Abstract
People living with type 1 diabetes (T1D) have an increased risk of cardiovascular disease (CVD), and it is the leading cause of morbidity and mortality in this population. CVD risk increases with each uncontrolled risk factor, even in individuals with good glycaemic control. Recommendations for assessing CVD risk in the T1D population are extended from those for type 2 diabetes (T2D) even though the physiopathology and underlying mechanisms of atherosclerosis in T1D are poorly understood and differ from those in T2D. Unlike the assessment of microvascular complications, which is well established in T1D, this is far from being the case for the comorbidities and risk associated with CVD. Aside from classical cardiovascular comorbidities, carotid ultrasound can be useful to stratify CVD risk. The utilization of specific risk scales such as the Steno Type 1 Risk Engine can help to more accurately classify cardiovascular risk in these individuals. The cornerstones of the management of cardiovascular risk in T1D are the promotion of the Mediterranean diet, tight glycaemic control (glycated haemoglobin (HbA1c) < 7%), blood pressure < 130/80 mmHg in most patients, and low-density lipoprotein (LDL) cholesterol < 100 mg/dL in moderate-risk individuals, < 70 mg/dL in high-risk individuals, and < 55 mg/dL in very high-risk individuals. Conventional medical follow-up of patients with T1D should be individualized (approximately 2–3 visits per year), and a carotid ultrasound evaluation is recommended every 5 years in the absence of significant preclinical atherosclerosis or more often in those with severe preclinical atherosclerosis. Antithrombotic therapy is recommended in those receiving secondary prevention, those with stenosis > 50% in any arterial bed, and those with an impaired ankle-brachial index. This document is a proposal of a practical approach for the evaluation, classification, and management of CVD risk in individuals living with T1D.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
People living with type 1 diabetes (T1D) have an increased risk of cardiovascular disease (CVD), which is the leading cause of morbidity and mortality in this population. The risk increases with each uncontrolled risk factor. |
Most of the recommendations for assessing CVD risk in people living with T1D are extended from those related to T2D. Therefore, specific clinical recommendations are needed. |
This document is intended to be a proposal suggesting a practical approach for the evaluation, classification, and management of CVD risk in individuals living with T1D, considering the use of carotid ultrasound to guide treatment. |
Rationale: Importance of Cardiovascular Disease in Persons with Type 1 Diabetes
In people living with type 1 diabetes (T1D), cardiovascular disease (CVD) remains the leading cause of morbidity and mortality. The risk of CVD in this population is four- to eight-fold higher than in the general population and contributes to a shorter life expectancy (10–15 years) [1, 2]. Cardiovascular risk increases with each uncontrolled risk factor, even in individuals with good glycaemic control, underscoring the relevance of comprehensive CVD risk management in this population [3]. Classical non-specific and specific CVD risk factors coexist in T1D, contributing to the atherosclerotic process [4, 5]. Although some recommendations have been developed in this regard [6, 7], one of the main limitations of CVD prevention guidelines in T1D is that many of the recommendations are extended from those for type 2 diabetes (T2D), despite the physiopathology and underlying mechanisms of atherosclerosis in T1D remaining poorly understood and differing from those in T2D. In addition, unlike the assessment of microvascular complications, which is well established in T1D, the evaluation of the comorbidities and risk associated with CVD is far from routine in these subjects.
Considering all of the above, and within the context of a unit specialized in the care of people with diabetes in a tertiary hospital, we propose the following protocol for the evaluation, classification, and management of CVD risk in individuals living with T1D.
This article is based on previously conducted studies and does not contain any new studies with human participants performed by any of the authors.
Objective
The objective is to regularly assess and quantify the risk of CVD in individuals with T1D, thus allowing the personalization of the most timely (effective and safe) treatment and patient follow-up.
Cardiovascular Risk Assessment
Clinical Data and Physical Examination
The following demographic characteristics and clinical data are included in the assessment of cardiovascular risk: age, gender, date of T1D diagnosis, duration of T1D, diabetes treatment, and presence of acute and chronic diabetic complications (micro- and macrovascular). Regarding acute complications, a history of severe hypoglycaemia is checked for, and hypoglycaemia awareness is evaluated using the Clarke test [8]. Admissions for diabetic ketoacidosis are recorded. In relation to microvascular complications, diabetic kidney disease (DKD) is checked for based on the albumin-to-creatinine ratio (ACR) and estimated glomerular filtration rate (eGFR). An ACR ≥ 30 mg/g (confirmed in at least two of three consecutive determinations) and/or a persistent eGFR < 60 mL/min/1.73 m2 are considered to indicate DKD [9]. The fundus oculi is used for the diagnosis of diabetic retinopathy, which is always confirmed by an ophthalmologist. Autonomic neuropathy and peripheral neuropathy are recorded, as is the presence of diabetic foot disease. Macrovascular complications are considered if acute myocardial infarction, stable or unstable angina, stroke, heart failure, or peripheral vascular disease is presented.
Additionally, a family history of premature CVD (men < 55, women < 65 years old) [10] and dyslipidaemia is recorded. For women, pregnancy or a history of miscarriage and comorbidities, such as preeclampsia, eclampsia, and/or small-for-gestational-age newborns, is recorded [11].
The presence of cardiovascular risk factors and the treatments received are registered, as are smoking habit and alcohol consumption. Additionally, weekly physical activity levels are assessed, with individuals considered to be active if they are performing at least 3.5 h of physical activity per week. The result of the PREDIMED-PLUS questionnaire (17 points) to assess adherence to the energy-restricted Mediterranean diet is recorded [12,13,14].
Regarding the physical examination, the following variables should be included: weight, height, body mass index (BMI), and waist and hip circumferences. Blood pressure (BP) and heart rate should also be measured.
Laboratory Evaluation
Parameters including glucose, creatinine, eGFR (Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI)), complete blood count, liver profile, lipid profile (total cholesterol, low-density lipoprotein (LDL) cholesterol (LDL-C), high-density lipoprotein (HDL) cholesterol (HDL-C), triglycerides, apolipoprotein B, lipoprotein (a) (Lp(a))), thyroid-stimulating hormone, glycated haemoglobin (HbA1c), and ACR are collected.
Preclinical Atherosclerosis Evaluation (Vascular Ultrasound)
The identification of preclinical atherosclerosis using carotid ultrasound has been shown to be correlated with cardiovascular events in T2D [15,16,17]. In the general population, showing the ultrasound results to patients with preclinical atherosclerosis improves cardiovascular risk at 1 and [18] and 3 years of follow-up [19]. Moreover, the identification of carotid plaques by carotid ultrasound in T1D has caused clinicians to intensify cardioprotective treatment [20].
Carotid ultrasound is performed to check for the presence of plaque and assess the carotid intima-media thickness (C-IMT). A standardized protocol for image acquisition is used, as described elsewhere [21, 22].
The presence of carotid plaque is defined as focal echo structures that encroach into the arterial lumen with an IMT ≥ 1.5 mm or involve at least 50% of the surrounding IMT, as measured from the media–adventitia interface to the intima–lumen surface [23]. Data on the mean and maximum C-IMT values of the common carotid artery, bulb, and right and left internal carotid arteries as well as data on the presence of plaques (i.e. location and maximum height) are collected (see Fig. 1).
The following patients with T1D and no history of CVD are eligible for the assessment of preclinical atherosclerosis by carotid ultrasound:
-
1.
T1D patients with DKD, regardless of age
-
2.
T1D patients aged ≥ 40 years
-
3.
T1D patients aged < 40 years with > 10 years of T1D duration and any of the following:
-
(a)
Diabetic retinopathy
-
(b)
Premature cardiovascular disease in first-degree relatives (< 55 years old in men and < 65 years old in women)
-
(c)
Active smoking habit
-
(d)
Hypertension
-
(e)
Atherogenic dyslipidaemia (corresponding to triglycerides > 150 mg/dL and/or HDL-C < 45 mg/dL in women or < 40 mg/dL in men or to treatment with fibrates)
-
(f)
Moderate/severe hypercholesterolaemia defined as LDL-C > 160 mg/dL or treatment with statins/ezetimibe
-
(g)
History of severe hypoglycaemia (hypoglycaemia requiring the assistance of a third party) and/or hypoglycaemia unawareness (Clarke questionnaire > 3)
-
(h)
History of preeclampsia/eclampsia
-
(i)
Optional: CVD risk ≥ 15% at 10 years, as calculated using the Steno T1 Risk Engine (ST1RE) scale (https://steno.shinyapps.io/T1RiskEngine).
-
(a)
Indications for Additional Complementary Tests
According to the latest clinical guidelines [24, 25], systematic screening for silent ischaemic heart disease is not recommended as it does not improve the prognosis compared to the appropriate treatment of different cardiovascular risk factors.
However, in some selected patients with T1D, additional complementary explorations may be indicated to more accurately stratify cardiovascular risk.
Ambulatory Blood Pressure Monitoring
People living with T1D have a higher prevalence of hypertensive disorders [26]. Ambulatory blood pressure monitoring (ABPM) can be useful to assess CVD risk in these individuals. In this regard, elevated BP values assessed by ABPM (especially nocturnal values) have been associated with increased arterial stiffness [27, 28] and a higher incidence of microvascular complications [28,29,30,31] in T1D. Additionally, an elevated nighttime BP evaluated by ABPM may be associated with increased all-cause mortality [32, 33].
Therefore, based on a modification of the latest recommendations [34], ABPM is suggested in people living with T1D who have the following:
-
1.
Conditions with a high frequency of isolated clinical hypertension (white coat hypertension):
-
(a)
Grade 1 hypertension (systolic blood pressure (SBP) 140–159 mmHg and diastolic blood pressure (DBP) 90–99 mmHg) in the clinical setting
-
(b)
Marked elevation of BP in the clinical setting without target organ damage
-
(a)
-
2.
Conditions with a high frequency of masked hypertension:
-
(a)
Normal to high BP values in the clinical setting (SBP 130–139 and DBP 85–89 mmHg).
-
(b)
Normal BP values in the clinical setting, but there is target organ damage (ventricular hypertrophy, abnormal ACR, etc.) or a high cardiovascular risk
-
(a)
-
3.
A history of gestational hypertension, preeclampsia, or intrauterine growth restriction in previous pregnancies
-
4.
Symptomatology consistent with hypotension in patients treated for hypertension
-
5.
Treatment-resistant hypertension (defined as the use of three or more antihypertensive drugs)
-
6.
Very marked variability between different clinical BP measurements
-
7.
Situations in which identification of the nighttime BP value or the "non-dipper" pattern is particularly useful (i.e. a persistently elevated ACR despite treatment)
-
8.
Optional: evaluation of BP control in treated patients (this is especially valuable in those at very high cardiovascular risk).
Ankle-Brachial Index
The role of the ankle-brachial index (ABI) in reclassifying cardiovascular risk is uncertain [35]. In the context of patients with T1D, it could be considered as an initial step in the study of patients with symptoms of intermittent claudication. In fact, peripheral artery disease can be one of the first manifestations of atherosclerotic disease in this population [36]; hence, the latest guidelines recommend that it should be periodically evaluated [24]. An ABI ≤ 0.90 is considered abnormal and diagnostic of peripheral artery disease, and values > 1.40 suggest vascular calcification (associated with a higher risk of future CVD) [37]. In the latter situation, additional non-invasive studies are recommended (toe-brachial index or duplex ultrasonography) [38].
Classification of Patients According to Overall Cardiovascular Risk
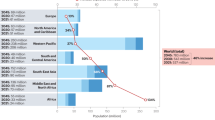
Population-based risk scales, even those specifically designed for patients with T2D, do not accurately estimate the risk of future cardiovascular disease in the population with T1D [39, 40]. In this regard, other tools, such as specific risk scales [6, 7] or the use of vascular ultrasound [41,42,43], may help to more accurately classify cardiovascular risk in these individuals. The following is a proposal for classifying the cardiovascular risk of patients with T1D (Fig. 2):
-
1.
Very high cardiovascular risk:
-
(a)
Patients with documented previous cardiovascular disease (coronary, cerebrovascular, peripheral vascular, heart failure, or aortic aneurysm)
-
(b)
T1D with established microvascular complications (diabetic retinopathy, kidney disease, or diabetic neuropathy (especially when cardiac autonomic manifestations are presented))*
-
(c)
T1D without microvascular complications but with three or more additional cardiovascular risk factors (active smoking habit, hypertension, baseline LDL-C > 160 mg/dL, obesity, high Lp(a) (> 50 mg/dL or > 125 nmol/L [44]), or a first-degree family history of premature CVD (< 55 in men, < 65 years old in women))*
-
(d)
Risk of fatal and non-fatal CVD ≥ 20% according to the ST1RE*
-
(e)
Advanced atherosclerosis on carotid ultrasound (defined as ≥ 50% stenosis, the presence of three or more plaques in both carotids, or the presence of a plaque at least 3 mm in height)
-
(a)
-
2.
High cardiovascular risk:
-
(a)
T1D with more than 10 years of duration, without microvascular complications, and with at least one additional cardiovascular risk factor (but always < 3)*
-
(b)
T1D onset at < 10 years of age and with > 20 years of diabetes duration*
-
(c)
Risk of fatal and non-fatal CVD is 10–20% according to the ST1RE*
-
(d)
Mild to moderate atherosclerosis on carotid ultrasound (defined as the presence of ≤ 2 plaques (without stenosis and with a height of < 3 mm)
-
(a)
-
3.
Moderate cardiovascular risk:
-
(a)
T1D individuals < 35 years of age, with < 10 years of disease duration, without microvascular complications or other cardiovascular risk factors, and without plaques on carotid ultrasound
-
(b)
Risk of fatal and non-fatal CVD is < 10% according to the ST1RE.
-
(a)
Risk categories and low-density-lipoprotein cholesterol goals according to carotid ultrasound results. CV cardiovascular, CVD cardiovascular disease, CVRF cardiovascular risk factors, DKD diabetic kidney disease, HbA1c glycated haemoglobin, HTN hypertension, LDL-C low-density-lipoprotein cholesterol, ST1RE Steno Type 1 Risk Engine, T1D type 1 diabetes, US ultrasound. ϮIn patients without documented cardiovascular disease and classified as being at high or very high risk according to clinical criteria or the Steno T1 Risk Engine (ST1RE), the absence of preclinical atherosclerosis (plaques) on vascular ultrasound decreases their estimated risk by one level (from very high to high or from high to moderate, respectively). *Defined as three or more plaques on carotid ultrasound, stenosis of at least 50%, or a plaque at least 3 mm in height. Also included in this category are patients with an ankle-brachial index (ABI) ≤ 0.9, those with coronary calcium > 300, or those with stenosis of at least 50% in another arterial bed, as evidenced by imaging tests. **Defined as two or fewer plaques in the carotid territory, with none being > 3 mm and without significant stenosis. ***Lipid-lowering drugs may not be necessary in patients with optimal glycaemic control (mean HbA1c ≤ 6.5%) and with an LDL-C of between 100 and 130 mg/dL
*In patients without documented CVD and who are classified as being at high or very high risk based on clinical criteria or the ST1RE, the absence of preclinical atherosclerosis (plaques) on vascular ultrasound would decrease their estimated risk by one level (from very high to high or from high to moderate, respectively).
Management of Cardiovascular Risk Factors
General Recommendations
Lifestyle changes are one of the cornerstones of treating people living with T1D and are the basis of CVD prevention. Individuals with T1D are increasingly found to be overweight or obese [45], and excess weight is associated with an increased risk of CVD [43, 46, 47]. Therefore, strategies for weight loss should be implemented in overweight or obese patients.
Undoubtedly, nutrition is a pivotal cornerstone in the management of these patients. Indeed, both the consumption of certain fats [48] and unhealthy eating patterns [49] have been associated with the development of chronic complications in T1D. In our setting, the Mediterranean diet is recommended, considering the evidence available for the general population [50] and in those with T1D [14]. Similarly, physical exercise should also be recommended as an effective measure for managing cardiovascular risk [51, 52].
Finally, owing to the close relationship between smoking and future CVD risk in patients with T1D [53], smoking cessation should be a primary goal in the prevention of CVD.
Glycaemic Control
People living with T1D should receive healthcare from a coordinated multidisciplinary team. Diabetes self-management education and support (DSMES) programmes are the cornerstone of treatment and have led to improvements in diabetes knowledge, healthy habits, glycaemic outcomes, and quality of life [54, 55]. These programmes focus on empowering patients with T1D by providing the necessary tools for decision-making related to self-care [56].
The patient should receive intensive treatment using multiple insulin doses (basal and bolus “prandial/correction” doses, including the use of connected “smartpens”) or continuous infusion devices (with a non-integrated continuous glucose sensor, integrated with some advanced functions, or in automatic insulin delivery system mode) [57].
Glycaemic Targets to Achieve Unless Contraindicated (Individualized)
-
HbA1c < 7% (6.5% in the absence of contraindications)
-
Recommended glycaemic goals according to the ambulatory glucose profile from continuous glucose monitoring (CGM): 70–180 mg/dL (within range) > 70% of the time; < 70 mg/dL (below range) < 4% of the time; < 54 mg/dL (below range) < 1% of the time; > 180 mg/dL (above range) < 25% of the time; and > 250 mg/dL (above range) < 5% of the time [58].
Lipid Control
According to the current consensus, the primary treatment goal for lipid control is LDL-C [24, 35, 59]. Although no studies have been specifically designed for the T1D population, previous meta-analyses [60] and population-based studies in patients with T1D [4, 61, 62] support LDL-C control as an effective measure to reduce the risk of cardiovascular events. Statins are generally the drugs of choice, but ezetimibe is especially indicated owing to increased markers of cholesterol absortion in this population [63, 64]. The use of bempedoic acid and proprotein convertase subtilisin/kexin type 9 inhibitors (PCSK9i) (both of which are monoclonal antibodies; examples include evolocumab, alirocumab, and small interfering RNA (inclisiran)) may be considered in selected patients in secondary prevention if treatment goals are not met [65].
The LDL-C goal is set and individualized based on the estimated risk of the patient, and it is adapted according to vascular ultrasound results (Fig. 2):
-
Very high risk:
-
General target: LDL-C < 55 mg/dL (especially in patients with previous CVD or a high atherosclerotic burden on vascular ultrasound)
-
A less strict goal of LDL-C < 70 mg/dL can be considered in subjects without CVD, without microvascular complications (especially DKD), and without a high atherosclerotic burden on vascular ultrasound (two or fewer plaques, no stenosis, or plaques > 3 mm)
-
-
High risk:
-
General target: LDL-C < 70 mg/dL (especially in individuals with evidence of mild/moderate preclinical atherosclerosis: two or fewer plaques, no stenosis, and plaques < 3 mm)
-
A less strict goal of LDL-C < 100 mg/dL can be considered in patients classified as high risk but without plaques on vascular ultrasound (especially in the absence of microvascular complications)
-
-
Moderate risk:
-
General target: LDL-C < 100 mg/dL; consider initiating lipid-lowering therapy in individuals with an elevated baseline LDL-C (> 160 mg/dL) or those with poor glycaemic control (HbA1c > 9%)
-
In patients < 30 years old who are classified as being at moderate risk (no plaques) and have LDL < 160 mg/dL, the initiation of lipid-lowering drugs can be postponed
-
In patients > 30–40 years old with LDL between 100 and 130 mg/dL, without plaques, and with good chronic glycaemic control (HbA1c ≤ 6.5%), initiation of lipid-lowering drugs can also be postponed.
-
In patients with triglycerides > 500 mg/dL despite lifestyle measures, the use of fibrates may be considered as a means to diminish the risk of pancreatitis. In those with contraindications for fibrates, moderate to high doses of omega-3 fatty acids (2–4 g/day) may be considered. The use of icosapent ethyl to reduce cardiovascular risk in this population has not been adequately studied.
Blood Pressure Control
The frequency of hypertension in young individuals with T1D is higher (4–7%) than that in the non-diabetic population (1–5%). Risk factors for hypertension in this population include obesity, autonomic dysfunction, and poor glycaemic control [66].
Blood pressure targets should be individualized [34]. We can consider the following objectives:
-
BP < 130/80 mmHg generally in all individuals with T1D
-
BP < 140/80 mmHg is recommended for individuals with T1D who are 65 to 79 years of age.
Angiotensin-converting-enzyme inhibitors (ACEi) or angiotensin receptor blockers (ARB) are suggested for the treatment of hypertension in individuals with coronary artery disease (CAD) or an ACR of 30–299 mg/g, and they are strongly recommended for individuals with an ACR ≥ 300 mg/g.
In individuals with an initial BP ≥ 150/90 mmHg, in addition to lifestyle therapy, prompt initiation and timely titration of two drugs or a single-pill combination of drugs is suggested (in the case of albuminuria or CAD, a combination of ACEi or ARB with a diuretic or calcium channel blocker is recommended). The combination of ACEi and ARB is contraindicated. In the case where the BP target is not met, an agent from a complementary antihypertensive drug class should be added. Finally, in cases presenting adverse effects or uncontrolled BP levels with the combination of three agents, the addition of a mineralocorticoid receptor antagonist can be considered [25].
According to the latest European guidelines [34, 35], if ABPM has been performed, the BP goals would be:
-
24-h assessment: < 130/80 mmHg
-
Daytime period: < 135/85 mmHg
-
Nighttime period: < 120/70 mmHg.
Antithrombotic Therapy
To date, there is no solid evidence supporting the systematic use of antiplatelets in primary prevention in individuals living with T1D. According to the last recommendations [24, 25, 35, 59], antiplatelets (aspirin 75–100 mg/day or clopidogrel 75 mg/day if aspirin is contraindicated) are advised in the following scenarios:
-
1.
Patients with previous atherosclerotic CVD (CAD, cerebrovascular disease, or peripheral artery disease)
-
2.
Patients with at least 50% stenosis in any arterial bed (carotid arteries, coronary arteries, or arteries of the lower extremities), as evidenced by imaging
-
3.
Patients with an ABI ≤ 0.9, especially in those with symptoms of intermittent claudication.
With a lower level of scientific evidence, antiplatelets could be considered in:
-
1.
Patients without CVD, but with a high atherosclerotic burden evidenced by imaging studies (e.g. three or more plaques in carotid territory or any plaque ≥ 3 mm), without significant stenosis (< 50%), and with clinical factors associated with extreme risk:
-
(a)
DKD with eGFR < 30 ml/min
-
(b)
DKD with eGFR < 60 ml/min and ACR ≥ 300 mg/g
-
(c)
Presence of three or more combined microvascular complications.
-
(a)
Patient Follow-Up
Medical Follow-Up
The conventional medical follow-up of patients with T1D requires approximately 2–3 visits per year, although this should be individualized. During follow-up visits, the following parameters should be evaluated:
-
Annually:
-
BP evaluation or ABPM as per clinical judgement
-
Weight and BMI assessment
-
Evaluation of insulin injection sites
-
History of smoking cessation or recommendations regarding smoking cessation
-
Assessment of hypoglycaemia awareness (Clarke test) in patients with preserved awareness; evaluation of the frequency of severe and non-severe hypoglycaemia episodes
-
Laboratory tests: liver function, basic urine profile, ACR, and complete blood count.
-
-
Biannually/three times a year (individualized):
-
Laboratory tests, including renal function (creatinine and eGFR), glucose, HbA1c, total cholesterol/triglycerides, and LDL-C and HDL-C
-
Assessment of general treatment adherence (nutritional recommendations, insulin dosing, antihypertensive drugs, statins, etc.)
-
Evaluation of glycaemic control with CGM [58]
-
Assessment of hypoglycaemia awareness (Clarke test) in patients with hypoglycaemia unawareness or in specific programmes aimed at improving hypoglycaemia awareness; evaluation of the frequency of severe and non-severe hypoglycaemia episodes in patients at high risk of hypoglycaemia.
-
Frequency of Preclinical Atherosclerosis Evaluation
Re-evaluation every 5 years is recommended in the absence of data suggestive of preclinical atherosclerosis or if there is non-severe preclinical atherosclerosis (two or fewer plaques < 3 mm and no significant stenosis).
Re-evaluation every 3 years is recommended in the presence of findings indicating severe preclinical atherosclerosis (three or more plaques or one plaque of at least 3 mm).
Annual examination is suggested in patients with significant stenosis (≥ 50%). If the stenosis remains stable, then evaluation can be performed every 2 years and subsequently every 2–3 years.
Conclusions
People living with T1D have an increased risk of CVD; however, most of the recommendations for cardioprotective measures and care have been based on other populations, such as people living with T2D. In this practical approach proposal, we highlight the key points for cardiovascular prevention specifically for individuals living with T1D. In addition to promoting a healthy lifestyle, including the Mediterranean diet, the cornerstones for reducing CVD burden include smoking cessation, BP control at < 130/80 mmHg, and the maintenance of optimal glycaemic control. We propose the use of the ST1RE scale and an evaluation of the presence of carotid plaques to tailor the targeting of LDL-C levels in each patient. Periodic personalized evaluation and control of each risk factor is recommended. The intention of our proposal for the management and follow-up of cardiovascular risk in patients living with T1D is to facilitate positive changes in the cardiovascular risk of this population.
References
Rawshani A, Rawshani A, Franzén S, Eliasson B, Svensson A-M, Miftaraj M, et al. Mortality and cardiovascular disease in type 1 and type 2 diabetes. N Engl J Med. 2017;376:1407–18.
Livingstone SJ, Levin D, Looker HC, Lindsay RS, Wild SH, Joss N, et al. Estimated life expectancy in a Scottish cohort with type 1 diabetes, 2008–2010. JAMA. 2015;313:37.
Rawshani A, Rawshani A, Franzén S, Eliasson B, Svensson A-M, Miftaraj M, et al. Range of risk factor levels. Circulation. 2017;135:1522–31.
Rawshani A, Rawshani A, Sattar N, Franzén S, Mcguire DK, Eliasson B, et al. Relative prognostic importance and optimal levels of risk factors for mortality and cardiovascular outcomes in type 1 diabetes mellitus. Circulation. 2019;139:1900–12.
Bebu I, Braffett BH, Orchard TJ, Lorenzi GM, Lachin JM. Mediation of the effect of glycemia on the risk of CVD outcomes in type 1 diabetes: the DCCT/EDIC study. Diabetes Care. 2019;42:1284–9.
Vistisen D, Andersen GS, Hansen CS, Hulman A, Henriksen JE, Bech-Nielsen H, et al. Prediction of first cardiovascular disease event in type 1 diabetes mellitus. Circulation. 2016;133:1058–66.
McGurnaghan SJ, McKeigue PM, Read SH, Franzen S, Svensson A-M, Colombo M, et al. Development and validation of a cardiovascular risk prediction model in type 1 diabetes. Diabetologia. 2021;64:2001–11.
Jansa M, Quirós C, Giménez M, Vidal M, Galindo M, Conget I. Psychometric analysis of the Spanish and Catalan versions of a questionnaire for hypoglycemia awareness. Med Clín Engl Ed. 2015;144:440–4.
de Boer IH, Khunti K, Sadusky T, Tuttle KR, Neumiller JJ, Rhee CM, et al. Diabetes management in chronic kidney disease: a consensus report by the American Diabetes Association (ADA) and kidney disease: improving global outcomes (KDIGO). Diabetes Care. 2022;45:3075–90.
Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2016;37:2315–81.
Amor AJ, Vinagre I, Valverde M, Pané A, Urquizu X, Meler E, et al. Preeclampsia is associated with increased preclinical carotid atherosclerosis in women with type 1 diabetes. J Clin Endocrinol Metab. 2020;105:85–95.
Martínez-González MA, Buil-Cosiales P, Corella D, Bulló M, Fitó M, Vioque J, et al. Cohort profile: design and methods of the PREDIMED-Plus randomized trial. Int J Epidemiol. 2019;48:387–388o.
Schröder H, Zomeño MD, Martínez-González MA, Salas-Salvadó J, Corella D, Vioque J, et al. Validity of the energy-restricted Mediterranean diet adherence screener. Clin Nutr. 2021;40:4971–9.
Serés-Noriega T, Viñals C, Perea V, Mesa A, Boswell L, Mariaca K, et al. Adherence to an energy-restricted Mediterranean diet is associated with the presence and burden of carotid atherosclerosis in people with type 1 diabetes. Diabetes Metab Res Rev. 2024;40(3): e3783.
Baber U, Mehran R, Sartori S, Schoos MM, Sillesen H, Muntendam P, et al. Prevalence, impact, and predictive value of detecting subclinical coronary and carotid atherosclerosis in asymptomatic adults: the bioimage study. J Am Coll Cardiol. 2015;65:1065–74.
Vigili de Kreutzenberg S, Fadini GP, Guzzinati S, Mazzucato M, Volpi A, Coracina A, et al. Carotid plaque calcification predicts future cardiovascular events in type 2 diabetes. Diabetes Care. 2015;38:1937–44.
Polak JF, Pencina MJ, Pencina KM, O’Donnell CJ, Wolf PA, D’Agostino RB. Carotid-wall intima-media thickness and cardiovascular events. N Engl J Med. 2011;365:213–21.
Näslund U, Ng N, Lundgren A, Fhärm E, Grönlund C, Johansson H, et al. Visualization of asymptomatic atherosclerotic disease for optimum cardiovascular prevention (VIPVIZA): a pragmatic, open-label, randomised controlled trial. Lancet. 2019;393:133–42.
Bengtsson A, Norberg M, Ng N, Carlberg B, Grönlund C, Hultdin J, et al. The beneficial effect over 3 years by pictorial information to patients and their physician about subclinical atherosclerosis and cardiovascular risk: results from the VIPVIZA randomized clinical trial. Am J Prev Cardiol. 2021;7: 100199.
Boswell L, Serés-Noriega T, Mesa A, Perea V, Pané A, Viñals C, et al. Carotid ultrasonography as a strategy to optimize cardiovascular risk management in type 1 diabetes: a cohort study. Acta Diabetol. 2022;59(12):1563–74.
Amor AJ, Ortega E, Perea V, Cofán M, Sala-Vila A, Nuñez I, et al. Relationship between total serum bilirubin levels and carotid and femoral atherosclerosis in familial dyslipidemia. Arterioscler Thromb Vasc Biol. 2017;37:2356–63.
Junyent M, Cofán M, Núñez I, Gilabert R, Zambón D, Ros E. Influence of HDL cholesterol on preclinical carotid atherosclerosis in familial hypercholesterolemia. Arterioscler Thromb Vasc Biol. 2006;26:1107–13.
Touboul P-J, Hennerici MG, Meairs S, Adams H, Amarenco P, Bornstein N, et al. Mannheim carotid intima-media thickness and plaque consensus (2004–2006–2011). Cerebrovasc Dis. 2012;34:290–6.
Marx N, Federici M, Schütt K, Müller-Wieland D, Ajjan RA, Antunes MJ, et al. 2023 ESC guidelines for the management of cardiovascular disease in patients with diabetes. Eur Heart J. 2023;44:4043–140.
ElSayed NA, Aleppo G, Bannuru RR, Bruemmer D, Collins BS, Das SR, et al. 10. Cardiovascular disease and risk management: standards of care in diabetes—2024. Diabetes Care. 2024;47:S179-218.
Lithovius R, Groop P-H. The many faces of hypertension in individuals with type 1 diabetes. Diabetes Res Clin Pract. 2023;197: 110564.
Lithovius R, Gordin D, Forsblom C, Saraheimo M, Harjutsalo V, Groop P-H. Ambulatory blood pressure and arterial stiffness in individuals with type 1 diabetes. Diabetologia. 2018;61:1935–45.
Gourgari E, Mete M, Dimatulac M, Cogen F, Brady T. Blood pressure during sleep is associated with arterial stiffness and urine microalbumin to creatinine ratio in youth with type 1 diabetes. J Diabetes Complic. 2020;34: 107678.
Rodrigues TC, Canani LH, Viatroski RS, Hoffmann LH, Esteves JF, Gross JL. Masked hypertension, nocturnal blood pressure and retinopathy in normotensive patients with type 1 diabetes. Diabetes Res Clin Pract. 2010;87:240–5.
Mateo-Gavira I, Vílchez-López FJ, García-Palacios MV, Carral-San Laureano F, Jiménez-Carmona S, Aguilar-Diosdado M. Nocturnal blood pressure is associated with the progression of microvascular complications and hypertension in patients with type 1 diabetes mellitus. J Diabetes Complic. 2016;30:1326–32.
Jorge da Silva Franco R, Antonio Vieira Filho J, Inomata Cardoso da Silva D, Cuadrado Martin L, Alves Silva B, Garcia Zanati Bazan S, et al. Non-dipping circadian pattern as a predictor of incipient nephropathy in normotensive normoalbuminuric type 1 diabetics. Chronobiol Int. 2023;40:1523–8.
Chiriacò M, Sacchetta L, Forotti G, Leonetti S, Nesti L, Taddei S, et al. Prognostic value of 24-hour ambulatory blood pressure patterns in diabetes: a 21-year longitudinal study. Diabetes Obes Metab. 2022;24:2127–37.
Hjortkjær HØ, Persson F, Theilade S, Winther SA, Tofte N, Ahluwalia TS, et al. Non-dipping and higher nocturnal blood pressure are associated with risk of mortality and development of kidney disease in type 1 diabetes. J Diabetes Complic. 2022;36: 108270.
Mancia G, Kreutz R, Brunström M, Burnier M, Grassi G, Januszewicz A, et al. 2023 ESH guidelines for the management of arterial hypertension The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension. J Hypertens. 2023;41:1874–2071.
Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42:3227–337.
Giménez-Pérez G, Viñals C, Mata-Cases M, Vlacho B, Real J, Franch-Nadal J, et al. Epidemiology of the first-ever cardiovascular event in people with type 1 diabetes: a retrospective cohort population-based study in Catalonia. Cardiovasc Diabetol. 2023;22:179.
Aboyans V, Criqui MH, Abraham P, Allison MA, Creager MA, Diehm C, et al. Measurement and Interpretation of the Ankle–Brachial index. Circulation. 2012;126:2890–909.
Aboyans V, Ricco J-B, Bartelink M-LEL, Björck M, Brodmann M, Cohnert T, et al. ESC guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European Society for Vascular Surgery (ESVS). Eur Heart J. 2017;2018(39):763–816.
Pesantez M, Ebekozien O, Vendrame F. Type 1 diabetes and cardiovascular health. Endocrinol Metab Clin N Am. 2024;53:151–63.
Zgibor JC, Piatt GA, Ruppert K, Orchard TJ, Roberts MS. Deficiencies of cardiovascular risk prediction models for type 1 diabetes. Diabetes Care. 2006;29:1860–5.
Viñals C, Conget I, Pané A, Boswell L, Perea V, Blanco AJ, et al. Steno type 1 risk engine and preclinical atherosclerosis in Mediterranean individuals with type 1 diabetes. Diabetes Metab Res Rev. 2020;36: e3320.
Serés-Noriega T, Giménez M, Perea V, Boswell L, Viñals C, Blanco J, et al. Use of the steno T1 risk engine identifies preclinical atherosclerosis better than use of ESC/EASD-2019 in adult subjects with type 1 diabetes at high risk. Diabetes Care. 2022;45(10):2412–21.
Pané A, Conget I, Boswell L, Ruiz S, Viñals C, Perea V, et al. Insulin resistance is associated with preclinical carotid atherosclerosis in patients with type 1 diabetes. Diabetes Metab Res Rev. 2020;36:1–11.
Kronenberg F, Mora S, Stroes ESG, Ference BA, Arsenault BJ, Berglund L, et al. Lipoprotein(a) in atherosclerotic cardiovascular disease and aortic stenosis: a European Atherosclerosis Society consensus statement. Eur Heart J. 2022;43:3925–46.
Van Der Schueren B, Ellis D, Faradji RN, Al-Ozairi E, Rosen J, Mathieu C. Obesity in people living with type 1 diabetes. Lancet Diabetes Endocrinol. 2021;9(11):776–85.
Nyström T, Holzmann MJ, Eliasson B, Svensson AM, Sartipy U. Estimated glucose disposal rate predicts mortality in adults with type 1 diabetes. Diabetes Obes Metab. 2018;20:556–63.
Dahlström EH, Dahlström D, Sandholm N, Forsblom CM, Thorn LM, Jansson FJ, et al. Body mass index and mortality in individuals with type 1 diabetes on behalf of the FinnDiane Study Group. J Clin Endocrinol Metab. 2019;104:5195–204.
Mesa A, Cofán M, Esmatjes E, Perea V, Boswell L, Giménez M, et al. Biomarkers of fatty acid intake are independently associated with preclinical atherosclerosis in individuals with type 1 diabetes. Eur J Nutr. 2021;60:4595–605.
Granado-Casas M, Ramírez-Morros A, Martín M, Real J, Alonso N, Valldeperas X, et al. Type 1 diabetic subjects with diabetic retinopathy show an unfavorable pattern of fat intake. Nutrients. 2018;10(9):1184.
Estruch R, Ros E, Salas-Salvadó J, Covas M-I, Corella D, Arós F, et al. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med. 2018;378: e34.
Tikkanen-Dolenc H, Wadén J, Forsblom C, Harjutsalo V, Thorn LM, Saraheimo M, et al. Frequent and intensive physical activity reduces risk of cardiovascular events in type 1 diabetes. Diabetologia. 2017;60:574–80.
Tikkanen-Dolenc H, Wadén J, Forsblom C, Harjutsalo V, Thorn LM, Saraheimo M, et al. Physical activity reduces risk of premature mortality in patients with type 1 diabetes with and without kidney disease. Diabetes Care. 2017;40:1727–32.
Feodoroff M, Harjutsalo V, Forsblom C, Groop P-H. Dose-dependent effect of smoking on risk of coronary heart disease, heart failure and stroke in individuals with type 1 diabetes. Diabetologia. 2018;61:2580–9.
Haas L, Maryniuk M, Beck J, Cox CE, Duker P, Edwards L, et al. National standards for diabetes self-management education and support. Diabetes Care. 2014;37:S144–53.
Cooke D, Bond R, Lawton J, Rankin D, Heller S, Clark M, et al. Structured type 1 diabetes education delivered within routine care: impact on glycemic control and diabetes-specific quality of life. Diabetes Care. 2013;36:270–2.
Holt RIG, DeVries JH, Hess-Fischl A, Hirsch IB, Kirkman MS, Klupa T, et al. The management of type 1 diabetes in adults. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2021;64:2609–52.
ElSayed NA, Aleppo G, Bannuru RR, Bruemmer D, Collins BS, Ekhlaspour L, et al. 7. Diabetes technology: standards of care in diabetes—2024. Diabetes Care. 2024;47:S126–44.
ElSayed NA, Aleppo G, Bannuru RR, Bruemmer D, Collins BS, Ekhlaspour L, et al. 6. Glycemic goals and hypoglycemia: standards of care in diabetes—2024. Diabetes Care. 2024;47:S111–25.
Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41:255–323.
Downs JR, Gotto A, Clearfield M, Holdaas H, Gordon D, Davis B, et al. Efficacy of cholesterol-lowering therapy in 18 686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet. 2008;371:117–25.
Hero C, Rawshani A, Svensson A-M, Franzén S, Eliasson B, Eeg-Olofsson K, et al. Association between use of lipid-lowering therapy and cardiovascular diseases and death in individuals with type 1 diabetes. Diabetes Care. 2016;39:996–1003.
Hero C, Karlsson SA, Franzén S, Svensson A-M, Miftaraj M, Gudbjörnsdottir S, et al. Adherence to lipid-lowering therapy and risk for cardiovascular disease and death in type 1 diabetes mellitus: a population-based study from the Swedish National Diabetes Register. BMJ Open Diab Res Care. 2020;8:719.
Semova I, Levenson AE, Krawczyk J, Bullock K, Williams KA, Paul Wadwa R, et al. Type 1 diabetes is associated with an increase in cholesterol absorption markers but a decrease in cholesterol synthesis markers in a young adult population. J Clin Lipidol. 2019;13:940–6.
Ciriacks K, Coly G, Krishnaswami S, Patel SB, Kidambi S. Effects of simvastatin and ezetimibe in lowering low-density lipoprotein cholesterol in subjects with type 1 and type 2 diabetes mellitus. Metab Syndr Relat Disord. 2015;13:84–90.
Chait A, Eckel RH, Vrablik M, Zambon A. Lipid-lowering in diabetes: an update. Atherosclerosis. 2023;394:117313.
Bjornstad P, Donaghue KC, Maahs DM. Macrovascular disease and risk factors in youth with type 1 diabetes: time to be more attentive to treatment? Lancet Diabetes Endocrinol. 2018;6:809–20.
Medical Writing/Editorial Assistance
We thank Donna Pringle for language assistance.
Funding
No funding or sponsorship was received for this study or the publication of this article.
Author information
Authors and Affiliations
Contributions
All authors (Clara Viñals, Ignacio Conget, Montse Granados, Marga Giménez, and Antonio J. Amor) were involved in the design of the content and the writing and drafting of the article, and they approved the article submitted.
Corresponding authors
Ethics declarations
Conflict of Interest
Clara Viñals, Ignacio Conget, Montse Granados, and Marga Giménez have nothing to disclose. Antonio J. Amor is a member of the Editorial Board of Diabetes Therapy. Antonio J. Amor was not involved in the selection of peer reviewers for the manuscript or any of the subsequent editorial decisions.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Viñals, C., Conget, I., Granados, M. et al. Evaluation of Cardiovascular Risk in People with Type 1 Diabetes: A Comprehensive and Specific Proposed Practical Approach. Diabetes Ther (2024). https://doi.org/10.1007/s13300-024-01616-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13300-024-01616-4