Abstract
Introduction
The effects of switching DPP-4 inhibitors in type 2 diabetes mellitus (T2DM) patients are being widely studied. However, information of which factors affect the therapeutic response is limited. We evaluated the difference in HbA1c lowering effect by comorbidity and other variables after switching to anagliptin in patients with T2DM inadequately controlled by other DPP-4 inhibitors.
Methods
In a multicenter, open-label, single-arm, prospective observational study, patients with T2DM, HbA1c ≥ 7.0% who have taken DPP-4 inhibitors other than anagliptin, either alone or in combination (DPP-4 inhibitors + metformin/sulfonylurea (SU)/thiazolidinedione (TZD)/insulin), for at least 8 weeks were enrolled. After the switch to anagliptin, HbA1c and available clinical characteristics were determined.
Results
The change in HbA1c levels from baseline to week 12 and 24 was − 0.40% and − 0.42% in all patients. However, comparing the subgroups without and with comorbidities, the change in HbA1c levels at weeks 12 and 24 was − 0.68% and − 0.89% vs. − 0.27% and 0.22%, respectively. In addition, the proportion of patients achieving HbA1c < 7% from baseline to week 12 and 24 was increased to 70% and 70% vs. 20% and 24%, respectively. Duration of T2DM and different subtype classes of DPP-4 inhibitor did not significantly contribute to the change in HbA1c.
Conclusion
In patients with T2DM poorly controlled by other DPP-4 inhibitors, HbA1c levels were significantly decreased after switching to anagliptin. Given that the change in HbA1c was greater in patients without comorbidities than in patients with comorbidities, switching to anagliptin before adding other oral hypoglycemic agents (OHAs) may be an option in patients without comorbidities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Glycemic control depends on the types and doses of hypoglycemic agents, but reports suggest that other factors such as baseline HbA1c, age, duration of T2DM, and comorbidities may also play a role. |
Previous switching studies have shown the additional blood glucose control effect, and yet it is still unclear which factors affect the change in glycemic control. |
Therefore, we assessed the factors that can predict therapeutic response when switching from previous DPP-4 inhibitors to anagliptin in T2DM patients who had not responded well to other DPP-4 inhibitors. |
What was learned from the study? |
By switching from other DPP-4 inhibitors to anagliptin, patients without comorbidities had lower HbA1c levels than patients with comorbidities. |
This finding suggests that switching to anagliptin may be an option for patients with diabetes mellitus who do not respond to DPP-4 inhibitors and have no comorbidities. |
Introduction
Type 2 diabetes mellitus (T2DM) is a chronic, progressive disease, and long-term diabetic patients often require multiple combinations of oral hypoglycemic agents (OHAs) since glucose control cannot be managed properly along the duration of the disease [1, 2]. The American Diabetes Association (ADA), European Association for the Study of Diabetes (EASD) and Korean Diabetes Association (KDA) guidelines for T2DM recommend metformin as first-line therapy. However, if the glycemic target is not met with metformin alone, adjunctive treatment with various OHAs is recommended [3, 4].
Dipeptidyl peptidase-4 (DPP-4) inhibitors are suggested as second- or third-line therapy for patients on first-line metformin treatment [3, 4] because of their high efficacy, low risk of hypoglycemia, and neutral effect on body weight [5,6,7,8,9,10,11]. In addition, DPP-4 inhibitors have shown greater glucose-lowering efficacy, particularly in Asians. Meta-analysis of many clinical studies has demonstrated that DPP-4 inhibitors are more likely to decrease HbA1c in Asian patients, favoring DPP-4 inhibitors; thus, these drugs are among those most commonly prescribed [12].
Anagliptin is a novel selective DPP-4 inhibitor that improves glycemic control by increasing insulin secretion via incretin stimulation and suppressing excessive glucagon secretion [13]. Because of its short half-life, anagliptin should be taken twice daily [14]. Therefore, it increases GLP-1 levels by more than twofold while decreasing DPP-4 enzymatic activity by > 80% [13]. Several clinical studies have shown that anagliptin has the same blood glucose-lowering effectiveness and safety as other DPP-4 inhibitors. In addition, unlike traditional DPP-4 inhibitors, anagliptin may be effective in patients with high BMI [15, 16].
Glycemic control depends on the types and doses of hypoglycemic agents, but previous reports suggest that other factors such as baseline HbA1c, age, duration of T2DM, and comorbidities may also contribute [17,18,19,20,21]. Considering the addition of DPP-4 inhibitors for blood glucose control, real-world [22] and other studies have reported that switching treatment between DPP-4 inhibitors without additional hypoglycemic agents is also effective [23,24,25,26,27,28]. Although many switching studies have shown the efficacy of DPP-4 inhibitors, it is still unclear which factor affects the change in therapeutic response. Therefore, this study assessed the therapeutic effects of switching from other DPP-4 inhibitors to anagliptin in T2DM patients with inadequate glycemic control.
Methods
Participants
The inclusion criteria were as follows: (1) age ≥ 19 years; (2) type 2 diabetes mellitus with a HbA1c ≥ 7.0%; (3) received DPP-4 inhibitors other than anagliptin, either alone or in combination [DPP-4 inhibitors + metformin/sulfonylurea (SU)/thiazolidinedione (TZD)/insulin], for at least 8 weeks. The exclusion criteria were as follows: (1) patients who were given anagliptin before registration; (2) any patient considered ineligible for this study by the investigator. All patients provided informed consent before participating in this study. This study was conducted in compliance with the Declaration of Helsinki and the protocol approved by each institutional or central Institutional Review Board (IRB) including the Catholic University of Korea Bucheon St. Mary's Hospital IRB (no. HC17OODI0113, etc.). The details of ethics committees of participating centers are provided in Supplementary Table S6.
Study Design
This was an open-label, single-arm, multicenter prospective observational study in patients with T2DM. The study was conducted between July 1, 2017, and March 31, 2022 (registered on theClinicalTrials.gov: NCT04267601). Subjects visited the study site at baseline to measure HbA1c and other clinical parameters such as body weight, estimated glomerular filtration rate (eGFR), aspartate aminotransferase (AST), and alanine aminotransferase (ALT). After baseline, data were collected, and the previously taken DPP-4 inhibitors were switched to anagliptin for the following 24 weeks. HbA1c and other clinical parameters were measured in subjects at weeks 12 and 24. Baseline concomitant antidiabetic regimens (such as metformin, TZD, insulin, SU, and others) were maintained throughout the study.
The main objective of this study was to evaluate therapeutic responses in T2DM patients after switching from other DPP-4 inhibitors to anagliptin. The primary endpoint was to investigate the change in HbA1c according to switching among DPP-4 inhibitors.
Subgroup Analysis
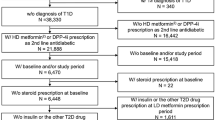
Overall, 1119 patients with HbA1c ≥ 7% were analyzed by DPP-4 binding pattern, maximum serum concentration (Cmax) of DPP-4 inhibitors, comorbidities, and T2DM duration subgroups to evaluate the factors influencing therapeutic response (Fig. 1); 223 patients had partially missing data and therefore were eliminated.
DPP-4 has a wide substrate binding pocket composed of four subsites (S1, S1′, S2, S2′, and S2 extensive), and current inhibitors bind to DPP-4 by fitting into multiple subsites. In particular, Class I inhibitors (saxagliptin and vildagliptin) bind to the S1 and S2 subsites, the core of the binding and central scaffolds of all Class I, II, and III inhibitors. Class II inhibitors (alogliptin and linagliptin) bind to S1, S2, S1′, and S2′ pockets. Lastly, Class III inhibitors (anagliptin, evogliptin, gemigliptin, sitagliptin, teneligliptin) bind to S1, S2, and S2 extensive pockets [29]. To determine the association between pharmacokinetic and pharmacodynamic parameters, correlation analysis was conducted between changes of HbA1c according to switching from DPP-4 inhibitors to anagliptin and Cmax of each DPP-4 inhibitor.
Comorbidities among patients in this study include the following types: dyslipidemia, hypertension, angina, diabetic retinopathy, and atherosclerosis. Only ≥ 5% reported comorbidities among the study patients were analyzed. When categorized by comorbidities, there were 322 patients without comorbidities and 797 with comorbidities.
The duration of T2DM was then classified into < 5 years, 5–10 years, and < 10 years (Supplementary Figure S1). When the duration of T2DM was further classified into each group, there were 153 patients with < 5-year duration of T2DM, 51 patients with 5–10-year duration of T2DM, and 31 patients with ≥ 10-year duration of T2DM among patients without comorbidities and 128 patients with < 5-year duration of T2DM, 178 patients with 5–10-year duration of T2DM, and 355 patients with ≥ 10-year duration of T2DM among patients with comorbidities.
Statistical Analysis
All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA). Continuous variables were described using descriptive statistics [mean ± standard deviation (SD)], and categorical variables were presented as counts (percentages). A p value < 0.05 was considered statistically significant.
Results
Patient Disposition and Demographics
Table 1 shows the baseline characteristics of 1119 patients with T2DM showing HbA1c ≥ 7% despite treatment with DPP-4 inhibitors. The DPP-4 inhibitors in the previous therapy, including saxagliptin, vildagliptin, alogliptin, linagliptin, evogliptin, gemigliptin, sitagliptin, and teneligliptin, were switched to anagliptin. Then, using comorbidities such as dyslipidemia, hypertension, angina, diabetic retinopathy, and atherosclerosis as subgroup classification, the baseline characteristics that showed a significant difference between the without comorbidities group and the with comorbidities group were the duration of T2DM (4.0 vs. 11.4 years, p < 0.001) and the frequency of concomitant medications. The proportion of patients using concomitant medications was higher in the with comorbidities group.
Efficacy
The overall change in HbA1c was − 0.40% at week 12 and − 0.42% at week 24, indicating a significant reduction from baseline (p < 0.05) (Fig. 2, Supplementary Table S1). We analyzed HbA1c decreasing effect in patients with baseline HbA1c values based on 8%, and both groups with baseline HbA1c of < 8 and ≥ 8% showed significant reduction. These were greater in patients with baseline HbA1c ≥ 8% (− 0.69% at week 12, − 0.73% at week 24) compared to < 8% (− 0.24% at week 12, − 0.24% at week 24) (Supplementary Table S2). We also evaluated the change in HbA1c after switching to anagliptin from other DPP-4 inhibitors according to DPP-4 binding patterns (Class I, II, III) (Fig. 2), and there were no differences in HbA1c reduction between binding patterns (Fig. 2, Supplementary Table S1). Nonetheless, the correlation analysis between the change in HbA1c and the maximum serum concentration (Cmax) of DPP-4 inhibitors in all groups suggests a greater reduction in HbA1c when the DPP-4 inhibitors with low Cmax were switched to anagliptin (r2 = 0.5401) (Fig. 3, Supplementary Table S1) [30].
In a further analysis by comorbidities, the change of HbA1c in the without comorbidities group was − 0.68% at week 12 and − 0.89% at week 24, showing a significant reduction from baseline (p < 0.001). In comparison, the change of HbA1c in the with comorbidities group was − 0.27% at week 12 and − 0.22% at week 24, showing a significant but less pronounced reduction from baseline (p < 0.05) than in the without comorbidities group (Fig. 4-a, Supplementary Table S3).
Impact according to switching from dipeptidyl peptidase-4 inhibitors to anagliptin in T2DM patients. a Change from baseline in HbA1c by comorbidities. b Proportion of HbA1c target achieved by comorbidities. c Change from baseline in HbA1c by duration of T2DM. d Proportion of HbA1c target achieved by duration of T2DM. B baseline; 12w 12 weeks; 24w 24 weeks
In the without comorbidities group, the proportion of patients who achieved the HbA1c target of < 7% was 10% at baseline, 70% (including 12% below 6.5% and 58% between 6.5 and 7%) at week 12, and 70% (including 29% below 6.5% and 41% between 6.5 and 7%) at week 24. The fraction of patients with < 6.5% HbA1c after switching to anagliptin increased throughout treatment. Contrastingly, in the with comorbidities group, the proportion was 4% at baseline, 20% (4% < 6.5% and 16% between 6.5 and 7%) at week 12, and 24% (6% < 6.5% and 18% between 6.5 and 7%) at week 24 (Fig. 4b, Supplementary Table S4).
We evaluated the change in HbA1c after switching to anagliptin according to the duration of T2DM (Fig. 4c). In the without comorbidities group, there was no difference in HbA1c change by the duration of T2DM: − 0.69% at week 12 and − 0.91% at week 24 in patients with < 5-year duration, − 0.66% at week 12 and − 0.79% at week 24 in the patients with 5–10-year duration, and − 0.71% at week 12 and − 0.98% at week 24 in the patients with ≥ 10-year duration (p > 0.05) (Fig. 4c, left; Supplementary Table S3). Similarly, there was no difference in the changes in HbA1c by the duration of T2DM in the with comorbidities group: − 0.47% at week 12 and − 0.30% at week 24 in patients with < 5-year duration, − 0.22% at week 12 and − 0.22% at week 24 in the patients with 5–10-year duration, and − 0.23% at week 12 and − 0.20% at week 24 in the patients with ≥ 10-year duration (p > 0.05) (Fig. 4c, right; Supplementary Table S3). Regardless of the duration of T2DM, the changes in HbA1c in the without comorbidities group were significantly more than those observed in the with comorbidities group.
The proportion of patients who achieved the HbA1c target of < 7% in the without comorbidities group was 11% at baseline, 85% at week 12, and 87% at week 24 with < 5-year duration of T2DM; in patients with 5–10-year duration, the proportion was 6% at baseline, 47% at week 12, and 44% at week 24; in patients with ≥ 10-year duration, the proportion was 10% at baseline, 34% at week 12, and 32% at week 24 (Fig. 4d, left; Supplementary Table S4). In the with comorbidities group, the proportion of patients who achieved the HbA1c target of < 7% was 5% at baseline, 27% at week 12, and 28% at week 24 with < 5-year duration of T2DM; in patients with 5–10-year duration, the proportion was 4% at baseline, 18% at week 12, and 24% at week 24; in patients with ≥ 10 years of duration, the proportion was 3% at baseline, 19% at week 12, and 22% at week 24 (Fig. 4d, right; Supplementary Table S4). The multivariate analysis was conducted using ANCOVA with concomitant medication, type of therapy before switching, duration of diabetes, and class of DPP-4 inhibitors as covariates. The change of HbA1c was significant between with and without comorbidities at week 24 (Supplementary Table S5).
Clinical Characteristics
Table 2 demonstrates the clinical characteristics of the study subjects with and without comorbidities after switching from DPP-4 inhibitors to anagliptin. Body weight, eGFR, and AST values did not change after switching to anagliptin (p > 0.05) at weeks 12 and 24. These results were unchanged when analyzed by comorbidity and duration of T2DM. However, ALT decreased significantly from 29.2 U/l at baseline to 26.8 U/l at week 12 (p = 0.021); ALT decreased to 27.5 U/l at week 24, but not significantly (p > 0.05).
Discussion
Current treatment for patients with T2DM who do not achieve adequate glucose control recommends adding various OHAs to previous therapy [3, 4]. Metformin is prescribed as first-line anti-diabetic treatment, and if the patients who taking metformin with OHA has insufficient glycemic control, dose increase or addition of other agent is required. However, this strategy may result in increased financial burdens and safety risks. In practice, switching to a different DPP-4 inhibitor improves glycemic control rather than a step-up approach to DPP-4 inhibitor-containing regimens. Many previous studies have investigated the additional glucose-lowering effect of switching DPP-4 inhibitors and reported a significant reduction in HbA1C after switching [23,24,25,26,27,28]. As a result, switching therapy has emerged as a viable treatment option for effectively lowering HbA1c in diabetic patients. Therefore, finding a factor that can predict therapeutic response when changing drugs between DPP-4 inhibitors is critical.
In our study, the patients who switched from other DPP-4 inhibitors to anagliptin had a change in HbA1c level of − 0.42% at week 24. Previous studies showed that DPP-4 inhibitors switching to teneligliptin resulted in changes of − 0.39% (12w), − 0.44% (24w), and − 0.52% (52w) [24]. Also, switching from sitagliptin 50 mg to vildagliptin 100 mg resulted in a reduction of HbA1c from 8.15% to 7.86% after 6 months. In this study, the reduction of HbA1c was comparable to glucosidase (GI) type add-on therapy (acarbose, voglibose, or miglitol) and was even more effective than increasing the DPP-4 inhibitor dosage [25]. All these results suggest that switching between DPP-4 inhibitors may be beneficial.
To identify a factor that can predict therapeutic response when switching anagliptin from other DPP-4 inhibitors, we first assessed the efficacy of lowering HbA1c by subgroups. In our study, having no comorbidities was a predicted therapeutic factor for improved glucose control with switching therapy. The change in HbA1c in patients without comorbidities was − 0.89% at week 24, whereas it was − 0.22% at week 24 in the with comorbidities group. Also, in the without comorbidities group, the proportion of reaching the target of < 6.5% HbA1c after switching was much more significant than those in the with comorbidities group. The clinical implication of HbA1c < 6.5% indicates that the patient is in the prediabetes range, indicating that the risk of diabetic complications is lower [31, 32]. Although the reduction in HbA1c following switching to anagliptin was more significant in patients with baseline HbA1c ≥ 8%, baseline HbA1c was similar in the group with (7.97%) and without comorbidities (7.89%), so more decreasing efficacy without comorbidities is still meaningful (Table 2, Supplementary Table S2). Consequently, our findings suggest that switching to anagliptin may be an option for type 2 diabetic patients who exhibit an inadequate response to DPP-4 inhibitors and have no comorbidities.
Since it is known that the duration of diabetes is an independent factor impacting HbA1c control, we examined the effect of T2DM duration on HbA1c change [33, 34]. There was no difference in the reducing effect of HbA1c based on the duration of T2DM in the groups without and with comorbidities. However, we observed that switching to anagliptin early in treatment will be most effective in the without comorbidities group because the proportion reaching the target HbA1c of < 7% was highest in the < 5-year duration T2DM patients (Fig. 4-d, Supplementary Table S4).
DPP-4 inhibitors interact differently with the active sites of DPP-4 and are thus divided into three classes, with anagliptin belonging to Class III (binds to S1, S2, S1′, and S2 extensive subsites) [35, 36]. In our study, we evaluated the effect of switching from class I, II, or III to anagliptin by classifying the DPP-4 inhibitors used before switching to anagliptin based on their binding characteristics and observed no difference in HbA1c change.
To further explain the additional HbA1c-lowering effect after switching to anagliptin, we examined the correlation between the maximum serum concentration (Cmax) of DPP inhibitors (r2 = 0.5401). Switching from DPP-4 inhibitors with a lower Cmax to anagliptin (Cmax, 476 ng/ml) resulted in a more significant reduction in HbA1c. Considering these findings, DPP-4 inhibitors with a low Cmax are unlikely to inhibit existing or newly produced DPP-4 target proteins entirely. Reports indicate that all DPP-4 inhibitors can antagonize > 80% of DPP-4 [37, 38], but the Cmax of the drug for each target organ may vary depending on the DPP-4 inhibitor. The evidence that Cmax affects the therapeutic response is unclear. The Cmax value is likely to vary depending on the characteristics of the patients involved in the study (especially by ethnicity). However, according to Erina Shigematsu et al. [28], the switch from vildagliptin (50 mg, twice daily; Cmax 397 ng/ml) to sitagliptin (100 mg, daily; Cmax 390 ng/ml) resulted in no change in HbA1c, but the switch from alogliptin (25 mg, twice daily; Cmax 110 ng/ml) to sitagliptin (100 mg, daily; Cmax 390 ng/ml) produced a significant reduction in HbA1c (− 0.3%, p < 0.05).
This study has several limitations. First, because it was a non-comparative, single-arm study without a control group, some confounding factors, such as concomitant diseases or other heterogeneous drugs, might have influenced glycemic control. Additionally, the possibility of confounding factors and bias due to the limited number of patients in the subgroups cannot be ruled out. Further mechanism analysis such as functional assay of α- and β-cells is needed to understand the factors influencing glycemic control, and these will provide the exact scientific evidence. Second, it is unclear whether the characteristics of the patient group that can benefit from switching to anagliptin are specific to anagliptin, which warrants further studies. Third, there is the risk of inaccuracy in the presence of comorbidities since it relies only on the patient’s record rather than the actual results of a medical examination. Consequently, an additional randomized-controlled trial with cross-over design between anagliptin and other DPP-4 inhibitors is required to confirm the switching effect in the future.
In conclusion, this was the first study to evaluate the effect of comorbidities and duration of T2DM on HbA1c reduction after switching between DPP-4 inhibitors. Our findings will help identify patients who would benefit from switching with an additional HbA1c-lowering effect.
Conclusion
In patients with T2DM poorly controlled by other DPP-4 inhibitors, HbA1c levels were significantly decreased after switching to anagliptin. Because the change in HbA1c was greater in patients without comorbidities than in those with comorbidities, switching to anagliptin before adding additional OHAs may be an option in patients without comorbidities. By switching between DPP-4 inhibitors, more benefits can be expected, such as lower healthcare costs, better patient compliance, and improved safety.
References
Chaudhury A, Duvoor C, Dendi VSR, et al. Clinical review of antidiabetic drugs: implications for type 2 diabetes mellitus management. Front Endocrinol (Lausanne). 2017;8:6.
Feingold KR. Oral and injectable (non-insulin) pharmacological agents for the treatment of type 2 diabetes. Endotext. South Dartmouth: MDTextcom Inc; 2000.
Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41(12):2669–701.
Hur KY, Moon MK, Park JS, et al. 2021 clinical practice guidelines for diabetes mellitus of the Korean Diabetes Association. Diabetes Metab J. 2021;45(4):461–81.
Richard KR, Shelburne JS, Kirk JK. Tolerability of dipeptidyl peptidase-4 inhibitors: a review. Clin Ther. 2011;33(11):1609–29.
Ahrén B. DPP-4 inhibition and the path to clinical proof. Front Endocrinol (Lausanne). 2019;10:376.
Aschner P, Kipnes MS, Lunceford JK, Sanchez M, Mickel C, Williams-Herman DE. Effect of the dipeptidyl peptidase-4 inhibitor sitagliptin as monotherapy on glycemic control in patients with type 2 diabetes. Diabetes Care. 2006;29:2632–7.
Mikhail N. Combination therapy with DPP-4 inhibitors and pioglitazone in type 2 diabetes: theoretical consideration and therapeutic potential. Vasc Health Risk Manag. 2008;4:1221–7.
Wu D, Li L, Liu C. Efficacy and safety of dipeptidyl peptidase-4 inhibitors and metformin as initial combination therapy and as monotherapy in patients with type 2 diabetes mellitus: a meta-analysis. Diabetes Obes Metab. 2014;16:30–7.
Wang F, He Y, Zhang R, Zeng Q, Zhao X. Combination therapy of metformin plus dipeptidyl peptidase-4 inhibitor versus metformin plus sulfonylurea and their association with a decreased risk of cardiovascular disease in type 2 diabetes mellitus patients. Medicine (Baltimore). 2017;96: e7638.
Lin YH, Huang H. Predictors of the efficacy of dipeptidyl peptidase-4 inhibitors in taiwanese patients with type 2 diabetes mellitus. Diabetes Metab Syndr Obes. 2019;12:2725–33.
Cai X, Han X, Luo Y, Ji L. Efficacy of dipeptidyl-peptidase-4 inhibitors and impact on β-cell function in Asian and Caucasian type 2 diabetes mellitus patients: a meta-analysis. J Diabetes. 2015;7(3):347–59.
Nishio S, Abe M, Ito H. Anagliptin in the treatment of type 2 diabetes: safety, efficacy, and patient acceptability. Diabetes Metab Syndr Obes. 2015;8:163–71.
Furuta S, Smart C, Hackett A, Benning R, Warrington S. Pharmacokinetics and metabolism of [14C]anagliptin, a novel dipeptidyl peptidase-4 inhibitor, in humans. Xenobiotica. 2013;43(5):432–42.
Kaku K. Efficacy and safety of anagliptin add-on therapy in Japanese patients with type 2 diabetes. Jpn Pharmacol Ther. 2012;40(9):745–70.
Chihara A, Tanaka A, Morimoto T, et al. Differences in lipid metabolism between anagliptin and sitagliptin in patients with type 2 diabetes on statin therapy: a secondary analysis of the REASON trial. Cardiovasc Diabetol. 2019. https://doi.org/10.1186/s12933-019-0965-3.
Ghouse J, Isaksen JL, Skov MW, et al. Effect of diabetes duration on the relationship between glycaemic control and risk of death in older adults with type 2 diabetes. Diabetes Obes Metab. 2020;22(2):231–42.
Cho YK, Lee J, Kang YM, et al. Clinical parameters affecting the therapeutic efficacy of empagliflozin in patients with type 2 diabetes. PLoS ONE. 2019;14(8): e0220667.
Urina-Jassir M, Herrera-Parra LJ, Vargas JAH, et al. The effect of comorbidities on glycemic control among Colombian adults with diabetes mellitus: a longitudinal approach with real-world data. Endocr Disord. 2021;21(1):128.
Jeon JY, Kim DJ, Ko SH, et al. Current status of glycemic control of patients with diabetes in Korea: the Fifth Korea National Health and Nutrition Examination Survey. Diabetes Metab J. 2014;38(3):197–203.
Kim BY, Jung CH, Mok JO, Kim CH. Factors associated with long-term oral hypoglycemic agent responsiveness in korean patients with type 2 diabetes mellitus. Diabetes Metab J. 2011;35(3):282–9.
Ogundipe O, Mazidi M, Chin KL, et al. Real-world adherence, persistence, and in-class switching during use of dipeptidyl peptidase-4 inhibitors: a systematic review and meta-analysis involving 594,138 patients with type 2 diabetes. Acta Diabetol. 2021;58(1):39–46.
Kim HJ, Kim YS, Lee CB, et al. Efficacy and safety of switching to teneligliptin in patients with type 2 diabetes inadequately controlled with dipeptidyl peptidase-4 inhibitors: a 12-week interim report. Diabetes Ther. 2019;10:1271–82.
Kim HJ, Kim YS, Lee CB, et al. Efficacy and safety of switching to teneligliptin in patients with type 2 diabetes inadequately controlled with dipeptidyl peptidase-4 inhibitors: 52-week results from a prospective observational study. Diabetes Ther. 2021;12:2907–20.
Tanaka M, Nishimura T, Sekioka R, Itoh H. Dipeptidyl peptidase-4 inhibitor switching as an alternative add-on therapy to current strategies recommended by guidelines: analysis of a retrospective cohort of type 2 diabetic patients. J Diabetes Metab. 2016;7:9.
Han E, Lee M, Lee YH, et al. Effect of switching from linagliptin to teneligliptin dipeptidyl peptidase-4 inhibitors in older patients with type 2 diabetes mellitus. Diabetes Metab Syndr Obes. 2020;13:4113–21.
Suzuki Y, Tanaka A, Tanaka M, et al. Clinical effectiveness of switching between DPP-4 inhibitors in patients with type 2 diabetes mellitus. Int J Clin Pharmacol Ther. 2019;57(9):474–7.
Shigematsu E, Yamakawa T, Oba MS, et al. A randomized controlled trial of vildagliptin versus alogliptin: effective switch from sitagliptin in patients with type 2 diabetes. J Clin Med Res. 2017;9(7):567–72.
Nabeno M, Akahoshi F, Kishida H, et al. A comparative study of the binding modes of recently launched dipeptidyl peptidase IV inhibitors in the active site. Biochem Biophys Res Commun. 2013;434(2):191–6.
Sung-Ho K, Jung-Hwa Y, Woo JL, et al. Gemigliptin: an update of its clinical use in the management of type 2 diabetes mellitus. Diabetes Metab J. 2016;40(5):339–53.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37(1):S81–90.
Sherwani IS, et al. Significance of HbA1c test in diagnosis and prognosis of diabetic patients. Biomarker Insights. 2016;11:95–104.
Ghouse J, Isaksen J, Shov MW, et al. Effect of diabetes duration on the relationship between glycaemic control and risk of death in older adults with type 2 diabetes. Diabetes Obes Metab. 2020;22(2):231–42.
Lind M, Imberg H, Coleman RL, Nerman O, Homlan RR. Historical HbA1c values may explain the type 2 diabetes legacy effect: UKPDS 88. Diabetes Care. 2021;44:2231–7.
Watanabe YS, Yasuda Y, Kojima Y, et al. Anagliptin, a potent dipeptidyl peptidase IV inhibitor: its single-crystal structure and enzyme interactions. J Enzyme Inhib Med Chem. 2015;30(6):981–8.
Gallwitz B. Clinical use of DPP-4 inhibitors. Front Endocrinol (Lausanne). 2019;10:389.
Makrilakis K. The role of DPP-4 inhibitors in the treatment algorithm of type 2 diabetes mellitus: when to select, what to expect. Int J Environ Res Public Health. 2019;16(15):2720.
Hu P, Yin Q, Deckert F, et al. Pharmacokinetics and pharmacodynamics of vildagliptin in healthy Chinese volunteers. J Clin Pharmacol. 2009;49(1):39–49.
Acknowledgements
Funding
This study and the journal's Rapid Service Fee were supported by JW pharmaceutical (Seoul, Republic of Korea), which was involved in the study design; the collection, analysis, and interpretation of the data; and the decision to submit the paper for publication.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Sang-Yong Kim and Sungrae Kim contributed to the design and conduct of the study and the acquisition, analysis, and interpretation of data, and drafted the manuscript. All authors reviewed and approved the final manuscript.
Disclosures
Sang-Yong Kim declares that he has no conflict of interest. Sungrae Kim received research grants from JW pharmaceutical for coordination of this study.
Compliance with Ethics Guidelines
This study was performed in compliance with the Korea Good Clinical Practice (KGCP), International Council for Harmonization-GCP (ICH-GCP), and all applicable regulations. This study was reviewed and approved by the respective Institutional Review Boards (IRB) and details of ethics committees are provided in Supplementary Table S6. All patients provided informed consent before participating in this study. This study was conducted in compliance with the Declaration of Helsinki.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
13300_2022_1339_MOESM1_ESM.jpg
Supplementary file1 Figure S1. Histogram of HbA1c according to duration of diabetes mellitus. a: Without comorbidities. b: With comorbidities. (JPG 96 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kim, SY., Kim, S. Therapeutic Effects of Switching to Anagliptin from Other DPP-4 Inhibitors in T2DM Patients with Inadequate Glycemic Control: A Non-interventional, Single-Arm, Open-Label, Multicenter Observational Study. Diabetes Ther 14, 109–121 (2023). https://doi.org/10.1007/s13300-022-01339-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-022-01339-4