Abstract
The report of death of a person from amebic meningoencephalitis, the proverbial “brain-eating ameba,” Naegleria fowleri, acquired in a state park lake in Iowa in July 2022 has once again raised the seasonal alarms about this pathogen. While exceptionally rare, its nearly universal fatality rate has panicked the public and made for good copy for the news media. This review will address free-living ameba that have been identified as causing CNS invasion in man, namely, Naegleria fowleri, Acanthamoeba species, Balamuthia mandrillaris, and Sappinia diploidea (Table 1). Of note, several Acanthamoeba spp. and Balamuthia mandrillaris may also be associated with localized extra-CNS infections in individuals who are immunocompetent and disseminated disease in immunocompromised hosts. These ameba are unique from other protozoa in that they are free-living, have no known insect vector, do not result in a human carrier state, and are typically unassociated with poor sanitation.
Similar content being viewed by others
References
Anderlini P, Przepiorka D, Luna M, Langford L, Andreeff M, Claxton D, Deisseroth AB (1994) Acanthamoeba meningoencephalitis after bone marrow transplantation. Bone Marrow Transplant 14(3):459–461
Capewell LG, Harris AM, Yoder JS, Cope JR, Eddy BA, Roy SL, Visvesvara GS, Fox LM, Beach MJ (2015) Diagnosis, clinical course, and treatment of primary amoebic meningoencephalitis in the United States, 1937–2013. J Pediatric Infect Dis Soc 4(4):e68-75
CDC (2022) Amebic meningitis. Meningitis Retrieved July 11, 2022, from https://www.cdc.gov/meningitis/amebic.html
Chotmongkol V, Pipitgool V, Khempila J (1993) Eosinophilic cerebrospinal fluid pleocytosis and primary amebic meningoencephalitis. Southeast Asian J Trop Med Public Health 24(2):399–401
Cope JR, Ali IK (2016) Primary amebic meningoencephalitis: what have we learned in the last 5 years? Curr Infect Dis Rep 18(10):31
da Rocha-Azevedo B, Tanowitz HB, Marciano-Cabral F (2009) Diagnosis of infections caused by pathogenic free-living amoebae. Interdiscip Perspect Infect Dis 2009:251406
Diaz JH (2011) The public health threat from Balamuthia mandrillaris in the southern United States. J La State Med Soc 163(4):197–204
dos Santos NG (1970) Fatal primary amebic meningoencephalitis. A retrospective study in Richmond, Virginia. Am J Clin Pathol 54(5):737–742
Duma RJ, Ferrell HW, Nelson EC, Jones MM (1969) Primary amebic meningoencephalitis. N Engl J Med 281(24):1315–1323
Duma RJ, Rosenblum WI, McGehee RF, Jones MM, Nelson EC (1971) Primary amoebic meningoencephalitis caused by Naegleria. Two new cases, response to amphotericin B, and a review. Ann Intern Med 74(6):923–931
Dunand VA, Hammer SM, Rossi R, Poulin M, Albrecht MA, Doweiko JP, DeGirolami PC, Coakley E, Piessens E, Wanke CA (1997) Parasitic sinusitis and otitis in patients infected with human immunodeficiency virus: report of five cases and review. Clin Infect Dis 25(2):267–272
Fowler M, Carter RF (1965) Acute pyogenic meningitis probably due to Acanthamoeba sp.: a preliminary report. Br Med J 2(5464):740–742
Gharpure R, Bliton J, Goodman A, Ali IKM, Yoder J, Cope JR (2021) Epidemiology and clinical characteristics of primary amebic meningoencephalitis caused by Naegleria fowleri: a global review. Clin Infect Dis 73(1):e19–e27
Gonzalez MM, Gould E, Dickinson G, Martinez AJ, Visvesvara G, Cleary TJ, Hensley GT (1986) Acquired immunodeficiency syndrome associated with Acanthamoeba infection and other opportunistic organisms. Arch Pathol Lab Med 110(8):749–751
Griesemer DA, Barton LL, Reese CM, Johnson PC, Gabrielsen JA, Talwar D, Visvesvara GS (1994) Amebic meningoencephalitis caused by Balamuthia mandrillaris. Pediatr Neurol 10(3):249–254
Grunnet ML, Cannon GH, Kushner JP (1981) Fulminant amebic meningoencephalitis due to Acanthamoeba. Neurology 31(2):174–176
John DT (1982) Primary amebic meningoencephalitis and the biology of Naegleria fowleri. Annu Rev Microbiol 36:101–123
Keane NA, Lane LM, Canniff E, Hare D, Doran S, Wallace E, Hutchinson S, Healy ML, Hennessy B, Meaney J, Chiodini P, O’Connell B, Beausang A, Vandenberghe E (2020) A surviving case of Acanthamoeba granulomatous amebic encephalitis in a hematopoietic stem cell transplant recipient. Am J Case Rep 21:e923219
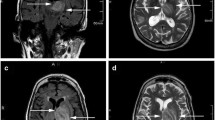
Kidney DD, Kim SH (1998) CNS infections with free-living amebas: neuroimaging findings. AJR Am J Roentgenol 171(3):809–812
Lawande RV, John I, Dobbs RH, Egler LJ (1979) A case of primary amebic meningoencephalitis in Zaria, Nigeria. Am J Clin Pathol 71(5):591–594
Linam WM, Ahmed M, Cope JR, Chu C, Visvesvara GS, da Silva AJ, Qvarnstrom Y, Green J (2015) Successful treatment of an adolescent with Naegleria fowleri primary amebic meningoencephalitis. Pediatrics 135(3):e744-748
Ma P, Visvesvara GS, Martinez AJ, Theodore FH, Daggett PM, Sawyer TK (1990) Naegleria and Acanthamoeba infections: review. Rev Infect Dis 12(3):490–513
Marciano-Cabral F, Cline ML, Bradley SG (1987) Specificity of antibodies from human sera for Naegleria species. J Clin Microbiol 25(4):692–697
Martinez AJ (1980) Is Acanthamoeba encephalitis an opportunistic infection? Neurology 30(6):567–574
Martinez AJ (1985) Free living amebas: natural history, prevention, diagnosis, pathology and treatment of disease. FL, CRC Publishing, Boca Raton
Martinez AJ (1991) Infection of the central nervous system due to Acanthamoeba. Rev Infect Dis 13(Suppl 5):S399-402
Martinez J, Duma RJ, Nelson EC, Moretta FL (1973) Experimental naegleria meningoencephalitis in mice. Penetration of the olfactory mucosal epithelium by Naegleria and pathologic changes produced: a light and electron microscope study. Lab Invest 29(2):121–133
Phillips BC, Gokden M, Petersen E (2013) Granulomatous encephalitis due to Balamuthia mandrillaris is not limited to immune-compromised patients. Clin Neurol Neurosurg 115(7):1102–1104
Schuster FL, Glaser C, Honarmand S, Maguire JH, Visvesvara GS (2004) Balamuthia amebic encephalitis risk, Hispanic Americans. Emerg Infect Dis 10(8):1510–1512
Seas C, Bravo F (2022) Free-living amebas and Prototheca. UpToDate. W. P. F. and C. A, Kauffman, Wolters Kluwer
Sell JJ, Rupp FW, Orrison WW Jr (1997) Granulomatous amebic encephalitis caused by acanthamoeba. Neuroradiology 39(6):434–436
Sheng WH, Hung CC, Huang HH, Liang SY, Cheng YJ, Ji DD, Chang SC (2009) First case of granulomatous amebic encephalitis caused by Acanthamoeba castellanii in Taiwan. Am J Trop Med Hyg 81(2):277–279
Singh P, Kochhar R, Vashishta RK, Khandelwal N, Prabhakar S, Mohindra S, Singhi P (2006) Amebic meningoencephalitis: spectrum of imaging findings. AJNR Am J Neuroradiol 27(6):1217–1221
Singh U (2005) Free-living amebas. In: Mandell GL, Bennett JE, Dolin R (eds) Principles and Practice of Infectious Diseases, vol 2. Elsevier Churchill Livingstone, Philadelphia, PA, pp 3111–3121
Sison JP, Kemper CA, Loveless M, McShane D, Visvesvara GS, Deresinski SC (1995) Disseminated acanthamoeba infection in patients with AIDS: case reports and review. Clin Infect Dis 20(5):1207–1216
Viriyavejakul P, Rochanawutanon M, Sirinavin S (1997) Naegleria meningomyeloencephalitis. Southeast Asian J Trop Med Public Health 28(1):237–240
Visvesvara GS, Peralta MJ, Brandt FH, Wilson M, Aloisio C, Franko E (1987) Production of monoclonal antibodies to Naegleria fowleri, agent of primary amebic meningoencephalitis. J Clin Microbiol 25(9):1629–1634
Wellings FM, Amuso PT, Chang SL, Lewis AL (1977) Isolation and identification of pathogenic Naegleria from Florida lakes. Appl Environ Microbiol 34(6):661–667
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Berger, J.R. Amebic infections of the central nervous system. J. Neurovirol. 28, 467–472 (2022). https://doi.org/10.1007/s13365-022-01096-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13365-022-01096-x