Abstract
Introduction
The aim of this study was to assess the efficacy and safety of switching to teneligliptin from other dipeptidyl peptidase-4 (DPP-4) inhibitors in patients with type 2 diabetes mellitus (T2DM) inadequately controlled despite treatment with a stable dose of other DPP-4 inhibitors.
Methods
Patients with glycosylated hemoglobin (HbA1c) ≥ 7% despite taking DPP-4 inhibitors other than teneligliptin, with or without other antidiabetic agents, for at least 3 months were enrolled in this study. Patients on DPP-4 inhibitors administered prior to participation in this study were switched to 20 mg teneligliptin once daily and the dose was maintained for the 52-week study period. The primary endpoint was the change in HbA1c at week 12. Fasting plasma glucose (FPG) and the blood lipid profile were also evaluated. Adverse events were monitored for safety assessment.
Results
At weeks 12, 24, and 52, the HbA1c values significantly decreased by − 0.39, − 0.44, and − 0.52%, respectively, compared to the baseline value (p < 0.0001); in addition, 56.3, 60.3, and 62.3% of patients, respectively, achieved decreases in HbA1c of at least 0.3%, and 40.1, 46.5, and 52.4% of patients, respectively, achieved decreases in HbA1c of at least 0.5%. The proportion of the patient population achieving HbA1c < 7.0% increased throughout the study period, reaching 30.4, 35.4, and 36.9% at weeks 12, 24, and 52, respectively; at these same time points, the percentage of patients achieving HbA1c < 6.5% increased to 9.5, 11.9, and 13.2% of the total study population. FPG levels and lipid parameters were also significantly decreased after teneligliptin treatment. There were no significant safety concerns.
Conclusion
Our results suggest the significant glucose-lowering effect of teneligliptin after switching from other DPP-4 inhibitors in patients with T2DM. The improvement in glycemic control was maintained for up to 52 weeks without safety concerns.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Teneligliptin, an antidiabetic agent classified as a class III dipeptidyl peptidase-4 (DPP-4) inhibitor, has a unique structural feature that provides strong binding to DPP-4 enzymes. |
We investigated the efficacy and safety of switching to teneligliptin from other DPP-4 inhibitors in patients with type 2 diabetes mellitus (T2DM) inadequately controlled despite treatment with a stable dose of other DPP-4 inhibitors. |
What was learned from the study? |
Glycosylated hemoglobin (HbA1c) levels decreased significantly in these patients with T2DM after the switch to teneligliptin, and the improvement in glycemic control was maintained for up to 52 weeks without safety concerns. |
The results suggest that the HbA1c decreases observed in this study may be evidence of the superior potency of teneligliptin. |
Introduction
The global prevalence of diabetes was estimated to be 9.3% of the world’s adult population in 2019 and projected to reach 10.2% by 2030 and 10.9% by 2045 [1]. Diabetes is a progressive disease, with progression associated with worsening glycemic control and increased risk for chronic hyperglycemia-induced complications, including microvascular and macrovascular diseases [2]. These co-morbidities exacerbate the burden of diabetes on individuals and healthcare systems. Consequently, optimal glucose management is required to prevent or delay the onset of complications [3].
Dipeptidyl peptidase-4 (DPP-4) inhibitors increase the levels of active incretin hormones by inhibiting DPP-4 activity, improving hyperglycemia in a glucose-dependent manner through the stimulation of insulin secretion and inhibition of glucagon secretion. Consequently, DPP-4 inhibitors have been used as antidiabetic drugs that can decrease glucose fluctuations in diabetic patients, with good safety [4, 5]. DPP-4 inhibitors are currently the most popular add-on therapy to metformin and sulfonylureas (SU) and their use has gradually increased in recent years [6].
DPP-4 has multiple binding sites that determine the potency and selectivity of different DPP-4 inhibitors. In comparison to other DDP-4 inhibitors, teneligliptin has a unique structural feature that enables relatively stronger binding [7]. Previous studies have shown that teneligliptin can significantly reduce glycosylated hemoglobin (HbA1c) when administered as monotherapy or as adjuvant to metformin, glimepiride, or insulins [8,9,10,11,12]. Meta-analyses showed that compared with placebo, DPP-4 inhibitors lowered HbA1c by 0.65% [13] and teneligliptin lowered HbA1c by 0.82%, a significant reduction [14]. These somewhat larger changes may indicate that teneligliptin has a greater efficacy than other DPP-4 inhibitors, but only limited information on switching from other DPP-4 inhibitors to teneligliptin is currently available.
Consequently, the aim of this study was to evaluate the efficacy and safety of switching from therapy with other DPP-4 inhibitors to teneligliptin in patients with type 2 diabetes mellitus (T2DM) and inadequate glycemic control despite treatment with a stable dose of other DPP-4 inhibitors. We previously reported 12-week interim results in which blood glucose was lowered further without any safety concerns after the switch to teneligliptin [15]. Here, we report the final results of the 52-week study.
Methods
Study Design and Participants
This 52-week, open-label, single-arm, multicenter, prospective observational study was conducted in the Republic of Korea between January 2016 and September 2019 (ClinicalTrials.gov: NCT03793023). The planned number of participating sites was initially 105, but ultimately 90 hospitals actually participated. All patients provided written informed consent before being enrolled in the study. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the institutional review board of each center or by the local institutional review board (IRB), including Ajou University Hospital IRB (AJIRB-MED-OBS-15-410) [a full list of participating centers is provided in Electronic Supplementary Material (ESM) Table S2].
A detailed description of the study design and the eligibility criteria for study participants have been previously described in the 12-week interim report [15]. Briefly, patients with T2DM whose HbA1c was ≥ 7% despite taking DPP-4 inhibitors with or without other antidiabetic agents for at least 3 months were screened and enrolled. Eligible patients switched prior DPP-4 inhibitors to teneligliptin (20 mg/day) and baseline concomitant antidiabetic regimens were maintained for 52 weeks. Patients were removed from the study if any of the following occurred: adverse events that made it difficult to continue; modification of another antidiabetic treatment; participant’s decision to withdraw consent for any reason; violation of inclusion/exclusion criteria; lost to follow-up; and if, in the investigators’ opinion, a patient was unable to continue to participate. Study visits were scheduled at baseline and at weeks 12, 24, and 52 after the switch to teneligliptin. To evaluate the effect of switching from other DPP-4 inhibitors to teneligliptin, patients’ HbA1c, fasting plasma glucose (FPG), serum lipid [total cholesterol, low-density lipoprotein-cholesterol (LDL-C), high-density lipoprotein-cholesterol (HDL-C), and triglyceride values], weight, and body mass index (BMI) were assessed. Data on adverse events (AEs) were also collected.
Outcome Measures
The primary endpoint was the mean change in HbA1c from baseline to week 12. The secondary endpoints included the mean change in HbA1c from baseline to weeks 24 and 52; mean change in FPG, weight, BMI, and serum lipids from baseline to weeks 12, 24, and 52; the percentage of participants achieving HbA1c < 7% or < 6.5% at weeks 12, 24, and 52; and the percentage of patients with HbA1c reduction of ≥ 0.3% or ≥ 0.5% from baseline to weeks 12, 24, and 52. For the primary endpoint, subgroup analysis was performed to evaluate the change in HbA1c values at 12 weeks after switching to teneligliptin therapy according to age, duration of T2DM, baseline BMI, and baseline HbA1c values.
Safety was assessed by monitoring AEs, hypoglycemic events, laboratory tests, and vital signs. A hypoglycemic episode was identified by asking patients about their experience of hypoglycemic symptoms or a self-monitoring blood glucose level of < 70 mg/dL with or without one of the following symptoms: sweating, fatigue, dizziness, headache, tremor, hunger, irritability, and seizure. Severe hypoglycemia was defined as requiring the assistance of another person to take corrective action [16].
Statistical Analysis
All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA). Continuous variables of the baseline demographic and biochemical parameters were described as descriptive statistics [mean ± standard deviation (SD)], and categorical variables were presented as counts with percentages. The efficacy set included all patients who were enrolled and reported at least one HbA1c level after receiving study treatment. The safety analysis set included all patients who received at least one dose of the study drug. Missing data were not imputed.
We calculated the sample size to achieve at least 90% power with a 0.05% significance level to detect a 0.3% change in HbA1c after switching to teneligliptin [15]. The null hypotheses were that there would be no difference in HbA1c after 12 weeks of switching therapy (1) from each of the six original DPP-4 inhibitors to teneligliptin or (2) from DPP-4 inhibitors overall to teneligliptin.
Changes in any efficacy measure from baseline to each time point were analyzed using paired t test at a two-sided significance level of 5%. For the primary endpoint, multiple testing correction was performed based on Hochberg’s step-up method.
All AEs were classified according to the Medical Dictionary for Regulatory Activities Version 23.0 (MedDRA 23.0), and the incidence rate and number of events were presented according to System Organ Class (SOC) and preferred terms (PT) categorization.
Results
Baseline Characteristics of Patients
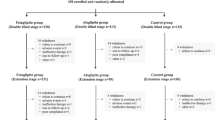
A total of 2983 patients were enrolled out of the 3093 patients screened, of which 2923 patients were analyzed as a safety set and 2501 patients were included in an efficacy set (Fig. 1). The number of patients for whom efficacy data were available varied during the 52-week study period, with efficacy data available for 1895, 1683, and 1503 patients at weeks 12, 24, and 52, respectively.
The baseline characteristics of the study population are summarized in Table 1. The mean (±SD) age of patients was 63.1 ± 11.0 years, with patients aged > 65 years accounting for 46.4% of the study population, and 51.70% (1293/2501) were male. The mean duration of T2DM was 8.8 ± 7.2 years. The mean HbA1c values at baseline were 7.94 ± 0.96%. Prior to enrolling in the study, approximately 15% of patients had been treated with a DDP-4 inhibitor as monotherapy, while the other patients had been treated with a DPP-4 inhibitor as an add-on therapy with one or more antidiabetic agents. Prior to the switch to teneligliptin, the most frequently administered DPP-4 inhibitor was linagliptin (34.4%), followed, in decreasing order of use, by sitagliptin (25.6%), gemigliptin (13.3%), vildagliptin (13.1%), saxagliptin (8.6%), and alogliptin (5.0%).
Efficacy
Glycosylated hemoglobin values decreased significantly 12 weeks after switching treatment to teneligliptin, and these reductions were maintained through to 52 weeks. Overall, HbA1c was 7.94% at baseline, subsequently significantly decreasing to 7.53% (− 0.39%; p < 0.0001), 7.45% ( − 0.44%; p < 0.0001), and 7.42% (− 0.52%; p < 0.0001) at weeks 12, 24, and 52, respectively (Table 2; Fig. 2a). In the individual DPP-4 inhibitor groups, the ranges of differences were − 0.16 to − 0.51, − 0.23 to − 0.56 and − 0.22 to − 0.69 at weeks 12, 24 and 52, respectively, compared to the baseline (ESM Table S1).
HbA1c levels after 52 weeks of treatment with teneligliptin. a Changes in HbA1c levels at weeks 12, 24, and 52. Values are presented as the mean ± standard error (SE). Asterisk indicates statistically significant difference according to the paired t test vs. the baseline HbA1c values. b Percentage of patients with a decrease in HbA1c of ≥ 0.3 and ≥ 0.5%. c Percentage of patients achieving HbA1c < 7.0 and < 6.5%, respectively
At weeks 12, 24, and 52 after the switch to teneligliptin, 56.3, 60.3, and 62.3% of patients showed a decrease in HbA1c of at least 0.3%, and 40.1, 46.5, and 52.4% of patients showed a decrease in HbA1c of at least 0.5% (Fig. 2b). In terms of response rate, the proportion of patients who achieved HbA1c < 7.0% increased throughout the study period, with 30.4, 35.4, and 36.9% of patients achieving HbA1c < 7% at weeks 12, 24, and 52, respectively. A similar trend was observed for patients achieving HbA1c < 6.5%, with 9.5, 11.9, and 13.2% of patients achieving this outcome at weeks 12, 24, and 52, respectively (Fig. 2c).
In the subgroup analysis at week 12, the effect on HbA1c of switching to teneligliptin treatment was consistent across subgroups. The mean changes in HbA1c in patients aged < 65 and ≥ 65 years were statistically significant (− 0.40 and − 0.38%, respectively; p < 0.0001; Fig. 3a). Patients with T2DM duration of < 5 years had a decrease in HbA1c of 0.60% and those with T2DM duration of ≥ 5 years had a decrease of 0.28%; the reductions in both subgroups were significant (p < 0.0001; Fig. 3b). Hyperglycemia was also attenuated regardless of BMI. All BMI subgroups (< 23, ≥ 23 and < 25, ≥ 25 kg/m2) showed a significant reduction in HbA1c (− 0.37, − 0.43, and − 0.37%, respectively; p < 0.0001 (Fig. 3c). Patients with baseline HbA1c values of both ≥ 8% and < 8% showed significant improvement (p < 0.0001; Fig. 3d); however, the reduction was greater in patients with baseline HbA1c ≥ 8%.
Change in HbA1c values according to baseline characteristics. Changes in HbA1c values according to age (a), duration of T2DM (b), BMI (c), and baseline HbA1c value (d). Values are presented as the mean ± SE. Asterisk indicates statistically significant difference according to the paired t test vs. the baseline HbA1c values
Results for other secondary outcomes are also presented in Table 2. Significant decreases from baseline in FPG levels were observed at 12, 24, and 52 weeks, with mean differences of − 11.1, − 19.4, and − 24.1 mg/dL, respectively (p < 0.0001). Teneligliptin significantly decreased the lipid parameters at weeks 12, 24, and 52, including total cholesterol (− 5.97, − 7.65, and − 13.75 mg/dL, respectively; p < 0.0001) and LDL-C (− 3.54, − 4.06, and − 7.35 mg/dL, respectively; p < 0.001). Triglyceride levels were significantly decreased at weeks 24 and 52, with mean differences of − 14.8 and − 21.0 mg/dL, respectively (p = 0.0007 and p < 0.0001), whereas there were no significant changes in HDL-C throughout the study. There were significant differences in weight at weeks 12 and 24 (p < 0.0001 and p = 0.0046); however, the final values at week 52 showed no changes compared to baseline (p = 0.6992).
Safety
From the 2923 patients in the safety set, a total of 332 AEs were reported in 218 patients (incidence rate 7.46%) and 30 adverse drug reactions were reported in 26 patients (incidence rate 0.89%) during the 52-week study period (Table 3).
The most frequent AE reported was hypoglycemia (0.51% of patients), with dizziness, dyspepsia, and headache reported as secondary AEs at an incidence rate of 0.41%. Of the 15 patients who reported hypoglycemia, three reported severe hypoglycemia (0.10%); of these three patients, one patient taking SU, another was on SU and insulin combination therapy, and the third patient was taking metformin. All three patients recovered.
The overall incidence rate of serious AEs was 1.78%; these included hyperglycemia (0.21%), pneumonia (0.14%), cardiac failure (0.10%), and others. Causal relationships with teneligliptin were considered to be unlikely.
Discussion
The results of this study show that switching from other DPP-4 inhibitors to teneligliptin was well tolerated by the patients with T2DM in this study and effected a significant decrease in HbA1c level. These results are generally consistent with those of the interim analysis at 12 weeks showing improvement in glycemic control, with improvement maintained for up to 52 weeks of teneligliptin treatment without safety concerns [15].
In the pathogenesis of T2DM, insulin resistance leads to the acceleration of insulin secretion that eventually results in subsequent deterioration of β-cell function. DPP-4 inhibitors have been shown to have good glycemic durability that allows them to alleviate β-cell apoptosis and protect β-cell mass and function [17]. Our results showing sustained improvement in HbA1c levels for 52 weeks after switching from other DPP-4 inhibitors correspond with those from previous studies that reported the long-term durability of teneligliptin [18, 19]. A meta-analysis of DPP-4 inhibitors reported that they significantly decreased HbA1c for 2 years [20], while another study with teneligliptin reported sustained efficacy over 3 years [18].
While present guidelines suggest adding different classes of hypoglycemic agents to the therapeutic regimen of patients who do not achieve adequate glycemic control, this strategy may increase the pill and economic burdens. A previous study of switching from sitagliptin to vildagliptin also reported a significant glucose-lowering effect [21]. Similarly, another study of switching from linagliptin to teneligliptin also reported significant amelioration in glycemic parameters, such as HbA1c (7.9 ± 1.3% to 7.5 ± 1.2%; p < 0.001), fasting blood glucose (148.1 ± 47.1 to 139.6 ± 43.4 mg/dL; p = 0.041), and postprandial blood glucose (224.8 ± 77.4 to 205.8 ± 70.8 mg/dL; p = 0.002) [22]. Switching oral antidiabetic drugs within the same class could effectively lower blood glucose without the addition of another drug, and switching to teneligliptin from other DPP-4 inhibitors could be an alternative option.
In addition, FPG levels also decreased during the observation period after switching to teneligliptin. A number of studies have reported that teneligliptin therapy decreased not only HbA1c but also FPG, 2-h postprandial glucose, or 24-h blood glucose levels [4, 10, 23, 24]. These results support the facilitating effect of teneligliptin in glycemic control. The glucose-lowering effect of teneligliptin observed in the present study may be partially mediated by its unique structure and properties that differentiate it from other DPP-4 inhibitors. Teneligliptin consists of a considerably rigid “J-shaped” anchor lock structure formed by five rings, four of which directly bind to DPP-4, providing stronger binding than other DPP-4 inhibitors [23]. It has also been suggested that the binding interactions with the hydrogen bond in the S2 subsite and hydrophobic interaction in the extensive S2 subsite may contribute the stronger binding affinity of teneligliptin [23]. The unique structure of teneligliptin also contributes to a delayed dissociation rate and half maximal inhibitory concentration (IC50), thus indicating teneligliptin as a more potent inhibitor than other DPP-4 inhibitors [25, 26].
In this study, total cholesterol, LDL-C, and triglyceride values initially decreased and these decreases were maintained during the study period. The decreases in lipid profiles were consistent those reported from other studies in which incretin therapies, including DPP-4 inhibitors, were found to improve lipid profiles through effects on insulin secretion and inhibition of postprandial lipoprotein secretion [27, 28]. Similarly, teneligliptin has been reported to significantly reduce total cholesterol, LDL-C, and triglyceride in previous studies [29,30,31]. Overall, our results indicate that clinically relevant changes in glycemic control and improved lipid profiles can be achieved with teneligliptin, even after switching from other DPP-4 inhibitors.
With regard to safety, teneligliptin was well tolerated for 52 weeks. The AE profile was similar to that described elsewhere [19, 32], and only 0.51% of patients reported hypoglycemic events during the study period. All patients who reported hypoglycemic events were also taking other glucose-lowering agents, such as SU and insulin, which are known to be high-risk drugs for hypoglycemia.
This study has several limitations, one of which is its non-comparative, single-arm design. Since this study did not have a control group, there could be several confounding factors, such as heterogeneities in concomitant disease or other concomitant medication. Furthermore, information on changes in lipid-modifying drug or diet was not fully collected or analyzed. Lifestyle changes during the observation period may have affected the study results. An additional limitation of our study includes a low follow-up rate after 52 weeks of the study period. However, despite these limitations, this study is significant in that it reports large-scale, real-world data. Moreover, the study showed that teneligliptin effectively improved and maintained glycemic control for 52 weeks without safety concerns in patients with T2DM.
Conclusion
This study showed the efficacy and safety of teneligliptin after switching from other DPP-4 inhibitors in patients with inadequately controlled T2DM despite treatment. A significant glucose-lowering effect was observed and maintained for 52 weeks. With regard to safety, there were no significant safety concerns, which is similar to known profiles.
References
Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract. 2019;157:107843.
Ha KH, Kim DJ. Current status of managing diabetes mellitus in Korea. Korean J Intern Med. 2016;31:845–50.
Jung CH, Son JW, Kang S, et al. Diabetes fact sheets in Korea, 2020: an appraisal of current status. Diabetes Metab J. 2021;45:1–10.
Kishimoto M. Teneligliptin: a DPP-4 inhibitor for the treatment of type 2 diabetes. Diabetes Metab Syndr Obes. 2013;6:187–95.
Nakamura Y, Hasegawa H, Tsuji M, et al. Diabetes therapies in hemodialysis patients: dipeptidase-4 inhibitors. World J Diabetes. 2015;6:840–9.
Korean Diabetes Association. Diabetes fact sheets in Korea, 2018: an appraisal of current status. 2018. https://www.diabetes.or.kr/bbs/skin/dianews/download.php?code=admin&number=1859. Accessed 30 Jun 2021.
Maladkar M, Sankar S, Kamat K. Teneligliptin: heralding change in type 2 diabetes. J Diabetes Mellitus. 2016;6:113–31.
Kadowaki T, Kondo K. Efficacy and safety of teneligliptin added to glimepiride in Japanese patients with type 2 diabetes mellitus: a randomized, double-blind, placebo-controlled study with an open-label, long-term extension. Diabetes Obes Metab. 2014;16:418–25.
Kadowaki T, Kondo K, Sasaki N, et al. Efficacy and safety of teneligliptin add-on to insulin monotherapy in Japanese patients with type 2 diabetes mellitus: a 16-week, randomized, double-blind, placebo-controlled trial with an open-label period. Expert Opin Pharmacother. 2017;18:1291–300.
Hong S, Park CY, Han KA, et al. Efficacy and safety of teneligliptin, a novel dipeptidyl peptidase-4 inhibitor, in Korean patients with type 2 diabetes mellitus: A 24-week multicentre, randomized, double-blind, placebo-controlled phase III trial. Diabetes, Obes Metab. 2016;18:528–32.
Kim MK, Rhee E-J, Han KA, et al. Efficacy and safety of teneligliptin, a dipeptidyl peptidase-4 inhibitor, combined with metformin in Korean patients with type 2 diabetes mellitus: a 16-week, randomized, double-blind, placebo-controlled phase III trial. Diabetes Obes Metab. 2015;17:309–12.
Bryson A, Jennings PE, Deak L, Paveliu FS, Lawson M. The efficacy and safety of teneligliptin added to ongoing metformin monotherapy in patients with type 2 diabetes: a randomized study with open label extension. Expert Opin Pharmacother. 2016;17:1309–16.
Park H, Park C, Kim Y, Rascati KL. Efficacy and safety of dipeptidyl peptidase-4 inhibitors in type 2 diabetes: meta-analysis. Ann Pharmacother [Internet]. 2012;46:1453–69.
Li X, Huang X, Bai C, et al. Efficacy and safety of teneligliptin in patients with type 2 diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. Front Pharmacol. 2018;9:449.
Kim HJ, Kim YS, Lee CB, et al. Efficacy and safety of switching to teneligliptin in patients with type 2 diabetes inadequately controlled with dipeptidyl peptidase-4 inhibitors: a 12-week interim report. Diabetes Ther. 2019;10:1271–82.
Seaquist ER, Anderson J, Childs B, et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. J Clin Endocrinol Metab. 2013;98:1845–59.
Chen K, Kang D, Yu M, et al. Direct head-to-head comparison of glycaemic durability of dipeptidyl peptidase-4 inhibitors and sulphonylureas in patients with type 2 diabetes mellitus: a meta-analysis of long-term randomized controlled trials. Diabetes Obes Metab. 2018;20:1029–33.
Kadowaki T, Haneda M, Ito H, Sasaki K, Matsukawa M, Yamada Y. Long-term, real-world safety and efficacy of teneligliptin: a post-marketing surveillance of more than 10,000 patients with type 2 diabetes in Japan. Adv Ther. 2020;37:1065–86.
Kadowaki T, Haneda M, Ito H, Sasaki K, Yamada Y. Long-term safety and efficacy of teneligliptin in elderly patients with type 2 diabetes: subgroup analysis of a 3-year post-marketing surveillance in Japan. Adv Ther. 2020;37:2477–92.
Esposito K, Chiodini P, Maiorino MI, Bellastella G, Capuano A, Giugliano D. Glycaemic durability with dipeptidyl peptidase-4 inhibitors in type 2 diabetes: a systematic review and meta-analysis of long-term randomised controlled trials. BMJ Open. 2014;10(4):e005442.
Tanaka M, Nishimura T, Sekioka R, Itoh H. Dipeptidyl peptidase-4 inhibitor switching as an alternative add-on therapy to current strategies recommended by guidelines: analysis of a retrospective cohort of type 2 diabetic patients. J Diabetes Metab. 2016;7(9):701.
Han E, Lee M, Lee YH, et al. Effect of switching from linagliptin to teneligliptin dipeptidyl peptidase-4 inhibitors in older patients with type 2 diabetes mellitus. Diabetes Metab Syndr Obes. 2020;13:4113–21.
Nabeno M, Akahoshi F, Kishida H, et al. A comparative study of the binding modes of recently launched dipeptidyl peptidase IV inhibitors in the active site. Biochem Biophys Res Commun. 2013;434:191–6.
Sharma SK, Panneerselvam A, Singh KP, Parmar G, Gadge P, Swami OC. Teneligliptin in management of type 2 diabetes mellitus. Diabetes, Metab Syndr Obes Targets Ther. 2016;9:251–60.
Schnapp G, Klein T, Hoevels Y, Bakker RA, Nar H. Comparative analysis of binding kinetics and thermodynamics of dipeptidyl peptidase-4 inhibitors and their relationship to structure. J Med Chem. 2016;59:7466–77.
Fukuda-Tsuru S, Anabuki J, Abe Y, Yoshida K, Ishii S. A novel, potent, and long-lasting dipeptidyl peptidase-4 inhibitor, teneligliptin, improves postprandial hyperglycemia and dyslipidemia after single and repeated administrations. Eur J Pharmacol. 2012;696:194–202.
Mulvihill EE. Dipeptidyl peptidase inhibitor therapy in type 2 diabetes: Control of the incretin axis and regulation of postprandial glucose and lipid metabolism. Peptides. 2018;100:158–64.
Tsimihodimos V, Elisaf M. Incretins and lipid metabolism. Curr Med Chem. 2018;25:2133–9.
Tomonaga O, Kobayashi M, Tagawa R, Higami Y. The effects of teneligliptin on lipid profile: A prospective study for comparison of biomarkers before and after a meal. J Endocrinol Metab. 2020;10:79–88.
Kusunoki M, Sato D, Nakamura T, et al. DPP-4 inhibitor teneligliptin improves insulin resistance and serum lipid profile in Japanese patients with type 2 diabetes. Drug Res (Stuttg). 2014;65:532–4.
Parmar VM, Goswami SS. Efficacy and safety of teneligliptin as add-on therapy to conventional therapy in Indian patients with type 2 diabetes mellitus. Asian J Pharm Clin Res. 2019;12(12):116–20.
Kadowaki T, Marubayashi F, Yokota S, Katoh M, Iijima H. Safety and efficacy of teneligliptin in Japanese patients with type 2 diabetes mellitus: a pooled analysis of two Phase III clinical studies. Expert Opin Pharmacother. 2015;16:971–81.
Acknowledgements
The authors thank the investigators and the participants of the study.
Funding
Sponsorship for this study and the Rapid Service Fee were funded by Handok Inc., Seoul, Republic of Korea. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship of this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
HJK and KWL contributed to the design and conduct of the study and the acquisition, analysis, and interpretation of data, and drafted the manuscript. YSK, CBL, M-GC, H-JC, SKK, JMY, THK, JHL, KJA, and KWM contributed to the conduct of the study and the interpretation of data. EJK and YKK contributed to the design of the study and analysis of data. All authors reviewed and approved the final manuscript.
Disclosures
Eun Jung Kyung and Yeo Kyeong Kim are employees of Handok Inc. Hae Jin Kim, Young Sik Kim, Chang Beom Lee, Moon-Gi Choi, Hyuk-Jae Chang, Soo Kyoung Kim, Jae Myung Yu, Tae Ho Kim, Ji Hyun Lee, Kyu Jeung Ahn, Kyung Wan Min and Kwan Woo Lee have nothing to disclose.
Compliance with Ethics Guidelines
All patients provided written informed consent before being enrolled in the study. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the institutional review board of each center or by the local institutional review board (IRB), including Ajou University Hospital IRB (AJIRB-MED-OBS-15-410) (a full list of participating centers is provided in ESM Table S2).
Data Availability
The datasets generated and/or analyzed during this study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kim, H.J., Kim, Y.S., Lee, C.B. et al. Efficacy and Safety of Switching to Teneligliptin in Patients with Type 2 Diabetes Inadequately Controlled with Dipeptidyl Peptidase-4 Inhibitors: 52-Week Results from a Prospective Observational Study. Diabetes Ther 12, 2907–2920 (2021). https://doi.org/10.1007/s13300-021-01148-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-021-01148-1