Abstract
Background
STELLA-LONG TERM was a 3-year post-marketing surveillance study that evaluated the long-term safety and effectiveness of ipragliflozin in Japanese patients with type 2 diabetes mellitus (T2DM). This subgroup analysis examined the safety and effectiveness of ipragliflozin in treatment-naïve and non-naïve patients.
Materials and methods
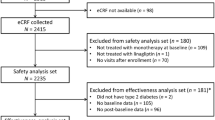
Patients were stratified into two subgroups: treatment-naïve (patients who had not received any antidiabetic drugs before starting ipragliflozin monotherapy) and non-naïve (all other patients). Patients who had added or switched antidiabetic drugs during follow-up were excluded from the analysis from that point. The incidence of adverse drug reactions (ADRs) and changes from baseline in glycosylated hemoglobin (HbA1c), body weight, fasting plasma glucose (FPG) and laboratory parameters were assessed.
Results
Of the 11,051 patients in the safety analysis set, 1980 patients (17.92%) were treatment-naïve and 9071 (82.08%) were non-naïve. In the safety analysis set, treatment-naïve patients reported significantly lower incidences of ADRs (10.81% vs 20.87%; p < 0.001) and serious ADRs (0.86% vs 2.09%; p < 0.001) compared with non-naïve patients, as well as significantly lower incidences of polyuria/pollakiuria, volume depletion-related events, skin complications and renal disorders. In the effectiveness analysis, sustained and significant reductions from baseline to 36 months were observed in HbA1c, FPG and body weight in both treatment-naïve and non-naïve patients (all p < 0.001 vs baseline).
Conclusions
Over 3 years, ipragliflozin was better tolerated in treatment-naive than in non-naive Japanese patients with T2DM and had similar efficacy in these populations. Therefore, ipragliflozin is a useful first-line treatment option for patients with T2DM.
Clinical trial registration
ClinicalTrials.gov: NCT02479399.

Similar content being viewed by others
References
Araki E, Goto A, Kondo T, Noda M, Noto H, Origasa H, Osawa H, Taguchi A, Tanizawa Y, Tobe K, Yoshioka N. Japanese clinical practice guideline for diabetes 2019. J Diabetes Investig. 2020;11(4):1020–76. https://doi.org/10.1111/jdi.13306.
Arnott C, Li Q, Kang A, Neuen BL, Bompoint S, Lam CSP, Rodgers A, Mahaffey KW, Cannon CP, Perkovic V, Jardine MJ, Neal B. Sodium-glucose cotransporter 2 inhibition for the prevention of cardiovascular events in patients with type 2 diabetes mellitus: a systematic review and meta-analysis. J Am Heart Assoc. 2020;9(3):e014908. https://doi.org/10.1161/JAHA.119.014908.
Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, Edwards R, Agarwal R, Bakris G, Bull S, Cannon CP, Capuano G, Chu PL, de Zeeuw D, Greene T, Levin A, Pollock C, Wheeler DC, Yavin Y, Zhang H, Zinman B, Meininger G, Brenner BM, Mahaffey KW, Investigators CT. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380(24):2295–306. https://doi.org/10.1056/NEJMoa1811744.
Radholm K, Figtree G, Perkovic V, Solomon SD, Mahaffey KW, de Zeeuw D, Fulcher G, Barrett TD, Shaw W, Desai M, Matthews DR, Neal B. Canagliflozin and heart failure in type 2 diabetes mellitus: results from the CANVAS program. Circulation. 2018;138(5):458–68. https://doi.org/10.1161/CIRCULATIONAHA.118.034222.
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, Broedl UC, Inzucchi SE, Investigators E-RO. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–28. https://doi.org/10.1056/NEJMoa1504720.
Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, Federici M, Filippatos G, Grobbee DE, Hansen TB, Huikuri HV, Johansson I, Juni P, Lettino M, Marx N, Mellbin LG, Ostgren CJ, Rocca B, Roffi M, Sattar N, Seferovic PM, Sousa-Uva M, Valensi P, Wheeler DC. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41(2):255–323. https://doi.org/10.1093/eurheartj/ehz486.
Irons BK, Minze MG. Drug treatment of type 2 diabetes mellitus in patients for whom metformin is contraindicated. Diabetes Metab Syndr Obes. 2014;7:15–24. https://doi.org/10.2147/DMSO.S38753.
Davies MJ, D’Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, Rossing P, Tsapas A, Wexler DJ, Buse JB. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41(12):2669–701. https://doi.org/10.2337/dci18-0033.
Bailey CJ, Morales Villegas EC, Woo V, Tang W, Ptaszynska A, List JF. Efficacy and safety of dapagliflozin monotherapy in people with type 2 diabetes: a randomized double-blind placebo-controlled 102-week trial. Diabet Med. 2015;32(4):531–41. https://doi.org/10.1111/dme.12624.
Ferrannini E, Ramos SJ, Salsali A, Tang W, List JF. Dapagliflozin monotherapy in type 2 diabetic patients with inadequate glycemic control by diet and exercise: a randomized, double-blind, placebo-controlled, phase 3 trial. Diabetes Care. 2010;33(10):2217–24. https://doi.org/10.2337/dc10-0612.
Ferrannini E, Seman L, Seewaldt-Becker E, Hantel S, Pinnetti S, Woerle HJ. A phase IIb, randomized, placebo-controlled study of the SGLT2 inhibitor empagliflozin in patients with type 2 diabetes. Diabetes Obes Metab. 2013;15(8):721–8. https://doi.org/10.1111/dom.12081.
Kutoh E, Wada A, Murayama T, Takizawa Y. Canagliflozin as an initial therapy in drug-naive subjects with type 2 diabetes mellitus: a potential involvement of atherogenic lipids in its glycemic efficacy. Drugs R D. 2017;17(2):313–20. https://doi.org/10.1007/s40268-017-0179-7.
Muscelli E, Astiarraga B, Barsotti E, Mari A, Schliess F, Nosek L, Heise T, Broedl UC, Woerle HJ, Ferrannini E. Metabolic consequences of acute and chronic empagliflozin administration in treatment-naive and metformin pretreated patients with type 2 diabetes. Diabetologia. 2016;59(4):700–8. https://doi.org/10.1007/s00125-015-3845-8.
Nishimura R, Tanaka Y, Koiwai K, Inoue K, Hach T, Salsali A, Lund SS, Broedl UC. Effect of empagliflozin monotherapy on postprandial glucose and 24-hour glucose variability in Japanese patients with type 2 diabetes mellitus: a randomized, double-blind, placebo-controlled, 4-week study. Cardiovasc Diabetol. 2015;14:11. https://doi.org/10.1186/s12933-014-0169-9.
Roden M, Weng J, Eilbracht J, Delafont B, Kim G, Woerle HJ, Broedl UC, Investigators E-RMt. Empagliflozin monotherapy with sitagliptin as an active comparator in patients with type 2 diabetes: a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Diabetes Endocrinol. 2013;1(3):208–19. https://doi.org/10.1016/S2213-8587(13)70084-6.
Poole RM, Dungo RT. Ipragliflozin: first global approval. Drugs. 2014;74(5):611–7. https://doi.org/10.1007/s40265-014-0204-x.
Kadokura T, Akiyama N, Kashiwagi A, Utsuno A, Kazuta K, Yoshida S, Nagase I, Smulders R, Kageyama S. Pharmacokinetic and pharmacodynamic study of ipragliflozin in Japanese patients with type 2 diabetes mellitus: a randomized, double-blind, placebo-controlled study. Diabetes Res Clin Pract. 2014;106(1):50–6. https://doi.org/10.1016/j.diabres.2014.07.020.
Kashiwagi A, Akiyama N, Shiga T, Kazuta K, Utsuno A, Yoshida S, Ueyama E. Efficacy and safety of ipragliflozin as an add-on to a sulfonylurea in Japanese patients with inadequately controlled type 2 diabetes: results of the randomized, placebo-controlled, double-blind, phase III EMIT study. Diabetol Int. 2015;6:125–38. https://doi.org/10.1007/s13340-014-0184-9.
Kashiwagi A, Kazuta K, Takinami Y, Yoshida S, Utsuno A, Nagase I. Ipragliflozin improves glycemic control in Japanese patients with type 2 diabetes mellitus: the BRIGHTEN study. Diabetol Int. 2015;6:8–18. https://doi.org/10.1007/s13340-014-0164-0.
Kashiwagi A, Kazuta K, Yoshida S, Nagase I. Randomized, placebo-controlled, double-blind glycemic control trial of novel sodium-dependent glucose cotransporter 2 inhibitor ipragliflozin in Japanese patients with type 2 diabetes mellitus. J Diabetes Investig. 2014;5(4):382–91. https://doi.org/10.1111/jdi.12156.
Kashiwagi A, Shiga T, Akiyama N, Kazuta K, Utsuno A, Yoshida S, Ueyama E. Efficacy and safety of ipragliflozin as an add-on to pioglitazone in Japanese patients with inadequately controlled type 2 diabetes: results of the randomized, placebo-controlled, double-blind, placebo-controlled study (the SPOTLIGHT study). Diabetol Int. 2015;6:104–16. https://doi.org/10.1007/s13340-014-0182-y.
Kashiwagi A, Takahashi H, Ishikawa H, Yoshida S, Kazuta K, Utsuno A, Ueyama E. A randomized, double-blind, placebo-controlled study on long-term efficacy and safety of ipragliflozin treatment in patients with type 2 diabetes mellitus and renal impairment: results of the long-term ASP1941 safety evaluation in patients with type 2 diabetes with renal impairment (LANTERN) study. Diabetes Obes Metab. 2015;17(2):152–60. https://doi.org/10.1111/dom.12403.
Kashiwagi A, Isaka H, Nakahama H, Kazuta K, Utsuno A, Yoshida S. Long-term safety, tolerability and efficacy of ipragliflozin in combination with nateglinide in Japanese patients with type 2 diabetes mellitus inadequately controlled with nateglinide alone—CANDLE study [in Japanese]. Jpn Pharmacol Ther. 2014;42:959–75.
Kashiwagi A, Isaka H, Takinami Y, Kazuta K, Utsuno A, Yoshida S. Long-term safety and efficacy of ipragliflozin in combination with an α-glucosidase inhibitor in Japanese patients with type 2 diabetes mellitus inadequately controlled with an α-glucosidase inhibitor alone–AGLOW study [in Japanese]. Jpn Pharmacol Ther. 2014;42:923–39.
Kashiwagi A, Kawano H, Kazuta K, Utsuno A, Yoshida S. Long-term safety, tolerability and efficacy of ipragliflozin in Japanese patients with type 2 diabetes mellitus—IGNITE study [in Japanese]. Jpn Pharmacol Ther. 2015;43:85–100.
Kashiwagi A, Kazuta K, Goto K, Yoshida S, Ueyama E, Utsuno A. Ipragliflozin in combination with metformin for the treatment of Japanese patients with type 2 diabetes: ILLUMINATE, a randomized, double-blind, placebo-controlled study. Diabetes Obes Metab. 2015;17(3):304–8. https://doi.org/10.1111/dom.12331.
Ito Y, Van Schyndle J, Nishimura T, Sugitani T, Kimura T. Drug utilization patterns in patients with diabetes initiating sodium glucose co-transporter-2 inhibitors (SGLT2i) in Japan: a multi-database study (2014–2017). Diabetes Ther. 2019;10(6):2233–49. https://doi.org/10.1007/s13300-019-00710-2.
Nakamura I, Maegawa H, Tobe K, Uno S. Real-world evidence for long-term safety and effectiveness of ipragliflozin in Japanese patients with type 2 diabetes mellitus: final results of a 3-year post-marketing surveillance study (STELLA-LONG TERM). Expert Opin Pharmacother. 2021;22(3)373–387. https://www.tandfonline.com/doi/full/10.1080/14656566.2020.1817388.
Maegawa H, Tobe K, Tabuchi H, Nakamura I. Baseline characteristics and interim (3-month) efficacy and safety data from STELLA-LONG TERM, a long-term post-marketing surveillance study of ipragliflozin in Japanese patients with type 2 diabetes in real-world clinical practice. Expert Opin Pharmacother. 2016;17(15):1985–94. https://doi.org/10.1080/14656566.2016.1217994.
Austin RP. Polypharmacy as a risk factor in the treatment of type 2 diabetes. Diabetes Spectr. 2006;19:13–6. https://doi.org/10.2337/diaspect.19.1.13.
Valenza PL, McGinley TC, Feldman J, Pate P, Cornejo K, Liang N, Anmolsingh R, McNaughton N. Dangers of polypharmacy. In: Firstenburg MS, editor. Vignettes in patient safety. InTech Open; 2017. p. 47–70.
Billings LK, Parkin CG, Price D. Baseline glycated hemoglobin values predict the magnitude of glycemic improvement in patients with type 1 and type 2 diabetes: subgroup analyses from the DIAMOND study program. Diabetes Technol Ther. 2018;20(8):561–5. https://doi.org/10.1089/dia.2018.0163.
Gentilella R, Romera I, Nicolay C, Buzzetti R, Vazquez LA, Sesti G. Change in HbA1c across the baseline HbA1c range in type 2 diabetes patients receiving once-weekly dulaglutide versus other incretin agents. Diabetes Ther. 2019;10(3):1113–25. https://doi.org/10.1007/s13300-019-0625-3.
Miura H, Sakaguchi K, Okada Y, Yamada T, Otowa-Suematsu N, So A, Komada H, Hirota Y, Ohara T, Kuroki Y, Hara K, Matsuda T, Kishi M, Takeda A, Yokota K, Tamori Y, Ogawa W. Effects of ipragliflozin on glycemic control, appetite and its related hormones: a prospective, multicenter, open-label study (SOAR-KOBE Study). J Diabetes Investig. 2019;10(5):1254–61. https://doi.org/10.1111/jdi.13015.
Takahara M, Shiraiwa T, Matsuoka TA, Katakami N, Shimomura I. Ameliorated pancreatic beta cell dysfunction in type 2 diabetic patients treated with a sodium-glucose cotransporter 2 inhibitor ipragliflozin. Endocr J. 2015;62(1):77–86. https://doi.org/10.1507/endocrj.EJ14-0335.
Kitada M, Hirai T, Koya D. Significance of SGLT2 inhibitors: lessons from renal clinical outcomes in patients with type 2 diabetes and basic researches. Diabetol Int. 2020;11(3):245–51. https://doi.org/10.1007/s13340-020-00444-8.
Fioretto P, Zambon A, Rossato M, Busetto L, Vettor R. SGLT2 inhibitors and the diabetic kidney. Diabetes Care. 2016;39(Supplement 2):S165–71. https://doi.org/10.2337/dcS15-3006.
Tobe K, Maegawa H, Nakamura I, Uno S. Safety and effectiveness of ipragliflozin in Japanese patients with type 2 diabetes mellitus and impaired renal function: subgroup analysis of a 3-year post-marketing surveillance study (STELLA-LONG TERM). Diabetol Int. 2021;12:181–196. https://doi.org/10.1007/s13340-020-00470-6.
Osonoi T, Nakamoto S, Saito M, Tamasawa A, Ishida H, Osonoi Y. Efficacy of ipragliflozin as monotherapy or as add-on therapy with other oral antidiabetic medications for treating type 2 diabetes in Japanese patients with inadequate glycemic control: a subgroup analysis based on patient characteristics. J Diabetes Investig. 2018;9(2):341–53. https://doi.org/10.1111/jdi.12705.
Lo KB, Gul F, Ram P, Kluger AY, Tecson KM, McCullough PA, Rangaswami J. The effects of SGLT2 inhibitors on cardiovascular and renal outcomes in diabetic patients: a systematic review and meta-analysis. Cardiorenal Med. 2020;10(1):1–10. https://doi.org/10.1159/000503919.
Acknowledgements
The authors thank all the participants in this study. Medical writing support was provided by Catherine Rees and Sarah Greig, PhD, of inScience Communications, Springer Healthcare; this medical writing support was funded by Astellas Pharma Inc.
Funding
This study was funded by Astellas Pharma Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
HM received lecture fees from MSD K.K., Nippon Boehringer Ingelheim Co. Ltd., Mitsubishi Tanabe Pharma Corporation, Sanofi K.K., Astellas Pharma Inc., Takeda Pharmaceutical Co. Ltd., Kowa Pharmaceutical Co. Ltd., Daiichi Sankyo Co. Ltd., Novo Nordisk Pharma Ltd., Eli Lilly Japan K.K. and Kissei Pharmaceutical Co. Ltd.; research support from Astellas Pharma Inc., Astra Zeneca K.K., Nippon Boehringer Ingelheim Co. Ltd., Sunstar Inc., Mitsubishi Tanabe Pharma Corporation, Kyowa Hakko Kirin Co. Ltd., Nissan Chemical Corporation and MIKI Corporation; grants from Takeda Pharmaceutical Co. Ltd., Astellas Pharma Inc., MSD K.K., Nippon Boehringer Ingelheim Co. Ltd., Kyowa Hakko Kirin Co. Ltd., Taisho Pharma Co. Ltd., Kowa Pharmaceutical Co. Ltd., Ono Pharmaceutical Co. Ltd., Daiichi Sankyo Co. Ltd., Sanofi K.K., Mitsubishi Tanabe Pharma Corporation, Sanwa Kagaku Kenkyusho Co. Ltd., Eli Lilly Japan K.K., Sumitomo Dainippon Pharma Co. Ltd., Novo Nordisk Pharma Ltd., Bayer Yakuhin Ltd., Teijin Pharma Limited, Shionogi & Co. Ltd., Fuji Yakuhin Co. Ltd., Pfizer Inc., MIKI Corporation, Mochida Pharmaceutical Co. Ltd., Novartis Pharma K.K. and Nipro Corporation. KT received lecture fees from MSD K.K., Novo Nordisk Pharma Ltd., Kowa Pharmaceutical Co. Ltd.; grants from Daiichi Sankyo Co. Ltd., Ono Pharmaceutical Co. Ltd., Takeda Pharmaceutical Co. Ltd., Nippon Boehringer Ingelheim Co. Ltd., MSD K.K., Mitsubishi Tanabe Pharma Corporation, Teijin Pharma Limited, Eli Lilly Japan K.K., Asahi Kasei Pharma Corporation, The Mitsubishi Foundation and Suntory Global Innovation Center Ltd. IN and SU are employees of Astellas Pharma Inc.
Human rights statement and informed consent
This study was conducted in compliance with Japanese Good Post-marketing Study Practice (GPSP) regulations. Under these regulations, informed consent was not necessary because the study involved anonymized data collected from clinical settings.
Data sharing statement
Researchers may request access to anonymized participant level data, trial level data and protocols from Astellas sponsored clinical trials at http://www.clinicalstudydatarequest.com. For the Astellas criteria on data sharing see: https://clinicalstudydatarequest.com/Study-Sponsors/Study-Sponsors-Astellas.aspx.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Maegawa, H., Tobe, K., Nakamura, I. et al. Real-world evidence for long-term safety and effectiveness of ipragliflozin in treatment-naïve versus non-naïve Japanese patients with type 2 diabetes mellitus: subgroup analysis of a 3-year post-marketing surveillance study (STELLA-LONG TERM). Diabetol Int 12, 430–444 (2021). https://doi.org/10.1007/s13340-021-00501-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-021-00501-w