Abstract
Purpose of Review
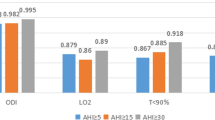
This review explores recent investigations into the clinical impact of different apnea–hypopnea index (AHI) scoring criteria, namely the minimal oxygen desaturation required to score hypopnea (3% vs 4%), in patients with obstructive sleep apnea (OSA).
Recent Findings
Analyses of prior large cohort studies on OSA with the goal of re-interpretation of polysomnography using a 3% desaturation threshold for hypopnea have demonstrated that overall prevalence of OSA increases when using the more liberal desaturation criterion. Certain groups of patients are more likely to require a 3% desaturation rule to meet the diagnostic criteria for OSA, specifically, women, younger patients, and patients with positional-dependent OSA. The adverse clinical outcomes linked to untreated OSA diagnosed with a 4% rule persist when re-interpreting data with a 3% desaturation standard.
Summary
Adoption of the American Academy of Sleep Medicine (AASM) 3% desaturation recommended scoring criteria for hypopnea expectantly increases the prevalence of OSA in the general population. In turn, many more would be eligible to receive OSA treatment. OSA diagnosed using a 3% desaturation hypopnea criteria caries adverse health and behavioral risk. Access to treatment of OSA diagnosed using the 3% desaturation criteria will reduce the health burden of untreated OSA.
Similar content being viewed by others
References
Berry RB, Abreu AR, Krishnan V, Quan SF, Strollo PJ Jr, Malhotra RK. A transition to the American Academy of Sleep Medicine–recommended hypopnea definition in adults: initiatives of the Hypopnea Scoring Rule Task Force. J Clin Sleep Med. 2022;18(5):1419–25.
Berry RB, Brooks R, Gamaldo CE, Harding SM, Marcus C, Vaughn BV. The AASM manual for the scoring of sleep and associated events. Rules, Terminology and Technical Specifications, Darien, Illinois, American Academy of Sleep Medicine. 2012;176:2012.
Punjabi NM, Newman AB, Young TB, Resnick HE, Sanders MH. Sleep-disordered breathing and cardiovascular disease: an outcome-based definition of hypopneas. Am J Respir Crit Care Med. 2008;177(10):1150–5.
Won CH, Qin L, Selim B, Yaggi HK. Varying hypopnea definitions affect obstructive sleep apnea severity classification and association with cardiovascular disease. J Clin Sleep Med. 2018;14(12):1987–94.
Korotinsky A, Assefa SZ, Diaz-Abad M, Wickwire EM, Scharf SM. Comparison of American Academy of Sleep Medicine (AASM) versus Center for Medicare and Medicaid Services (CMS) polysomnography (PSG) scoring rules on AHI and eligibility for continuous positive airway pressure (CPAP) treatment. Sleep and Breathing. 2016;20(4):1169–74.
BaHammam AS, Obeidat A, Barataman K, Bahammam SA, Olaish AH, Sharif MM. A comparison between the AASM 2012 and 2007 definitions for detecting hypopnea. Sleep and Breathing. 2014;18(4):767–73.
Duce B, Milosavljevic J, Hukins C. The 2012 AASM respiratory event criteria increase the incidence of hypopneas in an adult sleep center population. J Clin Sleep Med. 2015;11(12):1425–31.
Mansukhani MP, Kolla BP, Wang Z, Morgenthaler TI. Effect of varying definitions of hypopnea on the diagnosis and clinical outcomes of sleep-disordered breathing: a systematic review and meta-analysis. J Clin Sleep Med. 2019;15(5):687–96.
Johnson KG, Johnson DC, Thomas RJ, Rastegar V, Visintainer P. Cardiovascular and somatic comorbidities and sleep measures using three hypopnea criteria in mild obstructive sleep-disordered breathing: sex, age, and body mass index differences in a retrospective sleep clinic cohort. J Clin Sleep Med. 2020;16(10):1683–91.
Khalid F, Ayache M, Auckley D. The differential impact of respiratory event scoring criteria on CPAP eligibility in women and men. J Clin Sleep Med. 2021;17(12):2409–14.
Newman AB, Nieto FJ, Guidry U, Lind BK, Redline S, Shahar E, Pickering TG. Quan for the Sleep Heart Health Study Research Group SF. Relation of sleep-disordered breathing to cardiovascular disease risk factors: the Sleep Heart Health Study. Am Journal Epidemiol. 2001;154(1):50–9.
Budhiraja R, Javaheri S, Parthasarathy S, Berry RB, Quan SF. Incidence of hypertension in obstructive sleep apnea using hypopneas defined by 3 percent oxygen desaturation or arousal but not by only 4 percent oxygen desaturation. J Clin Sleep Med. 2020;16(10):1753–60.
Budhiraja R, Quan SF. Long-term all-cause mortality risk in obstructive sleep apnea using hypopneas defined by a ≥ 3 percent oxygen desaturation or arousal. Southwest J Pulmon Crit Care. 2021;23:23.
Jung SY, Rhee EH, Al-Dilaijan KF, Kim SW, Min JY. Impact of AASM 2012 recommended hypopnea criteria on surgical outcomes for obstructive sleep apnea. Laryngoscope. 2020;130(3):825–31.
Kapur V, Blough DK, Sandblom RE, Hert R, de Maine JB, Sullivan SD, Psaty BM. The medical cost of undiagnosed sleep apnea. Sleep. 1999;22(6):749–55.
Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MS, Morrell MJ, Nunez CM, Patel SR, Penzel T, Pépin JL, Peppard PE. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019;7(8):687–98.
He B, Al-Sherif M, Wu Y, Higgins S, Schwarz EI, Luo Y, Said AF, Refat N, Wahab NH, Steier J. Apnoea-hypopnoea-index comparing the 2007 and 2012 American Academy of Sleep Medicine criteria in chronic obstructive pulmonary disease/obstructive sleep apnoea overlap syndrome. J Thorac Dis. 2020;12(Suppl 2):S112.
Malhotra A, Ayappa I, Ayas N, Collop N, Kirsch D, Mcardle N, Mehra R, Pack AI, Punjabi N, White DP, Gottlieb DJ. Metrics of sleep apnea severity: beyond the apnea-hypopnea index. Sleep. 2021;44(7):zsab030.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors did not receive support from any organization for the work submitted. The authors have no relevant financial interest to disclose. Dr. Alexandre Abreu serves as Director on the Board of the American Academy of Sleep Medicine. The remaining authors have no known financial interest to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kalra, A., Chediak, A., Latorre, C.C. et al. Making Mountains Out of Molehills: Scoring Hypopnea Based on 3 and 4% Desaturation of Oxyhemoglobin. Curr Pulmonol Rep 12, 239–243 (2023). https://doi.org/10.1007/s13665-023-00323-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13665-023-00323-y