Abstract
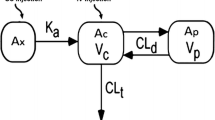
Goto-Kakizaki (GK) rats represent a unique non-obese and lean model with manifestation of type 2 diabetes (T2DM) broadly mimicking the human T2DM development. Therefore, in addition to the use of GK rats to test the efficacy of drugs, it may represent a great tool to study the influence of altered physiological process and/or organ specific pathophysiological changes (i.e., liver, kidney, etc.) on the disposition of drugs. The objectives of the review were: (a) to compile the published pharmacokinetic data of several drugs, such as cephalexin, cyclosporine, exendin-4, gliclazide, grepafloxacin, rosuvastatin, salsalate, salicylic acid, and theophylline, in GK rats relative to normal rats; and (b) critically evaluate the possible role of physiologically altered processes on the pharmacokinetics of reviewed drugs. The drugs chosen for this review provided a spread of various physiological processes and represented reasonable pool of published data set to fulfil the objectives of the review. The use of GK rats for gathering pharmacokinetic data may aid in making decisions on candidate selection and/or anticipating clinical pharmacology-related issues to the aid drug development in the diabetes area. However, given the interplay and complexities of multiple pathways governing drug disposition, caution needs to be exercised in data interpretation.
Similar content being viewed by others
References
Blair M. Diabetes mellitus review. Urol Nurs. 2016;36:27–36.
George AM, Jacob AG, Fogelfeld L. Lean diabetes mellitus: an emerging entity in the era of obesity. World J Diabetes. 2015;6:613–20.
Zaccardi F, Webb DR, Yates T, Davies MJ. Pathophysiology of type 1 and type 2 diabetes mellitus: a 90-year perspective. Postgrad Med J. 2016;92:63–9.
Cornell S. Continual evolution of type 2 diabetes: an update on pathophysiology and emerging treatment options. Ther Clin Risk Manag. 2015;11:621–32.
Buchwald H, Menchaca HJ, Michalek VN, Bertin NT. Ileal effect on blood glucose, HbA1c, and GLP-1 in Goto-Kakizaki rats. Obes Surg. 2014;24:1954–60.
Portha B, Giroix MH, Tourrel CC, Le-Stunff H, Movassat J. The GK rat: a prototype for the study of non-overweight type 2 diabetes. Methods Mol Biol. 2012;933:125–59.
Xue B, Sukumaran S, Nie J, Jusko WJ, Dubois DC, Almon RR. Adipose tissue deficiency and chronic inflammation in diabetic Goto-Kakizaki rats. PLoS One. 2011;6:e17386.
Almon RR, DuBois DC, Lai W. XueB, Nie J, JuskoWJ. Gene expression analysis of hepatic roles in cause and development of diabetes in Goto-Kakizaki rats. J Endocrinol. 2009;200:331–46.
Santos MS, Santos DL, Palmeira CM, Seiça R, Moreno AJ, Oliveira CR. Brain and liver mitochondria isolated from diabetic Goto-Kakizaki rats show different susceptibility to induced oxidative stress. Diabetes Metab Res Rev. 2001;17:223–30.
Goto Y, Kakizaki M. The spontaneous diabetic rat: a model of non-insulin dependent diabetes mellitus. Proc Jpn Acad. 1981;57:381–4.
Goto Y, Suzuki K, Sasaki M, Toyota T. Development of diabetes in the non-obese NIDDM rat (GK rat). AdvExp Med Biol. 1988;246:29–31.
McIntosh CHS, Pederson RA. Noninsulin-dependent animal models of diabetes mellitus. In: McNeill JH, editor. Experimental models of diabetes. Boca Raton: CRC; 1999. p. 337–98.
Watanabe K, Terada K, Sato J. Intestinal absorption of cephalexin in diabetes mellitus model rats. Eur J Pharm Sci. 2003;19:91–8.
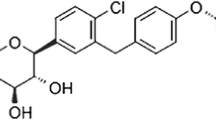
Ogata M, Uchimura T, Iizuka Y, Murata R, Suzuki S, Toyota T, Hikichi N. Effect of non-insulin dependent diabetes on cyclosporin a disposition in Goto-Kakizaki (GK) Rats. Biol Pharm Bull. 1997;20:1026–9.
Gao W, Jusko WJ. Pharmacokinetic and pharmacodynamic modeling of exendin-4 in type 2 diabetic Goto-Kakizaki rats. JPET. 2011;336:881–90.
Center for drug evaluation research. BYETTA® (exenatide injection) pharmacology review, US FDA, NDA 21-773, 2005. pp. 1–393.
Mustajarvi II, Ihalmo P, Uutela P, Madetoja M, Kortejarvi H, Ketola RA, Yliperttula M. Hypoglycemic interaction of two drugsin control rats and in a rat model of diabetes. Univ Helsinki. 2013:52–54.
Watanabea M, Kobayashia M, Oguraa J, Takahashib N, Yamaguchia H, Isekia K. Alteration of pharmacokinetics of grepafloxacin in type 2 diabetic rats. J Pharm Pharm Sci. 2014;17:25–33.
He L, Yang Y, Guo C, Yao D, Liu HH, Sheng JJ, Zhou WP, Ren J, DongLiu X, Pan GY. Opposite regulation of hepatic breast cancer resistance protein in type 1 and 2 diabetesmellitus. Eur J Pharmacol. 2014;724:185–92.
Cao Y, DuBois DC, Almon RR, Jusko WJ. Pharmacokinetics of salsalate and salicylic acid in normal and diabetic rats. Biopharm Drug Dispos. 2012;33:285–91.
Takahashi A, Saito K, Takizawa Y, Murata R. Effect of Diabetes on theophylline disposition in the rat. Jpn J Hosp Pharm. 1999;25:603–7.
Terada T, Sawada K, Saito H, Hashimoto Y, Inui K. Functional characteristics of basolateral peptide transporter in the human intestinal cell line Caco-2. Am J Physiol. 1999;276:1435–41.
Ogihara H, Saito H, Shin BC, Terada T, Takenoshita S, Nagamachi Y, Inui K, Takata K. Immuno-localization of1 H/peptide co-transporter in rat digestive tract. Biochem Biophys Res Commun. 1996;220:848–52.
Padoin C, Tod M, Perret G, Petitjean O. Analysis of the pharmacokinetic interaction between cephalexin and quinapril by a nonlinear mixed-effect model. Antimicrob Agents Chemother. 1998;42:1463–9.
Hsiu SL, Hou YC, Wang YH, Tsao CW, Su SF, Chao PD. Quercetin significantly decreased cyclosporin oral bioavailability in pigs and rats. Life Sci. 2002;72:227–35.
Ogata M, Iizuka Y, Murata R, Hikichi N. Effect of streptozotocin-induced diabetes on cyclosporin A disposition in rats. Biol Pharm Bull. 1996;19:1586–90.
Copley K, McCowen K, Hiles R, Nielsen LL, Young A, Parkes DG. Investigation of exenatide elimination and its in vivo and in vitro degradation. Curr Drug Metab. 2006;7:367–74.
Herings RM, de Boer A, Stricker BH, Leufkens HG, Porsius A. Hypoglycaemia associated with use of inhibitors of angiotensin converting enzyme. Lancet. 1995;345:1195–8.
Yamaguchi H, Yano I, Hashimoto Y, Inui K. Secretory mechanisms of grepafloxacin andlevofloxacin in the human intestinal cell line Caco-2. J Pharmacol Exp Ther. 2000;295:360–6.
Yamaguchi H, Yano I, Saito H, Inui K. Pharmacokinetic role of P-glycoprotein in oral bioavailability and intestinal secretion of grepafloxacin in vivo. J Pharmacol Exp Ther. 2002;300:1063–9.
Nawa A, Fujita-Hamabe W, Tokuyama S. Inducible nitric oxide synthase-mediated decrease of intestinal P-glycoprotein expression under streptozotocin-induced diabetic conditions. Life Sci. 2010;86:402–9.
Hobbs M, Parker C, Birch H, Kenworthy K. Understanding the interplay of drug transporters involved in the disposition of rosuvastatin in the isolated perfused rat liver using a physiologically-based pharmacokinetic model. Xenobiotica. 2012;42:327–38.
Huang L, Wan Y, Grimm S. ATP-dependent transport of rosuvastatin in membrane vesicles expressing breast cancer resistance protein. Drug Metab Dispos. 2006;34:738–42.
Anderson K, Wherle L, Park M, Nelson K, Nguyen L. Salsalate, an old, inexpensive drug with potential new indications: a review of the evidence from 3 recent studies. Am Health Drug Benefits. 2014;7:231–5.
Faghihimani E, Aminorroaya A, Rezvanian H, Adibi P, Ismail-Beigi F, Amini M. Salsalate improves glycemic control in patients with newly diagnosed type 2 diabetes. Acta Diabetol. 2013;5:537–43.
Goldfine AB, Silver R, Aldhahi W, Cai D, Tatro E, Lee J, Shoelson SE. Use of salsalate to target inflammation in the treatment of insulin resistance and type 2. Clin Transl Sci. 2008;1:36–43.
Dahlqvist R, Billing B, Miners JO, Birkett DJ. Nonlinear metabolic disposition of theophylline. Ther Drug Monit. 1984;6:290–7.
Srinivas NR. Strategies for preclinical pharmacokinetic investigation in streptozotocin-induced diabetes mellitus (DMIS) and alloxan-induced diabetes mellitus (DMIA) rat models: case studies and perspectives. Eur J Drug Metab Pharmacokinet. 2015;40:1–12.
Marathe CS, Rayner CK, Jones KL, Horowitz M. Novel insights into the effects of diabetes on gastric motility. Expert Rev Gastroenterol Hepatol. 2016;10:581–93.
Thazhath SS, Marathe CS, Wu T, Chang J, Khoo J, Kuo P, Checklin HL, Bound MJ, Rigda RS, Crouch B, Jones KL, Horowitz M, Rayner CK. The glucagon-like peptide 1 receptor agonist exenatide inhibits small intestinal motility, flow, transit, and absorption of glucose in healthy subjects and patients with type 2 diabetes: a randomized controlled trial. Diabetes. 2016;65:269–75.
Boll M, Markovich D, Weber WM, Korte H, Daniel H, Murer H. Expression cloning of a cDNA from rabbit small intestine related to proton-coupled transport of peptides, beta-lactam antibiotics and ACE-inhibitors. Pflugers Arch. 1994;429:146–9.
Watanabe K, Sawano T, Endo T, Sakata M, Sato J. Studies on intestinal absorption of sulpiride: transepithelial transport of sulpiride across the human intestinal cell line Caco-2. Biol Pharm Bull. 2002;25:1345–50.
Moisés EC, Duarte LB, Cavalli RC, Marques MP, Lanchote V, Duarte G, da Cunha SP. Pharmacokinetics of lidocaine and its metabolite in peridural anesthesia administered to pregnant women with gestational diabetes mellitus. Eur J Clin Pharmacol. 2008;64:1189–96.
Matzke GR, Frye RF, Early JJ, Straka RJ, Carson SW. Evaluation of the influence of diabetes mellitus on antipyrine metabolism and CYP1A2 and CYP2D6 activity. Pharmacotherapy. 2000;20:182–90.
Moss DM, Neary M, Owen A. The role of drug transporters in the kidney: lessons from tenofovir. Front Pharmacol. 2014;5:248.
Tzvetkov MV, dos Santos Pereira JN, Meineke I, Saadatmand AR, Stingl JC, Brockmöller J. Morphine is a substrate of the organic cation transporter OCT1 and polymorphisms in OCT1 gene affect morphine pharmacokinetics after codeine administration. Biochem. Pharmacol. 2013;86:666–78.
Moss DM, Kwan WS, Liptrott NJ, Smith DL, Siccardi M, Khoo SH, Back DJ, Owen A. Raltegravir is a substrate for SLC22A6: a putative mechanism for the interaction between raltegravir and tenofovir. Antimicrob Agents Chemother. 2011;55:879–87.
DeGorter MK, Xia CQ, Yang JJ, Kim RB. Drug transporters in drug efficacy and toxicity. Annu Rev Pharmacol Toxicol. 2012;52:249–73.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors are employees of Cadila Health Care Ltd. and wish to declare that they have no conflict of interest or competing interests in the contents of the review manuscript (ZRC Publication No. 488).
Funding
The present work was not funded by any external sources.
Rights and permissions
About this article
Cite this article
Patel, H., Giri, P. & Srinivas, N.R. Review of Pharmacokinetic Data of Different Drug Classes in Goto-Kakizaki Rats, a Non-obese Model for Type 2 Diabetes Mellitus: Case Studies and Perspectives. Eur J Drug Metab Pharmacokinet 42, 173–182 (2017). https://doi.org/10.1007/s13318-016-0373-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-016-0373-y