Abstract
Decades of experience supports LDLT as a favorable strategy to reduce waitlist mortality. The multiple regenerative pathways of hepatocytes and other hepatic cells justify the rationale behind it. Nonetheless, living liver donation is still underused and its broader implementation is challenging, mostly due to variability in practices leading to concerns related to donor safety. A non-systematic literature search was conducted for peer-reviewed original articles related to pre-operative evaluation of living liver donor candidates. Eligible studies were synthesized upon consensus for discussion in this up-to-date review. Review of the literature demonstrate that the importance of preoperative assessment of vascular, biliary and liver volume to ensure donor safety and adequate surgical planning for graft procurement is widely recognized. Moreover, data indicates that anatomic variants in vascular and biliary systems in healthy donors are common, present in up to 50% of the population. Therefore, comprehensive mapping and visualizations of each component is needed. Different imaging modalities are reported across practices and are discussed in detail. Lastly, assessment of liver volume must take into account several technical and donor factors that increase the chances of errors in volume estimation, which occurs in up to 10% of the cases. Experience suggests that maximizing donor safety and lessening their risks is a result of integrated experience between hepatobiliary and transplant surgery, along with multidisciplinary efforts in performing a comprehensive pre-operative donor assessment. Although technical advances have increased the accuracy of volume estimation, over- or under-estimation remains a challenge that needs further attention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Waitlist mortality continues to be a noxious reality despite constant efforts to reduce it. The limited availability of acceptable quality grafts from deceased donors in relation to the increasingly high demand has lead transplant teams to constantly search for alternatives to replenish the organ pool. Decades of experience supports living donor liver transplant (LDLT) as a feasible pathway to achieve faster access to transplantation, and therefore, as a favorable strategy to reduce waitlist mortality [1, 2]. In addition, the comprehensive pre-operative evaluation of living donor candidates ensures transplantation with overall high-quality allografts conveying additional benefits, including higher survival rates to the recipient when compared to LT with deceased donors [3,4,5].
The multiple regenerative pathways of hepatocytes and other hepatic cells justify the rationale behind LDLT. More importantly, this intrinsic capacity is even more evident within normal hepatic tissue [6], which is expected to be the case for a living donor. Experimental models have demonstrated activation of pathways leading to liver regeneration as early as 2 h after partial hepatectomies [6]. In humans, increased-regenerative markers have been observed within the first days following living donor hepatectomy, with evidence of almost all functional and volumetric recovery within the first 3–4 months up to over a year depending on the donated graft [7,8,9]. Although differences in the regenerative extent and time between donors and recipients have been observed, the regenerative ability of the liver also safeguards that the transplanted segment into the recipient will restore liver function and volumes, with observed reconstitution percent up to 93% after 3 months of LDLT [10,11,12].
Despite that, LDLT is still underused and broader implementation of this technique has been challenging [1]. In a recent meeting report by the American Society of Transplantation LDLT Consensus Conference Working Group, three main themes were identified as barriers limiting LDLT, including position toward it and data gaps related to candidate and donor selection, as well as post-transplant outcomes and long-term monitoring [1]. Interestingly, the theme with the greatest number of identified barriers was related to evaluation and selection for LDLT, which highlighted the existence of a “gray zone” in donor selection, mostly driven by the current variability in donor assessment across centers. Consequently, this variability limits the ability to quantify relative and absolute donor risk, a major pillar for LDLT [1]. Therefore, standardization of practices and a clear understanding of the pre-operative evaluation for living donors is crucial. Here, we aim to present an up-to-date review of pre-operative assessment practices of living liver donor candidates, with a particular focus on vascular and biliary, as well as volumetric evaluation.
Methods
A non-systematic literature search was conducted in PubMed/Medline database during August–October 2023 for peer-reviewed original articles related to pre-operative evaluation of living liver donor candidates. No time limitations filters were set. However, in order present an up-to-date review, articles published in the last 5–10 years were preferentially included. English-language literature including retrospective studies, single/multicenter cohorts, case reports, as well as systematic reviews and meta-analysis were reviewed. Google Scholar database was also queried as an attempt to capture available literature in understudied topics. Articles deemed relevant were assessed and selected upon consensus among authors for discussion in this comprehensive narrative synthesis of previously published information.
Addressing the challenges
Minimizing donor risks and complication rates is a primary goal during LDLT. Although mortality rate following living donor hepatectomy is close to zero, reported minor and major complications rates range from 1.7 to 43.1%, and 2.1 to 28%, respectively [13,14,15,16]. The wide range might reflect the variability among practices across centers and the lack of standardization when it comes to pre- and post-operative assessment of living liver donors. Previous reports have shown that increasing experience and volume of cases are associated to improved donor outcomes [14, 16]. Therefore, it is important that the transplant community—particularly those interested in performing LDLT—recognize that optimization of donor safety is a result of team effort, rather than individual work. In our experience, this goal can be achieved by establishing a multidisciplinary living donor team that continuously evaluate tasks checklists, performs weekly planning meetings and quality reviews, provides active social and ethics support, and share a commitment to quality improvement and generating new knowledge.
Donor evaluation
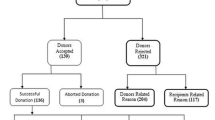
Despite slight variations depending on the region of practice, criteria for living liver donation often consider candidates that are in good overall physical and mental health, are ≥ 18 years of age—and generally < 60y—, and are able to provide informed consent [17,18,19]. The medical evaluation must address areas related to general medical history, psychosocial history, physical exam, transmittable disease testing, case-specific and liver-related laboratory testing, and anatomic assessment [17]. As pertinent for the present review, we will now discuss the components of the anatomic assessment.
The importance of vascular anatomy evaluation and volume estimation
Anatomic assessment of a living liver donor candidate is perhaps the most challenging, yet most important, step during pre-operative evaluation. A summary of important considerations during anatomic assessment of living liver donor candidates is depicted in Table 1. A comprehensive radiologic evaluation allows not only to ensure eligibility and quality of the potential graft, but also to perform appropriate surgical planning for both procedures, the donor hepatectomy and the recipient transplant [20, 21]. Donor candidates must complete serial assessments of vascular anatomy, biliary anatomy and liver volumes. Although, the lack of recognized guidelines limits standardization of practices and imaging modalities to be used, donor safety remains the primary goal during evaluation. Therefore, imaging techniques must be carefully selected based on each center’s resources availability and expertise [21]. Moreover, it is of utmost importance to meet the requirements set forth by designated transplant organizations depending on the region of practice to ensure that the transplant hospital has adequate resources in place to perform living donor assessment, surgical procedures and guarantee adequate recovery. For instance, detailed requirements for liver transplant programs that perform living donor recovery in the United States can be found on the Organ Procurement and Transplantation Network (OPTN) Membership Application for Liver Transplant Programs Part 9 [22].
Vascular anatomy
Arterial anatomy
Identification of presence of hepatic artery (HA) anatomic variations, as well as adequate length measurement of the arteries before bifurcation are crucial components of the surgical planning for graft procurement and reconstruction, which can be quite challenging and complex depending on the anatomic variation. Three-dimensional (3D) reconstruction of the HA anatomy using contrast-enhanced computed tomography angiography (CTA) and magnetic resonance angiography (MRA) with Gadolinium-based contrast agents are the main imaging techniques for arterial assessment [21, 23]. In comparison with two-dimensional CT, the higher spatial resolution of 3D—CTA imaging allows visualization of even the most complex hepatic artery branches configurations, including evaluation of segment IV anatomy [21, 23, 24]. CTA potential superiority remains true against MRA, which has lower spatial resolution than CTA, is more prone to respiratory motion artifacts and is more technically demanding [21]. Therefore, CTA is usually the preferred modality across centers. Nonetheless, associated risks including exposure to high radiation and inherent risks associated with intravenous contrast use should be consider when assessing living donor candidates [25]. Recent efforts toward non-contrast modalities to minimize such harms without compromising visualization scores and diagnostic ability seems promising and need to be further evaluated [25, 26].
The conventional hepatic arterial anatomy, where the common hepatic artery (CHA) arises from the celiac trunk, then branches into the gastroduodenal artery and proper hepatic artery, with the latest further bifurcating into the right (RHA) and left hepatic artery (LHA), is present in about 55 to 76% of the donors [21, 24, 27]. Nevertheless, variations in intrahepatic and extrahepatic branching of hepatic arteries have been observed in up to 50% of the cases. Commonly used classifications for anatomic variants of the hepatic artery are shown in Fig. 1. Inadequate evaluation of such variants leads to detrimental peri- and post-operative complications for donors and recipients, including inadvertent intraoperative injury, excessive dissection, graft hypoperfusion, and increased risk of hepatic artery thrombosis [21, 24]. Important attention must be placed in situations where the right hepatic artery passes behind or through the head of the pancreas, and cases where an accessory LHA runs along the ligamentum venosum fissure with the native LHA running a normal course. These variations are the two most common, reported to be present in 3.7% and 3.2% of the donors, respectively [21]. Nonetheless, surgeons are required to have vast knowledge of the normal anatomy and possible variations to plan ahead complex reconstructions when needed.
Venous anatomy
Hemodynamics of the portal system and hepatic veins are complex. Moreover, segmental and territorial venous distribution differs vastly among individuals [28, 29]. Thus, favorable outcomes for both, donors and recipients, depend on adequate determination of volume dominance patterns, detailed venous mapping and comprehensive flow assessment [29]. The preferred imaging modalities are 3-dimensional (3D) reconstruction CT with volumetric measurements and magnetic resonance imaging (MRI) [21, 30]. MRI provides the highest contrast resolution for evaluation of venous structures depending on the sequence used (i.e., hepatobiliary phase T1-weighted and steady-state free precession) [21]. Current evidence suggest that 4-dimensional (4D) flow MRI allows for non-invasive detailed anatomic and functional assessments, including measurements of velocity and flows in the portal vein (PV) [28]. However, wide clinical implementation of 4D flow MRI is limited by its long-acquisition time and bounded availability [28].
Portal vein
In about 65% of the population, the PV is formed by the confluence of the splenic vein and the superior mesenteric vein, later branching into a left PV—supplying hepatic segments I to IV—and a right PV—supplying segments V and VIII anteriorly, and segments VI and VII posteriorly—[31]. On the other hand, anatomic variations are present in up to 35% of the population [21, 31]. Although, anatomic variants of the left PV rarely interfere with donor candidacy [23], variations in the right PV can confer significant risks for the remnant liver, interfere with the parenchymal transection plane, and increase the risk for PV thrombosis in the recipient [21, 30,31,32,33]. In addition, due to similar embryologic origins, portal system variants are often associated with variants in the biliary system [21, 32,33,34]. Thus, these cases are usually of high technical complexity and detailed pre-operative imaging assessment and planning of reconstruction techniques are needed to guarantee safe use of such grafts.
Common PV variations observed in living donor candidates include trifurcation of the main PV, caudal origin of the right-posterior segmental branch, and left PV origin of the right-posterior segmental branch [30, 31, 33] (Fig. 2). In the conventional presentation, the donor’s right PV is usually anastomosed to the recipient’s main portal trunk [30]. In the presence of anatomic variations, reconstruction of the PV orifice depends on the type of anomaly and can be achieved by unification or back-wall plasty, back-wall plasty with saphenous vein graft interposition, or Y-graft interposition with cryopreserved iliac vein graft, among others. More complex scenarios may require reconstruction using quilt venoplasty and vessel extension using cryopreserved iliac veins [30, 32]. Yilmaz and colleagues described the Malatya approach for reconstruction of anomalous PV configurations in the right lobe for LDLT and found significantly less rates of PV thrombosis and longer survival rates when compared to traditional reconstruction techniques [30]. Decision on which reconstruction technique to perform should be made on a case-by-case basis and requires strict follow-up of PV patency, including intraoperative Doppler ultrasonography and sequential post-operative follow-up according to each center’s protocol. Detailed surgical description of the different available reconstruction techniques and grafts, as well their advantages/disadvantages have been previously discussed elsewhere [30, 32, 33, 35].
Common/clinically relevant classifications for anatomic variants of the portal vein. A anterior branch, F falciform ligament, LPV left portal vein, P posterior branch, P4 portal venous branch to segment 4, P5 portal venous branch to segment 5, P8 portal venous branch to segment 8, PV portal vein, RPV right portal vein; *Anatomic variations of the intrahepatic portal vein [60,61,62]
Hepatic veins
The impact of venous outflow in graft regeneration and its role in postoperative outcomes is well elucidated [21, 35]. Important considerations when evaluating donor’s hepatic veins (HV) for appropriate surgical planning and determination of recipient’s adequacy include: (1) anatomy of HV, particularly middle hepatic vein (MHV) and venous tributaries, (2) recipients’ risk factors, and (3) donors’ risk factors.
The usual anatomic distribution of the HV consist of a right trunk—right hepatic vein (RHV)- which drain segments VII and VI, and a common trunk giving rise to the MHV and left hepatic vein (LHV), draining segments IV, V and VIII, and II-III, respectively [21]. Anatomic variants have been observed in approximately 40% of living donor candidates, with the most common represented by the presence of an accessory (inferior) right hepatic vein draining segment VI and the inferior aspect of segment VII [21]. Relevant classifications for anatomic variants of the hepatic vein are shown in Fig. 3. In a recent study, Senne et al. found that grafts without an accessory RHV demonstrated a pattern of drainage volume distribution of RHV dominance in 82% of the cases, followed by MHV in 16.5% and to a lesser extent LHV (1.5%). On the other hand, in the presence of an accessory HV the dominant drainage volume distribution shifted toward the MHV (49%), followed by the RHV (48%) [29]. In common practice, accessory hepatic veins with small diameter are usually ligated. However, if the diameter is approximately > 4 mm, anastomosis to the recipient inferior vena cava (IVC) is recommended to avoid congestion of the posterior segments [21]. This approach is preferred in our practice. However, practices can vary based on surgeon’s preference. Some groups use the “saline test” or probing, where cold saline is flushed into the vein under evaluation to assess the presence of veno-venous communications and to better guide the need for reconstruction [36, 37].
Common/clinically relevant classifications for anatomic variants of the hepatic vein. ASSV anterior superior segmental vein, IHV inferior hepatic veins, IVC inferior vena cava, LMV left median vein, LHV left hepatic vein, MHV middle hepatic vein. *Variations of the superior right hepatic vein [63,64,65]
Despite years of experience and several reports of postoperative outcomes in donors and recipients, inclusion of the MHV in the right graft for LDLT remains a topic of debate. In grafts where the MHV is not procured, identification and characterization of MHV segment V and VIII tributaries requires particular attention. The International Liver Transplant Society Guideline on Living Liver Donation recommends reconstruction of segment V and VIII tributaries with diameters > 5 mm to reduce the risk of anterior segment congestion, graft dysfunction and to improve recipient outcomes [19]. Other practices recommend backtable reconstruction of tributaries measuring ≥ 4 mm [21, 23]. Multiple reconstruction techniques with favorable outcomes have been reported. A common practice to reconstruct the MHV is to create a neo-MHV by end-to-side anastomosis of both tributaries to an interposition graft [38]. Interposition grafts commonly used for reconstruction include cryopreserved deceased donor iliac veins, allogenic vascular grafts and polytetrafluoroethylene grafts [35]. Recent reports support the use of synthetic over biologic grafts for MHV reconstruction in adult-to-adult LDLT [39]. The limited supply, constrained storage life, and restrictions on adequate diameter and length for reconstruction are among the shortcomings of biologic grafts [39]. On the other hand, synthetic grafts may result in accidental migration or persistence of non-degradable foreign bodies [40, 41]. A handful of authors have studied short- and long- term patency rates between different materials for vessel reconstruction [39,40,41]. However, the impact of the reconstruction material on LDLT recipient’s postoperative outcomes is an understudied area and further research is needed to better elucidate the most suitable material for MHV reconstruction in LDLT.
Finally, identification of recipients and donors’ factors associated with negative impact on outflow hemodynamics is critical during LDLT pre-operative evaluation. Poorer outcomes, including development of small for size syndrome, are associated to recipients with a graft-to-recipient weight ratio (GRWR) < 0.8%, presence of portal hypertension, sarcopenia and high Model for end-stage Liver disease (MELD) scores [35]. Similarly, grafts from donors with steatosis, which limits tolerance to portal hyperperfusion, as well as those with low-estimated future remnant volume (FRV) conveys increased risks for negative outcomes [35]. Therefore, presence of these conditions require special attention and reconsideration of donor-recipient pairing might be needed.
Biliary anatomy
The intricate anatomy of bile duct confluence adds complexity to the already technically challenging donor and recipient surgery. Moreover, surgeons must be aware of the different possible anatomic variants (Fig. 4), which can be found in almost half of the population [21, 42]. Importantly, anatomic variations are more common in the right hepatic duct, including drainage of the right-posterior duct into the left hepatic duct, trifurcation of the biliary ducts and right-posterior duct draining into the common hepatic duct [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42]. Therefore, detailed evaluation of donors’ bile duct anatomy is needed to achieve successful postoperative outcomes. (Fig. 5).
Common/clinically relevant classifications for anatomic variants of the bile ducts. A anterior-sectional bile duct, CHD common hepatic duct, LHD left hepatic duct, RAHD right-anterior hepatic duct, RPHD right-posterior hepatic duct, P posterior-sectional bile duct, *Confluence patterns of the right and left intrahepatic bile ducts [66, 67]
Pre-operative assessment with magnetic resonance cholangiopancreatography (MRCP) in a living donor candidate with two separate right hepatic ducts (A). Intraoperative cholangiogram of the same donor consistent with preoperative MRI findings with evidence of two right hepatic ducts draining separately into the main and left hepatic ducts (B). Arrows: right-anterior and right-posterior hepatic ducts
Intraoperative cholangiogram with cannulation of the cystic duct is the gold standard imaging technique for evaluation of biliary anatomy [23, 42]. Nonetheless, pre-operative assessment with magnetic resonance cholangiopancreatography (MRCP) is usually the preferred method for pre-operative donor evaluation due to its non-invasive nature, high sensitivity and high accuracy in detecting anatomic variants in the biliary tract [21, 42]. Diagnostic accuracy, possibility to detect second and third order bile ducts, and degree of compromise by respiratory motion and ghosting artifacts varies among techniques [21, 23]. Data suggest that a combination of T1-weighted and T2-weighted sequences for depiction of bile ducts provides improved diagnostic accuracy [21, 23]. As for the hepatobiliary contrast agent, gadoxetate disodium is usually preferred due to its higher percentage of biliary excretion and shorter delay for the hepatobiliary phase when compared to other agents [21]. In the last decade, the potential benefits of near-infrared imaging with indocyanine green (ICG), a sterile, liver-specific, non-ionizing, non-toxic and water-soluble fluorescent dye as an adjuvant in hepatobiliary surgery has been widely recognized [43, 44]. Initial experience with ICG fluorescence cholangiography for living donor hepatectomy demonstrated its role in improving outcomes for LDLT, achieving reduction of biliary complications for donors and recipients [45, 46]. The real-time identification of the biliary tract around the hilar plate allows for optimal identification of bile duct anatomy variations and facilitate it safe dissection and appropriate division points for bile ducts during open or laparoscopic LDLT [47]. Current consensus recommendations for the use of ICG fluorescence in hepatobiliary surgery recommends a dose of 2.5 mg ICG administered intravenously for LDLT biliary mapping, 15 to 30 min before dissection of the hilar plate [47]. Nonetheless, available literature pertinent to ICG fluorescence cholangiography for living donor hepatectomy is limited. Current practices support its use as a complementary tool, rather than a replacement for the current gold standard. Further evidence is needed in order standardize practices around its use, particularly under emerging approaches for living donor hepatectomy such minimally invasive techniques.
Although, a comprehensive pre-operative imaging of donors’ biliary anatomy will not ensure a complication-free procedure, it can definitely aid to minimize the associated risks. Biliary complications occur in up to 9% of donors and represent an important cause of donor morbidity following living donor hepatectomy [15, 48]. The severity of the complications in donors ranges from minor and self-limited to severe complications—usually related to bile leaks and biliary fistulas—leading to longer length of stay, higher readmission rates, higher costs of care, need for repeated interventions and lower quality of life [15, 48, 49]. Risk factors associated with biliary complications include anatomic intrahepatic duct type, donation of the right lobe and number of bile duct orifices in the RL [48].
Decision to proceed with donation in cases with complex biliary anatomy requires considerate deliberation based on centers’ capability and surgeons’ experience. Some suggest that donors with 3 or more right hepatic ducts, as well as those with variations that could compromise segmental bile drainage should be avoided [50]. Therefore, pre-operative mapping of the biliary anatomy is an important step during surgical planning, allowing the surgeon to determine donor candidacy, the most adequate bile duct transection line and most suitable technique for biliary anastomosis [23]. In the recipient, single duct anastomosis are more common, and are usually performed by duct-to-duct anastomosis with or without ductoplasty or Roux-en-Y. Nonetheless, presence of more than one duct constitutes an important number of cases and require particular attention to avoid technical complications and negative postoperative outcomes [51]. Decision to perform biliary reconstructions or ligation in such cases remains a topic of debate.
Liver volumes
The regenerative ability of the liver into a functional unit is influenced by the donor remnant fraction [12]. Although, there is not a standardized cut-off value, common practice is to ensure a remnant liver volume (RLV) to total liver volume (TLV) ratio ≥ 30% [52]. A recent meta-analysis found overall and minor morbidity to be significantly lower among donors with RLV/TLV ≥ 30% when compared to those < 30%. In addition, donors with RLV/TLV < 30% demonstrated a higher degree of impartment in postoperative liver function, evidenced by significantly higher peak bilirubin and peak INR levels vs donors in the RLV/TLV ≥ 30% group [52]. Therefore, living donation from donors with a low RLV/TLV (< 30%) may induce liver dysfunction and should be avoided if possible. Although reported incidence of post-hepatectomy liver failure is variable, it can be as high as 32% [21]. Therefore, estimation of liver volume is vital to ensure donor safety as the primary outcome during LDLT. However, when deciding appropriate donor-recipient pairing, it is important to have in mind that a GRWR ≥ 0.8% safeguards favorable outcomes in the recipient [53].
Precise estimation of liver volume is challenging, as it is affected not only by the technique used, but also by several donor’s characteristics including age, gender and presence of steatosis [21, 53]. Data suggest that pre-operative volume estimations can vary up to 10% when compared to actual graft weight measured intraoperatively [53]. Volume estimation can be performed by manual techniques including calculations based on surface body area, as well as semi-automated (conventional CT or MRI volumetry) and fully-automated imaging techniques with 3D reconstructions and segmentation of the liver [21, 53,54,55]. (Fig. 6). Technical advances and better understanding of deep learning models have allowed for the development of automatic methods that are reliable, operator independent, can be used in parallel and can provide improved performance of segmentation [54]. Moreover, conventional 2D imaging techniques fall short on consideration of blood volume within the liver, while modern 3D techniques with novel software allows for exclusion of blood volume, providing a more accurate assessment of liver parenchyma and less overall error in volume estimation [53, 55]. Efforts to develop highly accurate and advanced software specifically designed for the LDLT setting are currently ongoing [56, 57]. A recent report demonstrated accurate prediction of the actual graft weight among 106 living donors undergoing right lobe hepatectomy, left lobe hepatectomy and left lateral segmentectomies using a novel software. [56] In addition, it was found that 95.3% of the measurements were within the 95% range of agreement between the software and established manual measurements [56]. Development of LDLT-specific validated software such as that one is an important pillar toward safer practices in LDLT. Nonetheless, regardless of the technique used, to ensure donor safety surgeons need to account for all the possible factors leading to overestimation and underestimation errors on a case-by-case basis when deciding donor candidacy.
Liver volumetric assessment in a living donor candidate performed using semi-automated liver volumetry software with 3D reconstructions and segmentation of the liver (LiverVision® software) (A), allowing safe practices and accurate prediction of the actual graft weight for living donor liver transplantation (B)
Conclusion
Donor safety remains the main priority in LDLT. Anatomical variants in the vascular and biliary system are common among healthy donors. Although only in limited cases such variants affect donor candidacy, failure to identify them jeopardize donor and recipient safety, and increases technical complexity to the case. Experience suggests that maximizing donor safety and lessening their risks is a result of integrated experience between hepatobiliary and transplant surgery, along with multidisciplinary efforts in performing a comprehensive pre-operative donor assessment. Although, technical advances have increased the accuracy of volume estimation, over- or under-estimation remains a challenge that needs further attention.
Availability of data and materials
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
Jesse MT, Jackson WE, Liapakis A, Ganesh S, Humar A, Goldaracena N, Levitsky J, Mulligan D, Pomfret EA, Ladner DP, Roberts JP, Mavis A, Thiessen C, Trotter J, Winder GS, Griesemer AD, Pillai A, Kumar V, Verna EC, LaPointe Rudow D, Han HH (2023) Living donor liver transplant candidate and donor selection and engagement: Meeting report from the living donor liver transplant consensus conference. Clin Transplant 37(7):e14954. https://doi.org/10.1111/ctr.14954. (Epub 2023 Mar 16. PMID: 36892182)
Barbetta A, Aljehani M, Kim M, Tien C, Ahearn A, Schilperoort H, Sher L, Emamaullee J (2021) Meta-analysis and meta-regression of outcomes for adult living donor liver transplantation versus deceased donor liver transplantation. Am J Transplant 21(7):2399–2412. https://doi.org/10.1111/ajt.16440. (Epub 2021 Jan 5. PMID: 33300241; PMCID: PMC9048132)
Cavalcante LN, Queiroz RMT, Paz CLDSL, Lyra AC (2022) Better living donor liver transplantation patient survival compared to deceased donor—a systematic review and meta-analysis. Arq Gastroenterol 59(1):129–136. https://doi.org/10.1590/S0004-2803.202200001-22. (PMID: 35442323)
Kim EJ, Lim S, Chu CW, Ryu JH, Yang K, Park YM, Choi BH, Lee TB, Lee SJ (2017) Clinical impacts of donor types of living vs. deceased donors: predictors of one-year mortality in patients with liver transplantation. J Korean Med Sci 32(8):1258–1262. https://doi.org/10.3346/jkms.2017.32.8.1258. (PMID: 28665060; PMCID: PMC5494323)
Olthoff KM, Smith AR, Abecassis M, Baker T, Emond JC, Berg CL, Beil CA, Burton JR Jr, Fisher RA, Freise CE, Gillespie BW, Grant DR, Humar A, Kam I, Merion RM, Pomfret EA, Samstein B, Shaked A (2015) Defining long-term outcomes with living donor liver transplantation in North America. Ann Surg 262(3):465–75. https://doi.org/10.1097/SLA.0000000000001383. (PMID: 26258315; PMCID: PMC4545521)
Michalopoulos GK, Bhushan B (2021) Liver regeneration: biological and pathological mechanisms and implications. Nat Rev Gastroenterol Hepatol 18(1):40–55. https://doi.org/10.1038/s41575-020-0342-4. (Epub 2020 Aug 6 PMID: 32764740)
Klink T, Simon P, Knopp C, Ittrich H, Fischer L, Adam G, Koops A (2014) Liver remnant regeneration in donors after living donor liver transplantation: long-term follow-up using CT and MR imaging. Rofo 186(6):598–605. https://doi.org/10.1055/s-0033-1355894. (Epub 2013 Dec 17 PMID: 24347356)
Duclos J, Bhangui P, Salloum C, Andreani P, Saliba F, Ichai P, Elmaleh A, Castaing D, Azoulay D (2016) Ad integrum functional and volumetric recovery in right lobe living donors: is it really complete 1 year after donor hepatectomy? Am J Transplant 16(1):143–156. https://doi.org/10.1111/ajt.13420. (Epub 2015 Aug 17 PMID: 26280997)
Satilmis B, Akbulut S, Sahin TT, Dalda Y, Tuncer A, Kucukakcali Z, Ogut Z, Yilmaz S (2023) Assessment of liver regeneration in patients who have undergone living donor hepatectomy for living donor liver transplantation. Vaccines 11(2):244. https://doi.org/10.3390/vaccines11020244. (PMID:36851123;PMCID:PMC9962137)
Fingas CD, Beste M, Penndorf V, Sydor S, Nadalin S, Bechmann L, Paul A, Gerken G, Canbay A, Jochum C (2018) Liver regeneration-related cytokine profiles in donors and recipients before and after living-donor liver transplant. Exp Clin Transplant 16(5):554–561. https://doi.org/10.6002/ect.2017.0039. (Epub 2018 Apr 9 PMID: 29633929)
Zhang Y, Li B, He Q, Chu Z, Ji Q (2022) Comparison of liver regeneration between donors and recipients after adult right lobe living-donor liver transplantation. Quant Imaging Med Surg 12(6):3184–3192. https://doi.org/10.21037/qims-21-1077. (PMID:35655846;PMCID:PMC9131329)
Olthoff KM, Emond JC, Shearon TH, Everson G, Baker TB, Fisher RA, Freise CE, Gillespie BW, Everhart JE (2015) Liver regeneration after living donor transplantation: adult-to-adult living donor liver transplantation cohort study. Liver Transplant 21(1):79–88. https://doi.org/10.1002/lt.23966. (Epub 2014 Oct 6. PMID: 25065488; PMCID: PMC4276514)
Vargas PA, McCracken EKE, Mallawaarachchi I, Ratcliffe SJ, Argo C, Pelletier S, Zaydfudim VM, Oberholzer J, Goldaracena N (2021) Donor morbidity is equivalent between right and left hepatectomy for living liver donation: a meta-analysis. Liver Transpl 27(10):1412–1423. https://doi.org/10.1002/lt.26183. (Epub 2021 Jul 14 PMID: 34053171)
Bhatti ABH, Naqvi W, Ali N, Khan NY, Zia HH, Faiz BY, Ilyas A, Rana A, Khan NA (2022) Textbook outcome among voluntary donors undergoing major living donor hepatectomy. Langenbecks Arch Surg 407(7):2905–2913. https://doi.org/10.1007/s00423-022-02578-6. (Epub 2022 Jun 7. PMID: 35670859; PMCID: PMC9171097)
Mazzola A, Pittau G, Hong SK, Chinnakotla S, Tautenhahn HM, Maluf DG, Settmacher U, Spiro M, Raptis DA, Jafarian A, Cherqui D, ERAS4OLT.org Working Group (2022) When is it safe for the liver donor to be discharged home and prevent unnecessary re-hospitalizations?—a systematic review of the literature and expert panel recommendations. Clin Transplant 36(10):e14677. https://doi.org/10.1111/ctr.14677. (PMID: 35429941)
Gorgen A, Goldaracena N, Zhang W, Rosales R, Ghanekar A, Lilly L, Cattral M, Greig P, McCluskey S, McGilvray I, Selzner N, Bhat M, Selzner M, Levy G, Grant D, Sapisochin G (2018) Surgical complications after right hepatectomy for live liver donation: largest single-center western world experience. Semin Liver Dis 38(2):134–144. https://doi.org/10.1055/s-0038-1636932. (Epub 2018 Mar 22 PMID: 29566408)
Guidance for the Medical Evaluation of Potential Living Liver Donors. Organ Procurement and Transplantation Network. https://optn.transplant.hrsa.gov/professionals/by-topic/guidance/guidance-for-the-medical-evaluation-of-potential-living-liver-donors/ Accessed 17 Aug 2023
Kasiske BL, Ahn YS, Conboy M, Dew MA, Folken C, Levan ML, Humar A, Israni AK, Rudow DL, Trotter JF, Massie AB, Musgrove D, Living Donor Collective Participants (2021) Outcomes of living liver donor candidate evaluations in the Living Donor Collective pilot registry. Clin Transplant 35(9):e14394. https://doi.org/10.1111/ctr.14394. (Epub 2021 Aug 3. PMID: 34342054)
Miller CM, Durand F, Heimbach JK, Kim-Schluger L, Lee SG, Lerut J, Lo CM, Quintini C, Pomfret EA (2016) The international liver transplant society guideline on living liver donation. Transplantation 100(6):1238–1243. https://doi.org/10.1097/TP.0000000000001247. (PMID: 27120453)
Karakaya E, Akdur A, Ayvazoglu Soy EH, Harman A, Coskun M, Haberal M (2020) Our living donor protocol for liver transplant: a singlecenter experience. Exp Clin Transplant 18(6):689–695. https://doi.org/10.6002/ect.2020.0280. (PMID: 33187462)
Borhani AA, Elsayes KM, Catania R, Kambadakone A, Furlan A, Kierans AS, Kamath A, Harmath C, Horvat N, Humar A, Kielar AZ (2021) Imaging evaluation of living liver donor candidates: techniques, protocols, and anatomy. Radiographics 41(6):1572–1591. https://doi.org/10.1148/rg.2021210012. (PMID: 34597229)
Department of Health and Human Services Health Resources and Services Administration. OPTN Membership Application for Liver Transplant Programs. https://unos.org/wp-content/uploads/FORM-OPTN-Membership-App-Liver-LDLiver.pdf Accessed 1 Feb 2024
Hecht EM, Kambadakone A, Griesemer AD, Fowler KJ, Wang ZJ, Heimbach JK, Fidler JL (2019) Living donor liver transplantation: overview, imaging technique, and diagnostic considerations. AJR Am J Roentgenol 213(1):54–64. https://doi.org/10.2214/AJR.18.21034. (Epub 2019 Apr 11. Erratum in: AJR Am J Roentgenol. 2019 Sep;213(3):723. PMID: 30973783)
Yan J, Feng H, Wang H, Yuan F, Yang C, Liang X, Chen W, Wang J (2020) Hepatic artery classification based on three-dimensional CT. Br J Surg 107(7):906–916. https://doi.org/10.1002/bjs.11458. (Epub 2020 Feb 14 PMID: 32057096)
Lin WC, Chen CM, Westphalen AC, Lin TY, Chang CH, Chen LK, Lin CW, Yeh CC, Yu J, Jeng LB, Chen JH (2023) Non-contrast-enhanced MR arteriography of potential living-related liver donor: using contrast enhanced CT arteriography as standard reference. J Magn Reson Imaging 58(3):894–904. https://doi.org/10.1002/jmri.28571. (Epub 2022 Dec 27 PMID: 36573963)
Liao CC, Chen MH, Yu CY, Tsang LL, Chen CL, Hsu HW, Lim WX, Chuang YH, Huang PH, Cheng YF, Ou HY (2022) Non-contrast-enhanced and contrast-enhanced magnetic resonance angiography in living donor liver vascular anatomy. Diagnostics 12(2):498. https://doi.org/10.3390/diagnostics12020498. (PMID:35204588;PMCID:PMC8871101)
Khalid A, Saleem MA, Ihsan-Ul-Haq, Khan Y, Rashid S, Dar FS (2023) Anatomical variations in living donors for liver transplantation-prevalence and relationship. Langenbecks Arch Surg 408(1):323. https://doi.org/10.1007/s00423-023-03066-1. (PMID: 37597008)
Oechtering TH, Roberts GS, Panagiotopoulos N, Wieben O, Reeder SB, Roldán-Alzate A (2022) Clinical applications of 4D flow MRI in the portal venous system. Magn Reson Med Sci. 21(2):340–353. https://doi.org/10.2463/mrms.rev.2021-0105. (Epub 2022 Jan 25. PMID: 35082218; PMCID: PMC9680553)
Senne M, Sgourakis G, Molmenti EP, Schroeder T, Beckebaum S, Nadalin S, Malagó M, Radtke A (2022) Portal and hepatic venous territorial mapping in healthy human livers: virtual three-dimensional computed tomography size-shape-topography study. Exp Clin Transplant 20(9):826–834. https://doi.org/10.6002/ect.2022.0053. (PMID: 36169105)
Yilmaz S, Kayaalp C, Isik B, Ersan V, Otan E, Akbulut S, Dirican A, Kutlu R, Kahraman AS, Ara C, Yilmaz M, Unal B, Aydin C, Piskin T, Ozgor D, Ates M, Ozdemir F, Ince V, Koc C, Baskiran A, Dogan SM, Barut B, Sumer F, Karakas S, Kutluturk K, Yologlu S, Gozukara H (2017) Reconstruction of anomalous portal venous branching in right lobe living donor liver transplantation: Malatya approach. Liver Transpl 23(6):751–761. https://doi.org/10.1002/lt.24753. (PMID: 28240812)
Carneiro C, Brito J, Bilreiro C, Barros M, Bahia C, Santiago I, Caseiro-Alves F (2019) All about portal vein: a pictorial display to anatomy, variants and physiopathology. Insights Imaging 10(1):38. https://doi.org/10.1186/s13244-019-0716-8. (PMID:30900187;PMCID:PMC6428891)
Guler N, Dayangac M, Yaprak O, Akyildiz M, Gunay Y, Taskesen F, Tabandeh B, Bulutcu F, Yuzer Y, Tokat Y (2013) Anatomical variations of donor portal vein in right lobe living donor liver transplantation: the safe use of variant portal veins. Transpl Int 26(12):1191–1197. https://doi.org/10.1111/tri.12190. (Epub 2013 Oct 15 PMID: 24252057)
Kuriyama N, Tanemura A, Hayasaki A, Fujii T, Iizawa Y, Kato H, Murata Y, Azumi Y, Kishiwada M, Mizuno S, Usui M, Sakurai H, Isaji S (2018) Feasibility and outcomes of direct dual portal vein anastomosis in living donor liver transplantation using the right liver graft with anatomic portal vein variations. Transplant Proc 50(9):2640–2644. https://doi.org/10.1016/j.transproceed.2018.03.053. (Epub 2018 Mar 15 PMID: 30401366)
Takeishi K, Shirabe K, Yoshida Y, Tsutsui Y, Kurihara T, Kimura K, Itoh S, Harimoto N, Yamashita YI, Ikegami T, Yoshizumi T, Nishie A, Maehara Y (2015) Correlation between portal vein anatomy and bile duct variation in 407 living liver donors. Am J Transplant 15(1):155–160. https://doi.org/10.1111/ajt.12965. (Epub 2014 Dec 17 PMID: 25521764)
Vargas PA, Khanmammadova N, Balci D, Goldaracena N (2023) Technical challenges in LDLT—overcoming small for size syndrome and venous outflow reconstruction. Transplant Rev 37(1):100750. https://doi.org/10.1016/j.trre.2023.100750. (Epub 2023 Feb 27. PMID: 36878038)
Naganathan S, Gupta S (2017) Hepatic venous outflow reconstruction in partial liver grafts: the middle path. Indian J Transplant 11(2):77–78. https://doi.org/10.4103/ijot.ijot_18_17
Har B, Balradja I, Sreejith S, Chikkala BR, Dey R, Acharya MR, Pandey Y, Agarwal S, Gupta S, Verma S (2021) The importance of Inferior Hepatic vein reconstruction in right lobe liver grafts: Does it really matter? J Liver Transplant 3:100025. https://doi.org/10.1016/j.liver.2021.100025
Taha AMI, Abdalla AM, Hassan RA, Elkhateb AI, Ali AM (2023) Outflow reconstruction in right lobe living donor liver transplant: middle hepatic vein reconstruction versus separate tributaries to inferior vena cava anastomosis. Exp Clin Transplant 21(3):245–250. https://doi.org/10.6002/ect.2022.0417. (PMID: 36987800)
Lee SH, Na GH, Choi HJ, Kim DG, You YK (2019) Impact of the reconstruction material on the patency of middle hepatic vein in living donor liver transplantation using the right liver. Transplant Proc 51(8):2745–2749. https://doi.org/10.1016/j.transproceed.2019.03.075. (PMID: 31563244)
Kim SH, Hwang S, Ha TY, Song GW, Jung DH, Ahn CS, Moon DB, Kim KH, Park GC, Lee SG (2016) Usability of cryopreserved aortic allografts for middle hepatic vein reconstruction during living-donor liver transplantation. J Gastrointest Surg 20(5):1049–1055. https://doi.org/10.1007/s11605-015-3048-0. (Epub 2015 Dec 14 PMID: 26666546)
Park GC, Hwang S, Ha TY, Song GW, Jung DH, Ahn CS, Moon DB, Kim KH, Yoon YI, Cho HD, Kwon JH, Chung YK, Kang SH, Jung IJ, Choi JU, Lee SG (2019) Hemashield vascular graft is a preferable prosthetic graft for middle hepatic vein reconstruction in living donor liver transplantation. Ann Transplant 17(24):639–646. https://doi.org/10.12659/AOT.919780. (PMID:31844037;PMCID:PMC6936210)
Jaganathan S, Ray B, Velaga J (2023) Our experience in tracking the tract: normal biliary anatomy and variants on magnetic resonance cholangiopancreatography in living donor liver transplantation. Cureus 15(2):e34695. https://doi.org/10.7759/cureus.34695. (PMID:36793499;PMCID:PMC9924704)
Lau NS, Ly M, Liu K, Majumdar A, McCaughan G, Crawford M, Pulitano C (2022) Current and potential applications for indocyanine green in liver transplantation. Transplantation 106(7):1339–1350. https://doi.org/10.1097/TP.0000000000004024. (Epub 2021 Dec 27 PMID: 34966106)
Kalayarasan R, Chandrasekar M, Sai Krishna P, Shanmugam D (2023) Indocyanine green fluorescence in gastrointestinal surgery: appraisal of current evidence. World J Gastrointest Surg 15(12):2693–2708. https://doi.org/10.4240/wjgs.v15.i12.2693. (PMID:38222003;PMCID:PMC10784830)
Mizuno S, Isaji S (2010) Indocyanine green (ICG) fluorescence imaging-guided cholangiography for donor hepatectomy in living donor liver transplantation. Am J Transplant 10(12):2725–2726. https://doi.org/10.1111/j.1600-6143.2010.03288.x. (Epub 2010 Nov 9 PMID: 21062417)
Mizuno S, Inoue H, Tanemura A, Murata Y, Kuriyama N, Azumi Y, Kishiwada M, Usui M, Sakurai H, Tabata M, Yamada R, Yamamoto N, Sugimoto K, Shiraki K, Takei Y, Isaji S (2014) Biliary complications in 108 consecutive recipients with duct-to-duct biliary reconstruction in living-donor liver transplantation. Transplant Proc 46(3):850–855. https://doi.org/10.1016/j.transproceed.2013.11.035. (PMID: 24767364)
Wang X, Teh CSC, Ishizawa T, Aoki T, Cavallucci D, Lee SY, Panganiban KM, Perini MV, Shah SR, Wang H, Xu Y, Suh KS, Kokudo N (2021) Consensus guidelines for the use of fluorescence imaging in hepatobiliary surgery. Ann Surg 274(1):97–106. https://doi.org/10.1097/SLA.0000000000004718. (PMID: 33351457)
Woo HY, Lee IS, Chang JH, Youn SB, Bae SH, Choi JY, Chun HJ, You YK, Kim DG, Yoon SK (2018) Outcome of donor biliary complications following living donor liver transplantation. Korean J Intern Med 33(4):705–715. https://doi.org/10.3904/kjim.2017.264. (Epub 2018 Mar 14. PMID: 29529841; PMCID: PMC6030404)
Simoes P, Kesar V, Ahmad J (2015) Spectrum of biliary complications following live donor liver transplantation. World J Hepatol 7(14):1856–1865. https://doi.org/10.4254/wjh.v7.i14.1856. (PMID:26207167;PMCID:PMC4506943)
Sapisochin G, Goldaracena N, Laurence JM, Levy GA, Grant DR, Cattral MS (2016) Right lobe living-donor hepatectomy-the Toronto approach, tips and tricks. Hepatobiliary Surg Nutr 5(2):118–126. https://doi.org/10.3978/j.issn.2304-3881.2015.07.03. (PMID:27115005;PMCID:PMC4824748)
Baker TB, Zimmerman MA, Goodrich NP, Samstein B, Pomfret EA, Pomposelli JJ, Gillespie BW, Berg CL, Emond JC, Merion RM (2017) Biliary reconstructive techniques and associated anatomic variants in adult living donor liver transplantations: the adult-to-adult living donor liver transplantation cohort study experience. Liver Transpl 23(12):1519–1530. https://doi.org/10.1002/lt.24872.PMID:28926171;PMCID:PMC5818204
Kim SH, Kim KH, Cho HD (2023) Donor safety of remnant liver volumes of less than 30% in living donor liver transplantation: a systematic review and meta-analysis. Clin Transplant 2:e15080. https://doi.org/10.1111/ctr.15080. (Epub ahead of print. PMID: 37529969)
Testa G, Nadalin S, Klair T, Florman S, Balci D, Frola C, Spiro M, Raptis DA, Selzner M, ERAS4OLT.org working group (2022) Optimal surgical workup to ensure safe recovery of the donor after living liver donation—a systematic review of the literature and expert panel recommendations. Clin Transplant 36(10):e14641. https://doi.org/10.1111/ctr.14641. (PMID: 35258132)
Kavur AE, Gezer NS, Barış M, Şahin Y, Özkan S, Baydar B, Yüksel U, Kılıkçıer Ç, Olut Ş, Bozdağı Akar G, Ünal G, Dicle O, Selver MA (2020) Comparison of semi-automatic and deep learning-based automatic methods for liver segmentation in living liver transplant donors. Diagn Interv Radiol 26(1):11–21. https://doi.org/10.5152/dir.2019.19025. (PMID:31904568;PMCID:PMC7075579)
Mohapatra N, Gurumoorthy Subramanya Bharathy K, Kumar Sinha P, Vasantrao Sasturkar S, Patidar Y, Pamecha V (2020) Three-dimensional volumetric assessment of graft volume in living donor liver transplantation: does it minimise errors of estimation? J Clin Exp Hepatol 10(1):1–8. https://doi.org/10.1016/j.jceh.2019.03.006. (Epub 2019 Mar 26. PMID: 32025161; PMCID: PMC6995882)
Balci D, Kirimker O, Kologlu M et al (2019) Validating a new software for 3D reconstruction and volumetric analysis in living donor liver transplantation. HPB 21(Suppl 2):S286. https://doi.org/10.1016/j.hpb.2019.10.1784
Balci D, Kirimker EO, Raptis DA, Gao Y, Kow AWC (2022) Uses of a dedicated 3D reconstruction software with augmented and mixed reality in planning and performing advanced liver surgery and living donor liver transplantation (with videos). Hepatobiliary Pancreat Dis Int 21(5):455–461. https://doi.org/10.1016/j.hbpd.2022.09.001. (Epub 2022 Sep 8 PMID: 36123242)
Michels NA (1966) Newer anatomy of the liver and its variant blood supply and collateral circulation. Am J Surg 112(3):337–347. https://doi.org/10.1016/0002-9610(66)90201-7. (PMID: 5917302)
Hiatt JR, Gabbay J, Busuttil RW (1994) Surgical anatomy of the hepatic arteries in 1000 cases. Ann Surg 220(1):50–52. https://doi.org/10.1097/00000658-199407000-00008. (PMID:8024358; PMCID:PMC1234286)
Cheng YF, Huang TL, Chen CL, Sheen-Chen SM, Lui CC, Chen TY, Lee TY (1997) Anatomic dissociation between the intrahepatic bile duct and portal vein: risk factors for left hepatectomy. World J Surg 21(3):297–300. https://doi.org/10.1007/s002689900232. (PMID: 9015174)
Covey AM, Brody LA, Getrajdman GI, Sofocleous CT, Brown KT (2004) Incidence, patterns, and clinical relevance of variant portal vein anatomy. AJR Am J Roentgenol 183(4):1055–1064. https://doi.org/10.2214/ajr.183.4.1831055. (PMID: 15385304)
Nakamura T, Tanaka K, Kiuchi T, Kasahara M, Oike F, Ueda M, Kaihara S, Egawa H, Ozden I, Kobayashi N, Uemoto S (2002) Anatomical variations and surgical strategies in right lobe living donor liver transplantation: lessons from 120 cases. Transplantation 73(12):1896–1903. https://doi.org/10.1097/00007890-200206270-00008. (PMID: 12131684)
Cheng YF, Huang TL, Chen CL, Chen TY, Huang CC, Ko SF, Lee TY (1996) Variations of the left and middle hepatic veins: application in living related hepatic transplantation. J Clin Ultrasound 24(1):11–16. https://doi.org/10.1002/jcu.1996.1870240103. (PMID: 8655660)
Radtke A, Schroeder T, Sotiropoulos GC, Molmenti E, Schenk A, Paul A, Nadalin S, Lang H, Saner F, Peitgen HO, Broelsch CE, Malagò M (2005) Anatomical and physiological classification of hepatic vein dominance applied to liver transplantation. Eur J Med Res 10(5):187–194 (PMID: 15946917)
De Cecchis L, Hribernik M, Ravnik D, Gadzijev EM (2000) Anatomical variations in the pattern of the right hepatic veins: possibilities for type classification. J Anat 197(Pt 3):487–93. https://doi.org/10.1046/j.1469-7580.2000.19730487.x. (PMID: 11117632; PMCID: PMC1468147)
Huang TL, Cheng YF, Chen CL, Chen TY, Lee TY (1996) Variants of the bile ducts: clinical application in the potential donor of living-related hepatic transplantation. Transplant Proc 28(3):1669–1670 (PMID: 8658831)
Ohkubo M, Nagino M, Kamiya J, Yuasa N, Oda K, Arai T, Nishio H, Nimura Y (2004) Surgical anatomy of the bile ducts at the hepatic hilum as applied to living donor liver transplantation. Ann Surg 239(1):82–86. https://doi.org/10.1097/01.sla.0000102934.93029.89. (PMID: 14685104; PMCID: PMC1356196)
Funding
None.
Author information
Authors and Affiliations
Contributions
NG, PV and LM participated in conception and design of the manuscript, writing of the paper, and drafting of the manuscript. PV participated in creation and design of included figures/illustrations. NG and LM participated in critical revision of the manuscript for important, intellectual content. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Declaration of Generative AI and AI-assisted technologies in the writing process
No Generative AI and AI-assisted technologies were used during the preparation of this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Goldaracena, N., Vargas, P.A. & McCormack, L. Pre-operative assessment of living liver donors’ liver anatomy and volumes. Updates Surg (2024). https://doi.org/10.1007/s13304-024-01806-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13304-024-01806-6