Abstract
Background and Objective
Platelets play a pivotal role in thrombotic events associated with acute coronary syndrome (ACS), making oral antiplatelet therapy a cornerstone in antithrombotic strategies. The dosing regimen for the oral antiplatelet drug ticagrelor warrants evaluation to ensure its appropriateness in clinical practice. Therefore, this study aimed to investigate the real-world clinical application of ticagrelor by determining the optimal therapeutic concentration of ticagrelor in Chinese patients undergoing percutaneous coronary intervention (PCI).
Methods
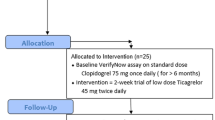
We enrolled a cohort of 912 patients who underwent PCI with drug-eluting stent implantation for the treatment of ACS. We measured steady-state plasma drug concentrations using high-performance liquid chromatography–tandem mass spectrometry. The therapeutic drug concentration range at steady state was established on the basis of clinical pharmacodynamic indices, with verification of reliability through concentration-effect analysis and receiver operating characteristic curve assessment.
Results
Analysis of plasma samples from the 912 patients revealed significant variations in the steady-state trough concentration of ticagrelor associated with factors such as gender, age, hypertension, and hyperlipidemia. On the basis of this analysis, the optimal therapeutic range for steady-state trough concentration was determined to be 240.65–335.83 ng/mL. Furthermore, the upper limit values for steady-state concentration were established at 439.97 ng/mL for male patients and 347.06 ng/mL for female patients.
Conclusions
This study provides robust and reliable insights into the optimal therapeutic steady-state trough concentrations of ticagrelor in Chinese patients with post-percutaneous coronary intervention. These findings have significant implications for guiding the rational use of antiplatelet drugs and facilitating precise drug administration in Chinese patients undergoing percutaneous coronary intervention.




Similar content being viewed by others
References
Husted S, Emanuelsson H, Heptinstall S, Sandset PM, Wickens M, Peters G. Pharmacodynamics, pharmacokinetics, and safety of the oral reversible P2Y12 antagonist AZD6140 with aspirin in patients with atherosclerosis: a double-blind comparison to clopidogrel with aspirin. Eur Heart J. 2006;27(9):1038–47. https://doi.org/10.1093/eurheartj/ehi754.
Husted S, Giezen V. Ticagrelor: the first reversibly binding oral P2Y12 receptor antagonist. Cardiovasc Ther. 2009;27(4):259–74. https://doi.org/10.1111/j.1755-5922.2009-00096.x.
Dhillon S. Ticagrelor: a review of its use in adults with acute coronary syndromes. Am J Cardiovasc Drugs. 2015;15(1):51–68. https://doi.org/10.1007/s40256-015-0108-5.
Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045–57. https://doi.org/10.1056/NEJMoa0904327.
Teng DR. Pharmacokinetic, pharmacodynamic and pharmacogenetic profile of the oral antiplatelet agent ticagrelor. Clin Pharmacokinet. 2012;51(5):305–18. https://doi.org/10.2165/11630960-000000000-00000.
Kelemen H, Hancu G, Papp LA. Analytical methodologies for the determination of ticagrelor. Biomed Chromatogr. 2019;33: e4528. https://doi.org/10.1002/bmc.4528.
Li H, Butler K, Yang L, Yang Z, Teng R. Pharmacokinetics and tolerability of single and multiple doses of ticagrelor in healthy Chinese subjects: an open-label, sequential, two-cohort, single-centre study. Clin Drug Investig. 2012;32(2):87–97. https://doi.org/10.2165/11595930-000000000-00000.
Li JG, Tang WF, Storey RF, Husted S, Teng R. Population pharmaacokinetics of ticagrelor in patients with acute coronary syndromes. Int J Clin Pharmacol Ther. 2016;54(9):666–74. https://doi.org/10.5414/CP202549.
Jeong Y. “East Asian paradox”: challenge for the current antiplatelet strategy of “one-guideline-fits-all races” in acute coronary syndrome. Curr Cardiol Rep. 2014;16(5):485. https://doi.org/10.1007/s-11886-014-0485-4.
Levine G, Jeong Y, Goto S, Anderson J, Huo Y, Mega J, Taubert K, Smith S. Expert consensus document: World Heart Federation expert consensus statement on antiplatelet therapy in East Asian patients with ACS or undergoing PCI. Nat Rev Cardiol. 2014;11(10):597–606. https://doi.org/10.1038/nrcardio.2014.104.
Shi J, He M, Wang W, Liu J, Zhang H, Sun D, Li J, Mu H, Xu M, Zhao C, Wang J, Zhang C, Cang H, Zhao S, Zhang Z, Li Y. Efficacy and safety of different ticagrelor regimens versus clopidogrel in patients with coronary artery disease: a retrospective multicenter study (SUPERIOR). Platelets. 2021;32(1):120–9. https://doi.org/10.1080/09537104.2020.1732328.
Krakowiak A, Kuleta J, Plech I, Zarebinski M, Wojciechowska M, Wretowski D, Cudnoch-Jedrzejewska A. Ticagrelor-related severe dyspnoea: mechanisms, characteristic features, differential diagnosis and treatment. Clin Med Insights Case Rep. 2020;13:117954762095663. https://doi.org/10.1177/1179547620956634.
Han Y. Chinese expert consensus statement on dual antiplatelet therapy in patients with coronary artery disease. Eur Heart J. 2021;13:1283–5. https://doi.org/10.1093/eurheartj/ehab741.
Husted SE, Storey RF, Bliden K. Pharmacokinetics and pharmacodynamics of ticagrelor in patients with stable coronary artery disease. Clin Pharmacokinet. 2012;51(6):397–409.
Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, Kaul S, Wiviott SD, Menon V, Nikolsky E, Serebruany V, Valgimigli M, Vranckx P, Taggart D, Sabik JF, Cutlip DE, Krucoff MW, Ohman M, Steg PG, White H. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011;123(23):2736–47. https://doi.org/10.1161/CIRCULATIO-NAHA.110.009449.
Cardiovascular Laboratory Medicine Professional Committee of Laboratory Physicians Branch of Chinese Medical Doctor Association. Expert consensus on the application of platelet function detection in antiplatelet therapy in patients with acute coronary syndrome. Natl Med J China. 2018;6(22):98.
Hiasa Y, Teng R, Emanuelsson H. Pharmacodynamics, pharmacokinetics and safety of ticagrelor in Asian patients with stable coronary artery disease. Cardiovasc Interv Ther. 2014;29(4):324–33. https://doi.org/10.1007/s12928-014-0277-1.
Wang HX. The effective concentration range of lamotrigine in epilepsy patients. Chin J Clin Pharmacol. 2019;35(1):4.
Danielak D, Karaźniewicz-Łada M, Główka F. Ticagrelor in modern cardiology an up-to-date review of most important aspects of ticagrelor pharmacotherapy. Expert Opin Pharmacother. 2017. https://doi.org/10.1080/14656566-2017.1421634.
Butler K, Teng R. Pharmacokinetics, pharmacodynamics, and safety of ticagrelor in volunteers with severe renal impairment. J Clin Pharmacol. 2013;52(9):75–8. https://doi.org/10.1177/0091270011415526.
Arora S, Shemisa K, Vaduganathan M, Qamar A, Gupta A, Garg SK, Kumbhani DJ, Mayo H, Khalili H, Pandey A, Das SR. Premature ticagrelor discontinuation in secondary prevention of atherosclerotic CVD: JACC review topic of the week. J Am Coll Cardiol. 2019;73(19):2454–64. https://doi.org/10.1016/j.jacc.2019.03.470.
Feit F, Voeltz MD, Attubato MJ, Lincoff AM, Chew DP, Bittl JA, Topol EJ, Manoukian SV. Predictors and impact of major hemorrhage on mortality following percutaneous coronary intervention from the REPLACE-2Trial. Am J Cardiol. 2007;100(9):1364–9. https://doi.org/10.1016/j.amjcard.2007.06.026.
Teng R, Butler K. Effect of the CYP3A inhibitors, diltiazem and ketoconazole, on ticagrelor pharmacokinetics in healthy volunteers. J Drug Assess. 2013;2(1):30–9. https://doi.org/10.3109/2155-6660.2013.785413.
Acknowledgments
The authors extend their gratitude to the study participants. They also acknowledge the contributions of all members of the Anhui Provincial Key Laboratory for Enhancing and Evaluating the Quality of Chinese Medicine, whose suggestions and discussions were instrumental in preparing this manuscript. Additionally, they thank Editage (www.editage.cn) for their assistance with English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Anhui Scientific Research and Innovation Team of Quality Evaluation and Improvement of Traditional Chinese Medicine (2022AH010090).
Conflict of Interest
The author(s) declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics Approval
Ethics Committee of Nanjing First Hospital approved the study protocol (approval number KY2019530-05). The study was conducted in accordance with the International Conference on Harmonisation Guideline for Good Clinical Practice and the Declaration of Helsinki.
Consent to participate
All subjects provided written informed consent before participation
Consent for publication
Not applicable.
Availability of Data and Material
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Code Availability
Not applicable.
Authors Contributions
SZ was responsible for conception and design, data collection, interpretation of the data, drafting of the article, final approval of the manuscript, and statistical analysis; QJ and NC for interpretation of the data and data collection; and YZ and XC for conception and design, final approval of the manuscript, and supervision. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zheng, S., Jie, Q., Chen, N. et al. Ticagrelor Steady-State Trough Concentration in Chinese Patients Undergoing Percutaneous Coronary Intervention. Eur J Drug Metab Pharmacokinet 49, 33–42 (2024). https://doi.org/10.1007/s13318-023-00867-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-023-00867-z