Brenner H, Frank B, Ma J, Ulrich CM, White E, Newcomb PA, Kooperberg C, LaCroix AZ, Prentice RL, Jackson RD, Schoen RE, Chanock SJ, Berndt SI, Hayes RB, Caan BJ, Potter JD, Hsu L, Bézieau S, Chan AT, Hudson TJ, Peters U. Characterization of gene-environment interactions for colorectal cancer susceptibility loci. Cancer Res. 2012;72(8):2036–44. https://doi.org/10.1158/0008-5472.CAN-11-4067. Epub 2012 Feb 24. PMID: 22367214; PMCID: PMC3374720.s
Kantor ED, Hutter CM, Minnier J, Berndt SI, Brenner H, Caan BJ, Campbell PT, Carlson CS, Casey G, Chan AT, Chang-Claude J, Chanock SJ, Cotterchio M, Du M, Duggan D, Fuchs CS, Giovannucci EL, Gong J, Harrison TA, Hayes RB, Henderson BE, Hoffmeister M, Hopper JL, Jenkins MA, Jiao S, Kolonel LN, Le Marchand L, Lemire M, Ma J, Newcomb PA, Ochs-Balcom HM, Pflugeisen BM, Potter JD, Rudolph A, Schoen RE, Seminara D, Slattery ML, Stelling DL, Thomas F, Thornquist M, Ulrich CM, Warnick GS, Zanke BW, Peters U, Hsu L, White E. Gene-environment interaction involving recently identified colorectal cancer susceptibility Loci. Cancer Epidemiol Biomarkers Prev. 2014;23(9):1824–33. https://doi.org/10.1158/1055-9965.EPI-14-0062. Epub 2014 Jul 3. PMID: 24994789; PMCID: PMC4209726.
Figueiredo JC, Hsu L, Hutter CM, Lin Y, Campbell PT, Baron JA, Berndt SI, Jiao S, Casey G, Fortini B, Chan AT, Cotterchio M, Lemire M, Gallinger S, Harrison TA, Le Marchand L, Newcomb PA, Slattery ML, Caan BJ, Carlson CS, Zanke BW, Rosse SA, Brenner H, Giovannucci EL, Wu K, Chang-Claude J, Chanock SJ, Curtis KR, Duggan D, Gong J, Haile RW, Hayes RB, Hoffmeister M, Hopper JL, Jenkins MA, Kolonel LN, Qu C, Rudolph A, Schoen RE, Schumacher FR, Seminara D, Stelling DL, Thibodeau SN, Thornquist M, Warnick GS, Henderson BE, Ulrich CM, Gauderman WJ, Potter JD, White E, Peters U; CCFR; GECCO. Genome-wide diet-gene interaction analyses for risk of colorectal cancer. PLoS Genet. 2014;10(4):e1004228. https://doi.org/10.1371/journal.pgen.1004228. PMID: 24743840; PMCID: PMC3990510.
Fung TT, Hu FB, Wu K, Chiuve SE, Fuchs CS, Giovannucci E. The Mediterranean and Dietary Approaches to Stop Hypertension (DASH) diets and colorectal cancer. Am J Clin Nutr. 2010;92(6):1429–35. https://doi.org/10.3945/ajcn.2010.29242. PMID: 21097651; PMCID: PMC2980967.
Gilsing AM, Schouten LJ, Goldbohm RA, Dagnelie PC, van den Brandt PA, Weijenberg MP. Vegetarianism, low meat consumption and the risk of colorectal cancer in a population based cohort study. Sci Rep. 2015;28(5):13484. https://doi.org/10.1038/srep13484. PMID: 26316135; PMCID: PMC4551995.
Bostick RM, Potter JD, Kushi LH, Sellers TA, Steinmetz KA, McKenzie DR, Gapstur SM, Folsom AR. Sugar, meat, and fat intake, and non-dietary risk factors for colon cancer incidence in Iowa women (United States). Cancer Causes Control. 1994;5(1):38–52. https://doi.org/10.1007/BF01830725. PMID: 8123778.
Kato I, Akhmedkhanov A, Koenig K, Toniolo PG, Shore RE, Riboli E. Prospective study of diet and female colorectal cancer: the New York University Women’s Health Study. Nutr Cancer. 1997;28(3):276–81. https://doi.org/10.1080/01635589709514588. PMID: 9343837.
Wei EK, Giovannucci E, Wu K, Rosner B, Fuchs CS, Willett WC, Colditz GA. Comparison of risk factors for colon and rectal cancer. Int J Cancer. 2004;108(3):433–42. https://doi.org/10.1002/ijc.11540. PMID: 14648711; PMCID: PMC2903217.
Lin J, Zhang SM, Cook NR, Lee IM, Buring JE. Dietary fat and fatty acids and risk of colorectal cancer in women. Am J Epidemiol. 2004;160(10):1011–22. https://doi.org/10.1093/aje/kwh319. PMID: 15522858.
Brink M, Weijenberg MP, de Goeij AF, Roemen GM, Lentjes MH, de Bruïne AP, Goldbohm RA, van den Brandt PA. Meat consumption and K-ras mutations in sporadic colon and rectal cancer in The Netherlands Cohort Study. Br J Cancer. 2005;92(7):1310–20. https://doi.org/10.1038/sj.bjc.6602491. PMID: 15812479; PMCID: PMC2361976.
Sato Y, Nakaya N, Kuriyama S, Nishino Y, Tsubono Y, Tsuji I. Meat consumption and risk of colorectal cancer in Japan: the Miyagi Cohort Study. Eur J Cancer Prev. 2006;15(3):211–8. https://doi.org/10.1097/01.cej.0000197455.87356.05. PMID: 16679863.
Oba S, Shimizu N, Nagata C, Shimizu H, Kametani M, Takeyama N, Ohnuma T, Matsushita S. The relationship between the consumption of meat, fat, and coffee and the risk of colon cancer: a prospective study in Japan. Cancer Lett. 2006;244(2):260–7. https://doi.org/10.1016/j.canlet.2005.12.037. Epub 2006 Mar 6 PMID: 16519996.
Spencer EA, Key TJ, Appleby PN, Dahm CC, Keogh RH, Fentiman IS, Akbaraly T, Brunner EJ, Burley V, Cade JE, Greenwood DC, Stephen AM, Mishra G, Kuh D, Luben R, Mulligan AA, Khaw KT, Rodwell SA. Meat, poultry and fish and risk of colorectal cancer: pooled analysis of data from the UK dietary cohort consortium. Cancer Causes Control. 2010;21(9):1417–25. https://doi.org/10.1007/s10552-010-9569-7. Epub 2010 May 1. Erratum in: Cancer Causes Control. 2011 Sep;22(9):1351. PMID: 20437091.
Zhang X, Giovannucci EL, Smith-Warner SA, Wu K, Fuchs CS, Pollak M, Willett WC, Ma J. A prospective study of intakes of zinc and heme iron and colorectal cancer risk in men and women. Cancer Causes Control. 2011;22(12):1627–37. https://doi.org/10.1007/s10552-011-9839-z. Epub 2011 Sep 11. PMID: 21909950; PMCID: PMC3694413.
Ollberding NJ, Wilkens LR, Henderson BE, Kolonel LN, Le Marchand L. Meat consumption, heterocyclic amines and colorectal cancer risk: the Multiethnic Cohort Study. Int J Cancer. 2012;131(7):E1125–33. https://doi.org/10.1002/ijc.27546. Epub 2012 Apr 5. PMID: 22438055; PMCID: PMC3553660.
Jones P, Cade JE, Evans CEL, Hancock N, Greenwood DC. The Mediterranean diet and risk of colorectal cancer in the UK Women’s Cohort Study. Int J Epidemiol. 2017;46(6):1786–96. https://doi.org/10.1093/ije/dyx155. PMID: 29025095.
Erben V, Carr PR, Holleczek B, Stegmaier C, Hoffmeister M, Brenner H. Dietary patterns and risk of advanced colorectal neoplasms: a large population based screening study in Germany. Prev Med. 2018;111:101–9. https://doi.org/10.1016/j.ypmed.2018.02.025 Epub 2018 Feb 23 PMID: 29477967.
•• Vieira AR, Abar L, Chan DSM, Vingeliene S, Polemiti E, Stevens C, Greenwood D, Norat T. Foods and beverages and colorectal cancer risk: a systematic review and meta-analysis of cohort studies, an update of the evidence of the WCRF-AICR Continuous Update Project. Ann Oncol. 2017;28(8):1788-1802. https://doi.org/10.1093/annonc/mdx171. PMID: 28407090. This systemic review and meta-analyses shows a positive correlation between red meat/processed meat and colorectal cancer after having included 111 cohort studies.
Schwingshackl L, Schwedhelm C, Hoffmann G, Knüppel S, Laure Preterre A, Iqbal K, Bechthold A, De Henauw S, Michels N, Devleesschauwer B, Boeing H, Schlesinger S. Food groups and risk of colorectal cancer. Int J Cancer. 2018;142(9):1748–58. https://doi.org/10.1002/ijc.31198. Epub 2017 Dec 14 PMID: 29210053.
Bradbury KE, Murphy N, Key TJ. Diet and colorectal cancer in UK Biobank: a prospective study. Int J Epidemiol. 2020;49(1):246–58. https://doi.org/10.1093/ije/dyz064. PMID: 30993317; PMCID: PMC7124508.
Saliba W, Rennert HS, Gronich N, Gruber SB, Rennert G. Red meat and processed meat intake and risk of colorectal cancer: a population-based case-control study. Eur J Cancer Prev. 2019;28(4):287–93. https://doi.org/10.1097/CEJ.0000000000000451. PMID: 30640205; PMCID: PMC6579698.
Mehta SS, Arroyave WD, Lunn RM, Park YM, Boyd WA, Sandler DP. A prospective analysis of red and processed meat consumption and risk of colorectal cancer in women. Cancer Epidemiol Biomarkers Prev. 2020;29(1):141–150. https://doi.org/10.1158/1055-9965.EPI-19-0459. Epub 2019 Oct 1. PMID: 31575555; PMCID: PMC6954313.
•• Mullie P, Guillot G, Pizot C, Autier P, Boyle P. Efforts needed for preventing breast and colorectal cancer through changes in dietary patterns. Eur J Public Health. 2021;31(2):355–60. https://doi.org/10.1093/eurpub/ckaa233. This study shows by how much Europeans and Americans will need to cut their daily red and processed meat intake to prevent one case of colorectal cancer.
Veettil SK, Wong TY, Loo YS, Playdon MC, Lai NM, Giovannucci EL, Chaiyakunapruk N. Role of diet in colorectal cancer incidence: umbrella review of meta-analyses of prospective observational studies. JAMA Netw Open. 2021;4(2). PMID: 33591366; PMCID: PMC7887658.
Liu L, Tabung FK, Zhang X, Nowak JA, Qian ZR, Hamada T, Nevo D, Bullman S, Mima K, Kosumi K, da Silva A, Song M, Cao Y, Twombly TS, Shi Y, Liu H, Gu M, Koh H, Li W, Du C, Chen Y, Li C, Li W, Mehta RS, Wu K, Wang M, Kostic AD, Giannakis M, Garrett WS, Hutthenhower C, Chan AT, Fuchs CS, Nishihara R, Ogino S, Giovannucci EL. Diets that promote colon inflammation associate with risk of colorectal carcinomas that contain Fusobacterium nucleatum. Clin Gastroenterol Hepatol. 2018;16(10):1622–1631.e3. https://doi.org/10.1016/j.cgh.2018.04.030. Epub 2018 Apr 24. PMID: 29702299; PMCID: PMC6151288.
Ijssennagger N, Belzer C, Hooiveld GJ, Dekker J, van Mil SW, Müller M, Kleerebezem M, van der Meer R. Gut microbiota facilitates dietary heme-induced epithelial hyperproliferation by opening the mucus barrier in colon. Proc Natl Acad Sci U S A. 2015;112(32):10038–43. https://doi.org/10.1073/pnas.1507645112. Epub 2015 Jul 27. PMID: 26216954; PMCID: PMC4538683.
Abu-Ghazaleh N, Chua WJ, Gopalan V. Intestinal microbiota and its association with colon cancer and red/processed meat consumption. J Gastroenterol Hepatol. 2021;36(1):75–88. https://doi.org/10.1111/jgh.15042. Epub 2020 Apr 3 PMID: 32198788.
Deplancke B, Gaskins HR. Hydrogen sulfide induces serum-independent cell cycle entry in nontransformed rat intestinal epithelial cells. FASEB J. 2003;17(10):1310–2. https://doi.org/10.1096/fj.02-0883fje. Epub 2003 May 8 PMID: 12738807.
Bastide NM, Chenni F, Audebert M, Santarelli RL, Taché S, Naud N, Baradat M, Jouanin I, Surya R, Hobbs DA, Kuhnle GG, Raymond-Letron I, Gueraud F, Corpet DE, Pierre FH. A central role for heme iron in colon carcinogenesis associated with red meat intake. Cancer Res. 2015;75(5):870–9. https://doi.org/10.1158/0008-5472.CAN-14-2554. Epub 2015 Jan 15 PMID: 25592152.
Kuhnle GG, Story GW, Reda T, Mani AR, Moore KP, Lunn JC, Bingham SA. Diet-induced endogenous formation of nitroso compounds in the GI tract. Free Radic Biol Med. 2007;43(7):1040–7. https://doi.org/10.1016/j.freeradbiomed.2007.03.011. Epub 2007 Mar 13 PMID: 17761300.
Cupid BC, Zeng Z, Singh R, Shuker DE. Detection of O6-carboxymethyl-2’-deoxyguanosine in DNA following reaction of nitric oxide with glycine and in human blood DNA using a quantitative immunoslot blot assay. Chem Res Toxicol. 2004;17(3):294–300. https://doi.org/10.1021/tx0340706. PMID: 15025499.
Srivenugopal KS, Yuan XH, Friedman HS, Ali-Osman F. Ubiquitination-dependent proteolysis of O6-methylguanine-DNA methyltransferase in human and murine tumor cells following inactivation with O6-benzylguanine or 1,3-bis(2-chloroethyl)-1-nitrosourea. Biochemistry. 1996;35(4):1328–34. https://doi.org/10.1021/bi9518205. PMID: 8573590.
Xu-Welliver M, Pegg AE. Degradation of the alkylated form of the DNA repair protein, O(6)-alkylguanine-DNA alkyltransferase. Carcinogenesis. 2002;23(5):823–30. https://doi.org/10.1093/carcin/23.5.823. PMID: 12016156.s.
Shuker DE, Margison GP. Nitrosated glycine derivatives as a potential source of O6-methylguanine in DNA. Cancer Res. 1997;57(3):366–9. PMID: 9012456.
Gottschalg E, Scott GB, Burns PA, Shuker DE. Potassium diazoacetate-induced p53 mutations in vitro in relation to formation of O6-carboxymethyl- and O6-methyl-2’-deoxyguanosine DNA adducts: relevance for gastrointestinal cancer. Carcinogenesis. 2007;28(2):356–62. https://doi.org/10.1093/carcin/bgl150. Epub 2006 Aug 22 PMID: 16926174.
Ambs S, Merriam WG, Bennett WP, Felley-Bosco E, Ogunfusika MO, Oser SM, Klein S, Shields PG, Billiar TR, Harris CC. Frequent nitric oxide synthase-2 expression in human colon adenomas: implication for tumor angiogenesis and colon cancer progression. Cancer Res. 1998;58(2):334–41. PMID: 9443414.
Li YY, Ge QX, Cao J, Zhou YJ, Du YL, Shen B, Wan YJ, Nie YQ. Association of Fusobacterium nucleatum infection with colorectal cancer in Chinese patients. World J Gastroenterol. 2016;22(11):3227–33. https://doi.org/10.3748/wjg.v22.i11.3227. PMID: 27004000; PMCID: PMC4789998.
Yachida S, Mizutani S, Shiroma H, Shiba S, Nakajima T, Sakamoto T, Watanabe H, Masuda K, Nishimoto Y, Kubo M, Hosoda F, Rokutan H, Matsumoto M, Takamaru H, Yamada M, Matsuda T, Iwasaki M, Yamaji T, Yachida T, Soga T, Kurokawa K, Toyoda A, Ogura Y, Hayashi T, Hatakeyama M, Nakagama H, Saito Y, Fukuda S, Shibata T, Yamada T. Metagenomic and metabolomic analyses reveal distinct stage-specific phenotypes of the gut microbiota in colorectal cancer. Nat Med. 2019;25(6):968–76. https://doi.org/10.1038/s41591-019-0458-7 Epub 2019 Jun 6 PMID: 31171880.
• Abed J, Emgård JE, Zamir G, Faroja M, Almogy G, Grenov A, Sol A, Naor R, Pikarsky E, Atlan KA, Mellul A, Chaushu S, Manson AL, Earl AM, Ou N, Brennan CA, Garrett WS, Bachrach G. Fap2 mediates Fusobacterium nucleatum colorectal adenocarcinoma enrichment by binding to tumor-expressed Gal-GalNAc. Cell Host Microbe. 2016;20(2):215-25. https://doi.org/10.1016/j.chom.2016.07.006. PMID: 27512904; PMCID: PMC5465824. This report shows that Fap2 mediates Fusobacterium nucleatum colorectal adenocarcinoma enrichment by binding to tumor-expressed Gal-GalNAc.
Kostic AD, Chun E, Robertson L, Glickman JN, Gallini CA, Michaud M, Clancy TE, Chung DC, Lochhead P, Hold GL, El-Omar EM, Brenner D, Fuchs CS, Meyerson M, Garrett WS. Fusobacterium nucleatum potentiates intestinal tumorigenesis and modulates the tumor-immune microenvironment. Cell Host Microbe. 2013;14(2):207–15. https://doi.org/10.1016/j.chom.2013.07.007. PMID: 23954159; PMCID: PMC3772512.
Rubinstein MR, Wang X, Liu W, Hao Y, Cai G, Han YW. Fusobacterium nucleatum promotes colorectal carcinogenesis by modulating E-cadherin/β-catenin signaling via its FadA adhesin. Cell Host Microbe. 2013;14(2):195–206. https://doi.org/10.1016/j.chom.2013.07.012. PMID: 23954158; PMCID: PMC3770529.
Gur C, Ibrahim Y, Isaacson B, Yamin R, Abed J, Gamliel M, Enk J, Bar-On Y, Stanietsky-Kaynan N, Coppenhagen-Glazer S, Shussman N, Almogy G, Cuapio A, Hofer E, Mevorach D, Tabib A, Ortenberg R, Markel G, Miklić K, Jonjic S, Brennan CA, Garrett WS, Bachrach G, Mandelboim O. Binding of the Fap2 protein of Fusobacterium nucleatum to human inhibitory receptor TIGIT protects tumors from immune cell attack. Immunity. 2015;42(2):344–355. https://doi.org/10.1016/j.immuni.2015.01.010. Epub 2015 Feb 10. PMID: 25680274; PMCID: PMC4361732.
Yang Y, Weng W, Peng J, Hong L, Yang L, Toiyama Y, Gao R, Liu M, Yin M, Pan C, Li H, Guo B, Zhu Q, Wei Q, Moyer MP, Wang P, Cai S, Goel A, Qin H, Ma Y. Fusobacterium nucleatum increases proliferation of colorectal cancer cells and tumor development in mice by activating Toll-like receptor 4 signaling to nuclear factor-κB, and up-regulating expression of microRNA-21. Gastroenterology. 2017;152(4):851–866.e24. https://doi.org/10.1053/j.gastro.2016.11.018. Epub 2016 Nov 19. PMID: 27876571; PMCID: PMC5555435.
Moore WE, Moore LH. Intestinal floras of populations that have a high risk of colon cancer. Appl Environ Microbiol. 1995;61(9):3202–7. https://doi.org/10.1128/aem.61.9.3202-3207.1995. PMID: 7574628; PMCID: PMC167598.
Wang Y, Wan X, Wu X, Zhang C, Liu J, Hou S. Eubacterium rectale contributes to colorectal cancer initiation via promoting colitis. Gut Pathog. 2021;13(1):2. https://doi.org/10.1186/s13099-020-00396-z . PMID: 33436075; PMCID: PMC7805161.
Clinical Trials. 'Meat-based versus pesco-vegetarian diet and colorectal cancer' (ID: NCT03416777). 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT03416777. Accessed 25 July 2021.
Clinical Trials. ‘Effects of replacing red meat with legumes on biomarkers of chronic diseases in healthy men (Leg4Life)’ (ID: NCT04599920). 2021. https://clinicaltrials.gov/ct2/show/NCT04599920. Accessed 25 July 2021.
Clinical Trials. ‘Role of diet on the microbiome of the digestive system’ (ID: NCT04666727). 2021. https://clinicaltrials.gov/ct2/show/NCT04666727. Accessed 25 July 2021.
Clinical Trials. ‘Virtual human delivered nutrition module for CRC prevention’ (NCT04192071). 2021. https://clinicaltrials.gov/ct2/show/NCT04192071. Accessed 25 July 2021.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors do not have any potential conflicts of interest to disclose.
Human and Animal Rights and Informed Consent
As this was a review paper, no human or animal research was conducted by the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cancer
Rights and permissions
About this article
Cite this article
Kossenas, K., Constantinou, C. Epidemiology, Molecular Mechanisms, and Clinical Trials: an Update on Research on the Association Between Red Meat Consumption and Colorectal Cancer. Curr Nutr Rep 10, 435–467 (2021). https://doi.org/10.1007/s13668-021-00377-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13668-021-00377-x