Abstract
Atopic dermatitis (AD) is a highly heterogeneous chronic inflammatory skin disorder that is frequently associated with a plethora of comorbidities. AD is, therefore, considered a systemic disease impacted by a considerable burden and leading to poor quality of life, especially in patients with moderate-to-severe disease. Since atopic and non-atopic comorbidities can further worsen the disease course, accurate establishment of the patient’s individual intrinsic risk profile and needs is crucial and may help in guiding the selection of the best treatment option. Better quality of care for patients with AD can be delivered through a multidisciplinary team led by a dermatologist, for comprehensive patient management. The implementation of a multidisciplinary approach for AD could enhance the delivery of optimised and safe treatments, improve the standard of care and patient outcomes in the short and long term, and prevent or delay the lifelong impact of uncontrolled AD. Understanding the unmet needs, assessing correctly the patient risk profile and enhancing the shared patient–physician decision-making process can lead to disease control and quality-of-life improvement, especially in the context of the introduction of newer treatment for AD. This narrative review is a call for more data to establish standardised patient profiles and multidisciplinary strategies in AD management. In view on the fast-evolving treatments for AD, this review aims at highlighting the importance of a multidisciplinary approach to a comprehensive assessment and holistic care in patients with moderate-to-severe AD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The complex nature and chronic course of atopic dermatitis (AD) may require a holistic approach delivered through multidisciplinary management. |
Patients with moderate-to-severe AD with an additional burden of atopic or non-atopic comorbidities should be considered for multidisciplinary care. |
Multidisciplinary approach in AD can contribute to improving short- and long-term patient outcomes. |
The overall patients’ quality of life and the standard of care can benefit from multidisciplinary care. |
Introduction
Atopic dermatitis (AD) is the most prevalent chronic inflammatory skin disease in the world [1]. Both prevalence and incidence of AD vary according to geographical regions; in a recent systematic review, the 1-year prevalence of doctor-diagnosed adult AD ranged from 1.2% in Asia to 17.1% in Europe [2].
Generally, AD is characterised clinically by eczematous lesions with intense itch and discomfort [1]. However, atypical clinical patterns have also been described. In the early acute phase, skin lesions appear mainly as poorly defined, red patches with vesicles, exudation and crusting. Scaling, fissuring and lichenification occur in the chronic phase [1]. The heterogeneity of the disease leads to the co-existence of multiple trajectories of disease presentation and history [3]. The AD severity can range from minimal flexural eczema (e.g. in the antecubital and popliteal folds), or eczema limited to the hands, to erythroderma [1, 4, 5]. Some atypical clinical phenotypes, such as nummular eczema or prurigo nodularis, have been reported, particularly in adult patients [6].
The phenotypical heterogeneity is caused by a complex and multifactorial pathogenesis. In AD, external (environmental noxious stimuli) and internal (genetic factors, immune dysregulation, impaired skin barrier and skin microbiome) alterations initiate, orchestrate and sustain chronic inflammation [7]. Clearly, the disease heterogeneity may also lead to diagnostic difficulties. In adults, the differential diagnosis includes contact dermatitis, psoriasis, pityriasis rosea, cutaneous T-cell lymphoma, seborrheic dermatitis, tinea corporis, pityriasis rubra pilaris and asteatotic eczema [1, 8].
AD is associated with multiple comorbidities, and in particular, significant overall morbidity is linked to severe AD [9, 10]. Patients with AD suffer from physical, psychological and social impairments that may result in a cumulative life-long burden for which the term ‘cumulative life course impairment’ (CLCI) was coined to describe the irreversible damage. The risk factors for CLCI in AD include disease severity, the presence of comorbidities and an early onset of the disease [11]. Moreover, because of a large number of atopic and non-atopic comorbidities and systemic immune activation, it has been proposed to consider AD a systemic disease [12,13,14]. In fact, the EuroGuiDerm guidelines recommend treating the individual as a whole and not just the skin condition [15]. For this reason, a more diffuse introduction of multidisciplinary management would improve the standard of care in AD as the formation of multidisciplinary teams was shown to be one of the best clinical practices used by leading AD centres [16].
The aim of this narrative review is to discuss the disease, its comorbidities and the evolving therapeutic options and to describe the role of multidisciplinary teams in the management of moderate to-severe AD. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Comorbidities and Disease Burden
AD is associated with a spectrum of atopic comorbidities, including asthma, hay fever and food allergy. Also, individuals with AD appear to be at a higher risk than people without of AD of developing multiple allergic/autoimmune or immune-mediated, neuropsychiatric disorders, ocular, infectious, cardiovascular conditions, osteoporosis and cancer that negatively impact their quality of life [10, 17, 18]. It is thought that the potential causal relationship between certain types of comorbidities and AD is multifactorial and bidirectional and may involve transcutaneous exposure to allergens due to impaired skin barrier [19]. The identification of specific comorbidities is important and may guide specific treatment approaches [10, 19].
Allergic rhinitis, asthma, food allergy and eosinophilic esophagitis are well-known atopic comorbidities of AD. Because of shared pathogenesis, patients with AD have three- to fourfold increased odds of having associated atopic comorbidities. The pooled prevalence of rhinitis, asthma or both in patients with AD is 40.5%, 25.7% and 14.2%, respectively. A total of 24.1% adults with AD have food allergy. Also, more severe AD is associated with increased likelihood of atopic comorbidities, including asthma [10].
Some of the most frequent non-atopic autoimmune comorbidities associated with AD include alopecia areata (AA), vitiligo, Hashimoto disease, inflammatory bowel disease and coeliac disease [17, 20]. The odds ratio for having AA in patients with AD is increased up to tenfold, and the severity of AA may be worse in individuals with AD, especially those with filaggrin gene mutations. Vitiligo, coeliac disease, chronic urticaria, inflammatory bowel disease, systemic lupus erythematosus and rheumatoid arthritis are 1.5–2 times more common in patients with AD compared with control groups [10].
AD is also strictly associated with several mental health conditions. This association has been linked to the chronic nature of AD and to the severity of disease signs, with itch being the most pervasive condition. Risk of depression, anxiety, suicidal thoughts or attention disorders is more than double in patients with AD compared with healthy people [17, 19]. The factors predominantly contributing to the occurrence of these comorbidities are persistence and severity of pruritus, sleep disturbance, social stigma and social isolation, poor quality of life, and neuroinflammation [19].
Ocular manifestations, such as atopic keratoconjunctivitis (AKC), blepharitis, conjunctivitis, tear film disturbances, keratoconus, uveitis, cataract and retinal detachment, may affect patients with AD more frequently than non-atopic individuals [21, 22]. AKC is a severe inflammatory condition of the entire ocular surface; if untreated, it may lead to blindness because of corneal neovascularisation and opacities and corneal epithelial stem cell destruction, as well as cicatricial sequelae [23]. The symptom of itch in AD often results in eye rubbing. Studies link eye rubbing to keratoconus and retinal detachment in AD. In addition, eye rubbing and the severity of lesions on the face were shown to be involved in the progression of cataract or intraocular lens subluxation following surgery to correct cataract [21].
Finally, severe AD is a risk factor for cutaneous and extracutaneous infections due to impairment of skin barrier and dysbiosis [19]. A meta-analysis showed that children and adults with AD had higher prevalence than the control populations of ear infections, strep throat and urinary tract infections but not pneumonia [24].
Although reported by some authors, there is no conclusive evidence of the association between AD and cardiovascular disease (CVD) or of higher incidence of risk factors for CVD in the population of patients with AD [10, 25]. Moreover, according to a systematic review and meta-analysis, AD is unlikely to be an independent risk factor for cardiometabolic disease [26]. However, dermatologists should be aware of this potential relationship that will need to be confirmed in the future [27].
Not surprisingly, due to the complexity of presentation and the numerous comorbidities, AD is associated with a significant physical, psychological and economic burden [28,29,30]. Patients’ lives are affected by the disease at all times throughout the day [31]. The worsening of the quality of life in AD is associated with particular pattern of cutaneous involvement (head/face/neck and hand), with the presence of atopic and non-atopic comorbidities and with the severity of pruritus [32]. Compared with those with mild and moderate AD, patients with severe disease [stratified on the basis of the Investigator’s Global Assessment (IGA); mean SCORing AD (SCORAD) 68.4 ± 14.9 and mean Eczema Area and Severity Index (EASI) 22.7 ± 13.9 in the group with severe AD] have a more substantial burden of disease across multiple aspects (more comorbidities, more pain and pruritus, worse sleep quality and higher levels of depression and anxiety; p < 0.001 for all) [28]. Similarly, compared with those with controlled disease, patients with uncontrolled disease [according to the Atopic Dermatitis Control Tool (ADCT)] were at a significantly higher risk of experiencing high level of stress and were more likely to miss work [33]. Because of productivity loss and direct medical costs, AD is associated with in annual societal costs of an estimated €30 billion across Europe (€15.2 billion due to missed workdays or reduced productivity, €10.1 billion due to direct medical costs and €4.7 billion due to personal expenditure of patients/or their families) [34].
Treatment Options
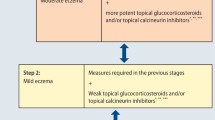
The treatment of AD is challenging [35]. Until recently, the challenges were related to the difficulties in long-term management due to the lack of effective therapies, or the potential of adverse events following long-term treatment and the lack of care pathways. Also, there is a challenge of timely assessment and introduction of the appropriate treatment, which is often delayed due to a time lag of referral to a specialist [16]. An optimal management of patients with AD with topical or systemic agents requires a multifaceted strategy to address all the different aspect of the disease [36]. Recently, both EuroGuiDerm and AAD guidelines have been updated to reflect the continuous progress and evolution in the field.
Regarding the systemic treatments in severe adult AD, the latest update of the EuroGuiDerm guidelines recommends, with a strong level of recommendation, six systemic drugs: cyclosporin, dupilumab, tralokinumab and the Janus kinase inhibitors abrocitinib, baricitinib and upadacitinib. In exceptional cases, the EuroGuiDerm suggests systemic corticosteroids, but only as a rescue therapy. This last recommendation’s strength is weak [37]. The EuroGuiDerm guidelines base their recommendations on a living systematic review and network meta-analysis that compares reported efficacy and safety of systemic treatments for AD in clinical trials [38]. The American Academy of Dermatology (AAD) guidelines, on the other hand, make a strong recommendation to use dupilumab, tralokinumab, abrocitinib, baricitinib and upadacitinib and a conditional recommendation to use azathioprine, cyclosporine, methotrexate and mycophenolate. AAD guidelines advise against the use of systemic corticosteroids [39], possibly because their use can be associated with a higher risk of certain adverse events [40].
Studies show that treat-to-target approach could simplify the management and raise the bar of the therapeutic goals in the disease [41]. Moreover, such strategy has the potential to optimise short- and long-term patient outcomes, although studies that investigate this possibility are still ongoing [42].
The enormous effort to translate the knowledge acquired at the bench into new treatments has been excellently reviewed by Facheris et al. [7].
Unmet Needs
There are numerous unmet needs in AD. A recent Delphi consensus of Italian experts described three areas of unmet needs in AD: (i) better diagnostic tools, (ii) management and prognosis, and (iii) treatment [43]. To date, there are no reliable diagnostic or prognostic biomarkers to distinguish AD from other skin conditions and to predict disease course and treatment response [44]; hence, the clinical approach remains crucial. The identification of biomarkers to trustworthily stratify disease endotypes will help in personalising the treatment in patients with AD. Such biomarkers would also be useful to predict the disease course. In fact, the disease can be self-remitting in nature; however, there are no tools for predicting who will and who will not go into a spontaneous remission [43]. Many biomarkers have been proposed and are being tested, but none of them has as yet been introduced into clinical practice (reviewed in [44, 45]).
Many adults with moderate-to-severe AD remain symptomatic, suffer recurrent flares and have an impaired quality of life despite systemic treatment as shown by a recent real-world analysis in the USA [46]. In this study, adults with AD with a disease duration of at least 5 years (n = 801), who were on systemic treatment or phototherapy for at least 6 months, were administered a survey to assess symptoms, treatment and quality of life. A total of 63.6% of patients used (only) topical corticosteroids, and > 80% experienced at least one flare, underlining how undertreated may patients be [46]. A more recent multi-country analysis of patients from the MEASURE-AD study confirmed that patients with moderate-to-severe AD experience substantial disease burden and that their AD is uncontrolled [47]. In an Italian study, only 2.8% of patients reported total satisfaction with the treatment received [48]. This suggest that better treatments or personalised treatments remain an unmet patient need. Moreover, as treatment may be needed lifelong, the appropriate long-term approaches in patients with moderate-to-severe AD must be established [49]. Furthermore, the promptness of healthcare during disease flare should be ensured as well as psychological support [50].
Other unmet needs in AD concern gaining patient’s perspectives on their treatment needs, expectations and drivers of decision-making. Also, patients have the perception that clinicians underestimate the burden of AD [31], emphasising the misalignment between patients’ expectations and clinicians’ goals that is present in several chronic skin diseases [51].
This can be improved and possibly overcome by using a patient-centric approach that combines treat-to-target principles with shared decision-making [52].
The unmet needs also concern the quality of care that patients with AD receive. In particular, Guttman-Yassky et al. identified four obstacles to the delivery of good quality care in AD: (i) misconceptions about AD (e.g. poor understanding of causes and triggers, false belief that AD is a paediatric disease, or that it is contagious, leading to patient marginalisation), (ii) late referral/access to an AD specialist, (iii) poor access/adherence to treatments by patients with AD, and (iv) the difficulties in managing the complexity of AD and its comorbidities [53].
Multidisciplinary Approach in AD
The Atopic Dermatitis Quality of Care (ADQoC) initiative described good practices for addressing the challenges mentioned naming the structured multidisciplinary team as a high-priority good practice implementation [53].
The EuroGuiDerm guidelines on AD state that most patients with AD must be treated by a dermatologist and a paediatrician for children but take into account the complexity of the disease and the presence of comorbidities and/or risk factors in some patients; other specialists may be required for a multidisciplinary approach [15, 27]. Multidisciplinary team approach brings together the skills and experience of specialists from different disciplines. Each specialist assesses a patient from their own perspective, ensuring skill mixing [54]. The team should meet regularly to discuss patients and the future directions for their care [55]. The knowledge and the experience of the team is the sum of the knowledge of each individual specialist and, therefore, can provide more insights than each specialist working alone [55] and may provide the best treatment for each patient offering a holistic approach [56]. There are two basic models for the delivery of multidisciplinary care: the creation of disease-specific, comprehensive centres or healthcare systems in which primary care providers coordinate patient’s care and seek support from specialists through referrals [57].
In the case of AD, the multidisciplinary teams must be coordinated by a dermatologist, as only specialists from this clinical speciality have the skills needed to diagnose AD, which is a skin condition, and define the patient’s treatment targets [3, 41]. The work of a multidisciplinary team has to result in an agreed treatment plan, avoid contradictory advice and lead to better control of AD and its co-morbidities. As a result, the severity of the skin condition, treatment adherence and overall quality of life may improve [15]. Multidisciplinary care can also be delivered through therapeutic patient education (TPE). TPE involves the transfer of skills from healthcare professionals to patients or their families and is managed by multidisciplinary teams composed of nurses, psychologists, dermatologists, and dieticians [58]. Experts worldwide agree that the integration of TPE into the management of patients with AD is useful [59].
The existing models of delivery of multidisciplinary care have been described elsewhere; a multidisciplinary team should involve different specialists: dermatologists, allergologists, ophthalmologists and possibly psychiatrists, nurses, psychologists, dieticians and also paediatricians [60]. The inclusion of both psychiatrists and psychologists underlines the importance of an integrated approach to the disease that considers also the mental health status [61]. The actual composition of the multidisciplinary team should be tailored to the needs of individuals patients and depend on what comorbidities they have (Table 1).
Finally, multidisciplinary care can be delivered via telemedicine. The University of Utrecht created an online ‘eczema portal’ for consulting, monitoring and self-management training for patients with AD and their caregiver. The researchers examined the feasibility of developing a Digital Eczema Centre starting from the online portal. An analysis showed that the creation of such a centre would increase the accessibility and quality of care and ensure continuation and coordination of patient care [62].
When Are Multidisciplinary Teams Needed?
Patients with comorbidities have complex needs. Despite this, they often receive fragmented care due to the traditional healthcare system models that are disease-oriented [63]. The EuroGuiDerm guidelines on AD state that patients with AD must, first of all, be treated by a dermatologist; however, other specialists may be required for a multidisciplinary approach that takes into account the complexity of the disease [15]. Whereas AD can be managed by a dermatologist alone, an overall assessment of the patient’s health conditions may require a multidisciplinary team when comorbidities are present.
Indeed, the presence of specific comorbidities in AD could guide the selection of treatment. For example, patients with AD and severe type 2 comorbidities such as asthma, allergic rhinosinusitis with nasal polyps, and/or eosinophil esophagitis may benefit from the IL-4 and IL-13 inhibitor, dupilumab, to treat all conditions. A model of tailored multidisciplinary care to guide eligibility for systemic treatments in patients with all type 2 inflammation disorders rather than specifically for patients with AD was proposed in Italy [64]. The Centre of Excellence in Type 2 Inflammation in Milan created a ‘Red Flags’ questionnaire to be administered to a patient at the first visit in order to survey and identify the type 2 inflammation disorders present in any given patient. The results of the questionnaire help in orienting the subsequent management and deciding what specialists should best care for that patient. The adopted approach optimised and standardised the patient journey and enables translational and clinical research. Similarly, patients with AD and concomitant rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis or inflammatory bowel disease are likely to benefit from a second-generation selective Janus kinase inhibitor targeting the JAK1 enzyme or both JAK1/JAK2 (i.e. baricitinib or upadacitinib) [15]. Given the potential relationship between monoclonals and ocular diseases, for patients with AD and the history of severe ocular surface disease, Janus kinase inhibitors or traditional systemic agent could be considered as a first-line systemic treatment option [65]. Janus kinase inhibitors provide an early itch control, which may be useful to stop and prevent the patients from eye rubbing [66]. Also, the Global Allergy and Asthma European Network (GA2LEN) created a subgroup dedicated to the care of patients with AD called GA2LEN ADCARE to identify the unmet needs in AD and devise an action plan for developing AD‐integrated care pathways [67].
Finally, a multidisciplinary approach may be useful to make therapeutic decisions in patients at a high risk of major adverse cardiovascular events, malignancy or thromboembolic events to guarantee the safest treatment option for each individual patient and an optimal disease management [68]. Clearly, to determine whether multidisciplinary management would be helpful in any given individual with AD, a clinical assessment of the patient profile is a pivotal step.
Patient Profiles in AD
At present, there are no universally accepted patient profiles to guide clinical decisions.
In 2022, Chovatiya and Silverberg proposed a comprehensive framework to standardise the assessment of patients with AD and called it DESCRIBE-AD, an acronym that stands for assessments of Dermatitis morphology and phenotype, Evolution of disease, Symptom severity, Comorbid health disorders, Response to therapy, Intensity of lesions, Burden of disease and Extent of lesions in AD. The framework helps characterise the heterogeneity of AD and inform therapeutic stratification [69].
Facheris et al. stratified adult patients with AD on the basis of the age of disease onset, clinical presentation features, intensity of symptoms and the presence of comorbidities. Patients with paediatric onset persisting into adulthood have, generally, more inflamed lesional skin and more compromised epidermal barrier. Patients with adult-onset AD show higher rates of cardiovascular comorbidities. The existence of the two endophenotypes may suggest that different specific treatments should be used in the two groups [70].
Clinical features at presentation were analysed in a study from the Scandinavian countries. Through a consensus process, Thyssen et al. identified six adult patient profiles that correspond to how commonly AD presents in terms of the predominant anatomical location and type of lesions, selected comorbidities or the age of onset. The identified profiles included moderate-to-severe head and neck dermatitis, moderate-to-severe AD with type I allergies, moderate-to-severe AD with hand eczema, moderate-to-severe AD with recurrent infections, moderate-to-severe lichenified AD with severe itch and moderate-to-severe late-onset AD. For each patient profile, the experts developed a set of statements concerning the diagnosis, patient education and treatment specific to that patient [71]. More work is needed to determine to validate and adopt the profile classification or to propose an alternative.
Shared Patient–Physician Decision-Making in AD
In today’s patient-centred medicine, patient’s needs and preferences constitute the central pillar of therapeutical decision-making and must be considered as recommended by EuroGuiDerm [15]. During such a process, patients describe their experience of the disease and its burden and communicate their expectations, whilst the physicians explain the management options and describe the advantages and disadvantages of the different drug classes available. Together, they set realistic and beneficial treatment goals. When the final choice is the result of a shared conviction, patient adherence to treatment increases [15]. In a quantitative study conducted with the participation of 20 adult patients with AD, the respondents stressed the need for individualised approaches in all aspects of care they receive (information provided, interaction between patient and physician, if treatment goals needed, and criteria for novel therapy choice) [50]. Thomas et al. showed that patients with AD mostly consider treatments’ benefits and risks. In this study, patients expressed the preference for drugs with a rapid onset of action, oral administration, necessity of less frequent monitoring, and a flexibility in the administration schedule. They would trade in higher efficacy for these characteristics [72]. Similar results were obtained in a qualitative interview study in the UK and USA. In both countries, for patients with AD of any age and disease severity, treatment efficacy, mode of administration and adverse effects were the most important attributes influencing the preferences [73]. Understanding patients' preferences for AD therapies can aid shared decision-making between clinicians and patients [72]. For example, a 6-week personalised integrative multidisciplinary (PIM) treatment programme incorporated the perspectives of children with AD and their parents to define clear treatment goals and strategies and was followed by a 6-month easy-access phase. Children and adolescents with difficult-to-treat AD, seemingly unresponsive to the guideline-driven therapies, improved with the PIM approach [74].
Very recently, a shared decision-making approach to inform treatment and optimise management of AD was supported by the results from a post hoc analysis of data from the treatment arms of three recent phase 3 clinical trials involving adolescents and adults with moderate-to-severe AD [AD Up (NCT03568318), Measure Up 1 (NCT03569293) and Measure Up 2 (NCT03607422)], which showed the benefits of obtaining minimal disease activity (MDA) across physician and patient outcomes [75]. The concept of MDA combines the principles of treat-to-target with those of shared patient–physician decision-making. The patient selects between one and three most important disease symptoms (choosing from the itch, skin appearance/condition, sleep disturbance, mental health, skin pain and impact on daily living), whilst the physician selects an objective measure of disease (choosing from EASI, SCORAD and/or the IGA and body surface area). Next, based on physician’s recommendations and patient’s preferences, treatment targets are selected from a list of ‘moderate’ and ‘optimal’ [i.e. ≥ 90% improvement in EASI and a numeric rating scale of ≤ 1 for peak pruritus on the Worst Pruritus Numerical Rating Scale (WP-NRS; 0, no itch; 10, worst possible itch), sleep (Sleep-NRS; 0, no sleep loss; 11, no sleep at all) and pain (Pain-NRS; 0, no pain; 10, worse possible pain)] targets. MDA is defined as the achievement of optimal targets [52]. In an analysis of 2392 patients with AD, patients reaching optimal targets through the MDA approach based on achieving EASI 90 and WP-NRS ≤ 1 versus those reaching moderate or neither target had a higher proportion reporting meaningful improvements in AD symptoms, impact on daily activities and emotional state [75]. Moreover, compared with patients with moderate-to-severe AD treated with placebo, patients treated with upadacitinib obtained higher rates of MDA at 16 weeks (maintained through week 52), including rates of patients who reached score ≤ 1 on the Dermatology Life Quality Index (DLQI; 0, no impact of AD on quality of life; 30, worst impact of AD on quality of life) or of Children’s DLQI (CDLQI; 0, no impact on child’s quality of life; 30, worst impact on child’s quality of life) [76].
Conclusions and Future Vision
AD is characterised by complex interaction of clinical, genetic, behavioural and psychological factors generating multiple disease phenotypes and patient profiles, which can be treated by a dermatologist alone or by a multidisciplinary team. Is it possible to build a shared model of tailored multidisciplinary care to holistically evaluate the patient? Or alternatively, should the involvement of other specialists be foreseen in the diagnostic and therapeutic journey of patients with AD and decided on a case-by-case basis? More data are needed to fully answer these questions.
References
Weidinger S, Beck LA, Bieber T, Kabashima K, Irvine AD. Atopic dermatitis. Nat Rev Dis Primers. 2018;4(1):1.
Bylund S, Kobyletzki LB, Svalstedt M, Svensson A. Prevalence and incidence of atopic dermatitis: a systematic review. Acta Derm Venereol. 2020;100(12):adv00160.
Carrascosa JM, de la Cueva P, de Lucas R, Fonseca E, Martin A, Vicente A, et al. Patient journey in atopic dermatitis: the real-world scenario. Dermatol Ther (Heidelb). 2021;11(5):1693–705.
Stander S. Atopic dermatitis. N Engl J Med. 2021;384(12):1136–43.
Lobefaro F, Gualdi G, Di Nuzzo S, Amerio P. Atopic dermatitis: clinical aspects and unmet needs. Biomedicines. 2022;10(11):2927.
Girolomoni G, de Bruin-Weller M, Aoki V, Kabashima K, Deleuran M, Puig L, et al. Nomenclature and clinical phenotypes of atopic dermatitis. Ther Adv Chronic Dis. 2021;12:20406223211002980.
Facheris P, Jeffery J, Del Duca E, Guttman-Yassky E. The translational revolution in atopic dermatitis: the paradigm shift from pathogenesis to treatment. Cell Mol Immunol. 2023;20(5):448–74.
Barrett M, Luu M. Differential diagnosis of atopic dermatitis. Immunol Allergy Clin North Am. 2017;37(1):11–34.
Kiiski V, Ukkola-Vuoti L, Vikkula J, Ranta M, Lassenius MI, Kopra J. Effect of disease severity on comorbid conditions in atopic dermatitis: nationwide registry-based investigation in Finnish adults. Acta Derm Venereol. 2023;103:adv00882.
Thyssen JP, Halling AS, Schmid-Grendelmeier P, Guttman-Yassky E, Silverberg JI. Comorbidities of atopic dermatitis – what does the evidence say? J Allergy Clin Immunol. 2023;151(5):1155–62.
von Stulpnagel CC, Augustin M, Dupmann L, da Silva N, Sommer R. Mapping risk factors for cumulative life course impairment in patients with chronic skin diseases—a systematic review. J Eur Acad Dermatol Venereol. 2021;35(11):2166–84.
Oliveira C, Torres T. More than skin deep: the systemic nature of atopic dermatitis. Eur J Dermatol. 2019;29(3):250–8.
Gewiss C, Augustin M. Recent insights into comorbidities in atopic dermatitis. Expert Rev Clin Immunol. 2023;19(4):393–404.
Boguniewicz M, Alexis AF, Beck LA, Block J, Eichenfield LF, Fonacier L, et al. Expert perspectives on management of moderate-to-severe atopic dermatitis: a multidisciplinary consensus addressing current and emerging therapies. J Allergy Clin Immunol Pract. 2017;5(6):1519–31.
Wollenberg A, Kinberger M, Arents B, Aszodi N, Barbarot S, Bieber T, et al. First update of the living European guideline (EuroGuiDerm) on atopic eczema. J Eur Acad Dermatol Venereol. 2023;37(11):e1283–7.
Weidinger S, Nosbaum A, Simpson E, Guttman E. Good practice intervention for clinical assessment and diagnosis of atopic dermatitis: findings from the atopic dermatitis quality of care initiative. Dermatol Ther. 2022;35(3): e15259.
Paller A, Jaworski JC, Simpson EL, Boguniewicz M, Russell JJ, Block JK, et al. Major comorbidities of atopic dermatitis: beyond allergic disorders. Am J Clin Dermatol. 2018;19(6):821–38.
Silverberg JI. Selected comorbidities of atopic dermatitis: atopy, neuropsychiatric, and musculoskeletal disorders. Clin Dermatol. 2017;35(4):360–6.
Silverberg JI. Comorbidities and the impact of atopic dermatitis. Ann Allergy Asthma Immunol. 2019;123(2):144–51.
Davis DMR, Drucker AM, Alikhan A, Bercovitch L, Cohen DE, Darr JM, et al. American Academy of Dermatology Guidelines: awareness of comorbidities associated with atopic dermatitis in adults. J Am Acad Dermatol. 2022;86(6):1335–6.
Pietruszynska M, Zawadzka-Krajewska A, Duda P, Rogowska M, Grabska-Liberek I, Kulus M. Ophthalmic manifestations of atopic dermatitis. Postepy Dermatol Alergol. 2020;37(2):174–9.
Thyssen JP, Toft PB, Halling-Overgaard AS, Gislason GH, Skov L, Egeberg A. Incidence, prevalence, and risk of selected ocular disease in adults with atopic dermatitis. J Am Acad Dermatol. 2017;77(2):280–6.
Chen JJ, Applebaum DS, Sun GS, Pflugfelder SC. Atopic keratoconjunctivitis: a review. J Am Acad Dermatol. 2014;70(3):569–75.
Serrano L, Patel KR, Silverberg JI. Association between atopic dermatitis and extracutaneous bacterial and mycobacterial infections: a systematic review and meta-analysis. J Am Acad Dermatol. 2019;80(4):904–12.
Thyssen JP, Ross Terres JA, Pierce EJ, Feely MA, Silverberg JI. Prevalence, incidence and relative risk of cardiovascular disease risk factors in adults with atopic dermatitis: a systematic review. JEADV Clin Practice. 2023;2(1):5–18.
Thyssen JP, Halling-Overgaard AS, Andersen YMF, Gislason G, Skov L, Egeberg A. The association with cardiovascular disease and type 2 diabetes in adults with atopic dermatitis: a systematic review and meta-analysis. Br J Dermatol. 2018;178(6):1272–9.
Vittrup I, Thein D, Thomsen SF, Egeberg A, Thyssen JP. Risk factors that impact treatment with oral janus kinase inhibitors among adult patients with atopic dermatitis: a nationwide registry study. Acta Derm Venereol. 2024;104:adv18638.
de Bruin-Weller M, Gadkari A, Auziere S, Simpson EL, Puig L, Barbarot S, et al. The patient-reported disease burden in adults with atopic dermatitis: a cross-sectional study in Europe and Canada. J Eur Acad Dermatol Venereol. 2020;34(5):1026–36.
Elsawi R, Dainty K, Smith Begolka W, Barta K, Butler L, Capozza K, et al. The multidimensional burden of atopic dermatitis among adults: results from a large national survey. JAMA Dermatol. 2022;158(8):887–92.
Fasseeh AN, Elezbawy B, Korra N, Tannira M, Dalle H, Aderian S, et al. Burden of atopic dermatitis in adults and adolescents: a systematic literature review. Dermatol Ther (Heidelb). 2022;12(12):2653–68.
Wollenberg A, Gooderham M, Katoh N, Aoki V, Pink AE, Binamer Y, Silverberg JI. Understanding the impact of atopic dermatitis on patients: a large international, ethnically diverse survey-based qualitative study. Br J Dermatol. 2023;188:ljac140.023.
Silverberg JI, Simpson B, Abuabara K, Guttman-Yassky E, Calimlim B, Wegzyn C, et al. Prevalence and burden of atopic dermatitis involving the head, neck, face, and hand: a cross sectional study from the TARGET-DERM AD cohort. J Am Acad Dermatol. 2023;89(3):519–28.
Staumont-Salle D, Taieb C, Merhand S, Shourick J. The atopic dermatitis control tool: a high-performance tool for optimal support. Acta Derm Venereol. 2021;101(12):adv00618.
Augustin M, Misery L, von Kobyletzki L, Armario-Hita JC, Mealing S, Redding M. Unveiling the true costs and societal impacts of moderate-to-severe atopic dermatitis in Europe. J Eur Acad Dermatol Venereol. 2022;36(Suppl 7):3–16.
Bieber T. Atopic dermatitis: an expanding therapeutic pipeline for a complex disease. Nat Rev Drug Discov. 2022;21(1):21–40.
Kakkar V, Saini K, Singh KK. Challenges of current treatment and exploring the future prospects of nanoformulations for treatment of atopic dermatitis. Pharmacol Rep. 2023;75(5):1066–95.
Wollenberg A, Kinberger M, Arents B, Aszodi N, Barbarot S, Bieber T, et al. EuroGuiDerm on atopic eczema v2.2. European Dermatology Forum; 2023.
Drucker AM, Morra DE, Prieto-Merino D, Ellis AG, Yiu ZZN, Rochwerg B, et al. Systemic immunomodulatory treatments for atopic dermatitis: update of a living systematic review and network meta-analysis. JAMA Dermatol. 2022;158(5):523–32.
Davis DMR, Drucker AM, Alikhan A, Bercovitch L, Cohen DE, Darr JM, et al. Guidelines of care for the management of atopic dermatitis in adults with phototherapy and systemic therapies. J Am Acad Dermatol. 2024;90(2):e43–56.
Daniele S, Bunick C. JAK inhibitor safety compared to traditional systemic immunosuppressive therapies. J Drugs Dermatol. 2022;21(12):1298–303.
Renert-Yuval Y, Del Duca E, Arents B, Bissonnette R, Drucker AM, Flohr C, et al. Treat-to-target in dermatology: a scoping review and International Eczema Council survey on the approach in atopic dermatitis. J Eur Acad Dermatol Venereol. 2023;38:42.
De Bruin-Weller M, Deleuran M, Biedermann T, Bissonnette R, Foley P, Girolomoni G, et al. The treat-to-target project in atopic dermatitis: one year on. Acta Derm Venereol. 2023;103:adv5382.
Patrizi A, Costanzo A, Patruno C, Busa VM, Chiricozzi A, Girolomoni G. Unmet needs in atopic dermatitis management: an expert consensus. J Dermatolog Treat. 2022;33(5):2459–65.
Yu L, Li L. Potential biomarkers of atopic dermatitis. Front Med (Lausanne). 2022;9:1028694.
Renert-Yuval Y, Thyssen JP, Bissonnette R, Bieber T, Kabashima K, Hijnen D, Guttman-Yassky E. Biomarkers in atopic dermatitis – a review on behalf of the International Eczema Council. J Allergy Clin Immunol. 2021;147(4):1174–90.
Wei W, Ghorayeb E, Andria M, Walker V, Schnitzer J, Kennedy M, et al. A real-world study evaluating adeQUacy of Existing Systemic Treatments for patients with moderate-to-severe Atopic Dermatitis (QUEST-AD): baseline treatment patterns and unmet needs assessment. Ann Allergy Asthma Immunol. 2019;123(4):381–8.
Eyerich K, Gooderham MJ, Silvestre JF, Shumack SP, Mendes-Bastos P, Aoki V, et al. Real-world clinical, psychosocial and economic burden of atopic dermatitis: results from a multicountry study. J Eur Acad Dermatol Venereol. 2023.
Gori N, Chiricozzi A, Marsili F, Ferrucci SM, Amerio P, Battarra V, et al. National information campaign revealed disease characteristic and burden in adult patients suffering from atopic dermatitis. J Clin Med. 2022;11(17).
Costanzo A, Amerio P, Asero R, Chiricozzi A, Corazza M, Cristaudo A, et al. Long-term management of moderate-to-severe adult atopic dermatitis: a consensus by the Italian Society of Dermatology and Venereology (SIDeMaST), the Association of Italian Territorial and Hospital Allergists and Immunologists (AAIITO), the Italian Association of Hospital Dermatologists (ADOI), the Italian Society of Allergological, Environmental and Occupational Dermatology (SIDAPA), and the Italian Society of Allergy, Asthma and Clinical Immunology (SIAAIC). Ital J Dermatol Venerol. 2022;157(1):1–12.
de Wijs LEM, van Egmond S, Devillers ACA, Nijsten T, Hijnen D, Lugtenberg M. Needs and preferences of patients regarding atopic dermatitis care in the era of new therapeutic options: a qualitative study. Arch Dermatol Res. 2023;315(1):75–83.
Augustin M, Costanzo A, Pink A, Seneschal J, Schuster C, Mert C, et al. Real-world treatment patterns and treatment benefits among adult patients with atopic dermatitis: results from the atopic dermatitis patient satisfaction and unmet need survey. Acta Derm Venereol. 2022;102:adv00830.
Silverberg JI, Gooderham M, Katoh N, Aoki V, Pink AE, Binamer Y, Wollenberg A. Optimizing the management of atopic dermatitis with a new minimal disease activity concept and criteria and consensus-based recommendations for systemic therapy. Br J Dermatol. 2023;188(Supplement_2).
Guttman-Yassky E, Nosbaum A, Simpson E, Weidinger S. Pioneering global best practices in atopic dermatitis: results from the atopic dermatitis quality of care initiative. Clin Exp Dermatol. 2022;47(2):303–11.
European Observatory on Health Systems and Policies. How can skill-mix innovations support the implementation of integrated care for people with chronic conditions and multimorbidities. Policy Brief, No. 46. In: Winkelmann J, Scarpetti G, Williams GA, Maier CB, editors. Copenhagen; 2022. p. 43.
Jessup RL. Interdisciplinary versus multidisciplinary care teams: do we understand the difference? Aust Health Rev. 2007;31(3):330–1.
Nolte E, McKee M. Caring for people with chronic conditions: a health system perspective. Maidenhead: McGraw-Hill Education; 2008.
Grosse SD, Schechter MS, Kulkarni R, Lloyd-Puryear MA, Strickland B, Trevathan E. Models of comprehensive multidisciplinary care for individuals in the United States with genetic disorders. Pediatrics. 2009;123(1):407–12.
Barbarot S, Stalder JF. Therapeutic patient education in atopic eczema. Br J Dermatol. 2014;170(Suppl 1):44–8.
Stalder JF, Bernier C, Ball A, De Raeve L, Gieler U, Deleuran M, et al. Therapeutic patient education in atopic dermatitis: worldwide experiences. Pediatr Dermatol. 2013;30(3):329–34.
LeBovidge JS, Elverson W, Timmons KG, Hawryluk EB, Rea C, Lee M, Schneider LC. Multidisciplinary interventions in the management of atopic dermatitis. J Allergy Clin Immunol. 2016;138(2):325–34.
Senra MS, Wollenberg A. Psychodermatological aspects of atopic dermatitis. Br J Dermatol. 2014;170(Suppl 1):38–43.
van Os-Medendorp H, van Veelen C, Hover M, Eland-de Kok P, Bruijnzeel-Koomen C, Sonnevelt GJ, et al. The Digital Eczema Centre Utrecht. J Telemed Telecare. 2010;16(1):12–4.
Palmer K, Marengoni A, Forjaz MJ, Jureviciene E, Laatikainen T, Mammarella F, et al. Multimorbidity care model: Recommendations from the consensus meeting of the Joint Action on Chronic Diseases and Promoting Healthy Ageing across the Life Cycle (JA-CHRODIS). Health Policy. 2018;122(1):4–11.
Ferrucci SM, Tavecchio S, Angileri L, Blasi F, Brambilla P, Buoli M, et al. Center of excellence in type 2 inflammation: an organizational model of multidisciplinarity management of the patients affected by type 2 inflammation diseases. Arch Clin Biomed Res. 2021;5(6):983–92.
Adam DN, Gooderham MJ, Beecker JR, Hong CH, Jack CS, Jain V, et al. Expert consensus on the systemic treatment of atopic dermatitis in special populations. J Eur Acad Dermatol Venereol. 2023;37(6):1135–48.
Gao Q, Zhao Y, Zhang J. Efficacy and safety of abrocitinib and upadacitinib versus dupilumab in adults with moderate-to-severe atopic dermatitis: a systematic review and meta-analysis. Heliyon. 2023;9(6): e16704.
Zuberbier T, Beck LA, Bedbrook A, de Bruin-Weller M, Bousquet J, Cork M, et al. Developing integrated care pathways for atopic dermatitis-challenges and unmet needs. Clin Transl Allergy. 2023;13(3): e12236.
EMA. EMA recommends measures to minimise risk of serious side effects with Janus kinase inhibitors for chronic inflammatory disorders. Eur Med Agency; 2022.
Chovatiya R, Silverberg JI. DESCRIBE-AD: a novel classification framework for atopic dermatitis. J Am Acad Dermatol. 2022;87(3):541–50.
Facheris P, Da Rosa JC, Pagan AD, Angelov M, Del Duca E, Rabinowitz G, et al. Age of onset defines two distinct profiles of atopic dermatitis in adults. Allergy. 2023;78(8):2202–14.
Thyssen JP, Berents T, Bradley M, Deleuran M, Grimstad O, Korhonen L, et al. Clinical management of atopic dermatitis in adults: mapping of expert opinion in 4 Nordic countries using a modified Delphi process. Acta Derm Venereol. 2020;100(1):adv00015.
Thomas C, Raibouaa A, Wollenberg A, Capron JP, Krucien N, Karn H, Tervonen T. Patient preferences for atopic dermatitis medications in the UK, France and Spain: a discrete choice experiment. BMJ Open. 2022;12(8): e058799.
Ervin C, Crawford R, Evans E, Feldman SR, Zeichner J, Zielinski MA, et al. Patient and caregiver preferences on treatment attributes for atopic dermatitis. J Dermatolog Treat. 2022;33(4):2225–33.
Fieten KB, Schappin R, Zijlstra WT, Rijssenbeek-Nouwens L, Meijer Y, Pasmans S. Predictors of treatment success in children with difficult to treat atopic dermatitis using a personalized integrative multidisciplinary (PIM) treatment programme. J Eur Acad Dermatol Venereol. 2019;33(2):376–83.
Silverberg JI, Gooderham MJ, Katoh N, Aoki V, Pink Andrew E, Binamer Y, et al. Achievement of minimal disease activity is associated with improvements in symptoms, quality of life and treatment satisfaction in patients with atopic dermatitis. Br J Dermatol. 2023;188(Supplement_3).
Silverberg JI, Gooderham MJ, Katoh N, Aoki V, Pink AE, Binamer Y, et al. Treatment With Upadacitinib Increases the Achievement of Minimal Disease Activity Among Patients With Moderate-to-Severe Atopic Dermatitis: Results From Phase 3 Studies (Measure Up 1 and Measure Up 2). AAD Annual Meeting. San Diego, CA: American Academy of Dermatology; 2024.
Medical Writing and Editorial Assistance
The Authors would like to thank Mauro Pignataro, former employee of Clinical Network, for project management and Alicja M. Gruszka, MD PhD, an independent medical writer, who wrote the manuscript on behalf of Clinical Network. This medical writing assistance was funded by AbbVie.
Funding
AbbVie provided funding used to assist with the preparation of the manuscript and for Rapid Service Fee
Author information
Authors and Affiliations
Contributions
Paolo Amerio, Silvia Mariel Ferrucci, Marco Galluzzo, Maddalena Napolitano, Alessandra Narcisi, Anna Levi, Sara Di Fino, Chiara Palladino, Cataldo Patruno, and Mariateresa Rossi contributed equally to the design, literature review and manuscript conception, reviewed the drafts and approved the final version of the original and revised manuscripts.
Corresponding author
Ethics declarations
Conflicts of Interest
Paolo Amerio: acted as investigator, consultant and speaker for AbbVie, Eli Lilly, Sanofi, Galderma, Pfizer, Novartis, Leo Pharma; Silvia Mariel Ferrucci: acted as a principal investigator in clinical trials for AbbVie, Galderma, Amgen, Sanofi, Eli Lilly, Almirall, Novartis, Bayer and as a speaker and advisor for AbbVie, Almirall, Leo Pharma, Pfizer, Novartis, Menarini, Sanofi, Lilly; Marco Galluzzo: acted as a speaker and/or consultant for AbbVie, Almirall, Eli-Lilly, Janssen-Cilag, LeoPharma, Novartis, Sanofi, and acted as a principal investigator in clinical trials for Almirall, Incyte Corporation, Janssen-Cilag, LeoPharma, outside the submitted work; Maddalena Napolitano: acted as speaker, consultant and/or advisory board member for AbbVie, Eli Lilly, Leo Pharma, Novartis, and Sanofi; Alessandra Narcisi: acted as investigator, consultant, speaker and/or advisory board member for AbbVie, Eli Lilly, Novartis, UCB, Almirall, Leo Pharma, Pfizer, Sanofi, Janssen; Cataldo Patruno: acted as investigator, speaker, consultant, and/or advisory board member for AbbVie, Amgen, Eli Lilly, Galderma, Leo Pharma, Novartis, Pfizer, Pierre Fabre, and Sanofi; Mariateresa Rossi: acted as investigator, speaker, consultant, and/or advisory board member for AbbVie, Sanofi, Eli Lilly, Galderma, Leo Pharma, Pfizer, L’Oréal Paris; Anna Levi, Sara Di Fino, Chiara Palladino: employees of AbbVie and may own AbbVie stocks/options.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Amerio, P., Ferrucci, S.M., Galluzzo, M. et al. A Multidisciplinary Approach Is Beneficial in Atopic Dermatitis. Dermatol Ther (Heidelb) 14, 1443–1455 (2024). https://doi.org/10.1007/s13555-024-01185-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-024-01185-1