Abstract
Introduction
Limited information exists on the epidemiology, treatment, and burden of palmoplantar pustulosis (PPP) and defining the optimal course of treatment remains challenging without approved targeted treatments in most countries. Here, we describe the clinical and demographic characteristics, treatments received, and negative health outcomes experienced among patients with PPP in the United States (US) and Germany.
Methods
Retrospective cohort study between 2016 and 2021 using data from the US Merative™ MarketScan® Research Database and IQVIA™ German Disease Analyzer. Adult patients with PPP (ICD-10-CM L40.3) were followed from the date of their first qualifying PPP diagnosis and continued until the earlier of disenrollment or end date of database, during which treatment patterns and incidence rates of negative health outcomes were assessed. Treatment patterns included adherence, non-persistence, discontinuation, re-initiation, switching, and combination therapy.
Results
The prevalence of PPP was 0.005% and 0.065% in the MarketScan database and German Disease Analyzer, respectively, with 1629 and 3866 patients meeting the inclusion criteria. Most patients were female (71.3%, 67.8%), with mean (SD) age of 54.1 (11.7) and 56.9 (14.3) years, respectively. One year post index, most patients received topical treatment (77.4%, 65.3%), but non-persistence and discontinuation were high. Oral and biologic treatments displayed higher levels of adherence, particularly apremilast and tofacitinib among oral treatments and TNF inhibitors and IL-23 inhibitors among biologics. Rates of negative health outcomes were higher among patients not receiving treatment post-index compared with those receiving treatment post-index across both databases, regardless of prior treatment history.
Conclusions
Establishing treatment guidelines remains an unmet need for patients with PPP and could improve quality of life by reducing the occurrence of negative health outcomes. The findings from this study may provide insight into the effectiveness of current treatment options for patients with PPP and can be leveraged to support the development of treatment guidelines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Currently, no cure or approved standard of care exists for patients with palmoplantar pustulosis (PPP). |
Without established treatment guidelines, patients with PPP are less likely to receive optimal treatment and may be faced with increased negative health outcomes. |
The aim of this study was to describe the epidemiological characteristics, treatment patterns, and negative health outcomes among adult patients diagnosed with PPP. |
What was learned from this study? |
Most patients received topical treatment, but non-persistence and discontinuation were high; oral and biologic treatments displayed higher levels of adherence. |
Rates of negative health outcomes were higher among patients not receiving treatment post-index compared with those receiving treatment post-index. |
The lack of treatment guidelines may be indirectly increasing the risk of negative health outcomes. |
These findings provide insight into the treatment landscape for patients with PPP and may be leveraged to develop treatment guidelines. |
Introduction
Palmoplantar pustulosis (PPP) is a chronic inflammatory and recurrent skin condition characterized by pustules on the palms and soles [1]. In Western countries, the prevalence of PPP is estimated to be between 0.01 and 0.05% [1,2,3]. Although the International Psoriasis Council proposed that PPP should be considered a discrete skin disorder from psoriasis (PsO) [4], there has been continued debate on whether PPP is a variant of PsO, as > 10% of patients affected by psoriasis present with PPP as well. [1, 4,5,6,7,8]
Currently, no cure or approved standard of care exists for PPP, and defining the optimal course of treatment for patients with PPP has been challenging [9, 10]. Available treatment options focus mainly on symptom management and primarily include topical and systemic therapies, phototherapy, and targeted biologics; however, evidence on the risks and benefits of these treatments in this population is limited [11]. As new medications emerge and with some treatments already showing promising results in efficacy and safety, particularly in Japan where the prevalence of PPP is notably higher [12,13,14], establishing treatment guidelines is vital for the effective management and care of patients with PPP.
Without treatment guidelines, patients with PPP are less likely to receive optimal treatment [11, 15], and the current treatment landscape remains unknown. We describe the epidemiological characteristics, treatment patterns, and negative health outcomes among adult patients diagnosed with PPP across two large healthcare databases in the United States (US) and Germany.
Methods
Study Design and Data Sources
This retrospective cohort study utilized administrative claims data from the US Merative™ MarketScan® Commercial Database and electronic medical records (EMR) from the IQVIA™ German Disease Analyzer (DA). The US Merative MarketScan Commercial Database is a nationally representative data sample of the US population with employer-provided health insurance. This database contains de-identified patient-level data on inpatient, outpatient medical, and outpatient prescription drug experiences among approximately 40 million covered individuals from 160 contributing employers and 40 contributing health plans [16]. The German DA is an EMR database containing 8.5 million active, de-identified patients from primary care and specialist practices in Germany. Information collected includes demographic, diagnostic, lab tests and prescription data. The distributions of patients by health insurance fund (non-private) and age group in the German DA are very similar to the distributions found overall in the German population [17, 18]. As the data are de-identified and comply with the patient confidentiality requirements of the Health Insurance Portability and Accountability Act of 1996, this study was exempt from ethics review.
Study Population and Design
Patients eligible for study inclusion were ≥ 18 years of age, had a qualifying PPP diagnosis (ICD-10-CM L40.3), and satisfied the continuous enrollment criterion. In the US MarketScan database, patients were required to have at least 1 inpatient or 2 outpatient diagnoses of PPP within 30 and 365 days apart. The German DA only reports outpatient visits but has a confirmed diagnosis flag; patients were required to have a PPP diagnosis with a confirmed status flag. The index date was the date of PPP diagnosis; for patients satisfying the 2-outpatient criterion, the date of the initial outpatient diagnosis was considered the index date. For continuous enrollment, patients in the US MarketScan database were required to have medical and drug coverage for ≥ 365 days before index date to allow for assessment of baseline demographics and clinical characteristics; patients in the German DA were required to have evidence of ≥ 1 consultation within the year before index. Patients were further categorized by the presence of concomitant plaque PsO.
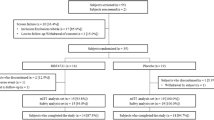
Patient follow-up began on the index date and continued until the earlier of disenrollment or end of database. The study period started on October 1, 2016 and ended at the latest date available (March 31, 2021). A summary of the overall study design is provided in Fig. 1.
Assessment of Epidemiological Characteristics and Medical History
The prevalence of PPP was calculated among all patients who had birth date and gender data available. Descriptive statistics on demographic and clinical characteristics were calculated for all patients diagnosed with PPP, with age calculated on the index date. Comorbidities and treatment history were evaluated during the baseline period. Lifestyle risk factors, such as alcohol use and smoking, are not captured well in these databases and thus were not evaluated. Patients were categorized as treatment-naïve if there was no evidence of receiving treatment during baseline; otherwise, patients were considered treatment-experienced.
Identification of Treatment Patterns
Assessed treatments were classified into 4 categories: topical agents (e.g., betamethasone, clobetasol), oral agents (e.g., apremilast, methotrexate), biologic agents (e.g., adalimumab, secukinumab, etanercept), phototherapy (e.g., excimer laser, ultraviolet light). Treatment types included in each category are described in eTable 1. Treatment patterns were evaluated 1 year after treatment initiation and included adherence, non-persistence, discontinuation, re-initiation, switching, and combination therapy. In the US MarketScan database, an allowable treatment gap of 61 days was used for all treatment lines [15, 19]. Sensitivity analyses with an 85-day allowable treatment gap were conducted in the US MarketScan database for select biologics (ustekinumab, risankizumab, tildrakizumab) with longer times between doses [20]. In the German DA, a 90-day allowable treatment gap was used to account for bulk prescriptions occurring in the database, consistent with other studies using German data sources [21, 22]. Definitions for treatment patterns are provided in Table 1.
Negative Health Outcome Assessment
Negative health outcomes for evaluation were selected based on existing literature on health outcomes related to psoriatic disease. Follow-up for outcome assessment began on index and continued until the earlier of disenrollment or end of database for all patients with PPP. For patients with PPP who received treatment post-index, we also evaluated outcomes starting on the date of treatment initiation for the first treatment received post-index through the earlier of disenrollment or end of database. In the US MarketScan database, outcomes were identified using a 1 inpatient or 2 outpatient diagnosis within 30 and 365 days apart algorithm; in the German DA, only outcomes with a confirmed status flag were considered.
Results
Prevalence of PPP and Patient Demographics
In the US MarketScan database, the prevalence of PPP was 0.005%, with 2453 patients identified. Among these, 1629 (66.4%) patients satisfied the inclusion criteria, of which 24.1% had evidence of plaque PsO comorbidity. Most patients were female (71.3%), and mean (standard deviation [SD]) age was 54.1 (11.7) years; 77.7% of all patients with PPP were aged 40 to 64 years (Table 2).
In the German DA, the prevalence of PPP was 0.065%, with 7124 patients identified. Among these, 3866 (54.3%) patients satisfied the inclusion criteria, of which 12.4% had concomitant plaque PsO. Mean (SD) age was 56.9 (14.3) years, with patients aged 40 to 64 years representing 57.5% of all patients with PPP; 67.8% (2620) were female (Table 2). Cohort attrition is provided in eFigure 1.
Clinical Characteristics and Treatment History
Among patients with PPP in the US MarketScan database, the most prevalent baseline comorbidities were hypertension (34.4%), hyperlipidemia (30.6%), pustulotic arthro-osteitis (16.7%), and diabetes mellitus (14.9%). When stratified by plaque PsO, similar results were observed; however, patients with PPP with plaque PsO were more likely to have psoriatic arthritis and/or depression, while those without plaque PsO were more likely to have pustulotic arthro-osteitis, cardiovascular disease, or SAPHO (synovitis, acne, pustulosis, hyperostosis, osteitis) syndrome. In the German DA, patients had much lower prevalence of comorbidities overall, and the most prevalent conditions were pustulotic arthro-osteitis (7.2%), hypertension (6.3%), depression (3.2%), and atopic dermatitis (3.2%). Patients with PPP with plaque PsO were more likely to have psoriatic arthritis, while those without plaque PsO were more likely to have pustulotic arthro-osteitis and hypertension (Table 2).
For treatment history, most patients with PPP in the US MarketScan database were treatment-experienced, regardless of plaque PsO comorbidity, although patients with PPP and plaque PsO were more likely to be treatment-experienced than those without plaque PsO. However, in the German DA, most patients with PPP without plaque PsO were treatment-naïve. In both databases, regardless of plaque PsO comorbidity, patients were most likely to have received topical treatment, followed by treatment with oral agents, biologics, and phototherapy (Table 2). Additional information on treatment history by drug class for both databases is provided in eTable 2.
Treatment Patterns
In the US MarketScan database, 1509 (92.6%) patients received treatment following their index date; most received topical (77.4%) and oral (62.3%) treatments, while 491 (30.1%) patients received a biologic agent and 186 (11.4%) patients received phototherapy. Mean time on treatment varied by treatment type; patients treated with biologics had the longest mean treatment length (342.7 days), while patients treated with topical agents had the shortest mean treatment length (117.4 days). Adherence was low across all treatment types, particularly with topical treatments (4.0%); however, even though non-persistence was high (83.0%) among patients treated with topical agents, 44.1% re-initiated topical treatment. Patients treated with phototherapy were more likely to discontinue (64.0%) or switch (50.5%) to another treatment category, and the proportion of patients receiving combination therapy was high across all treatment types, especially among those treated with biologics and phototherapy (Fig. 2).
Among patients who received topical treatment, most received topical steroids (97.9%), and those who did were less likely to discontinue (39.6%) or switch (54.5%) and more likely to re-initiate (44.4%) compared with those receiving other topical agents. The most common treatments among patients receiving oral therapy were oral steroids (64.6%), disease-modifying antirheumatic drugs (DMARDs; 31.1%), and apremilast (28.1%). Among those receiving oral therapy, patients treated with oral steroids or oral immunosuppressives were more likely to be non-persistent and to either discontinue or switch treatments; adherence was highest among patients treated with apremilast (45.6%). Treatment patterns across the subcategories of biologic treatment were similar. Among patients receiving biologic treatment, those treated with interleukin-23 (IL-23) inhibitors were observed to be more adherent (47.9%) and less likely to discontinue (25.0%), switch (27.1%), or be non-persistent (37.5%); however, tumor necrosis factor (TNF) inhibitors and IL-17A inhibitors were most used among patients treated with biologic agents at 56.0% and 37.7%, respectively, and TNF inhibitors had the longest mean length of treatment (293.7 days). Similarly, treatment patterns among patients treated with phototherapy were similar across phototherapy subgroups. Overall, patients who received phototherapy had low adherence (28.5%) and high discontinuation (64.0%) (eTable 3). Sensitivity analyses results with an 85-day allowable treatment gap are summarized in eTable 4.
In the German DA, 2852 (73.8%) patients received treatment following their PPP diagnosis. Similar to patients in the US MarketScan database, most received topical treatment (65.3%), followed by oral (23.5%) and biologic (3.8%) treatments. Adherence and mean treatment length were highest for patients on biologic treatment (44.6%; 422.1 days) and lowest for those receiving topical treatment (19.5%; 133.1 days). Patients receiving topical treatment were most likely to be non-persistent (63.0%); however, a quarter of the patients did re-initiate topical treatment. Patients who received oral treatment were more likely to discontinue (40.3%) and switch (24.1%) to another treatment category (Fig. 2).
Among patients who received topical treatment, most received topical steroids (96.6%), and those who did were less likely to discontinue (38.9%) or switch (14.3%) and more likely to re-initiate (24.3%) compared with those receiving other topical agents. Among patients receiving oral treatment, most received oral steroids (46.3%); however, adherence was highest among those treated with apremilast (46.7%); discontinuation and switching were highest among those treated with biotin. Among those treated with biologic agents, patients receiving TNF inhibitors and ustekinumab were observed to be on treatment for the longest time and were more likely to be adherent compared with those treated with other biologic agents. Patients treated with IL-17A inhibitors were more likely to discontinue (36.0%) or switch (29.3%) treatments (eTable 5). Treatment patterns stratified by plaque PsO comorbidity are available in eTables 3, 4 and 5.
Negative Health Outcome Rates
In the US MarketScan database, the most common negative health outcome post-index was infection (33.02 events per 100 person-years [PY]), followed by anxiety (8.88 events per 100 PY), back pain (7.93 events per 100 PY), and depression (7.19 events per 100 PY). In the German DA, infection was also the most observed outcome with a rate of 21.14 events per 100 PY, followed by depression (4.05 events per 100 PY), back pain (2.72 events per 100 PY), and hypersensitivity (2.00 events per 100 PY). Figure 3 provides the rates for all outcomes post-index. Similar results were observed when stratified by plaque PsO comorbidity (eFigures 2 and 3).
Stratifying the results by treatment status, in general, outcome rates were higher among patients without treatment post-index compared with those receiving treatment post-index across both databases, regardless of whether the patient was treatment-naïve or treatment-experienced before their PPP diagnosis. In the US MarketScan database, the largest discrepancies between those not receiving treatment post-index and those receiving treatment post-index were observed for infection, gastroesophageal reflux disease, and major adverse cardiovascular events. In the German DA, the largest discrepancies in rates between those not receiving treatment post-index and those receiving treatment post-index were observed for infection, depression, and headache. Rates for all outcomes stratified by treatment status are provided in eTable 6.
Discussion
Understanding the epidemiology and treatment landscape of patients with PPP is crucial in optimizing treatment of PPP as no standard of care currently exists. In both US and German cohorts, most patients were female and older, on average, than plaque PsO populations; these results are aligned with previous studies [23,24,25]. While the prevalence was significantly higher in the German cohort, plaque PsO comorbidity was much higher in the US cohort as observed in other studies [26, 27]; interestingly, most patients with PPP did not have concomitant plaque PsO comorbidity in either cohort. These findings may indicate differences in how PPP is defined and diagnosed in the US compared with Germany; due to the perception that PPP is related to plaque PsO, some physicians may record a plaque PsO diagnosis even with no clinical presentation. Most patients with PPP in the US were more likely to have received treatment before their PPP diagnosis, regardless of plaque PsO comorbidity, whereas in Germany, most patients with PPP only were observed to not have received prior treatment. This may be reflective of the higher proportions of baseline comorbidities observed in the US cohort or could suggest differences in prescribing practices, including off-label prescriptions, between the two countries due to the lack of established treatment guidelines [11, 28], or differences in insurance coverage and access to healthcare specialists such as dermatologists.
This study also demonstrated that among the treatment options available for patients with PPP, topical and oral treatments were the most used forms of treatment in the US and Germany. Similar results were observed in Asia by Miyazaki et al. [15]. Notably, use of oral steroids was high despite not being recommended for treating PPP, potentially indicative of the unavailability or ineffectiveness of other treatment options [29]. However, while topical and oral therapy were the most prescribed treatments, non-persistence was high for these treatments. Topical treatments, especially, were observed to have very low adherence and high non-persistence. Patients treated with biologics had the highest levels of adherence and lowest levels of discontinuation. Among oral treatments received, apremilast (PDE4 inhibitor) and tofacitinib (JAK inhibitor) were the only treatments with comparable treatment measures to biologics, with higher proportions of adherence and lower proportions of non-persistence, discontinuation, and switching compared with other oral treatment categories. Mean lengths of treatment for apremilast and tofacitinib were also similar to those for biologics; topical medications had the shortest treatment lengths. These oral therapies may be more cost-effective alternatives to biologic treatment [30, 31]. In the US, phototherapy appears to be used sparingly to treat patients with PPP, and treatment patterns across different phototherapy options were similar, with most patients discontinuing treatment within a year. In general, however, most treatments appeared to be prescribed as combination therapies to manage the symptoms and clinical burden associated with PPP, indicating a need for more effective treatment options to improve quality of life [32]. These findings may be used to support the development of treatment guidelines for patients with PPP.
For most negative health outcomes we assessed, rates were low. Infection, depression, and back pain were among those observed with the highest rates, particularly among patients not receiving treatment following their PPP diagnosis. Treatment of any type appeared to mitigate the occurrence of negative health outcomes, but PPP-only patients, particularly those in Germany, seemed less likely to receive treatment, specifically systemic treatment. Patients with PPP and concomitant plaque PsO may have been receiving treatment in accordance with the guidelines for plaque PsO, while the lack of treatment guidelines for PPP may have led to the undertreatment of patients with only PPP.
This study is limited to individuals with health coverage in the US MarketScan and German DA databases; thus, the results of this analysis may not be generalizable to those without health insurance. Coverage and representativeness of these databases are described elsewhere [16,17,18]. Additionally, as with most database studies, capture of diseases and treatments were reliant upon the recording of diagnosis and medication codes. Data on the presence of certain risk factors (particularly those related to lifestyle, genetics, environment, etc.) were not available. The presence of a prescription claim may not indicate that the medication was taken as prescribed. Similarly, the presence of a diagnosis code may not represent the positive presence of disease, as diagnoses may have been incorrectly coded or included as rule-out criteria rather than actual disease. Interpretation of these results should be considered in the context of these limitations.
Conclusions
While most patients with PPP received treatment following diagnosis, adherence to these treatments was low and rates of discontinuation were high. Treatments with the highest levels of adherence were apremilast (PDE4 inhibitor), tofacitinib (JAK inhibitor), TNF inhibitors, and IL-23 inhibitors. These treatment patterns may provide insight into the treatment landscape for patients with PPP as well as the effectiveness of current treatment options, which can be leveraged to develop treatment guidelines. The lack of treatment guidelines may be indirectly increasing the risk of negative health outcomes such as infection and depression, as patients not receiving treatment following their PPP diagnosis were observed to have higher rates of negative health outcomes. Addressing treatment gaps and establishing a standard of care for patients with PPP could potentially reduce disease burden and related healthcare resource utilization and costs.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Brunasso AMG, Puntoni M, Aberer W, Delfino C, Fancelli L, Massone C. Clinical and epidemiological comparison of patients affected by palmoplantar plaque psoriasis and palmoplantar pustulosis: a case series study. Br J Dermatol. 2013;168(6):1243–51. https://doi.org/10.1111/bjd.12223.
de Waal AC, van de Kerkhof PC. Pustulosis palmoplantaris is a disease distinct from psoriasis. J Dermatolog Treat. 2011;22(2):102–5. https://doi.org/10.3109/09546631003636817.
Asumalahti K, Ameen M, Suomela S, et al. Genetic analysis of PSORS1 distinguishes guttate psoriasis and palmoplantar pustulosis. J Invest Dermatol. 2003;120(4):627–32. https://doi.org/10.1046/j.1523-1747.2003.12094.x.
Ammoury A, El Sayed F, Dhaybi R, Bazex J. Palmoplantar pustulosis should not be considered as a variant of psoriasis. J Eur Acad Dermatol Venereol. 2008;22(3):392–3. https://doi.org/10.1111/j.1468-3083.2007.02344.x.
Mrowietz U, van de Kerkhof PC. Management of palmoplantar pustulosis: Do we need to change? Br J Dermatol. 2011;164(5):942–6. https://doi.org/10.1111/j.1365-2133.2011.10233.x.
Misiak-Galazka M, Wolska H, Rudnicka L. What do we know about palmoplantar pustulosis? J Eur Acad Dermatol Venereol. 2017;31(1):38–44. https://doi.org/10.1111/jdv.13846.
Parisi R, Symmons DPM, Griffiths CEM, Ashcroft DM. Global epidemiology of psoriasis: a systematic review of incidence and prevalence. J Invest Dermatol. 2013;133(2):377–85. https://doi.org/10.1038/jid.2012.339.
Murakami M, Terui T. Palmoplantar pustulosis: Current understanding of disease definition and pathomechanism. J Dermatol Sci. 2020;98(1):13–9. https://doi.org/10.1016/j.jdermsci.2020.03.003.
Shmidt E, Wetter DA, Ferguson SB, Pittelkow MR. Psoriasis and palmoplantar pustulosis associated with tumor necrosis factor-α inhibitors: the Mayo Clinic experience, 1998 to 2010. J Am Acad Dermatol. 2012;67(5):e179–85. https://doi.org/10.1016/j.jaad.2011.05.038.
Freitas E, Rodrigues MA, Torres T. Diagnosis, screening and treatment of patients with palmoplantar pustulosis (PPP): a review of current practices and recommendations. Clin Cosmet Investig Dermatol. 2020;13:561–78. https://doi.org/10.2147/CCID.S240607.
Obeid G, Do G, Kirby L, Hughes C, Sbidian E, Cleach LL. Interventions for chronic palmoplantar pustulosis. Cochrane Database Syst Rev. 2020;1(1):CD011628. https://doi.org/10.1002/14651858.CD011628.pub2.
Wilsmann-Theis D, Kromer C, Gerdes S, et al. A multicentre open-label study of apremilast in palmoplantar pustulosis (APLANTUS). J Eur Acad Dermatol Venereol. 2021;35(10):2045–50. https://doi.org/10.1111/JDV.17441.
Terui T, Okubo Y, Kobayashi S, et al. Efficacy and safety of apremilast for the treatment of Japanese patients with palmoplantar pustulosis: results from a phase 2, randomized, placebo-controlled study. Am J Clin Dermatol. 2023;24(5):837–47. https://doi.org/10.1007/s40257-023-00788-2.
Okubo Y, Morishima H, Zheng R, Terui T. Sustained efficacy and safety of guselkumab in patients with palmoplantar pustulosis through 1.5 years in a randomized phase 3 study. J Dermatol. 2021;48(12):1838–53. https://doi.org/10.1111/1346-8138.16132.
Miyazaki C, Sruamsiri R, Mahlich J, Jung W. Treatment patterns and healthcare resource utilization in palmoplantar pustulosis patients in Japan: a claims database study. PLoS ONE. 2020;15(5): e0232738. https://doi.org/10.1371/journal.pone.0232738.
IBM Watson Health. IBM MarketScan Research Databases for Life Sciences Researchers. https://www.ibm.com/downloads/cas/OWZWJ0QO
Rathmann W, Bongaerts B, Carius H-J, Kruppert S, Kostev K. Basic characteristics and representativeness of the German Disease Analyzer database. Int J Clin Pharmacol Ther. 2018;56(10):459–66. https://doi.org/10.5414/CP203320.
Becher H, Kostev K, Schröder-Bernhardi D. Validity and representativeness of the “Disease Analyzer” patient database for use in pharmacoepidemiological and pharmacoeconomic studies. Int J Clin Pharmacol Ther. 2009;47(10):617–26. https://doi.org/10.5414/cpp47617.
Armstrong AW, Koning JW, Rowse S, Tan H, Mamolo C, Kaur M. Under-treatment of patients with moderate to severe psoriasis in the United States: analysis of medication usage with health plan data. Dermatol Ther (Heidelb). 2017;7(1):97–109. https://doi.org/10.1007/s13555-016-0153-2.
Brownstone ND, Hong J, Mosca M, et al. Biologic Treatments of Psoriasis: An Update for the Clinician. Biol Targets Ther. 2021;15:39–51. https://doi.org/10.2147/BTT.S252578.
Ziller V, Kostev K, Kyvernitakis I, Boeckhoff J, Hadji P. Persistence and compliance of medications used in the treatment of osteoporosis–analysis using a large scale, representative, longitudinal German database. Int J Clin Pharmacol Ther. 2012;50(5):315–22. https://doi.org/10.5414/cp201632.
Eisen C, Lulic Z, Palacios-Moreno JM, et al. Persistence and adherence to dutasteride/tamsulosin fixed-dose versus free-combination alpha blocker/5ARI therapy in patients with benign prostate hyperplasia in Germany. Int J Clin Pharmacol Ther. 2020;58(1):37–49. https://doi.org/10.5414/CP203549.
Olazagasti JM, Ma JE, Wetter DA. Clinical features, etiologic factors, associated disorders, and treatment of palmoplantar pustulosis: the Mayo Clinic experience, 1996–2013. Mayo Clin Proc. 2017;92(9):1351–8. https://doi.org/10.1016/j.mayocp.2017.05.029.
Kubota K, Kamijima Y, Sato T, et al. Epidemiology of psoriasis and palmoplantar pustulosis: a nationwide study using the Japanese national claims database. BMJ Open. 2015. https://doi.org/10.1136/bmjopen-2014-006450.
Noe MH, Wan MT, Mostaghimi A, et al. Evaluation of a case series of patients with palmoplantar pustulosis in the United States. JAMA Dermatol. 2022;158(1):68–72. https://doi.org/10.1001/jamadermatol.2021.4635.
Andersen YMF, Augustin M, Petersen J, et al. Characteristics and prevalence of plaque psoriasis in patients with palmoplantar pustulosis. Br J Dermatol. 2019;181(5):976–82. https://doi.org/10.1111/bjd.17832.
Ramcharran D, Strober B, Gordon K, et al. The epidemiology of palmoplantar pustulosis: an analysis of multiple health insurance claims and electronic health records databases. Adv Ther. 2023;40(11):5090–101. https://doi.org/10.1007/s12325-023-02669-w.
Sevrain M, Richard M-A, Barnetche T, et al. Treatment for palmoplantar pustular psoriasis: systematic literature review, evidence-based recommendations and expert opinion. J Eur Acad Dermatol Venereol. 2014;28(Suppl. 5):13–6. https://doi.org/10.1111/jdv.12561.
Benjegerdes KE, Hyde K, Kivelevitch D, Mansouri B. Pustular psoriasis: pathophysiology and current treatment perspectives. Psoriasis (Auckl). 2016;6:131–44. https://doi.org/10.2147/PTT.S98954.
Marovt M, Marko PB. Apremilast monotherapy for palmoplantar pustulosis: report of three cases. SAGE Open Med Case Rep. 2021;9:2050313X211034926. https://doi.org/10.1177/2050313X211034926.
Bissonnette R, Haydey R, Rosoph LA, et al. Apremilast for the treatment of moderate-to-severe palmoplantar psoriasis: results from a double-blind, placebo-controlled, randomized study. J Eur Acd Dermatol Venereol. 2018;32(3):403–10. https://doi.org/10.1111/jdv.14647.
Langley RGB, Krueger GG, Griffiths CEM. Psoriasis: epidemiology, clinical features, and quality of life. Ann Rheum Dis. 2005;2(2):18–23. https://doi.org/10.1136/ard.2004.033217.
Medical Writing/Editorial Assistance
Writing support was provided by Amgen Inc. Sangeeta PC of CACTUS Life Sciences provided editorial support on behalf of Amgen Inc.
Funding
This study was funded by Amgen Inc.
Author information
Authors and Affiliations
Contributions
AC and MC had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: AC, MC. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: AC, MC. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: XD, FY, CL, TK, MD. Administrative, technical, or material support: A Cheng, MC. Supervision: Cheng, Cordey. Other – Editing and suggestions on content: D Neasham, BEE.
Corresponding author
Ethics declarations
Conflicts of Interest
Dr Cheng, Dr Cordey, and Dr Neasham reported being employees and stockholders of Amgen Inc. Ms Deng, Ms Yang, Ms Lue, Mr Kilcoyne, and Mr Duxbury reported being consultants for Amgen Inc. Dr Elewski reported receiving research funding from AbbVie, AnaptysBio, Boehringer Ingelheim, Bristol Myers Squibb (BMS), Celgene, Incyte, Leo, Lilly, Merck, Menlo, Novartis, Pfizer, Regeneron, UCB, Sun Pharma, Valeant (Ortho Dermatologics), and Vanda, and has received honoraria from Amgen, Arcutis, Boehringer Ingelheim, BMS, Celgene, Leo, Lilly, Novartis, UCB, and Valeant (Ortho Dermatologics).
Ethical Approval
As the data are de-identified and comply with the patient confidentiality requirements of the Health Insurance Portability and Accountability Act of 1996, this study was exempt from ethics review.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Cheng, A., Deng, X., Yang, F. et al. Treatment Patterns and Negative Health Outcomes in Palmoplantar Pustulosis Patients in Germany and the US. Dermatol Ther (Heidelb) 14, 627–641 (2024). https://doi.org/10.1007/s13555-024-01109-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-024-01109-z