Abstract
Introduction
BEYOND 7 demonstrated that a higher starting dose (0.3 U/kg) of insulin glargine 100 U/mL (Gla-100) is as safe as the standard starting dose (0.2 U/kg) in Chinese individuals with type 2 diabetes who had uncontrolled hyperglycaemia despite receiving oral antihyperglycaemic drugs. This post hoc analysis determined the effect of baseline characteristics on hypoglycaemia risk in these individuals.
Methods
Participants from BEYOND 7 were assessed based on their age at baseline (< 60 vs. ≥ 60 years), duration of diabetes (< 10 vs. ≥ 10 years), glycated haemoglobin (HbA1c; < 9 vs. ≥ 9%) and fasting plasma glucose level (FPG; < 11 vs. ≥ 11 mmol/L). Endpoints included the proportion of participants with overall confirmed (≤ 3.9 mmol/L) and symptomatic hypoglycaemia, as well as the proportion of participants who achieved an HbA1c < 7% without hypoglycaemia, the time to first achievement of fasting blood glucose (FBG) < 7 mmol/L and the change in HbA1c from baseline between the two treatment arms in each of these subgroups.
Results
The proportion of participants with overall confirmed (6.1–16.7%) or symptomatic hypoglycaemia (5.7–18.4%) or the proportion who achieved HbA1c < 7.0% without hypoglycaemia (23.6–47.4%) was similar between the two treatment arms in all subgroups, with the exception of participants with a baseline duration of diabetes ≥ 10 years who experienced more symptomatic hypoglycaemia if initiating Gla-100 at a dose of 0.3 versus 0.2 U/kg. Participants aged < 60 years with an HbA1c < 9% or ≥ 9% or a duration of diabetes of 2–10 years achieved an FBG < 7.0 mmol/L in a significantly shorter time with Gla-100 starting dose of 0.3 U/kg versus 0.2 U/kg (all p < 0.001). No significant differences were seen among the subgroups in terms of change from baseline in HbA1c.
Conclusions
Baseline age, duration of diabetes, HbA1c level and FPG level do not affect the risk of hypoglycaemia with a higher starting dose of Gla-100 versus its standard starting dose.
Trial registration
ClinicalTrials.gov: NCT02836704.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
BEYOND 7 was conducted to investigate the effects of initiating basal insulin glargine 100 U/mL (Gla-100) at a higher starting dose (0.3 U/kg) compared with the standard starting dose (0.2 U/kg) in obese or overweight Chinese individuals with type 2 diabetes (T2D) who had uncontrolled hyperglycaemia despite receiving oral antihyperglycaemic drugs. |
The study found that the higher starting dose of Gla-100 was as safe as the standard starting dose, and that self-monitored fasting blood glucose (FBG) targets were achieved earlier with the higher versus the standard dose. |
The aim of this post hoc analysis of BEYOND 7 was to determine if the baseline characteristics of individuals in the study had any effect on study outcomes. |
What was learned from the study? |
Baseline age (< 60 vs. ≥ 60 years), duration of diabetes (< 10 vs. ≥ 10 years), glycated haemoglobin (HbA1c; < 9% vs. ≥ 9%) or fasting plasma glucose (FPG; < 11 vs. ≥ 11 mmol/L) had no effect on the proportion of participants experiencing overall confirmed hypoglycaemia (≤ 3.9 mmol/L; 6.1–16.7%) or achieving an HbA1c < 7% without hypoglycaemia (23.6–47.4%) in BEYOND 7. |
In contrast, significantly more patients with a baseline duration of diabetes ≥ 10 years experienced symptomatic hypoglycaemia if initiating Gla-100 at the higher versus the standard dose (p = 0.011). |
Participants aged < 60 years with an HbA1c < 9% or ≥ 9% or a duration of diabetes of 2–10 years achieved an FBG < 7.0 mmol/L in a significantly shorter time with Gla-100 starting dose of 0.3 U/kg versus 0.2 U/kg (all p < 0.001). |
Introduction
Basal insulin is currently recommended for the management of hyperglycaemia in individuals with type 2 diabetes (T2D) when treatment with two or three oral antihyperglycaemic drugs (OADs) fails to effectively control hyperglycaemia [1]. However, the proportion of individuals achieving their glycaemic targets despite treatment with insulin (with or without OADs) is low, mainly due to the use of a suboptimal insulin dose [2]. Real-world data show that insulin is only uptitrated by 0.03–0.10 U/kg during the first 6–12 months after basal insulin initiation [3,4,5]. Insufficient dose titration largely undermines the efficacy of basal insulin, as reported in randomised controlled trials [6] and real-world clinical studies [3].
Both the initiation and maintenance of basal insulin in clinical practice are complicated by several patient- and physician-related challenges, including complexity of the therapeutic regimen, fear of treatment-related hypoglycaemia and weight gain, treatment costs, frustration regarding not reaching the titration goal and inconvenience and misconceptions about insulin being a terminal treatment [2, 7,8,9]. From the individual’s perspective, frustration at the time required to reach the titration goal is a more important barrier to achieving the glycaemic target than fear of hypoglycaemia [10]. Achieving early glycaemic control after basal insulin initiation, especially during the first 6 months, is important in predicting long-term glycaemic control [11]. Therefore, there is an urgent need to improve glycaemic control with the initiation of basal insulin treatment.
The BEYOND 7 trial was the first randomised controlled study to demonstrate that a higher starting dose (0.3 U/kg) of insulin glargine 100 U/mL (Gla-100) was as safe and effective as the standard starting dose (0.2 U/kg) in Chinese individuals with T2D who had uncontrolled hyperglycaemia despite being treated with two or three OADs [12]. The aim of this subgroup analysis of the BEYOND 7 study was to investigate the effect of baseline age, duration of diabetes and glycated haemoglobin (HbA1c) and fasting plasma glucose (FPG) levels on these outcomes.
Methods
Study Design, Participants and Assessments
BEYOND 7 was a 16-week, multicentre, randomised, open-label phase IV trial conducted at 51 centres in China between October 2016 and April 2018. The design of the BEYOND 7 study has been reported previously [13]. Briefly, the study consisted of a 2-week screening phase, followed by a 3-day run-in period, a 16-week treatment phase and a 1-week follow-up phase. Overweight and obese individuals (body mass index [BMI] 25–40 kg/m2; age 18–70 years) with a confirmed diagnosis of T2D for ≥ 2 years and who had uncontrolled hyperglycaemia (FPG > 9 mmol/L; HbA1c 7.5–11.0%) despite being treated with two or three OADs, were included in the study.
All eligible participants were randomised (1:1) to initiate treatment with once-daily subcutaneous injections of Gla-100 (Lantus SoloSTAR®; Sanofi-Aventis Deutschland GmbH, Frankfurt, Germany) at the standard starting dose (0.2 U/kg) or a higher starting dose (0.3 U/kg). The insulin dose was subsequently titrated throughout the study to achieve a self-monitored fasting blood glucose (SM-FBG) target of 5.6–7.0 mmol/L (see Electronic Supplementary Material [ESM] Table S1 for titration algorithm). The SM-FBG levels were recorded by each individual during the study using the sponsor-provided glucometer.
For this subgroup analysis, data from participants were assessed based on their baseline characteristics, including age (< 60 years vs. ≥ 60 years), duration of diabetes (2–10 vs. ≥ 10 years), HbA1c level (< 9% vs. ≥ 9%) and FPG level (< 11 vs. ≥ 11 mmol/L). The difference between the two treatment arms in the proportion of participants with overall confirmed hypoglycaemia (≤ 3.9 mmol/L) and symptomatic hypoglycaemia, as well as in the proportion of participants achieving an HbA1c < 7% without hypoglycaemia, all at 16 weeks, was determined in each of the abovementioned baseline characteristics subgroups. The time to first achievement of an FBG < 7 mmol/L and the change in HbA1c from baseline to week 16 were also compared between the two treatment arms in each of these subgroups.
Statistical Analyses
Log-binomial regression analysis was used to calculate an adjusted estimate of the difference between groups (estimated treatment difference [ETD]) in the proportion of participants with overall confirmed hypoglycaemia, symptomatic hypoglycaemia or an HbA1c < 7% without hypoglycaemia, in the time to first achievement of FBG < 7.0 mmol/L and in HbA1c change from baseline to week 16, after adjusting for each stratification factor (age, duration of diabetes, HbA1c and FPG). The 95% confidence intervals (CIs) for the difference was determined using normal approximation to the binomial. Non-inferiority was established if the CI values were < 10%. Heterogeneity was tested by further including each subgroup variable and its interaction with the treatment group in the log-binomial regression model for all participants and p values for the interaction were calculated.
Ethics
The BEYOND 7 study protocol was approved by the local institutional review board at each study site, and the study was conducted in accordance with the ethical standards of the institutional and/or national research committees at each centre and with the 1964 Declaration of Helsinki, as revised in 2013. All authors confirm that the study was strictly conducted as per the Good Clinical Practice guidelines and the manuscript complies with Good Publication Practice guidelines. All individuals included in the study provided written informed consent before initiating the trial. The study was registered at ClinicalTrials.gov (NCT02836704).
Results
Participant Characteristics
Overall, 1073 individuals were screened, and 892 (83.1%) were randomised to treatment. A total of 866 (97.1%) participants received ≥ 1 dose of Gla-100 and 814 (91.3%) participants completed the study (ESM Fig. S1). The baseline characteristics of participants included in the study (mean ± standard deviation: age 52.5 ± 9.7 years; BMI 27.8 ± 2.6 kg/m2) were generally similar between the two treatment arms (Table 1). A higher proportion of participants were aged < 60 years (76.6 vs. 70.9%) and male (61.6 vs. 56.4%) and had a duration of diabetes of < 10 years (73.9 vs. 68.8%) in the 0.3 U/kg treatment arm versus the 0.2 U/kg arm.
Outcomes
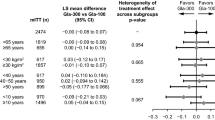
In the overall cohort, the incidence of confirmed hypoglycaemia was 11.0% in participants who started Gla-100 at 0.3 U/kg and 8.6% in those who started at 0.3 U/kg, and the incidence of symptomatic hypoglycaemia in these groups was 9.8 and 7.0%, respectively [12]. Generally, there were no significant differences between the two treatment arms in the proportion of participants with overall confirmed hypoglycaemia, symptomatic hypoglycaemia or an HbA1c < 7.0% without hypoglycaemia at 16 weeks (Fig. 1a–c), with the exception of patients with a baseline duration of diabetes ≥ 10 years who experienced more symptomatic hypoglycaemia if initiating Gla-100 at a dose of 0.3 U/kg versus 0.2 U/kg (ETD 9.94%, 95% CI 2.04–17.85; p = 0.030). Baseline age, duration of diabetes, HbA1c and FPG had no significant effect on any of these endpoints, with the exception of an increased rate of symptomatic hypoglycaemia when assessed by baseline duration of diabetes (p value for interaction 0.035).
Forest plots for the proportion of participants with overall confirmed hypoglycaemia (a), symptomatic hypoglycaemia (b) and a glycated haemoglobin < 7.0% without hypoglycaemia (c) by baseline characteristics subgroups in participants initiating insulin glargine 100 U/mL at a dose of 0.2 U/kg and 0.3 U/kg. The dotted vertical line represents a treatment difference of zero. Horizontal lines represent 95% confidence intervals. CI Confidence interval, ETD estimated treatment difference, FPG fasting plasma glucose, HbA1c glycated haemoglobin
Generally, the time to first achievement of an FBG < 7.0 mmol/L was shorter among participants treated with the Gla-100 starting dose of 0.3 U/kg than among participants in the 0.2 U/kg arm (Table 2). Among the baseline characteristics subgroups, individuals aged < 60 years, participants with an HbA1c < 9% or an HbA1c ≥ 9%, participants with a FPG < 11 mmol/L and individuals with a duration of diabetes of 2–10 years achieved an FBG < 7.0 mmol/L in a shorter time with a Gla-100 starting dose of 0.3 U/kg versus 0.2 U/kg (all p < 0.001; Table 2). In contrast, no significant difference in the time to first achievement of an FBG < 7.0 mmol/L between treatment groups was observed in individuals aged ≥ 60 years or those with a FPG ≥ 11 mmol/L. Baseline age, duration of diabetes, HbA1c and FPG had no significant effect on this endpoint (p values for interaction all > 0.1).
In general, the change in HbA1c from baseline to 16 weeks was numerically greater among participants treated with Gla-100 at the higher starting dose (0.3 U/kg) versus its standard starting dose (0.2 U/kg), although the between-group differences were not significant in any of the baseline characteristics subgroups (Table 2).
Discussion
The present post hoc analysis of the BEYOND 7 study showed that baseline age, duration of diabetes, HbA1c and FPG did not generally have a significant effect on the incidence of hypoglycaemia among Chinese individuals with T2D and uncontrolled hyperglycaemia who were treated with a higher starting dose (0.3 U/kg) of Gla-100 versus its standard starting dose (0.2 U/kg). The proportion of individuals experiencing hypoglycaemia (overall confirmed or symptomatic) or an HbA1c < 7% without hypoglycaemia, as well as the change from baseline in HbA1c at week 16 were also not significantly different between the two treatment arms in most of the baseline characteristics subgroups assessed. The only individuals in whom a difference in hypoglycaemia incidence was detected were those with a baseline duration of diabetes ≥ 10 years who experienced more symptomatic hypoglycaemia if initiating Gla-100 at a dose of 0.3 U/kg versus 0.2 U/kg. This was not unexpected since previous studies have shown that duration of T2D and insulin dose both increase the risk of hypoglycaemia [14, 15]. In these subgroups, no difference in confirmed hypoglycaemia was seen between the dose groups, which suggests that patients with a longer duration of T2D may be more alert to the symptoms of hypoglycaemia than those who have had T2D for < 10 years. These results suggest that overweight or obese individuals with T2D who have uncontrolled hyperglycaemia despite receiving treatment with OADs may benefit form a higher starting dose of basal insulin irrespective of their age at baseline, duration of diabetes, HbA1c level or FPG level.
Timely glycaemic control among individuals with T2D is important to delay the development of vascular complications [16]. However, although early initiation of basal insulin treatment is beneficial [17, 18], several barriers to insulin initiation and intensification exist, including the risk of hypoglycaemia and complexity of treatment regimens [2]. A simple and practical approach to overcoming these barriers is using a higher starting dose of basal insulin, as studied in the BEYOND 7 trial, which demonstrated shorter times to achieve FBG targets without increased risk of hypoglycaemia with a higher starting dose (0.3 U/kg) of Gla-100 versus its standard dose (0.2 U/kg) in Chinese individuals with T2D who had uncontrolled hyperglycaemia with OADs [12]. BEYOND 7 specifically enrolled people with T2D who were overweight or obese because these individuals are likely to require a higher initial dose of insulin [13]. The present analysis of the BEYOND 7 study showed that baseline characteristics, including age, diabetes duration, HbA1c and FPG, did not generally affect the greater change from baseline in HbA1c or reduced time required to achieve an FBG < 7 mmol/L seen in individuals treated with the higher starting dose of Gla-100 versus the standard dose (except in individuals aged < 60 years or those with a duration of diabetes < 10 years); however, studies in a larger population are warranted to confirm these results.
The American Association of Clinical Endocrinologists recommend a higher starting dose of basal insulin for individuals with an HbA1c > 8% [19, 20]. The present analysis showed no significant difference in the incidence of hypoglycaemia (overall confirmed or symptomatic) between the 0.3 U/kg versus 0.2 U/kg treatment groups. These results suggest that a higher starting dose (0.3 U/kg) of basal insulin is well tolerated in overweight or obese individuals with T2D, irrespective of their baseline HbA1c levels.
The main limitation of the present analysis is that it is post hoc, and therefore the original study was not powered to detect a significant treatment difference within each subgroup. Also, the effect of baseline characteristics on the incidence of nocturnal hypoglycaemia in the two treatment arms was not determined. Finally, we did not assess the effects of rapid intensive glycaemic control on visual acuity in BEYOND 7, which would have provided data on the effects of this regimen on early deterioration of diabetic retinopathy. Concerns have been raised that rapid intensive glycaemic control causes an exacerbation of diabetic retinopathy, the mechanism of which is not well understood, but long-term data suggest that sustained glycaemic control has an overall beneficial effect on microvascular complications such as retinopathy [21].
In conclusion, this post hoc analysis of the BEYOND 7 study demonstrated that the baseline age, diabetes duration, HbA1c level and FPG level of individuals did not significantly affect the incidence of overall confirmed or symptomatic hypoglycaemia among overweight or obese Chinese individuals with T2D treated with a higher (0.3 U/kg) versus standard (0.2 U/kg) starting dose of Gla-100. Individuals aged < 60 years or with a duration of diabetes < 10 years may achieve their FBG targets more quickly than those aged ≥ 60 years or with duration of diabetes ≥ 10 years.
References
American Diabetes Association. 7. Approaches to glycemic treatment. Diabetes Care. 2016;39(Suppl 1):S52–9.
Chan WB, Chen JF, Goh SY, et al. Challenges and unmet needs in basal insulin therapy: lessons from the Asian experience. Diabetes Metab Syndr Obes. 2017;10:10521–32.
Ji L, Zhang P, Zhu D, et al. Observational Registry of Basal Insulin Treatment (ORBIT) in patients with type 2 diabetes uncontrolled with oral antihyperglycaemic drugs: real-life use of basal insulin in China. Diabetes Obes Metab. 2017;19(6):822–30.
Pscherer S, Anderten H, Pfohl M, et al. Titration of insulin glargine 100 U/mL when added to oral antidiabetic drugs in patients with type 2 diabetes: results of the TOP-1 real-world study. Acta Diabetol. 2020;57(1):89–99.
Sehgal S, Khanolkar M. Starting insulin in type 2 diabetes: real-world outcomes after the first 12 months of insulin therapy in a New Zealand cohort. Diabetes Ther. 2015;6(1):49–60.
Misra A, Patel M, Agarwal P, et al. Effectiveness and safety of physician-led versus patient-led titration of insulin glargine in Indian patients with type 2 diabetes mellitus: a subanalysis of the Asian Treat to target LAntus Study (ATLAS). Diabetes Technol Ther. 2019;21(11):656–64.
Sorli C, Heile MK. Identifying and meeting the challenges of insulin therapy in type 2 diabetes. J Multidiscip Healthc. 2014;7:267–82.
Khunti K, Millar-Jones D. Clinical inertia to insulin initiation and intensification in the UK: a focused literature review. Prim Care Diabetes. 2017;11(1):3–12.
Guerci B, Chanan N, Kaur S, Jasso-Mosqueda JG, Lew E. Lack of treatment persistence and treatment nonadherence as barriers to glycaemic control in patients with type 2 diabetes. Diabetes Ther. 2019;10(2):437–49.
Berard L, Bonnemaire M, Mical M, Edelman S. Insights into optimal basal insulin titration in type 2 diabetes: results of a quantitative survey. Diabetes Obes Metab. 2018;20(2):301–8.
Blonde L, Meneghini L, Peng XV, et al. Probability of achieving glycemic control with basal insulin in patients with type 2 diabetes in real-world practice in the USA. Diabetes Ther. 2018;9(3):1347–58.
Ji L, Wan H, Wen B, et al. Higher versus standard starting dose of insulin glargine 100 U/mL in overweight or obese Chinese patients with type 2 diabetes: results of a multicentre, open-label, randomised controlled trial (BEYOND VII). Diabetes Obes Metab. 2020;22(5):838–46.
Ji L, Gao Z, Shi B, et al. Safety and efficacy of high versus standard starting doses of insulin glargine in overweight and obese Chinese individuals with type 2 diabetes mellitus inadequately controlled on oral antidiabetic medications (BEYOND VII): study protocol for a randomized controlled trial. Adv Ther. 2018;35(6):864–74.
Akram K, Pedersen-Bjergaard U, Borch-Johnsen K, Thorsteinsson B. Frequency and risk factors of severe hypoglycemia in insulin-treated type 2 diabetes: a literature survey. J Diabetes Complicat. 2006;20(6):402–8.
Silbert R, Salcido-Montenegro A, Rodriguez-Gutierrez R, Katabi A, McCoy RG. Hypoglycemia among patients with type 2 diabetes: epidemiology, risk factors, and prevention strategies. Curr Diab Rep. 2018;18(8):53.
Lovre D, Fonseca V. Benefits of timely basal insulin control in patients with type 2 diabetes. J Diabetes Complicat. 2015;29(2):295–301.
Owens DR. Clinical evidence for the earlier initiation of insulin therapy in type 2 diabetes. Diabetes Technol Ther. 2013;15(9):776–85.
Meneghini LF. Early insulin treatment in type 2 diabetes: what are the pros? Diabetes Care. 2009;32(Suppl 2):S266–9.
Handelsman Y, Bloomgarden ZT, Grunberger G, et al. American Association of Clinical Endocrinologists and American College of Endocrinology—clinical practice guidelines for developing a diabetes mellitus comprehensive care plan—2015. Endocr Pract. 2015;21(Suppl 1):1–87.
Bloomgarden ZT, Handelsman Y. Approaches to treatment 2: Comparison of American Association of Clinical Endocrinologists (AACE) and American Diabetes Association (ADA) type 2 diabetes treatment guidelines. J Diabetes. 2016;8(1):4–6.
Bain SC, Klufas MA, Ho A, Matthews DR. Worsening of diabetic retinopathy with rapid improvement in systemic glucose control: a review. Diabetes Obes Metab. 2019;21(3):454–66.
Acknowledgements
Funding
The BEYOND 7 study and this subgroup analysis were supported by Sanofi. Assistance for the development of this article, as well as the journal’s rapid service fee were funded by Sanofi. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Medical writing, editorial and other assistance
We would like to thank Nishad Parkar, PhD, of Springer Healthcare Communications for writing the outline and the first draft of the manuscript, and Catherine Rees of Springer Healthcare Communications for post-submission editorial assistance. The medical writing and editorial assistance were funded by Sanofi Aventis.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author contributions
Linong Ji, and Nan Cui participated in the trial design. Hailong Wan, Binhong Wen, Xueying Wang, Junfen Wang, Yunliang Zhang, Tao Ning, Binhong Duan, Yufang Li and Linong Ji contributed to the conduct of the trial and the data collection. Wei Feng and Xia Zhang contributed to the data analysis. All authors interpreted the data and participated in writing the report, with the support of medical writing services provided by the funder. All authors read and approved the submitted version of the report.
Disclosures
Hailong Wan, Binhong Wen, Xueying Wang, Junfen Wang, Yunliang Zhang, Tao Ning, Binhong Duan, and Yufang Li have nothing to disclose. Wei Feng, Xia Zhang and Nan Cui are employees of Sanofi China and may hold shares and/or stock options in the company. Linong Ji reported receiving consulting and lecture fees from Eli Lilly, Bristol-Myers Squibb, Novartis, Novo Nordisk, Merck, Bayer, Takeda, Sanofi, Roche and Boehringer Ingelheim and research grants from Roche and Sanofi.
Compliance with ethics guidelines
The BEYOND 7 study protocol was approved by the local institutional review board at each study site, and the study was conducted in accordance with the ethical standards of the institutional and/or national research committees at each centre and with the 1964 Declaration of Helsinki, as revised in 2013. All authors confirm that the study was strictly conducted as per the Good Clinical Practice guidelines and the manuscript complies with Good Publication Practice guidelines. All participants included in the study provided written informed consent before initiating the trial. The study was registered at ClinicalTrials.gov (NCT02836704).
Data availability
Qualified researchers may request access to participant level data and related study documents including the clinical study report, study protocol with any amendments, blank case report form, statistical analysis plan, and dataset specifications. Participant level data will be anonymised, and study documents will be redacted to protect the privacy of trial participants. Further details on Sanofi’s data sharing criteria, eligible studies, and process for requesting access can be found at: https://www.clinicalstudydatarequest.com.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wan, H., Wen, B., Wang, X. et al. Effect of Baseline Characteristics on Hypoglycaemia Risk with Insulin Glargine 100 U/mL: Post Hoc Analysis of the BEYOND 7 Study. Diabetes Ther 12, 2359–2369 (2021). https://doi.org/10.1007/s13300-021-01112-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-021-01112-z