Abstract
Background and Objective
The number of adults living with cystic fibrosis (CF) has increased and will continue to do so with the approval of cystic fibrosis transmembrane conductance regulator (CFTR) modulators. Because systemic aminoglycosides are commonly administered for CF pulmonary exacerbations, we sought to define optimized dosing regimens using a population pharmacokinetic modeling and simulation approach.
Methods
Adult CF patients admitted for pulmonary exacerbation, receiving at least 72 h of systemic gentamicin, tobramycin, or amikacin, with measured concentrations were included. Covariates [e.g., age, weight, creatinine clearance (CRCL)] were screened. Population modeling was completed using Monolix, and simulations were conducted in R. Simulated exposures were calculated using noncompartmental analysis. Once-daily fixed (10 mg/kg) and exposure-matched dosing (i.e., 15, 10, 7.5, 6 mg/kg for ages 20, 30, 40, and 50 years, respectively) strategies were compared. First-24 h exposures were evaluated for each strategy according to the probability of target attainment (PTA) (ratio of peak plasma concentrations relative to the minimum inhibitory concentration [Cmax/MIC] or ratio of the area under the concentration-time curve to MIC [AUC/MIC]) and the probability of toxic exposure (PTE) (trough concentration, Ctrough > 2 mg/l).
Results
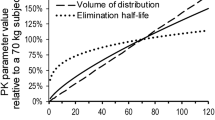
Forty-eight adult patients (55% female) were included. A one-compartment model best fit the data. Estimates for volume of distribution (V) and clearance (CL) were 22 l and 5.57 l/h, respectively. Weight significantly modified CL and V. Age significantly modified CL and was more influential than CRCL. PTA was > 90% at MICs ≤ 1 mg/l for fixed doses of 10 mg/kg and for exposure-matched doses at MIC ≤ 1 mg/l. Exposure-matched dosing reduced PTE roughly 50% in patients aged 40 and 50 years vs. fixed dosing.
Conclusions
Exposure-matching maintained PTA at MICs ≤ 1 mg/l while reducing toxicity risk in older patients compared to fixed dosing. Confirmatory studies are needed.


Similar content being viewed by others
References
Lubamba B, Dhooghe B, Noel S, Leal T. Cystic fibrosis: insight into CFTR pathophysiology and pharmacotherapy. Clin Biochem. 2012;45(15):1132–44.
Flume PA, Suthoff ED, Kosinski M, Marigowda G, Quittner AL. Measuring recovery in health-related quality of life during and after pulmonary exacerbations in patients with cystic fibrosis. J Cyst Fibros. 2019;18(5):737–42.
Cystic Fibrosis Foundation. Cystic Fibrosis Foundation Patient Registry 2019 Annual Data Report. Bethesda, Maryland: Cystic Fibrosis Foundation; 2020. https://www.cff.org/sites/default/files/2021-10/2019-Patient-Registry-Annual-Data-Report.pdf.
Espel JC, Palac HL, Cullina JF, Clarke AP, McColley SA, Prickett MH, et al. Antibiotic duration and changes in FEV(1) are not associated with time until next exacerbation in adult cystic fibrosis: a single center study. BMC Pulm Med. 2017;17(1):160.
Kapnadak SG, Dimango E, Hadjiliadis D, Hempstead SE, Tallarico E, Pilewski JM, et al. Cystic Fibrosis Foundation consensus guidelines for the care of individuals with advanced cystic fibrosis lung disease. J Cyst Fibros. 2020;19(3):344–54.
O’Donnell EP, Scarsi KK, Scheetz MH, Postelnick MJ, Cullina J, Jain M. Risk factors for aminoglycoside ototoxicity in adult cystic fibrosis patients. Int J Antimicrob Agents. 2010;36(1):94–5.
Bhatt JM. Treatment of pulmonary exacerbations in cystic fibrosis. Eur Respir Rev. 2013;22(129):205–16.
Flume PA, Mogayzel PJ Jr, Robinson KA, Goss CH, Rosenblatt RL, Kuhn RJ, et al. Cystic fibrosis pulmonary guidelines: treatment of pulmonary exacerbations. Am J Respir Crit Care Med. 2009;180(9):802–8.
Burkhardt O, Lehmann C, Madabushi R, Kumar V, Derendorf H, Welte T. Once-daily tobramycin in cystic fibrosis: better for clinical outcome than thrice-daily tobramycin but more resistance development? J Antimicrob Chemother. 2006;58(4):822–9.
Barras MA, Serisier D, Hennig S, Jess K, Norris RL. Bayesian estimation of tobramycin exposure in patients with cystic fibrosis. Antimicrob Agents Chemother. 2016;60(11):6698–702.
Moore RD, Lietman PS, Smith CR. Clinical response to aminoglycoside therapy: importance of the ratio of peak concentration to minimal inhibitory concentration. J Infect Dis. 1987;155(1):93–9.
Whitehead A, Conway SP, Etherington C, Caldwell NA, Setchfield N, Bogle S. Once-daily tobramycin in the treatment of adult patients with cystic fibrosis. Eur Respir J. 2002;19(2):303–9.
Wood PJ, Ioannides-Demos LL, Li SC, Williams TJ, Hickey B, Spicer WJ, et al. Minimisation of aminoglycoside toxicity in patients with cystic fibrosis. Thorax. 1996;51(4):369–73.
Hoff BM, Scheetz MH, Jain M, Cullina JF, Rhodes NJ. Exploring the relationship between FEV1 loss and recovery and aminoglycoside pharmacokinetics in adult patients with cystic fibrosis: implications for clinical dosing strategies. Pharmacotherapy. 2020;40(6):584–91.
Quon BS, Mayer-Hamblett N, Aitken ML, Smyth AR, Goss CH. Risk factors for chronic kidney disease in adults with cystic fibrosis. Am J Respir Crit Care Med. 2011;184(10):1147–52.
Mulherin D, Fahy J, Grant W, Keogan M, Kavanagh B, FitzGerald M. Aminoglycoside induced ototoxicity in patients with cystic fibrosis. Ir J Med Sci. 1991;160(6):173–5.
Caceres Guido P, Perez M, Halac A, Ferrari M, Ibarra M, Licciardone N, et al. Population pharmacokinetics of amikacin in patients with pediatric cystic fibrosis. Pediatr Pulmonol. 2019;54(11):1801–10.
Illamola SM, Huynh HQ, Liu X, Bhakta ZN, Sherwin CM, Liou TG, et al. Population pharmacokinetics of amikacin in adult patients with cystic fibrosis. Antimicrob Agents Chemother. 2018. https://doi.org/10.1128/AAC.00877-18.
Campbell D, Thomson AH, Stack B. Population pharmacokinetics of aminoglycoside antibiotics in patients with cystic fibrosis. Ther Drug Monit. 1999;21(3):281–8.
Sherwin CM, Zobell JT, Stockmann C, McCrory BE, Wisdom M, Young DC, et al. Pharmacokinetic and pharmacodynamic optimisation of intravenous tobramycin dosing among children with cystic fibrosis. J Pharmacokinet Pharmacodyn. 2014;41(1):71–9.
Wang X, Koehne-Voss S, Anumolu SS, Yu J. Population pharmacokinetics of tobramycin inhalation solution in pediatric patients with cystic fibrosis. J Pharm Sci. 2017;106(11):3402–9.
Coulthard KP, Peckham DG, Conway SP, Smith CA, Bell J, Turnidge J. Therapeutic drug monitoring of once daily tobramycin in cystic fibrosis–caution with trough concentrations. J Cyst Fibros. 2007;6(2):125–30.
Cockcroft DW, Gault H. Prediction of Creatinine Clearance from Serum Creatinine. Nephron. 1976;16(1):31–41.
Lixoft. Monolix 2019 User Guide. 2019. https://monolix.lixoft.com/single-page/.
Mould DR, Upton RN. Basic concepts in population modeling, simulation, and model-based drug development. CPT Pharmacomet Syst Pharmacol. 2012;1:6.
Nguyen TH, Mouksassi MS, Holford N, Al-Huniti N, Freedman I, Hooker AC, et al. Model evaluation of continuous data pharmacometric models: metrics and graphics. CPT Pharmacomet Syst Pharmacol. 2017;6(2):87–109.
Duffull SB, Wright DF, Winter HR. Interpreting population pharmacokinetic-pharmacodynamic analyses: a clinical viewpoint. Br J Clin Pharmacol. 2011;71(6):807–14.
Traynard P, Ayral G, Twarogowska M, Chauvin J. Efficient pharmacokinetic modeling workflow with the monolixsuite: a case study of remifentanil. CPT Pharmacomet Syst Pharmacol. 2020;9(4):198–210.
Lavielle M. mlxR: Simulation of Longitudinal Data. R package version 4.1.3.; 2020. https://cran.nexr.com/web/packages/mlxR/mlxR.pdf.
Venables WN, Smith DM, R Core Team. Notes on R: A Programming Environment for Data Analysis and Graphics. 2020. https://cran.r-project.org/doc/manuals/r-release/R-intro.pdf.
Lavielle M, Chauvin J. Rsmlx: R Speaks 'Monolix'. R package version 2.0.2.; 2019. https://cran.r-project.org/web/packages/Rsmlx/Rsmlx.pdf.
Gastonguay MR, El-Tahtawy A. Effect of NONMEM minimization status and number of replicates on bootstrap parameter distributions for population pharmacokinetic models: a case study. Clin Pharmacol Ther. 2005;77(2):2.
Bae K-S, Lee JE. pkr: Pharmacokinetics in R. R package version 0.1.2.; 2018. https://cran.r-project.org/web/packages/pkr/pkr.pdf.
Kirkpatrick CM, Duffull SB, Begg EJ. Pharmacokinetics of gentamicin in 957 patients with varying renal function dosed once daily. Br J Clin Pharmacol. 1999;47(6):637–43.
Drusano GL, Ambrose PG, Bhavnani SM, Bertino JS, Nafziger AN, Louie A. Back to the future: using aminoglycosides again and how to dose them optimally. Clin Infect Dis. 2007;45(6):753–60.
Mouton JW, Jacobs N, Tiddens H, Horrevorts AM. Pharmacodynamics of tobramycin in patients with cystic fibrosis. Diagn Microbiol Infect Dis. 2005;52(2):123–7.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. M100-ED30. Wayne, PA; 2020.
Mogayzel PJ Jr, Naureckas ET, Robinson KA, Mueller G, Hadjiliadis D, Hoag JB, et al. Cystic fibrosis pulmonary guidelines. Chronic medications for maintenance of lung health. Am J Respir Crit Care Med. 2013;187(7):680–9.
Bulitta JB, Duffull SB, Kinzig-Schippers M, Holzgrabe U, Stephan U, Drusano GL, et al. Systematic comparison of the population pharmacokinetics and pharmacodynamics of piperacillin in cystic fibrosis patients and healthy volunteers. Antimicrob Agents Chemother. 2007;51(7):2497–507.
Kidd JM, Sakon CM, Oleksiuk LM, Cies JJ, Pettit RS, Nicolau DP, et al. Pharmacokinetics of telavancin in adult patients with cystic fibrosis during acute pulmonary exacerbation. Antimicrob Agents Chemother. 2019. https://doi.org/10.1128/AAC.01914-19.
Smith AL, Fiel SB, Mayer-Hamblett N, Ramsey B, Burns JL. Susceptibility testing of Pseudomonas aeruginosa isolates and clinical response to parenteral antibiotic administration: lack of association in cystic fibrosis. Chest. 2003;123(5):1495–502.
Somayaji R, Parkins MD, Shah A, Martiniano SL, Tunney MM, Kahle JS, et al. Antimicrobial susceptibility testing (AST) and associated clinical outcomes in individuals with cystic fibrosis: a systematic review. J Cyst Fibros. 2019;18(2):236–43.
Hennig S, Standing JF, Staatz CE, Thomson AH. Population pharmacokinetics of tobramycin in patients with and without cystic fibrosis. Clin Pharmacokinet. 2013;52(4):289–301.
Davies DF, Shock NW. Age changes in glomerular filtration rate, effective renal plasma flow, and tubular excretory capacity in adult males. J Clin Invest. 1950;29(5):496–507.
Friedman SA, Raizner AE, Rosen H, Solomon NA, Sy W. Functional defects in the aging kidney. Ann Intern Med. 1972;76(1):41–5.
Nolt VD, Pijut KD, Autry EB, Williams WC, Burgess DS, Burgess DR, et al. Amikacin target achievement in adult cystic fibrosis patients utilizing Monte Carlo simulation. Pediatr Pulmonol. 2018;54(1):33–9.
Mendelman PM, Smith AL, Levy J, Weber A, Ramsey B, Davis RL. Aminoglycoside penetration, inactivation, and efficacy in cystic fibrosis sputum. Am Rev Respir Dis. 1985;132(4):761–5.
King P, Lomovskaya O, Griffith DC, Burns JL, Dudley MN. In vitro pharmacodynamics of levofloxacin and other aerosolized antibiotics under multiple conditions relevant to chronic pulmonary infection in cystic fibrosis. Antimicrob Agents Chemother. 2010;54(1):143–8.
Acknowledgements
The authors would like to thank Karen Zmuda for her assistance with the description of the assays conducted at Northwestern Medicine.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research. The study was completed as part of our normal work.
Conflicts of Interest
Roxane Rohani, Brian Hoff, Manu Jain, Alexander Philbrick, Sara Salama, Joanne F. Cullina, and Nathaniel J. Rhodes have no conflicts of interest to declare.
Ethics Approval
The study was approved by Institutional Review Boards at Northwestern University (#STU00088207) and Midwestern University (under reliance agreement).
Consent to Participate
A waiver of informed consent was granted by IRB for this retrospective cohort study.
Consent for Publication
Not applicable.
Availability of Data and Material
All data are contained within the manuscript or Supplement. Additional requests may be submitted to the corresponding author, but these are subject to IRB restrictions.
Code Availability (Software Application or Custom Code)
Not applicable
Author contribution
RR and NJR conceived of the work. RR conducted the modeling. PK models were independently confirmed by SS who also provided critical review of the manuscript. BH, MJ, AP, and JFC provided the data and provided critical review of the manuscript. The modeling and simulation work was supervised by NJR. NJR and RR wrote the initial draft of the manuscript and processed all revisions. All authors gave approval of the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rohani, R., Hoff, B., Jain, M. et al. Defining the Importance of Age-Related Changes in Drug Clearance to Optimizing Aminoglycoside Dosing Regimens for Adult Patients with Cystic Fibrosis. Eur J Drug Metab Pharmacokinet 47, 199–209 (2022). https://doi.org/10.1007/s13318-021-00734-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-021-00734-9