Abstract
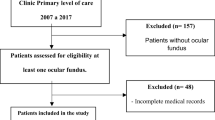
The aim of this study was to clarify the incidences of and the risk factors for severe retinopathy requiring photocoagulation therapy and albuminuria in Japanese patients with childhood-onset type 1 diabetes mellitus. A total of 756 patients from a cohort study by the Japanese Study Group of Insulin Therapy for Childhood and Adolescent Diabetes were included in the study. Patients were registered in 1995 or 2000, and HbA1cwas measured every 4 months and analyzed in central hospital for an average of 6 years. The presence of severe retinopathy requiring laser photocoagulation and the presence of albuminuria was checked for during the period 2010–2011. During a median of 18 (range: 15–21) years, 34 out of 756 patients underwent laser photocoagulation and 57 out of 605 patients developed albuminuria. A Cox proportional hazards model showed that the risk of severe retinopathy requiring laser photocoagulation increased by 1.15 (95% confidence interval [CI] 1.03–1.29, p = 0.012) with each increase of a year in the age at onset, by 4.03 (95% CI 1.20–13.5, p = 0.024) in females, and by 2.05 (95% CI 1.69–2.49, p < 0.0001) with each increase of 1% in HbA1c. The risk of albuminuria increased significantly, by 1.09 (95% CI 1.01–1.18 p = 0.037), with each increase of a year in the age at onset and by 2.38 (95% CI 1.93–2.97 p < 0.0001) with each increase of 1% in HbA1c. In Japanese patients with childhood-onset type 1 diabetes, older age at the onset of diabetes, female rather than male gender, and higher HbA1c were found to increase the risk of requiring photocoagulation. No patients with HbA1c < 7.5% developed severe retinopathy requiring photocoagulation therapy. The risk of developing albuminuria increased with age at onset of diabetes and HbA1c. Female gender was a strong risk factor for severe retinopathy requiring photocoagulation, but not for albuminuria.


Similar content being viewed by others
References
Coffey JT, Brandle M, Zhou H, Marriott D, Burke R, Tabaei BP, et al. Valuing health-related quality of life in diabetes. Diabetes Care. 2002;25:2238–43.
Nordwall M, Bojestig M, Arnqvist HJ, Ludvigsson J. Declining incidence of severe retinopathy and persisting decrease of nephropathy in an unselected population of type 1 diabetes: the Linkoping Diabetes Complications Study. Diabetologia. 2004;47:1266–72.
Hovind P, Tarnow L, Rossing K, Rossing P, Eising S, Larsen N, et al. Decreasing incidence of severe diabetic microangiopathy in type 1 diabetes. Diabetes Care. 2003;26:1258–64.
Reichard P, Nilsson BY, Rosenqvist U. The effect of long-term intensified insulin treatment on the development of microvascular complications of diabetes mellitus. N Engl J Med. 1993;329:304–9.
The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–86.
The DIAMOND Project Group. Incidence and trends of childhood type 1 diabetes worldwide 1990–1999. Diabet Med. 2006;23:857–66.
Diabetes Epidemiology Research International Mortality Study Group. Major cross-country differences in risk of dying for people with IDDM. Diabetes Care. 1991;14:49–54.
Matsuura N, Yokota Y, Kazahari K, et al. The Japanese Study Group of Insulin Therapy for Childhood and Adolescent Diabetes (JSGIT): initial aims and impact of the family history of type 1 diabetes mellitus in Japanese children. Pediatr Diabetes. 2001;2:160–9.
World Health Organization. Diabetes mellitus: report of a WHO study group. Technical report, series 727. Geneva: WHO; 1985.
Shima K, Endo J, Oimomi M, Omori Y, Katayama Y, Kanazawa Y, et al. Interlaboratory difference in GHb measurement in Japan: the fifth report of the GHb Standardization Committee, the Japan Diabetes Society (in Japanese). J Jpn Diabetes Soc. 1998;41:317–23.
Kashiwagi A, Kasuga M, Araki E, Oka Y, Hanafusa T, Ito H, et al. Committee on the Standardization of Diabetes Mellitus-Related Laboratory Testing of Japan Diabetes Society: international clinical harmonization of glycated hemoglobin in Japan: from Japan Diabetes Society to National Glycohemoglobin Standardization Program values. Diabetol Int. 2012;3:8–10.
Mortensen HB, Robertson KJ, Aanstoot HJ, Danne T, Holl RW, Hougaard P, et al. Insulin management and metabolic control of type 1 diabetes mellitus in childhood and adolescence in 18 countries. Diabetes Med. 1998;15:752–9.
Holl RW, Lang GE, Grabert M, Heinze E, Lang GK, Debatin KM, et al. Diabetic retinopathy in pediatric patients with type 1 diabetes: effect of diabetes duration, prepubertal and pubertal onset of diabetes, and metabolic control. J Pediatr. 1998;132:790–4.
Yokoyama H, Uchigata Y, Otani T, Saeki A, Aoki K, Kasahara T, Omori Y. Metabolic regulation and microangiopathy in a cohort of Japanese IDDM patients. Diabetes Res Clin Pract. 1995;29:203–9.
Yokoyama H, Uchigata Y, Otani T, Aoki K, Maruyama A, Maruyama H, et al. Development of proliferative retinopathy in Japanese patients with IDDM: Tokyo Women’s Medical College Epidemiologic Study. Diabetes Res Clin Pract. 1994;24:113–9.
Cawood EH, Bancroft J, Steel JM. Perimenstrual symptoms in women with diabetes mellitus and the relationship to diabetic control. Diabet Med. 1993;10:444–8.
Broe R, Rasmussen ML, Frydkjaer-Olsen U, Olsen BS, Mortensen HB, Peto T, et al. The 16-year incidence, progression and regression of diabetic retinopathy in young population-based Danish cohort with type 1 diabetes mellitus: the Danish Cohort of Pediatric Diabetes 1987 (DCPD1987). Acta Diabetol. 2014;51:413–20.
Schultz CJ, Konopelska-Bahu T, Dalton RN, Carrokk TA, Stratton I, Gale EA, et al. Microalbuminuria prevalence varies with age, sex, and puberty in children with type 1 diabetes followed from diagnosis in a longitudinal study: Oxford Regional Prospective Study Group. Diabetes Care. 1999;22:495–502.
Hovind P, Tarnow L, Rossing P, Jensen BR, Graue M, Torp I, et al. Predictors for the development of microalbuminuria and macroalbuminuria in patients with type 1 diabetes. BMJ. 2004;328:1105–10.
Sano H, Nishimura R, Asao K, Matsudaira T, Morimoto A, Agata T, et al. Blindness and laser photocoagulation in patients with childhood-onset type 1 diabetes in Japan. Br J Ophthalmol. 2009;93:726–30.
Kostraba JN, Dorman JS, Orchard TJ, Becker DJ, Ohki Y, Ellis D, et al. Contribution of diabetes duration before puberty to development of microvascular complications in IDDM subjects. Diabetes Care. 1989;12:686–93.
Acerini CL, Williams RM, Dunger DB. Metabolic impact of puberty on the course of type 1 diabetes. Diabetes Metab. 2001;27:S19–25.
Morimoto A, Nishimura R, Matsudaira T, Sano H, Tajima N. Diabetes Epidemiology Research International Study Group. Is pubertal onset a risk factor for blindness and renal replacement therapy in childhood-onset type 1 diabetes in Japan? Diabetes Care. 2007;30:2338–40.
Cameron FJ, Amin R, de Beaufort C, Codner R, Acerini CL. ISPAD clinical practice consensus guidelines 2014: diabetes in adolescence. Pediatric Diabetes. 2014;15(20):245–56.
Bryden KS, Peveler RC, Stein A, Neil A, Mayou RA, Dunger DB. Clinical and psychological course of diabetes from adolescence to young adulthood: a longitudinal cohort study. Diabetes Care. 2001;24:1536–40.
Wysocki T, Hough BS, Ward KM, Green LB. Diabetes mellitus in the transition to adulthood: adjustment, self-care, and health status. J Dev Behav Pediatr. 1992;13:194–201.
Amiel SA, Sherwin RS, Simonson DC, Lauritano AA, Tamborlane WV. Impaired insulin action in puberty. A contributing factor to poor glycemic control in adolescents with diabetes. N Engl J Med. 1986;315:215–9.
Hirose A, Furushima D, Yamaguchi N, Kitano S, Uchigata Y. Prediction of retinopathy at 20 years after onset in younger-onset type 1 diabetes using mean metabolic memory-free HbA1c values. Diabetes Care. 2013;36:3812–4.
Acknowledgements
This study was supported by a grant-in-aid from the Japan Diabetes Foundation. We would like to thank the following doctors who were members of the Japanese Study Group of Insulin Therapy for Childhood and Adolescent Diabetes (JSGIT): Masanori Adachi, M.D., and Katsuhiko Tachibana, M.D., Kanagawa Children’s Medical Center; Taiji Aso, M.D., and Rika Kizu, M.D., Department of Pediatrics, Yokosuka Kyousai Hospital; Masatoshi Fujimoto, M.D., Department of Pediatrics, St. Marianna University; Satoshi Fujitsuka, M.D., Akira Motegi, M.D., and Yoichi Morinishi, M.D., Department of Pediatrics, National Defence Medical Collage; Ikuma Fujiwara, M.D., and Eishin Ogawa, M.D., Department of Pediatrics, Tohoku University Hospital; Naoki Fukushima, M.D., Department of Pediatrics, Sapporo City General Hospital; Keiichi Hanaki, M.D., and Susumu Kanzaki, M.D., Department of Pediatrics, Tottori University; Yukihiro Hasegawa, M.D., Tokyo Kiyose Metropolitan Children’s Hospital; Takeki Hirano, M.D., Ibaragi Children’s Hospital; Reiko Horikawa, M.D., National Center for Child Health and Development; Tomoyuki Hotsubo, M.D., Department of Pediatrics, Tonan Hospital; Yutaka Igarashi, M.D., Igarashi Children’s Clinic; Masaru Inoue, M.D., and Susumu Kanzaki, M.D., Department of Pediatrics, Tokai University; Gen Isshiki, M.D., and Tomomi Hashimoto, M.D., Department of Pediatrics, Osaka City University Graduate School of Medicine; Yoshiya Ito, M.D., and Tokuo Mukai, M.D., Department of Pediatrics, Asahikawa Medical University; Kazuhiko Jinno, M.D., Department of Pediatrics, Hiroshima General Hospital of West Japan Railway Company; Sachiko Kanematsu, M.D., and Kaori Sasaki, M.D., Department of Pediatrics, Tokyo Women’s Medical University; Yoshihito Kasahara, M.D., Department of Pediatrics, Kanazawa University; Kaichi Kida, M.D., and Koji Takemoto, M.D., Department of Pediatrics, Ehime University Graduate School of Medicine; Nobuyuki Kikuchi, M.D., and Kentaro Shiga, M.D., Department of Pediatrics, Yokohama City University Medical Center; Hitoshi Kohno, M.D., and Saori Kinjo, M.D., Fukuoka Children’s Hospital; Masanori Minagawa, M.D., and Kaori Kinoshita, M.D., Department of Pediatrics, Chiba University; Akihiko Kinugasa, M.D., Department of Pediatrics, Kyoto Prefectural University of Medicine; Yukashi Ohki, M.D., and Megumi Kishi, M.D., Department of Pediatrics, Nippon Medical School; Koji Kobayashi, M.D., and Mie Mochizuki, M.D., Department of Pediatrics, Yamanashi University; Akemi Koike, M.D., Koike Children’s Clinic; Susumu Konda, M.D., Konda Children’s Clinic; Kazutaka Konishi, M.D., Abuyama Children’s Clinic; Ichiro Yokota, M.D., and Yumiko Kotani, M.D., Department of Pediatrics, Tokushima Univeisity Graduate School of Medicine; Kazumichi Onigata, M.D., Takanori Kowase, M.D., and Fumitake Mizoguchi, M.D., Department of Pediatrics, Gunma University; Hidenari Masuda, M.D., Department of Pediatrics, National Mie Hospital; Hisafumi Matsuoka, M.D., Department of Pediatrics, Tokyo Women’s Medical University Medical Center East; Yuko Miki, M.D., and Utako Sato, M.D., Department of Pediatrics, Tokyo University; Shigeki Miyamoto, M.D., and Rieko Takatani, M.D., Chiba Children’s Hospital; Tetsuo Mori, M.D., Department of Pediatrics, Nagano National Hospital; Yoshikazu Nishi, M.D., Department of Pediatrics, Hiroshima Red Cross Hospital; Osamu Nukada, M.D., Department of Pediatrics, Kobe City West Municipal Hospital; Haruo Ogawa, M.D., Kaoru Nasuda, M.D., and Kazuhiko Toya, M.D., Department of Pediatrics, Hamamatsu University School of Medicine; Taisuke Okada, M.D., Department of Pediatrics, Mominoki Hospital; Soroku Nishiyama, M.D., and Toshihisa Okada, M.D., Department of Pediatrics, Kumamoto University; Toshikazu Takahashi, M.D., Takahashi Clinic; Masakuni Tokuda, M.D., and Ryuzo Takaya, M.D., Department of Pediatrics, Osaka Medical College; Masaro Takesue, M.D., Department of Pediatrics, Japan Red Cross Musashino Hospital; Tokuo Taketani, M.D., Department of Pediatrics, Kurobe City Hospital; Yukifumi Yokota, M.D., and Noriyuki Takubo, M.D., Department of Pediatrics, Kitasato University; Masakuni Tokuda, M.D., Tokuda Children’s Clinic; Makoto Uchiyama, M.D., Department of Pediatrics, Niigata University.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Tatsuhiko Urakami has served in advisory panels for Novo Nordisk and Sanofi, and has served on speakers’ bureaus for Sanofi.
Human rights statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. Informed consent or a substitute for it was obtained from all patients before they were included in the study.
About this article
Cite this article
Takaike, H., Uchigata, Y., Matsuura, N. et al. The incidences of and risk factors for severe retinopathy requiring photocoagulation and albuminuria in Japanese patients with childhood-onset type 1 diabetes. Diabetol Int 9, 121–128 (2018). https://doi.org/10.1007/s13340-017-0336-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-017-0336-9