Abstract
Objective
To study whether addition of pidotimod to inhaled corticosteroid (ICS) therapy enhances control in children with persistent asthma, as compared to ICS therapy alone.
Design
Triple-blinded, randomized controlled trial.
Setting
Allergy and Asthma Clinic, Department of Pediatrics, at a tertiary care hospital between May, 2018 and June, 2019.
Patients
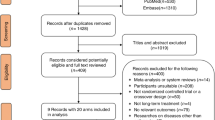
79 children (5–12 years) with newly diagnosed persistent asthma as per Global Initiative for Asthma guidelines.
Interventions
Children received 7 mL twice-a-day for 15 day, followed by 7 mL once-a-day for 45 days of either pidotimod (n=39) or placebo (n=40). In addition, both groups received inhaled budesonide via metered dose inhaler and spacer, throughout the study. Children were followed up every 4 weeks for a total of 12 weeks. At each follow-up visit, peak expiratory flow (PEF) and asthma symptom score and medicine adverse effects were recorded.
Main outcome measures
Change in PEF at 12 weeks compared to baseline. Secondary outcomes were PEF at each follow-up visit, asthma symptom score at each visit, change in asthma symptom score at 12 weeks, and adverse event profile.
Results
The median (IQR) change in PEF (from baseline to 12 weeks) was 13.0% (0.8%, 28.3%) in pidotimod group (n=35) vs 17.7% (4.3%, 35.2%) in placebo group (n=35) (P=0.69). All the secondary outcomes were also comparable between the two groups. There were no significant adverse effects observed.
Conclusions
Addition of pidotimod for 8 weeks to standard ICS therapy did not enhance asthma control compared to placebo.
Similar content being viewed by others
References
Ferrario BE, Garuti S, Braido F, et al. The state of art. Clin Mol Allergy. 2015;13:8.
Cohn L, Elias JA, Chupp GL. Asthma: mechanisms of disease persistence and progression. Ann Rev Immunol. 2004;22:789–815.
Gourgiotis D, Papadopoulos NG, Bossios A, et al. Immune modulator pidotimod decreases the in vitro expression of CD30 in peripheral blood mononuclear cells of atopic asthmatic and normal children. J Asthma. 2004;41:285–87.
Vargas CJB, Espinosa MS, Bolaños AJC, et al. Pidotimod in recurring respiratory infection in children with allergic rhinitis, asthma, or both conditions. Rev Alerg Mex. 2002;49:27–32 [Spanish].
Simonova AY. Prophylaxis of acute respiratory tract infections in children with recurrent bronchopulmonary disorders. Curr Pediatr. 2013;12:148–53.
Licari A, De Amici M, Nigrisoli S, et al. Pidotimod may prevent recurrent respiratory infections in children. Minerva Pediatr. 2014;66:363–7.
Valentini D, Di Camillo C, Mirante N, et al. Effects of Pidotimod on recurrent respiratory infections in children with Down syndrome: A retrospective Italian study. Ital J Pediatr. 2020;46:31.
Mameli C, Pasinato A, Picca M, et al. Pidotimod for the prevention of acute respiratory infections in healthy children entering into daycare: A double blind randomized placebo-controlled study. Pharmacol Res. 2015;97:79–83.
Global Initiative for Asthma. Global Stratergy for Asthma Management and Prevention, 2017. Accessed December 17, 2017. Available from: https:www.ginasthma.org
Singh M, Kumar L. Randomized comparison of a dry powder inhaler and metered dose inhaler with spacer in management of children with asthma. Indian Pediatr. 2001;38:24–8.
Culver BH, Graham BL, Coates AL, et al. Recommendations for a Standardized Pulmonary Function Report. An Official American Thoracic Society Technical Statement. Am J Respir Crit Care Med. 2017;196:1463–72.
Parmar V, Kumar L, Malik SK. Normal values of peak expiratory flow rates in healthy North Indian school children 6–16 years of age. Indian Pediatr. 1977;14:591–94.
Zhao X. Application analysis of pidotimod in the treatment of allergic rhinitis in children accompanied by allergic asthma. J Hainan Med Univ. 2017;4:148.
Kaznacheeva LF, Molokova AV, Kaznacheev KS, et al. Prophylaxis of recurrent respiratory infections in children with allergic diseases of respiratory tract. Vopr Sovrem Pediatr. 2010;9:64–66.
Namazova-Baranova LS, Alekseeva AA, Kharit SM, et al. Efficacy and safety of pidotimod in the prevention of recurrent respiratory infections in children: A multicentre study. Int J Immunopathol Pharmacol. 2014;27:413–19.
Das D, Narayanan V, Rathod R, et al. Efficacy of pidotimod in reducing recurrent respiratory tract infections in Indian children. New Indian Journal Pediatrics. 2017;6:101–10.
Santamaria F, Montella S, Stocchero M, et al. Effects of pidotimod and bifidobacteria mixture on clinical symptoms and urinary metabolomic profile of children with recurrent respiratory infections: a randomized placebo-controlled trial. Pulm Pharmacol Ther. 2019;58:101818.
Niu H, Wang R, Jia YT, et al. Pidotimod, an immuno-stimulant in pediatric recurrent respiratory tract infections: A meta-analysis of randomized controlled trials. Int Immunopharmacol. 2019;67:35–45.
Mahashur A, Thomas PK, Mehta P, et al. Pidotimod: In-depth review of current evidence. Lung India. 2019;36:422–33.
Zhao N, Liu C, Zhu C, et al. Pidotimod: a review of its pharmacological features and clinical effectiveness in respiratory tract infections. Expert Rev Anti Infect Ther. 2019;17:803–18.
Acknowledgements
Mr. Deepak Dhawan, Respiratory Technician, Advanced Pediatrics Centre, for performing PEF measurements in the enrolled children. Mrs. Deepika Rechal, Research Nurse, for assistance with enrolment and follow-up of children in this study.
Funding
M/s Wockhardt Limited (Mumbai, India) provided pidotimod and identical placebo, free of cost
Author information
Authors and Affiliations
Corresponding author
Additional information
Ethics Clearance
Institute’s Ethics Committee, PGIMER; No. NK/4232/MD/481 dated 20 March, 2018.
Contributors
RD: enrolled patients, collected data, interpreted them, and drafted the manuscript; JLM: conceived and designed the study, supervised data collection, revised and finalized the manuscript. He will act as guarantor of the study; MS: was overall in-charge of patient management and helped in manuscript writing. The final manuscript was approved by all authors.
Competing interest
None stated.
Rights and permissions
About this article
Cite this article
Deglurkar, R., Mathew, J.L. & Singh, M. Efficacy and Safety of Pidotimod in Persistent Asthma: A Randomized Triple-Blinded Placebo-Controlled Trial. Indian Pediatr 59, 201–205 (2022). https://doi.org/10.1007/s13312-022-2465-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13312-022-2465-x