Abstract
Ocular infection induced by bacteria and fungi is a major cause of visual impairment and blindness. Topical administration of antibiotics remains the first-line treatment, as effective eradication of pathogens is the core of the anti-infection strategy. Whereas, eye drops lack efficiency and have relatively low bioavailability. Intraocular injection may cause concurrent ocular damage and secondary infection. In addition, antibiotic-based management can be limited by the low sensitivity to multidrug-resistant bacteria. Nanomedicine is proposed as a prospective, effective, and noninvasive platform to mediate ocular delivery and combat pathogen or even resistant strains. Nanomedicine can not only carry antimicrobial agents to fight against pathogens but also directly active microbicidal capability, killing pathogens. More importantly, by modification, nanomedicine can achieve enhanced residence time and release time on the cornea, and easy penetration through corneal tissues into anterior and posterior segments of the eye, thus improving the therapeutic effect for ocular infection. In this review, several categories of antimicrobial nanomedicine are systematically discussed, where the efficiency and possibility of further embellishment and improvement to adapt to clinical use are also investigated. All in all, novel antimicrobial nanomedicine provides potent and prospective ways to manage severe and refractory ocular infections.
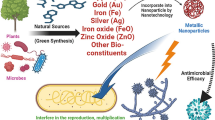
Graphical abstract















Similar content being viewed by others
References
WHO-Blindness and vision impairment. accessed at www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment.
Bourne RRA, Flaxman SR, Braithwaite T, Cicinelli MV, Das A, Jonas JB, et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(9):e888–97. https://doi.org/10.1016/s2214-109x(17)30293-0.
Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96(5):614–8. https://doi.org/10.1136/bjophthalmol-2011-300539.
Durand ML. Bacterial and fungal endophthalmitis. Clin Microbiol Rev. 2017;30(3):597–613. https://doi.org/10.1128/cmr.00113-16.
Keay L, Edwards K, Naduvilath T, Taylor HR, Snibson GR, Forde K, et al. Microbial keratitis predisposing factors and morbidity. Ophthalmology. 2006;113(1):109–16. https://doi.org/10.1016/j.ophtha.2005.08.013.
Hsu HY, Ernst B, Schmidt EJ, Parihar R, Horwood C, Edelstein SL. Laboratory results, epidemiologic features, and outcome analyses of microbial keratitis: a 15-year review from St. Louis Am J Ophthalmol. 2019;198:54–62. https://doi.org/10.1016/j.ajo.2018.09.032.
Liu HY, Chu HS, Wang IJ, Chen WL, Hu FR. Microbial keratitis in taiwan: a 20-year update. Am J Ophthalmol. 2019;205:74–81. https://doi.org/10.1016/j.ajo.2019.03.023.
Austin A, Lietman T, Rose-Nussbaumer J. Update on the management of infectious keratitis. Ophthalmology. 2017;124(11):1678–89. https://doi.org/10.1016/j.ophtha.2017.05.012.
Janagam DR, Wu L, Lowe TL. Nanoparticles for drug delivery to the anterior segment of the eye. Adv Drug Deliv Rev. 2017;122:31–64. https://doi.org/10.1016/j.addr.2017.04.001.
Gote V, Sikder S, Sicotte J, Pal D. Ocular drug delivery: present innovations and future challenges. J Pharmacol Exp Ther. 2019;370(3):602–24. https://doi.org/10.1124/jpet.119.256933.
Nguyen H, Eng S, Ngo T, Dass CR. Delivery of therapeutics for deep-seated ocular conditions—status quo. J Pharm Pharmacol. 2018;70(8):994–1001. https://doi.org/10.1111/jphp.12924.
Agrahari V, Mandal A, Agrahari V, Trinh HM, Joseph M, Ray A, et al. A comprehensive insight on ocular pharmacokinetics. Drug Deliv Transl Res. 2016;6(6):735–54. https://doi.org/10.1007/s13346-016-0339-2.
Singh M, Bharadwaj S, Lee KE, Kang SG. Therapeutic nanoemulsions in ophthalmic drug administration: concept in formulations and characterization techniques for ocular drug delivery. J Control Release. 2020;328:895–916. https://doi.org/10.1016/j.jconrel.2020.10.025.
du Toit LC, Pillay V, Choonara YE, Govender T, Carmichael T. Ocular drug delivery—a look towards nanobioadhesives. Expert Opin Drug Deliv. 2011;8(1):71–94. https://doi.org/10.1517/17425247.2011.542142.
Bennett NH, Chinnery HR, Downie LE, Hill LJ, Grover LM. Material, immunological, and practical perspectives on eye drop formulation. Adv Funct Mater. 2020;30(14):1908476. https://doi.org/10.1002/adfm.201908476.
Grassiri B, Zambito Y, Bernkop-Schnürch A. Strategies to prolong the residence time of drug delivery systems on ocular surface. Adv Colloid Interface Sci. 2021;288:102342. https://doi.org/10.1016/j.cis.2020.102342.
Relhan N, Forster RK, Flynn Jr. HW. Endophthalmitis: then and now. Am J Ophthalmol. 2018;187:xx-xxvii. https://doi.org/10.1016/j.ajo.2017.11.021.
Araújo J, Garcia ML, Mallandrich M, Souto EB, Calpena AC. Release profile and transscleral permeation of triamcinolone acetonide loaded nanostructured lipid carriers (TA-NLC): in vitro and ex vivo studies. Nanomedicine. 2012;8(6):1034–41. https://doi.org/10.1016/j.nano.2011.10.015.
Zhu S, Gong L, Li Y, Xu H, Gu Z, Zhao Y. Safety assessment of nanomaterials to eyes: an important but neglected issue. Adv Sci. 2019;6(16):1802289. https://doi.org/10.1002/advs.201802289.
Wang Y, Yang Y, Shi Y, Song H, Yu C. Antibiotic-free antibacterial strategies enabled by nanomaterials: progress and perspectives. Adv Mater. 2020;32(18):1904106. https://doi.org/10.1002/adma.201904106.
Fleiszig SMJ, Kroken AR, Nieto V, Grosser MR, Wan SJ, Metruccio MME, et al. Contact lens-related corneal infection: intrinsic resistance and its compromise. Prog Retin Eye Res. 2019:100804. https://doi.org/10.1016/j.preteyeres.2019.100804.
O’Callaghan R, Caballero A, Tang A, Bierdeman M. Pseudomonas aeruginosa keratitis: protease IV and PASP as corneal virulence mediators. Microorganisms. 2019;7(9):281. https://doi.org/10.3390/microorganisms7090281.
Lalitha P, Manoharan G, Karpagam R, Prajna NV, Srinivasan M, Mascarenhas J, et al. Trends in antibiotic resistance in bacterial keratitis isolates from South India. Br J Ophthalmol. 2017;101(2):108–13. https://doi.org/10.1136/bjophthalmol-2016-308487.
Chang VS, Dhaliwal DK, Raju L, Kowalski RP. Antibiotic resistance in the treatment of Staphylococcus aureus keratitis: a 20-year review. Cornea. 2015;34(6):698–703. https://doi.org/10.1097/ico.0000000000000431.
Cabrera-Aguas M, Khoo P, George CRR, Lahra MM, Watson SL. Antimicrobial resistance trends in bacterial keratitis over 5 years in Sydney. Australia Clin Exp Ophthalmol. 2020;48(2):183–91. https://doi.org/10.1111/ceo.13672.
Sharma P, Sharma N, Mishra P, Joseph J, Mishra DK, Garg P, et al. Differential expression of antimicrobial peptides in Streptococcus pneumoniae keratitis and STAT3-dependent expression of LL-37 by Streptococcus pneumoniae in human corneal epithelial cells. Pathogens. 2019;8(1):31. https://doi.org/10.3390/pathogens8010031.
Mahmoudi S, Masoomi A, Ahmadikia K, Tabatabaei SA, Soleimani M, Rezaie S, et al. Fungal keratitis: an overview of clinical and laboratory aspects. Mycoses. 2018;61(12):916–30. https://doi.org/10.1111/myc.12822.
Homa M, Galgoczy L, Manikandan P, Narendran V, Sinka R, Csernetics A, et al. South Indian isolates of the Fusarium solani species complex from clinical and environmental samples: identification, antifungal susceptibilities, and virulence. Front Microbiol. 2018;9:1052. https://doi.org/10.3389/fmicb.2018.01052.
Prajna NV, Krishnan T, Mascarenhas J, Rajaraman R, Prajna L, Srinivasan M, et al. The mycotic ulcer treatment trial: a randomized trial comparing natamycin vs voriconazole. JAMA ophthalmol. 2013;131(4):422–9. https://doi.org/10.1001/jamaophthalmol.2013.1497.
FlorCruz NV, Evans JR. Medical interventions for fungal keratitis. Cochrane Database Syst Rev. 2015(4):Cd004241. https://doi.org/10.1002/14651858.CD004241.pub4.
Bunya VY, Hammersmith KM, Rapuano CJ, Ayres BD, Cohen EJ. Topical and oral voriconazole in the treatment of fungal keratitis. Am J Ophthalmol. 2007;143(1):151–3. https://doi.org/10.1016/j.ajo.2006.07.033.
Klont RR, Eggink CA, Rijs AJ, Wesseling P, Verweij PE. Successful treatment of Fusarium keratitis with cornea transplantation and topical and systemic voriconazole. Clin Infect Dis. 2005;40(12):e110–2. https://doi.org/10.1086/430062.
Barnes PJ. Therapeutic strategies for allergic diseases. Nature. 1999;402(6760):31–8. https://doi.org/10.1038/35037026.
Lavigne F, Petrof BJ, Johnson JR, Lavigne P, Binothman N, Kassissia GO, et al. Effect of topical corticosteroids on allergic airway inflammation and disease severity in obstructive sleep apnoea. Clin Exp Allergy. 2013;43(10):1124–33. https://doi.org/10.1111/cea.12158.
Schmidt E, Kasperkiewicz M, Joly P. Pemphigus Lancet. 2019;394(10201):882–94. https://doi.org/10.1016/s0140-6736(19)31778-7.
Lee H-Y, Gao X, Barrasa MI, Li H, Elmes RR, Peters LL, et al. PPAR-α and glucocorticoid receptor synergize to promote erythroid progenitor self-renewal. Nature. 2015;522(7557):474–7. https://doi.org/10.1038/nature14326.
Wilhelmus KR. Indecision about corticosteroids for bacterial keratitis: an evidence-based update. Ophthalmology. 2002;109(5):835–42; quiz 43. https://doi.org/10.1016/s0161-6420(02)00963-6.
Fukuda K, Ishida W, Fukushima A, Nishida T. Corneal fibroblasts as sentinel cells and local immune modulators in infectious keratitis. Int J Mol Sci. 2017;18(9):1831. https://doi.org/10.3390/ijms18091831.
Rigas B, Huang W, Honkanen R. NSAID-induced corneal melt: clinical importance, pathogenesis, and risk mitigation. Surv Ophthalmol. 2020;65(1):1–11. https://doi.org/10.1016/j.survophthal.2019.07.001.
Ralph RA. Tetracyclines and the treatment of corneal stromal ulceration: a review. Cornea. 2000;19(3).
Grzybowski A, Turczynowska M, Kuhn F. The treatment of postoperative endophthalmitis: should we still follow the endophthalmitis vitrectomy study more than two decades after its publication? Acta Ophthalmol. 2018;96(5):e651–4. https://doi.org/10.1111/aos.13623.
Gause S, Hsu KH, Shafor C, Dixon P, Powell KC, Chauhan A. Mechanistic modeling of ophthalmic drug delivery to the anterior chamber by eye drops and contact lenses. Adv Colloid Interface Sci. 2016;233:139–54. https://doi.org/10.1016/j.cis.2015.08.002.
Han H, Yin Q, Tang X, Yu X, Gao Q, Tang Y, et al. Development of mucoadhesive cationic polypeptide micelles for sustained cabozantinib release and inhibition of corneal neovascularization. J Mater Chem B. 2020;8(23):5143–54. https://doi.org/10.1039/d0tb00874e.
Garg P, Venuganti VVK, Roy A, Roy G. Novel drug delivery methods for the treatment of keratitis: moving away from surgical intervention. Expert Opin Drug Deliv. 2019;16(12):1381–91. https://doi.org/10.1080/17425247.2019.1690451.
Chhonker YS, Prasad YD, Chandasana H, Vishvkarma A, Mitra K, Shukla PK, et al. Amphotericin-B entrapped lecithin/chitosan nanoparticles for prolonged ocular application. Int J Biol Macromol. 2015;72:1451–8. https://doi.org/10.1016/j.ijbiomac.2014.10.014.
Lyu Q, Peng L, Hong X, Fan T, Li J, Cui Y, et al. Smart nano-micro platforms for ophthalmological applications: the state-of-the-art and future perspectives. Biomaterials. 2021;270:120682. https://doi.org/10.1016/j.biomaterials.2021.120682.
Han H, Gao Y, Chai M, Zhang X, Liu S, Huang Y, et al. Biofilm microenvironment activated supramolecular nanoparticles for enhanced photodynamic therapy of bacterial keratitis. J Control Release. 2020;327:676–87. https://doi.org/10.1016/j.jconrel.2020.09.014.
Baelo A, Levato R, Julián E, Crespo A, Astola J, Gavaldà J, et al. Disassembling bacterial extracellular matrix with DNase-coated nanoparticles to enhance antibiotic delivery in biofilm infections. J Control Release. 2015;209:150–8. https://doi.org/10.1016/j.jconrel.2015.04.028.
Tahara K, Karasawa K, Onodera R, Takeuchi H. Feasibility of drug delivery to the eye’s posterior segment by topical instillation of PLGA nanoparticles. Asian J Pharm Sci. 2017;12(4):394–9. https://doi.org/10.1016/j.ajps.2017.03.002.
Chandasana H, Prasad YD, Chhonker YS, Chaitanya TK, Mishra NN, Mitra K, et al. Corneal targeted nanoparticles for sustained natamycin delivery and their PK/PD indices: an approach to reduce dose and dosing frequency. Int J Pharm. 2014;477(1–2):317–25. https://doi.org/10.1016/j.ijpharm.2014.10.035.
da Silva SB, Ferreira D, Pintado M, Sarmento B. Chitosan-based nanoparticles for rosmarinic acid ocular delivery—in vitro tests. Int J Biol Macromol. 2016;84:112–20. https://doi.org/10.1016/j.ijbiomac.2015.11.070.
Silva NC, Silva S, Sarmento B, Pintado M. Chitosan nanoparticles for daptomycin delivery in ocular treatment of bacterial endophthalmitis. Drug deliv. 2015;22(7):885–93. https://doi.org/10.3109/10717544.2013.858195.
Ahsan SM, Rao CM. Condition responsive nanoparticles for managing infection and inflammation in keratitis. Nanoscale. 2017;9(28):9946–59. https://doi.org/10.1039/c7nr00922d.
Huang JF, Zhong J, Chen GP, Lin ZT, Deng Y, Liu YL, et al. A hydrogel-based hybrid theranostic contact lens for fungal keratitis. ACS Nano. 2016;10(7):6464–73. https://doi.org/10.1021/acsnano.6b00601.
Khor E, Lim LY. Implantable applications of chitin and chitosan. Biomaterials. 2003;24(13):2339–49. https://doi.org/10.1016/s0142-9612(03)00026-7.
Jain S, Mistry MA, Swarnakar NK. Enhanced dermal delivery of acyclovir using solid lipid nanoparticles. Drug Deliv Transl Res. 2011;1(5):395–406. https://doi.org/10.1007/s13346-011-0036-0.
de Oliveira IF, Barbosa EJ, Peters MCC, Henostroza MAB, Yukuyama MN, dos Santos NE, et al. Cutting-edge advances in therapy for the posterior segment of the eye: solid lipid nanoparticles and nanostructured lipid carriers. Int J Pharm. 2020;589:119831. https://doi.org/10.1016/j.ijpharm.2020.119831.
Khames A, Khaleel MA, El-Badawy MF, El-Nezhawy AOH. Natamycin solid lipid nanoparticles - sustained ocular delivery system of higher corneal penetration against deep fungal keratitis: preparation and optimization. Int J Nanomedicine. 2019;14:2515–31. https://doi.org/10.2147/IJN.S190502.
Kakkar S, Karuppayil SM, Raut JS, Giansanti F, Papucci L, Schiavone N, et al. Lipid-polyethylene glycol based nano-ocular formulation of ketoconazole. Int J Pharm. 2015;495(1):276–89. https://doi.org/10.1016/j.ijpharm.2015.08.088.
Chetoni P, Burgalassi S, Monti D, Tampucci S, Tullio V, Cuffini AM, et al. Solid lipid nanoparticles as promising tool for intraocular tobramycin delivery: pharmacokinetic studies on rabbits. Eur J Pharm Biopharm. 2016;109:214–23. https://doi.org/10.1016/j.ejpb.2016.10.006.
Zubairu Y, Negi LM, Iqbal Z, Talegaonkar S. Design and development of novel bioadhesive niosomal formulation for the transcorneal delivery of anti-infective agent: in-vitro and ex-vivo investigations. Asian J Pharm Sci. 2015;10(4):322–30. https://doi.org/10.1016/j.ajps.2015.02.001.
Elmotasem H, Awad GEA. A stepwise optimization strategy to formulate in situ gelling formulations comprising fluconazole-hydroxypropyl-beta-cyclodextrin complex loaded niosomal vesicles and Eudragit nanoparticles for enhanced antifungal activity and prolonged ocular delivery. Asian J Pharm Sci. 2020;15(5):617–36. https://doi.org/10.1016/j.ajps.2019.09.003.
Dubald M, Bourgeois S, Andrieu V, Fessi H. Ophthalmic drug delivery systems for antibiotherapy—a review. Pharmaceutics. 2018;10(1):10. https://doi.org/10.3390/pharmaceutics10010010.
Shimanovich U, Gedanken A. Nanotechnology solutions to restore antibiotic activity. J Mater Chem B. 2016;4(5):824–33. https://doi.org/10.1039/c5tb01527h.
Obuobi S, Julin K, Fredheim EGA, Johannessen M, Škalko-Basnet N. Liposomal delivery of antibiotic loaded nucleic acid nanogels with enhanced drug loading and synergistic anti-inflammatory activity against S. aureus intracellular infections. J Control Release. 2020;324:620–32. https://doi.org/10.1016/j.jconrel.2020.06.002.
Yousry C, Zikry PM, Salem HM, Basalious EB, El-Gazayerly ON. Integrated nanovesicular/self-nanoemulsifying system (INV/SNES) for enhanced dual ocular drug delivery: statistical optimization, in vitro and in vivo evaluation. Drug Deliv Transl Res. 2020;10(3):801–14. https://doi.org/10.1007/s13346-020-00716-5.
Ghosh AK, Rudramurthy SM, Gupta A, Choudhary H, Singh S, Thakur A, et al. Evaluation of liposomal and conventional amphotericin B in experimental fungal keratitis rabbit model. Transl Vis Sci Technol. 2019;8(3):35. https://doi.org/10.1167/tvst.8.3.35.
Goldblum D, Frueh BE, Zimmerli S, Böhnke M. Treatment of postkeratitis fusarium endophthalmitis with amphotericin B lipid complex. Cornea. 2000;19(6):853–6. https://doi.org/10.1097/00003226-200011000-00019.
Akbari V, Abedi D, Pardakhty A, Sadeghi-Aliabadi H. Release studies on ciprofloxacin loaded non-ionic surfactant vesicles. Avicenna J Med Biotechnol. 2015;7(2):69–75.
Wang Y, Cheetham AG, Angacian G, Su H, Xie L, Cui H. Peptide-drug conjugates as effective prodrug strategies for targeted delivery. Adv Drug Deliv Rev. 2017;110–111:112–26. https://doi.org/10.1016/j.addr.2016.06.015.
Han H, Hou Y, Chen X, Zhang P, Kang M, Jin Q, et al. Metformin-induced stromal depletion to enhance the penetration of gemcitabine-loaded magnetic nanoparticles for pancreatic cancer targeted therapy. J Am Chem Soc. 2020;142(10):4944–54. https://doi.org/10.1021/jacs.0c00650.
Han H, Valdepérez D, Jin Q, Yang B, Li Z, Wu Y, et al. Dual enzymatic reaction-assisted gemcitabine delivery systems for programmed pancreatic cancer therapy. ACS Nano. 2017;11(2):1281–91. https://doi.org/10.1021/acsnano.6b05541.
Rautio J, Kumpulainen H, Heimbach T, Oliyai R, Oh D, Järvinen T, et al. Prodrugs: design and clinical applications. Nat Rev Drug Discov. 2008;7(3):255–70. https://doi.org/10.1038/nrd2468.
Rautio J, Meanwell NA, Di L, Hageman MJ. The expanding role of prodrugs in contemporary drug design and development. Nat Rev Drug Discov. 2018;17(8):559–87. https://doi.org/10.1038/nrd.2018.46.
Pandey M, Choudhury H, Abdul-Aziz A, Bhattamisra SK, Gorain B, Su JST et al. Advancement on sustained antiviral ocular drug delivery for herpes simplex virus keratitis: recent update on potential investigation. Pharmaceutics. 2020;13(1). https://doi.org/10.3390/pharmaceutics13010001.
Chen Y, Kalia YN. Short-duration ocular iontophoresis of ionizable aciclovir prodrugs: a new approach to treat herpes simplex infections in the anterior and posterior segments of the eye. Int J Pharm. 2018;536(1):292–300. https://doi.org/10.1016/j.ijpharm.2017.11.069.
Gao Y, Wang J, Chai M, Li X, Deng Y, Jin Q, et al. Size and charge adaptive clustered nanoparticles targeting the biofilm microenvironment for chronic lung infection management. ACS Nano. 2020;14(5):5686–99. https://doi.org/10.1021/acsnano.0c00269.
Lemire JA, Harrison JJ, Turner RJ. Antimicrobial activity of metals: mechanisms, molecular targets and applications. Nat Rev Microbiol. 2013;11(6):371–84. https://doi.org/10.1038/nrmicro3028.
Chandrangsu P, Rensing C, Helmann JD. Metal homeostasis and resistance in bacteria. Nat Rev Microbiol. 2017;15(6):338–50. https://doi.org/10.1038/nrmicro.2017.15.
Chernousova S, Epple M. Silver as antibacterial agent: ion, nanoparticle, and metal. Angew Chem Int Ed Engl. 2013;52(6):1636–53. https://doi.org/10.1002/anie.201205923.
Kim JA, Åberg C, Salvati A, Dawson KA. Role of cell cycle on the cellular uptake and dilution of nanoparticles in a cell population. Nat Nanotechnol. 2012;7(1):62–8. https://doi.org/10.1038/nnano.2011.191.
Alarcon EI, Vulesevic B, Argawal A, Ross A, Bejjani P, Podrebarac J, et al. Coloured cornea replacements with anti-infective properties: expanding the safe use of silver nanoparticles in regenerative medicine. Nanoscale. 2016;8(12):6484–9. https://doi.org/10.1039/c6nr01339b.
Eckhardt S, Brunetto PS, Gagnon J, Priebe M, Giese B, Fromm KM. Nanobio silver: its interactions with peptides and bacteria, and its uses in medicine. Chem Rev. 2013;113(7):4708–54. https://doi.org/10.1021/cr300288v.
Le Ouay B, Stellacci F. Antibacterial activity of silver nanoparticles: a surface science insight. Nano Today. 2015;10(3):339–54. https://doi.org/10.1016/j.nantod.2015.04.002.
Qing Y, Cheng L, Li R, Liu G, Zhang Y, Tang X, et al. Potential antibacterial mechanism of silver nanoparticles and the optimization of orthopedic implants by advanced modification technologies. Int J Nanomedicine. 2018;13:3311–27. https://doi.org/10.2147/IJN.S165125.
Seong M, Lee DG. Silver nanoparticles against Salmonella enterica serotype typhimurium: role of inner membrane dysfunction. Curr Microbiol. 2017;74(6):661–70. https://doi.org/10.1007/s00284-017-1235-9.
Chatterjee T, Chatterjee BK, Majumdar D, Chakrabarti P. Antibacterial effect of silver nanoparticles and the modeling of bacterial growth kinetics using a modified Gompertz model. Biochim Biophys Acta. 2015;1850(2):299–306. https://doi.org/10.1016/j.bbagen.2014.10.022.
Zhao R, Lv M, Li Y, Sun M, Kong W, Wang L, et al. Stable nanocomposite based on PEGylated and silver nanoparticles loaded graphene oxide for long-term antibacterial activity. ACS Appl Mater Interfaces. 2017;9(18):15328–41. https://doi.org/10.1021/acsami.7b03987.
Siritongsuk P, Hongsing N, Thammawithan S, Daduang S, Klaynongsruang S, Tuanyok A, et al. Two-phase bactericidal mechanism of silver nanoparticles against Burkholderia pseudomallei. PLoS ONE. 2016;11(12):e0168098. https://doi.org/10.1371/journal.pone.0168098.
Long Y-M, Hu L-G, Yan X-T, Zhao X-C, Zhou Q-F, Cai Y, et al. Surface ligand controls silver ion release of nanosilver and its antibacterial activity against Escherichia coli. Int J Nanomedicine. 2017;12:3193–206. https://doi.org/10.2147/ijn.s132327.
Franci G, Falanga A, Galdiero S, Palomba L, Rai M, Morelli G, et al. Silver nanoparticles as potential antibacterial agents. Molecules. 2015;20(5):8856–74. https://doi.org/10.3390/molecules20058856.
Du J. Antibacterial, anti-biofilm and anticancer potentials of green synthesized silver nanoparticles using benzoin gum (Styrax benzoin) extract. Bioprocess Biosyst Eng. 2016;39(12):1923–31. https://doi.org/10.1007/s00449-016-1666-x.
Toffoletto N, Saramago B, Serro AP. Therapeutic ophthalmic lenses: a review Pharmaceutics. 2020;13(1):36. https://doi.org/10.3390/pharmaceutics13010036.
Liu X, Chen J, Qu C, Bo G, Jiang L, Zhao H, et al. A mussel-inspired facile method to prepare multilayer-AgNP-loaded contact lens for early treatment of bacterial and fungal keratitis. ACS Biomater Sci Eng. 2018;4(5):1568–79. https://doi.org/10.1021/acsbiomaterials.7b00977.
Luo LJ, Lin TY, Yao CH, Kuo PY, Matsusaki M, Harroun SG, et al. Dual-functional gelatin-capped silver nanoparticles for antibacterial and antiangiogenic treatment of bacterial keratitis. J Colloid Interface Sci. 2019;536:112–26. https://doi.org/10.1016/j.jcis.2018.10.041.
Bhatia E, Banerjee R. Hybrid silver-gold nanoparticles suppress drug resistant polymicrobial biofilm formation and intracellular infection. J Mater Chem B. 2020;8(22):4890–8. https://doi.org/10.1039/d0tb00158a.
Maillard JY, Hartemann P. Silver as an antimicrobial: facts and gaps in knowledge. Crit Rev Microbiol. 2013;39(4):373–83. https://doi.org/10.3109/1040841x.2012.713323.
Masse F, Ouellette M, Lamoureux G, Boisselier E. Gold nanoparticles in ophthalmology. Med Res Rev. 2019;39(1):302–27. https://doi.org/10.1002/med.21509.
Prow TW. Toxicity of nanomaterials to the eye. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2010;2(4):317–33. https://doi.org/10.1002/wnan.65.
An W, Zhang Y, Zhang X, Li K, Kang Y, Akhtar S, et al. Ocular toxicity of reduced graphene oxide or graphene oxide exposure in mouse eyes. Exp Eye Res. 2018;174:59–69. https://doi.org/10.1016/j.exer.2018.05.024.
Gao L, Zhuang J, Nie L, Zhang J, Zhang Y, Gu N, et al. Intrinsic peroxidase-like activity of ferromagnetic nanoparticles. Nat Nanotechnol. 2007;2(9):577–83. https://doi.org/10.1038/nnano.2007.260.
Jiang B, Duan D, Gao L, Zhou M, Fan K, Tang Y, et al. Standardized assays for determining the catalytic activity and kinetics of peroxidase-like nanozymes. Nat Protoc. 2018;13(7):1506–20. https://doi.org/10.1038/s41596-018-0001-1.
Dong J, Song L, Yin J-J, He W, Wu Y, Gu N, et al. Co3O4 nanoparticles with multi-enzyme activities and their application in immunohistochemical assay. ACS Appl Mater Interfaces. 2014;6(3):1959–70. https://doi.org/10.1021/am405009f.
He W, Liu Y, Yuan J, Yin JJ, Wu X, Hu X, et al. Au@Pt nanostructures as oxidase and peroxidase mimetics for use in immunoassays. Biomaterials. 2011;32(4):1139–47. https://doi.org/10.1016/j.biomaterials.2010.09.040.
Natalio F, Andre R, Hartog AF, Stoll B, Jochum KP, Wever R, et al. Vanadium pentoxide nanoparticles mimic vanadium haloperoxidases and thwart biofilm formation. Nat Nanotechnol. 2012;7(8):530–5. https://doi.org/10.1038/nnano.2012.91.
Jawaid P, Rehman MU, Zhao QL, Takeda K, Ishikawa K, Hori M, et al. Helium-based cold atmospheric plasma-induced reactive oxygen species-mediated apoptotic pathway attenuated by platinum nanoparticles. J Cell Mol Med. 2016;20(9):1737–48. https://doi.org/10.1111/jcmm.12880.
Liang M, Yan X. Nanozymes: from new concepts, mechanisms, and standards to applications. Acc Chem Res. 2019;52(8):2190–200. https://doi.org/10.1021/acs.accounts.9b00140.
Liang M, Fan K, Pan Y, Jiang H, Wang F, Yang D, et al. Fe3O4 magnetic nanoparticle peroxidase mimetic-based colorimetric assay for the rapid detection of organophosphorus pesticide and nerve agent. Anal Chem. 2013;85(1):308–12. https://doi.org/10.1021/ac302781r.
Asati A, Kaittanis C, Santra S, Perez JM. pH-tunable oxidase-like activity of cerium oxide nanoparticles achieving sensitive fluorigenic detection of cancer biomarkers at neutral pH. Anal Chem. 2011;83(7):2547–53. https://doi.org/10.1021/ac102826k.
Fan K, Cao C, Pan Y, Lu D, Yang D, Feng J, et al. Magnetoferritin nanoparticles for targeting and visualizing tumour tissues. Nat Nanotechnol. 2012;7(7):459–64. https://doi.org/10.1038/nnano.2012.90.
Ezraty B, Gennaris A, Barras F, Collet JF. Oxidative stress, protein damage and repair in bacteria. Nat Rev Microbiol. 2017;15(7):385–96. https://doi.org/10.1038/nrmicro.2017.26.
Wang Z, Dong K, Liu Z, Zhang Y, Chen Z, Sun H, et al. Activation of biologically relevant levels of reactive oxygen species by Au/g-C3N4 hybrid nanozyme for bacteria killing and wound disinfection. Biomaterials. 2017;113:145–57. https://doi.org/10.1016/j.biomaterials.2016.10.041.
Wang H, Li P, Yu D, Zhang Y, Wang Z, Liu C, et al. Unraveling the enzymatic activity of oxygenated carbon nanotubes and their application in the treatment of bacterial infections. Nano Lett. 2018;18(6):3344–51. https://doi.org/10.1021/acs.nanolett.7b05095.
Xi J, Wei G, An L, Xu Z, Xu Z, Fan L, et al. Copper/carbon hybrid nanozyme: tuning catalytic activity by the copper State for antibacterial therapy. Nano Lett. 2019;19(11):7645–54. https://doi.org/10.1021/acs.nanolett.9b02242.
Yan Z, Bing W, Ding C, Dong K, Ren J, Qu X. A H2O2-free depot for treating bacterial infection: localized cascade reactions to eradicate biofilms in vivo. Nanoscale. 2018;10(37):17656–62. https://doi.org/10.1039/c8nr03963a.
Shan J, Li X, Yang K, Xiu W, Wen Q, Zhang Y, et al. Efficient bacteria killing by Cu2WS4 nanocrystals with enzyme-like properties and bacteria-binding ability. ACS Nano. 2019;13(12):13797–808. https://doi.org/10.1021/acsnano.9b03868.
Xu Z, Qiu Z, Liu Q, Huang Y, Li D, Shen X, et al. Converting organosulfur compounds to inorganic polysulfides against resistant bacterial infections. Nat Commun. 2018;9(1):3713. https://doi.org/10.1038/s41467-018-06164-7.
Li J, Yu Y, Zhang L. Bismuth oxyhalide nanomaterials: layered structures meet photocatalysis. Nanoscale. 2014;6(15):8473–88. https://doi.org/10.1039/c4nr02553a.
Hsu CL, Li YJ, Jian HJ, Harroun SG, Wei SC, Ravindranath R, et al. Green synthesis of catalytic gold/bismuth oxyiodide nanocomposites with oxygen vacancies for treatment of bacterial infections. Nanoscale. 2018;10(25):11808–19. https://doi.org/10.1039/c8nr00800k.
Kost OA, Beznos OV, Davydova NG, Manickam DS, Nikolskaya II, Guller AE, et al. Superoxide dismutase 1 nanozyme for treatment of eye inflammation. Oxid Med Cell Longev. 2015;2015:5194239. https://doi.org/10.1155/2016/5194239.
Brogden KA. Antimicrobial peptides: pore formers or metabolic inhibitors in bacteria? Nat Rev Microbiol. 2005;3(3):238–50. https://doi.org/10.1038/nrmicro1098.
Schneider VA, Coorens M, Ordonez SR, Tjeerdsma-van Bokhoven JL, Posthuma G, van Dijk A, et al. Imaging the antimicrobial mechanism(s) of cathelicidin-2. Sci Rep. 2016;6:32948. https://doi.org/10.1038/srep32948.
Schneider VAF, Coorens M, Tjeerdsma-van Bokhoven JLM, Posthuma G, van Dijk A, Veldhuizen EJA et al. Imaging the antistaphylococcal activity of CATH-2: mechanism of attack and regulation of inflammatory response. mSphere. 2017;2(6):e00370–17. https://doi.org/10.1128/mSphere.00370-17.
Wiradharma N, Khan M, Yong LK, Hauser CA, Seow SV, Zhang S, et al. The effect of thiol functional group incorporation into cationic helical peptides on antimicrobial activities and spectra. Biomaterials. 2011;32(34):9100–8. https://doi.org/10.1016/j.biomaterials.2011.08.020.
Ordonez SR, Amarullah IH, Wubbolts RW, Veldhuizen EJA, Haagsman HP. Fungicidal mechanisms of cathelicidins LL-37 and CATH-2 revealed by live-cell imaging. Antimicrob Agents Chemother. 2014;58(4):2240–8. https://doi.org/10.1128/aac.01670-13.
Menzel LP, Chowdhury HM, Masso-Silva JA, Ruddick W, Falkovsky K, Vorona R, et al. Potent in vitro and in vivo antifungal activity of a small molecule host defense peptide mimic through a membrane-active mechanism. Sci Rep. 2017;7(1):4353. https://doi.org/10.1038/s41598-017-04462-6.
Helmerhorst EJ, Troxler RF, Oppenheim FG. The human salivary peptide histatin 5 exerts its antifungal activity through the formation of reactive oxygen species. Proc Natl Acad Sci U S A. 2001;98(25):14637–42. https://doi.org/10.1073/pnas.141366998.
Ishida W, Harada Y, Fukuda K, Fukushima A. Inhibition by the antimicrobial peptide LL37 of lipopolysaccharide-induced innate immune responses in human corneal fibroblasts. Invest Ophthalmol Vis Sci. 2016;57(1):30–9. https://doi.org/10.1167/iovs.15-17652.
Hancock REW, Sahl H-G. Antimicrobial and host-defense peptides as new anti-infective therapeutic strategies. Nat Biotechnol. 2006;24(12):1551–7. https://doi.org/10.1038/nbt1267.
Parmar A, Lakshminarayanan R, Iyer A, Mayandi V, Leng Goh ET, Lloyd DG, et al. Design and syntheses of highly potent teixobactin analogues against Staphylococcus aureus, methicillin-resistant Staphylococcus aureus (MRSA), and vancomycin-resistant Enterococci (VRE) in vitro and in vivo. J Med Chem. 2018;61(5):2009–17. https://doi.org/10.1021/acs.jmedchem.7b01634.
Clemens LE, Jaynes J, Lim E, Kolar SS, Reins RY, Baidouri H, et al. Designed host defense peptides for the treatment of bacterial keratitis. Invest Ophthalmol Vis Sci. 2017;58(14):6273–81. https://doi.org/10.1167/iovs.17-22243.
Yang Z, He S, Wang J, Yang Y, Zhang L, Li Y, et al. Rational design of short peptide variants by using Kunitzin-RE, an amphibian-derived bioactivity peptide, for acquired potent broad-spectrum antimicrobial and improved therapeutic potential of commensalism coinfection of pathogens. J Med Chem. 2019;62(9):4586–605. https://doi.org/10.1021/acs.jmedchem.9b00149.
Nekoueian K, Amiri M, Sillanpaa M, Marken F, Boukherroub R, Szunerits S. Carbon-based quantum particles: an electroanalytical and biomedical perspective. Chem Soc Rev. 2019;48(15):4281–316. https://doi.org/10.1039/c8cs00445e.
Bing W, Sun H, Yan Z, Ren J, Qu X. Programmed bacteria death induced by carbon dots with different surface charge. Small. 2016;12(34):4713–8. https://doi.org/10.1002/smll.201600294.
Harroun SG, Lai JY, Huang CC, Tsai SK, Lin HJ. Reborn from the ashes: turning organic molecules to antimicrobial carbon quantum dots. ACS Infect Dis. 2017;3(11):777–9. https://doi.org/10.1021/acsinfecdis.7b00150.
Jian HJ, Wu RS, Lin TY, Li YJ, Lin HJ, Harroun SG, et al. Super-cationic carbon quantum dots synthesized from spermidine as an eye drop formulation for topical treatment of bacterial keratitis. ACS Nano. 2017;11(7):6703–16. https://doi.org/10.1021/acsnano.7b01023.
Jian HJ, Yu J, Li YJ, Unnikrishnan B, Huang YF, Luo LJ, et al. Highly adhesive carbon quantum dots from biogenic amines for prevention of biofilm formation. Chem Eng J. 2020;386:123913. https://doi.org/10.1016/j.cej.2019.123913.
Lin HY, Wang SW, Mao JY, Chang HT, Harroun SG, Lin HJ, et al. Carbonized nanogels for simultaneous antibacterial and antioxidant treatment of bacterial keratitis. Chem Eng J. 2021;411:128469. https://doi.org/10.1016/j.cej.2021.128469.
Hamblin MR. Antimicrobial photodynamic inactivation: a bright new technique to kill resistant microbes. Curr Opin Microbiol. 2016;33:67–73. https://doi.org/10.1016/j.mib.2016.06.008.
Kesavardhana S, Kanneganti T-D. Stressed-out ROS take a silent death route. Nat Immunol. 2018;19(2):103–5. https://doi.org/10.1038/s41590-017-0034-6.
Wainwright M, Maisch T, Nonell S, Plaetzer K, Almeida A, Tegos GP, et al. Photoantimicrobials—are we afraid of the light? Lancet Infect Dis. 2017;17(2):e49–55. https://doi.org/10.1016/s1473-3099(16)30268-7.
Han H, Jin Q, Wang H, Teng W, Wu J, Tong H, et al. Intracellular dual fluorescent lightup bioprobes for image-guided photodynamic cancer therapy. Small. 2016;12(28):3870–8. https://doi.org/10.1002/smll.201600950.
Lucky SS, Soo KC, Zhang Y. Nanoparticles in photodynamic therapy. Chem Rev. 2015;115(4):1990–2042. https://doi.org/10.1021/cr5004198.
Ren B, Li K, Liu Z, Liu G, Wang H. White light-triggered zwitterionic polymer nanoparticles based on an AIE-active photosensitizer for photodynamic antimicrobial therapy. J Mater Chem B. 2020;8(47):10754–63. https://doi.org/10.1039/d0tb02272a.
Parker S. The use of diffuse laser photonic energy and indocyanine green photosensitiser as an adjunct to periodontal therapy. Br Dent J. 2013;215(4):167–71. https://doi.org/10.1038/sj.bdj.2013.790.
Cieplik F, Deng D, Crielaard W, Buchalla W, Hellwig E, Al-Ahmad A, et al. Antimicrobial photodynamic therapy—what we know and what we don’t. Crit Rev Microbiol. 2018;44(5):571–89. https://doi.org/10.1080/1040841x.2018.1467876.
Parsons C, McCoy CP, Gorman SP, Jones DS, Bell SEJ, Brady C, et al. Anti-infective photodynamic biomaterials for the prevention of intraocular lens-associated infectious endophthalmitis. Biomaterials. 2009;30(4):597–602. https://doi.org/10.1016/j.biomaterials.2008.10.015.
Chen H, Yang J, Sun L, Zhang H, Guo Y, Qu J, et al. Synergistic chemotherapy and photodynamic therapy of endophthalmitis mediated by zeolitic imidazolate framework-based drug delivery systems. Small. 2019;15(47):e1903880. https://doi.org/10.1002/smll.201903880.
Su G, Wei Z, Wang L, Shen J, Baudouin C, Labbé A, et al. Evaluation of toluidine blue-mediated photodynamic therapy for experimental bacterial keratitis in rabbits. Transl Vis Sci Technol. 2020;9(3):13. https://doi.org/10.1167/tvst.9.3.13.
Shih MH, Huang FC. Effects of photodynamic therapy on rapidly growing nontuberculous mycobacteria keratitis. Invest Ophthalmol Vis Sci. 2011;52(1):223–9. https://doi.org/10.1167/iovs.10-5593.
Wu M-F, Deichelbohrer M, Tschernig T, Laschke MW, Szentmáry N, Hüttenberger D, et al. Chlorin e6 mediated photodynamic inactivation for multidrug resistant Pseudomonas aeruginosa keratitis in mice in vivo. Sci Rep. 2017;7(1):44537. https://doi.org/10.1038/srep44537.
Hu D, Deng Y, Jia F, Jin Q, Ji J. Surface charge switchable supramolecular nanocarriers for nitric oxide synergistic photodynamic eradication of biofilms. ACS Nano. 2020;14(1):347–59. https://doi.org/10.1021/acsnano.9b05493.
Chen X, Selloni A. Introduction: titanium dioxide (TiO2) nanomaterials. Chem Rev. 2014;114(19):9281–2. https://doi.org/10.1021/cr500422r.
Rajh T, Dimitrijevic NM, Bissonnette M, Koritarov T, Konda V. Titanium dioxide in the service of the biomedical revolution. Chem Rev. 2014;114(19):10177–216. https://doi.org/10.1021/cr500029g.
Gao Q, Feng T, Huang D, Liu P, Lin P, Wu Y, et al. Antibacterial and hydroxyapatite-forming coating for biomedical implants based on polypeptide-functionalized titania nanospikes. Biomater Sci. 2020;8(1):278–89. https://doi.org/10.1039/c9bm01396b.
Gomart G, Denis J, Bourcier T, Dory A, Abou-Bacar A, Candolfi E, et al. In vitro amoebicidal activity of titanium dioxide/UV—a combination against Acanthamoeba. Invest Ophthalmol Vis Sci. 2018;59(11):4567–71. https://doi.org/10.1167/iovs.18-25003.
Feng Y, Liu L, Zhang J, Aslan H, Dong M. Photoactive antimicrobial nanomaterials. J Mater Chem B. 2017;5(44):8631–52. https://doi.org/10.1039/c7tb01860f.
Li X, Bai H, Yang Y, Yoon J, Wang S, Zhang X. Supramolecular antibacterial materials for combatting antibiotic resistance. Adv Mater. 2019;31(5):1805092. https://doi.org/10.1002/adma.201805092.
Ueda K, Zhao J, Kim HJ, Sparrow JR. Photodegradation of retinal bisretinoids in mouse models and implications for macular degeneration. Proc Natl Acad Sci U S A. 2016;113(25):6904–9. https://doi.org/10.1073/pnas.1524774113.
Li L, Han X, Wang M, Li C, Jia T, Zhao X. Recent advances in the development of near-infrared organic photothermal agents. Chem Eng J. 2021:128844. https://doi.org/10.1016/j.cej.2021.128844.
Han H, Zhang S, Wang Y, Chen T, Jin Q, Chen Y, et al. Biomimetic drug nanocarriers prepared by miniemulsion polymerization for near-infrared imaging and photothermal therapy. Polymer. 2016;82:255–61. https://doi.org/10.1016/j.polymer.2015.11.022.
Tan L, Li J, Liu X, Cui Z, Yang X, Zhu S, et al. Rapid biofilm eradication on bone implants using red phosphorus and near-infrared light. Adv Mater. 2018;30(31):1801808. https://doi.org/10.1002/adma.201801808.
Li J, Liu X, Tan L, Cui Z, Yang X, Liang Y, et al. Zinc-doped Prussian blue enhances photothermal clearance of Staphylococcus aureus and promotes tissue repair in infected wounds. Nat Commun. 2019;10(1):4490. https://doi.org/10.1038/s41467-019-12429-6.
Zhang L, Wang Y, Wang J, Wang Y, Chen A, Wang C, et al. Photon-responsive antibacterial nanoplatform for synergistic photothermal-/pharmaco-therapy of skin infection. ACS Appl Mater Interfaces. 2019;11(1):300–10. https://doi.org/10.1021/acsami.8b18146.
Cai X, Gao W, Zhang L, Ma M, Liu T, Du W, et al. Enabling Prussian blue with tunable localized surface plasmon resonances: simultaneously enhanced dual-mode imaging and tumor photothermal therapy. ACS Nano. 2016;10(12):11115–26. https://doi.org/10.1021/acsnano.6b05990.
Weissleder R. A clearer vision for in vivo imaging. Nat Biotechnol. 2001;19(4):316–7. https://doi.org/10.1038/86684.
Yang Y, He P, Wang Y, Bai H, Wang S, Xu J-F, et al. Supramolecular radical anions triggered by bacteria in situ for selective photothermal therapy. Angew Chem Int Ed Engl. 2017;56(51):16239–42. https://doi.org/10.1002/anie.201708971.
Liu Y, Guo Z, Li F, Xiao Y, Zhang Y, Bu T, et al. Multifunctional magnetic copper ferrite nanoparticles as Fenton-like reaction and near-infrared photothermal agents for synergetic antibacterial therapy. ACS Appl Mater Interfaces. 2019;11(35):31649–60. https://doi.org/10.1021/acsami.9b10096.
He J, Huang X, Li YC, Liu Y, Babu T, Aronova MA, et al. Self-assembly of amphiphilic plasmonic micelle-like nanoparticles in selective solvents. J Am Chem Soc. 2013;135(21):7974–84. https://doi.org/10.1021/ja402015s.
Gao L, Fei J, Zhao J, Li H, Cui Y, Li J. Hypocrellin-loaded gold nanocages with high two-photon efficiency for photothermal/photodynamic cancer therapy in vitro. ACS Nano. 2012;6(9):8030–40.
Lee WC, Lim CHYX, Shi H, Tang LAL, Wang Y, Lim CT, et al. Origin of enhanced stem cell growth and differentiation on graphene and graphene oxide. ACS Nano. 2011;5(9):7334–41. https://doi.org/10.1021/nn202190c.
Yang K, Zhang S, Zhang G, Sun X, Lee S-T, Liu Z. Graphene in mice: ultrahigh in vivo tumor uptake and efficient photothermal therapy. Nano Lett. 2010;10(9):3318–23. https://doi.org/10.1021/nl100996u.
Chen Z, Zhao P, Luo Z, Zheng M, Tian H, Gong P, et al. Cancer cell membrane-biomimetic nanoparticles for homologous-targeting dual-modal imaging and photothermal therapy. ACS Nano. 2016;10(11):10049–57.
Cai Y, Liang P, Tang Q, Yang X, Si W, Huang W, et al. Diketopyrrolopyrrole-triphenylamine organic nanoparticles as multifunctional reagents for photoacoustic imaging-guided photodynamic/photothermal synergistic tumor therapy. ACS Nano. 2017;11(1):1054–63. https://doi.org/10.1021/acsnano.6b07927.
Xu JW, Yao K, Xu ZK. Nanomaterials with a photothermal effect for antibacterial activities: an overview. Nanoscale. 2019;11(18):8680–91. https://doi.org/10.1039/c9nr01833f.
Liu Y, Ai K, Liu J, Deng M, He Y, Lu L. Dopamine-melanin colloidal nanospheres: an efficient near-infrared photothermal therapeutic agent for in vivo cancer therapy. Adv Mater. 2013;25(9):1353–9. https://doi.org/10.1002/adma.201204683.
Cheng L, Yang K, Chen Q, Liu Z. Organic stealth nanoparticles for highly effective in vivo near-infrared photothermal therapy of cancer. ACS Nano. 2012;6(6):5605–13. https://doi.org/10.1021/nn301539m.
Cobley CM, Chen JY, Cho EC, Wang LV, Xia YN. Gold nanostructures: a class of multifunctional materials for biomedical applications. Chem Soc Rev. 2011;40(1):44–56. https://doi.org/10.1039/b821763g.
Kriegel I, Scotognella F, Manna L. Plasmonic doped semiconductor nanocrystals: properties, fabrication, applications and perspectives. Phys Rep. 2017;674:1–52. https://doi.org/10.1016/j.physrep.2017.01.003.
Chen J, Glaus C, Laforest R, Zhang Q, Yang M, Gidding M, et al. Gold nanocages as photothermal transducers for cancer treatment. Small. 2010;6(7):811–7. https://doi.org/10.1002/smll.200902216.
Khantamat O, Li CH, Yu F, Jamison AC, Shih WC, Cai C et al. Gold nanoshell-decorated silicone surfaces for the near-infrared (NIR) photothermal destruction of the pathogenic bacterium E. faecalis. ACS Appl Mater Interfaces. 2015;7(7):3981–93. https://doi.org/10.1021/am506516r.
Abdou Mohamed MA, Raeesi V, Turner PV, Rebbapragada A, Banks K, Chan WC. A versatile plasmonic thermogel for disinfection of antimicrobial resistant bacteria. Biomaterials. 2016;97:154–63. https://doi.org/10.1016/j.biomaterials.2016.04.009.
Hu D, Li H, Wang B, Ye Z, Lei W, Jia F, et al. Surface-adaptive gold nanoparticles with effective adherence and enhanced photothermal ablation of methicillin-resistant Staphylococcus aureus biofilm. ACS Nano. 2017;11(9):9330–9. https://doi.org/10.1021/acsnano.7b04731.
Wu S, Li A, Zhao X, Zhang C, Yu B, Zhao N, et al. Silica-coated gold-silver nanocages as photothermal antibacterial agents for combined anti-infective therapy. ACS Appl Mater Interfaces. 2019;11(19):17177–83. https://doi.org/10.1021/acsami.9b01149.
Peng Y, Liu Y, Lu X, Wang S, Chen M, Huang W, et al. Ag-hybridized plasmonic Au-triangular nanoplates: highly sensitive photoacoustic/Raman evaluation and improved antibacterial/photothermal combination therapy. J Mater Chem B. 2018;6(18):2813–20. https://doi.org/10.1039/c8tb00617b.
He J, Qiao Y, Zhang H, Zhao J, Li W, Xie T, et al. Gold–silver nanoshells promote wound healing from drug-resistant bacteria infection and enable monitoring via surface-enhanced Raman scattering imaging. Biomaterials. 2020;234:119763. https://doi.org/10.1016/j.biomaterials.2020.119763.
Wang S, Riedinger A, Li H, Fu C, Liu H, Li L, et al. Plasmonic copper sulfide nanocrystals exhibiting near-infrared photothermal and photodynamic therapeutic effects. ACS Nano. 2015;9(2):1788–800. https://doi.org/10.1021/nn506687t.
Dai X, Zhao Y, Yu Y, Chen X, Wei X, Zhang X, et al. Single continuous near-infrared laser-triggered photodynamic and photothermal ablation of antibiotic-resistant bacteria using effective targeted copper sulfide nanoclusters. ACS Appl Mater Interfaces. 2017;9(36):30470–9. https://doi.org/10.1021/acsami.7b09638.
Huang J, Zhou J, Zhuang J, Gao H, Huang D, Wang L, et al. Strong near-infrared absorbing and biocompatible CuS nanoparticles for rapid and efficient photothermal ablation of gram-positive and -negative bacteria. ACS Appl Mater Interfaces. 2017;9(42):36606–14. https://doi.org/10.1021/acsami.7b11062.
Qiao Y, Ping Y, Zhang H, Zhou B, Liu F, Yu Y, et al. Laser-activatable CuS nanodots to treat multidrug-resistant bacteria and release copper ion to accelerate healing of infected chronic nonhealing wounds. ACS Appl Mater Interfaces. 2019;11(4):3809–22. https://doi.org/10.1021/acsami.8b21766.
Xiao J, Zhu Y, Huddleston S, Li P, Xiao B, Farha OK, et al. Copper metal-organic framework nanoparticles stabilized with folic acid improve wound healing in diabetes. ACS Nano. 2018;12(2):1023–32. https://doi.org/10.1021/acsnano.7b01850.
Xiao J, Chen S, Yi J, Zhang H, Ameer GA. A cooperative copper metal-organic framework-hydrogel system improves wound healing in diabetes. Adv Funct Mater. 2017;27(1). https://doi.org/10.1002/adfm.201604872.
Qiao Y, He J, Chen W, Yu Y, Li W, Du Z, et al. Light-activatable synergistic therapy of drug-resistant bacteria-infected cutaneous chronic wounds and nonhealing keratitis by cupriferous hollow nanoshells. ACS Nano. 2020;14(3):3299–315. https://doi.org/10.1021/acsnano.9b08930.
Ye Y, He J, Qiao Y, Qi Y, Zhang H, Santos HA, et al. Mild temperature photothermal assisted anti-bacterial and anti-inflammatory nanosystem for synergistic treatment of post-cataract surgery endophthalmitis. Theranostics. 2020;10(19):8541–57. https://doi.org/10.7150/thno.46895.
Sahoo N, Narasimhan A, Dhar P, Das SK. Non-Fourier thermal transport induced structural hierarchy and damage to collagen ultrastructure subjected to laser irradiation. Int J Hyperthermia. 2018;34(3):229–42. https://doi.org/10.1080/02656736.2017.1342873.
Gao G, Jiang YW, Sun W, Guo Y, Jia HR, Yu XW, et al. Molecular targeting-mediated mild-temperature photothermal therapy with a smart albumin-based nanodrug. Small. 2019;15(33):e1900501. https://doi.org/10.1002/smll.201900501.
Pan L, Liu J, Shi J. Nuclear-targeting gold nanorods for extremely low NIR activated photothermal therapy. ACS Appl Mater Interfaces. 2017;9(19):15952–61. https://doi.org/10.1021/acsami.7b03017.
Ge JC, Jia QY, Liu WM, Lan MH, Zhou BJ, Guo L, et al. Carbon dots with intrinsic theranostic properties for bioimaging, red-light-triggered photodynamic/photothermal simultaneous therapy in vitro and in vivo. Adv Healthc Mater. 2016;5(6):665–75. https://doi.org/10.1002/adhm.201500720.
Wareham LK, Southam HM, Poole RK. Do nitric oxide, carbon monoxide and hydrogen sulfide really qualify as “gasotransmitters” in bacteria? Biochem Soc Trans. 2018;46(5):1107–18. https://doi.org/10.1042/BST20170311.
Macmicking J, Xie QW, Nathan C. Nitric oxide and macrophage function. Annu Rev Immunol. 1997;15(1):323–50. https://doi.org/10.1146/annurev.immunol.15.1.323.
Fang FC. Perspectives series: host/pathogen interactions. Mechanisms of nitric oxide-related antimicrobial activity. J Clin Invest. 1997;99(12):2818–25. https://doi.org/10.1172/jci119473.
Husain M, Bourret TJ, McCollister BD, Jones-Carson J, Laughlin J, Vazquez-Torres A. Nitric oxide evokes an adaptive response to oxidative stress by arresting respiration. J Biol Chem. 2008;283(12):7682–9. https://doi.org/10.1074/jbc.M708845200.
Jones-Carson J, Yahashiri A, Kim JS, Liu L, Fitzsimmons LF, Weiss DS et al. Nitric oxide disrupts bacterial cytokinesis by poisoning purine metabolism. Sci Adv. 2020;6(9):eaaz0260. https://doi.org/10.1126/sciadv.aaz0260.
Schapiro JM, Libby SJ, Fang FC. Inhibition of bacterial DNA replication by zinc mobilization during nitrosative stress. Proc Natl Acad Sci U S A. 2003;100(14):8496–501. https://doi.org/10.1073/pnas.1033133100.
Carpenter AW, Schoenfisch MH. Nitric oxide release: part II. therapeutic applications. Chem Soc Rev. 2012;41(10):3742–52. https://doi.org/10.1039/c2cs15273h.
Sadrearhami Z, Nguyen T-K, Namivandi-Zangeneh R, Jung K, Wong EHH, Boyer C. Recent advances in nitric oxide delivery for antimicrobial applications using polymer-based systems. J Mater Chem B. 2018;6(19):2945–59. https://doi.org/10.1039/c8tb00299a.
Riccio DA, Schoenfisch MH. Nitric oxide release: part I. macromolecular scaffolds. Chem Soc Rev. 2012;41(10):3731. https://doi.org/10.1039/c2cs15272j.
Aveyard J, Deller RC, Lace R, Williams RL, Kaye SB, Kolegraff KN, et al. Antimicrobial nitric oxide releasing contact lens gels for the treatment of microbial keratitis. ACS Appl Mater Interfaces. 2019;11(41):37491–501. https://doi.org/10.1021/acsami.9b13958.
Jeong H, Park JH, Shin JH, Yoo JC, Park CY, Hong J. Prolonged release period of nitric oxide gas for treatment of bacterial keratitis by amine-rich polymer decoration of nanoparticles. Chem Mater. 2018;30(23):8528–37. https://doi.org/10.1021/acs.chemmater.8b03332.
Yim B, Park JH, Jeong H, Hong J, Kim M, Chang M, et al. Effect of nitric oxide on Acanthamoeba castellanii. Invest Ophthalmol Vis Sci. 2018;59(8):3239–48. https://doi.org/10.1167/iovs.18-23786.
Deng Y, Jia F, Chen S, Shen Z, Jin Q, Fu G, et al. Nitric oxide as an all-rounder for enhanced photodynamic therapy: hypoxia relief, glutathione depletion and reactive nitrogen species generation. Biomaterials. 2018;187:55–65. https://doi.org/10.1016/j.biomaterials.2018.09.043.
Tellios V, Liu H, Tellios N, Li X, Hutnik CML. Administration of nitric oxide through a novel copper-chitosan delivery system in human corneal and limbal epithelial cell injury. Invest Ophthalmol Vis Sci. 2018;59(2):967–77. https://doi.org/10.1167/iovs.17-23044.
Huang D, Chen YS, Rupenthal ID. Overcoming ocular drug delivery barriers through the use of physical forces. Adv Drug Deliv Rev. 2018;126:96–112. https://doi.org/10.1016/j.addr.2017.09.008.
Funding
This research was supported by the Natural Science Foundation of China (Grant Nos. 22005265, 81870641), National Key R&D Program of China (Grant No. 2018YFC1106104), Key Research and Development Program of Zhejiang Province (Grant No. 2020C03035), the Joint Funds of the Zhejiang Provincial Natural Science Foundation of China (Grant No. LBY21E030002), Zhejiang TCM Science and Technology Program (Grant No. 2021ZQ053), and Zhejiang Provincial Ten Thousand Talents Program (Grant No. 2018R52001).
Author information
Authors and Affiliations
Contributions
All authors whose names appear on the submission made substantial contributions to the article. Wenjie Fan, Haijie Han—writing and original draft preparation; Wenjie Fan, Haijie Han, Yaoyao Chen, Xiaobo Zhang, Yifan Gao, Su Li, Qiao Jin, Jian Ji, Ke Yao—writing, editing, and critical revision of intellectual content; Haijie Han, Qiao Jin, Jian Ji, Ke Yao—conceptualization and supervision. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable. No human subjects or animal studies were involved in the manuscript.
Consent for publication
All authors have given their consent for publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fan, W., Han, H., Chen, Y. et al. Antimicrobial nanomedicine for ocular bacterial and fungal infection. Drug Deliv. and Transl. Res. 11, 1352–1375 (2021). https://doi.org/10.1007/s13346-021-00966-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-021-00966-x