Abstract
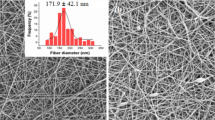
Analgesic creams find widespread application as adjuncts for localized anesthesia prior to surgical procedures. Nevertheless, the onset of analgesic action is protracted due to the skin barrier’s inherent characteristics, which necessitates prolonged intervals of patient and clinician waiting, consequently impinging upon patient compliance and clinician workflow efficiency. In this work, a biodegradable microneedles (MNs) patch was introduced to enhance the intradermal administration of lidocaine cream to achieve rapid analgesia through a minimally invasive and conveniently accessible modality. The polylactic acid (PLA) MNs were mass-produced using a simple hot-pressing method and served the purpose of creating microchannels across the skin’s surface for rapid absorption of lidocaine cream. Optical and electron microscopes were applied to meticulously scrutinize the morphology of the fabricated MNs, and the comprehensive penetration tests involving dynamometer tests, evaluation on porcine cadaver skin, artificial film, optical coherence tomography (OCT), transepidermal water loss, and analysis on rats’ skins, demonstrated the robust mechanical strength of PLA MNs for successful intradermal penetration. The behavioral pain sensitivity tests on living rats using Von Frey hair filaments revealed that the MN-assisted lidocaine treatment expeditiously accelerated the onset of action from 40 to 10 min and substantially enhanced the efficacy of localized anesthesia. Furthermore, different treatment protocols encompassing the sequence of drug application relative to MN treatment, MN dimensions, and the frequency of MN insertions exhibited noteworthy influence on the resultant local anesthesia efficacy. Together, these results demonstrated that the lidocaine cream followed by diverse PLA MN treatments would be a promising strategy for rapid clinical local anesthesia with wide-ranging applications.
Graphical abstract






Similar content being viewed by others
Data availability
The data are available from the corresponding author on reasonable request.
References
Tobe M, Suto T, Saito S. The history and progress of local anesthesia: multiple approaches to elongate the action. J Anesth. 2018;32(4):632–6.
Thorsell M, Holst P, Hyldahl HC, Weidenhielm L. Pain control after total knee arthroplasty: a prospective study comparing local infiltration anesthesia and epidural anesthesia. Orthopedics. 2010;33(2):75–80.
Obokhare J. Local and regional blocks for complex facial wound repair. Facial Plast Surg. 2021;37(04):446–53.
Ramadon D, Sutrisna LFP, Harahap Y, Putri KSS, Ulayya F, Hartrianti P, et al. Enhancing intradermal delivery of lidocaine by dissolving microneedles: comparison between hyaluronic acid and poly(vinyl pyrrolidone) backbone polymers. Pharmaceutics. 2023;15(1):289.
Xin Y, Wen X, Hamblin MR, Jiang X. Transdermal delivery of topical lidocaine in a mouse model is enhanced by treatment with cold atmospheric plasma. J Cosmet Dermatol. 2021;20(2):626–35.
Strichartz GR. The inhibition of sodium currents in myelinated nerve by quaternary derivatives of lidocaine. J Gen Physiol. 1973;62(1):37–57.
Fabbrocini G, De Vita V, Izzo R, Monfrecola G. The use of skin needling for the delivery of a eutectic mixture of local anesthetics. G Ital Dermatol Venereol. 2014;149(5):581–5.
Lander J, Hodgins M, Nazarali S, McTavish J, Ouellette J, Friesen E. Determinants of success and failure of EMLA. Pain. 1996;64(1):89–97.
Bahmani S, Khajavi R, Ehsani M, Rahimi MK, Kalaee MR. Transdermal drug delivery system of lidocaine hydrochloride based on dissolving gelatin/sodium carboxymethylcellulose microneedles. AAPS Open. 2023;9(1):7.
Zempsky WT, Robbins B, McKay K. Reduction of topical anesthetic onset time using ultrasound: a randomized controlled trial prior to venipuncture in young children. Pain Med. 2008;9(7):795–802.
Manjunatha RG, Prasad R, Sharma S, Narayan RP, Koul V. Iontophoretic delivery of lidocaine hydrochloride through ex-vivo human skin. J Dermatol Treat. 2020;31(2):191–9.
Zhang D, Ye D, Jing P, Tan X, Qiu L, Li T, et al. Design, optimization and evaluation of co-surfactant free microemulsion-based hydrogel with low surfactant for enhanced transdermal delivery of lidocaine. Int J Pharmaceut. 2020;586:119415.
Franz-Montan M, Baroni D, Brunetto G, Vieira Sobral VR, Goncalves da Silva CM, Venancio P, et al. Liposomal lidocaine gel for topical use at the oral mucosa: characterization, in vitro assays and in vivo anesthetic efficacy in humans. J Liposome Res. 2015;25(1):11–9.
Leng F, Wan J, Liu W, Tao B, Chen X. Prolongation of epidural analgesia using solid lipid nanoparticles as drug carrier for lidocaine. Reg Anesth Pain Med. 2012;37(2):159–65.
Bakonyi M, Berko S, Kovacs A, Budai-Szucs M, Kis N, Eros G, et al. Application of quality by design principles in the development and evaluation of semisolid drug carrier systems for the transdermal delivery of lidocaine. J Drug Delivery Sci Technol. 2018;44:136–45.
Babaie S, Ghanbarzadeh S, Davaran S, Kouhsoltani M, Hamishehkar H. Nanoethosomes for dermal delivery of lidocaine. Adv Pharm Bull. 2015;5(4):549–56.
Zhao X, Sun Y, Li Z. Topical anesthesia therapy using lidocaine-loaded nanostructured lipid carriers: tocopheryl polyethylene glycol 1000 succinate-modified transdermal delivery system. Drug Des, Dev Ther. 2018;12:4231–40.
Ramadon D, McCrudden MTC, Courtenay AJ, Donnelly RF. Enhancement strategies for transdermal drug delivery systems: current trends and applications. Drug Deliv Transl Re. 2021;12(4):758–91.
Chen BZ, He MC, Zhang XP, Fei WM, Cui Y, Guo XD. A novel method for fabrication of coated microneedles with homogeneous and controllable drug dosage for transdermal drug delivery. Drug Deliv Transl Re. 2022;12(11):2730–9.
Rouphael NG, Paine M, Mosley R, Henry S, McAllister DV, Kalluri H, et al. The safety, immunogenicity, and acceptability of inactivated influenza vaccine delivered by microneedle patch (TIV-MNP 2015): a randomised, partly blinded, placebo-controlled, phase 1 trial. Lancet. 2017;390(10095):649–58.
Al-Japairai KAS, Mahmood S, Almurisi SH, Venugopal JR, Hilles AR, Azmana M, et al. Current trends in polymer microneedle for transdermal drug delivery. Int J Pharm. 2020;587:119673.
Li JY, Feng YH, He YT, Hu LF, Liang L, Zhao ZQ, et al. Thermosensitive hydrogel microneedles for controlled transdermal drug delivery. Acta Biomater. 2022;153:308–19.
Al-Kasasbeh R, Brady AJ, Courtenay AJ, Larraneta E, McCrudden MTC, O’Kane D, et al. Evaluation of the clinical impact of repeat application of hydrogel-forming microneedle array patches. Drug Deliv Transl Res. 2020;10(3):690–705.
Howells O, Blayney GJ, Gualeni B, Birchall JC, Eng PF, Ashraf H, et al. Design, fabrication, and characterisation of a silicon microneedle array for transdermal therapeutic delivery using a single step wet etch process. Eur J Pharm Biopharm. 2022;171:19–28.
Hong C, Zhang G, Zhang W, Liu J, Zhang J, Chen Y, et al. Hair grows hair: Dual-effective hair regrowth through a hair enhanced dissolvable microneedle patch cooperated with the pure yellow light irradiation. Appl Mater Today. 2021;25:101188.
Sheng T, Luo B, Zhang W, Ge X, Yu J, Zhang Y, et al. Microneedle-mediated vaccination: innovation and translation. Adv Drug Delivery Rev. 2021;179:113919.
Bui VD, Son S, Xavier W, Nguyen VQ, Jung JM, Lee J, et al. Dissolving microneedles for long-term storage and transdermal delivery of extracellular vesicles. Biomaterials. 2022;287:121644.
Chen BZ, Zhao ZQ, Shahbazi M-A, Guo XD. Microneedle-based technology for cell therapy: current status and future directions. Nanoscale Horiz. 2022;7(7):715–28.
Chen X, Wang L, Yu H, Li C, Feng J, Haq F, et al. Preparation, properties and challenges of the microneedles-based insulin delivery system. J Controlled Release. 2018;288:173–88.
Li WX, Zhang XP, Chen BZ, Fei WM, Cui Y, Zhang CY, et al. An update on microneedle-based systems for diabetes. Drug Deliv Transl Re. 2022;12(10):2275–86.
Huang Y, Yu H, Wang L, Shen D, Ni Z, Ren S, et al. Research progress on cosmetic microneedle systems: preparation, property and application. Eur Polym J. 2022;163: 110942.
Larraneta E, Lutton REM, Woolfson AD, Donnelly RF. Microneedle arrays as transdermal and intradermal drug delivery systems: materials science, manufacture and commercial development. Mater Sci Eng R Rep. 2016;104:1–32.
Dabholkar N, Gorantla S, Waghule T, Rapalli VK, Kothuru A, Goel S, et al. Biodegradable microneedles fabricated with carbohydrates and proteins: revolutionary approach for transdermal drug delivery. Int J Biol Macromol. 2021;170:602–21.
Serrano G, Almudever P, Serrano JM, Cortijo J, Faus C, Reyes M, et al. Microneedling dilates the follicular infundibulum and increases transfollicular absorption of liposomal sepia melanin. Clin, Cosmet Invest Dermatol. 2015;8:313–8.
Shin Y, Kim J, Seok JH, Park H, Cha H-R, Ko SH, et al. Development of the H3N2 influenza microneedle vaccine for cross-protection against antigenic variants. Sci Rep. 2022;12(1):12189.
Lee H, Min HS, Jang M, Kang G, Gong S, Lee C, et al. Lidocaine-loaded dissolving microneedle for safe local anesthesia on oral mucosa for dental procedure. Expert Opin Drug Deliv. 2023;20(9):1251–65.
Lee B-M, Lee C, Lahiji SF, Jung U-W, Chung G, Jung H. Dissolving microneedles for rapid and painless local anesthesia. Pharmaceutics. 2020;12(4):366–79.
Courtenay AJ, McAlister E, McCrudden MTC, Vora L, Steiner L, Levin G, et al. Hydrogel-forming microneedle arrays as a therapeutic option for transdermal esketamine delivery. J Control Release. 2020;322:177–86.
Vora LK, Moffatt K, Tekko IA, Paredes AJ, Volpe-Zanutto F, Mishra D, et al. Microneedle array systems for long-acting drug delivery. Eur J Pharm Biopharm. 2021;159:44–76.
Zhao ZQ, Zhang BL, Chu HQ, Liang L, Chen BZ, Zheng H, et al. A high-dosage microneedle for programmable lidocaine delivery and enhanced local long-lasting analgesia. Biomater Adv. 2022;133:112620.
Hao YY, Yang Y, Li QY, Zhang XP, Shen CB, Zhang C, et al. Effect of polymer microneedle pre-treatment on drug distributions in the skin in vivo. J Drug Target. 2020;28(7–8):811–7.
Chen BZ, Liu JL, Li QY, Wang ZN, Zhang XP, Shen CB, et al. Safety evaluation of solid polymer microneedles in human volunteers at different application sites. ACS Appl Bio Mater. 2019;2(12):5616–25.
Yang Y, Chen BZ, Zhang XP, Zheng H, Li Z, Zhang CY, et al. Conductive microneedle patch with electricity-triggered drug release performance for atopic dermatitis treatment. ACS Appl Mater Interfaces. 2022;14(28):31645–54.
Zhang XP, Zhang BL, Chen BZ, Zhao ZQ, Fei WM, Cui Y, et al. Dissolving microneedle rollers for rapid transdermal drug delivery. Drug Deliv and Transl Re. 2022;12(2):459–71.
Lhernould MS, Deleers M, Delchambre A. Hollow polymer microneedles array resistance and insertion tests. Int J Pharm. 2015;480(1–2):152–7.
Donnelly RF, Majithiya R, Singh TRR, Morrow DIJ, Garland MJ, Demir YK, et al. Design, optimization and characterisation of polymeric microneedle arrays prepared by a novel laser-based micromoulding technique. Pharm Res. 2011;28(1):41–57.
Liu S, Jin MN, Quan YS, Kamiyama F, Katsumi H, Sakane T, et al. The development and characteristics of novel microneedle arrays fabricated from hyaluronic acid, and their application in the transdermal delivery of insulin. J Controlled Release. 2012;161(3):933–41.
Gomaa YA, Morrow DIJ, Garland MJ, Donnelly RF, El-Khordagui LK, Meidan VM. Effects of microneedle length, density, insertion time and multiple applications on human skin barrier function: assessments by transepidermal water loss. Toxicol In Vitro. 2010;24(7):1971–8.
Li M, Vora LK, Peng K, Donnelly RF. Trilayer microneedle array assisted transdermal and intradermal delivery of dexamethasone. Int J Pharm. 2022;612:121295.
Tena B, Escobar B, Jose Arguis M, Cantero C, Rios J, Gomar C. Reproducibility of electronic von Frey and von Frey monofilaments testing. Clin J Pain. 2012;28(4):318–23.
Yang H, Kang G, Jang M, Um DJ, Shin J, Kim H, et al. Development of lidocaine-loaded dissolving microneedle for rapid and efficient local anesthesia. Pharmaceutics. 2020;12(11):1067.
Li QY, Zhang JN, Chen BZ, Wang QL, Guo XD. A solid polymer microneedle patch pretreatment enhances the permeation of drug molecules into the skin. RSC Adv. 2017;7(25):15408–15.
Lutton REM, Moore J, Larrañeta E, Ligett S, Woolfson AD, Donnelly RF. Microneedle characterisation: the need for universal acceptance criteria and GMP specifications when moving towards commercialisation. Drug Deliv and Transl Re. 2015;5(4):313–31.
Kim M, Jung B, Park J-H. Hydrogel swelling as a trigger to release biodegradable polymer microneedles in skin. Biomaterials. 2012;33(2):668–78.
Wang H, Xu J, Xiang L. Microneedle-mediated transcutaneous immunization: potential in nucleic acid vaccination. Adv Healthc Mater. 2023;2300339.
Yan G, Warner KS, Zhang J, Sharma S, Gale BK. Evaluation needle length and density of microneedle arrays in the pretreatment of skin for transdermal drug delivery. Int J Pharm. 2010;391(1–2):7–12.
Bal SM, Caussin J, Pavel S, Bouwstra JA. In vivo assessment of safety of microneedle arrays in human skin. Eur J Pharm Sci. 2008;35(3):193–202.
Garland MJ, Migalska K, Mazlelaa T, Mahmood T, Raghu T, Singh R, et al. Microneedle arrays as medical devices for enhanced transdermal drug delivery. Expert Rev Med Devices. 2011;8(4):459–82.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical approval
Animal studies were approved by the institutional animal care committee of National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital (The ethical approval number: NCC2021A226). All procedures of animal studies were conducted in accordance with the animal guidelines for care and use of laboratory.
Consent to participate
Not applicable.
Consent for publication
The authors affirm that all of the listed authors actively contributed in the work which led to this paper and that they are all accountable for the work that has been published.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, Y., Zhao, Z.Q., Liang, L. et al. Toward a solid microneedle patch for rapid and enhanced local analgesic action. Drug Deliv. and Transl. Res. (2024). https://doi.org/10.1007/s13346-023-01486-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s13346-023-01486-6