Abstract
Introduction
International clinical trials have shown that linagliptin significantly improves glycemic control and can be used at a single dose regardless of renal function in patients with type 2 diabetes (T2D). However, to date, no studies have evaluated the use of linagliptin in Japanese patients with T2D by renal function in routine clinical care.
Methods
This was a subgroup analysis of data from a prospective observational post-marketing surveillance (PMS) study of linagliptin conducted in Japan that evaluated the safety and effectiveness of linagliptin in routine clinical care for 3 years in Japanese patients with T2D. The subgroup analysis examined the patient population of this PMS study according to renal function using estimated glomerular filtration rate (eGFR) data. The incidence of linagliptin-related adverse events (adverse drug reactions [ADRs]) was the primary endpoint, and the change in glycated hemoglobin (HbA1c) from baseline to last observation was the secondary endpoint.
Results
Of the 2235 patients included in the safety analysis, eGFR was ≥ 90 mL/min/1.73 m2 (defined as group G1) in 16.9% (n = 377), ≥ 60 to < 90 mL/min/1.73 m2 (group G2) in 44.5% (n = 995), ≥ 30 to < 60 mL/min/1.73 m2 (group G3) in 21.7% (n = 486), ≥ 15 to < 30 mL/min/1.73 m2 (group G4) in 2.6% (n = 58) and < 15 mL/min/1.73 m2 (group G5) in 1.7% (n = 37). No eGFR data were available for 12.6% (n = 282) of patients. In these GFR groups, the incidence of ADRs with linagliptin was 6.9% in group G1, 11.1% in group G2, 13.8% in group G3, 15.5% in group G4 and 16.2% in group G5; the change in HbA1c from baseline to the last observation was − 1.11, − 0.64, − 0.35, − 0.46 and − 0.54% in the respective subgroups.
Conclusions
Long-term linagliptin use showed sustained improvements in glycemic control with no new safety concerns regardless of renal function.
Trial Registration
ClinicalTrials.gov (NCT01650259).
Funding
This study was funded by Nippon Boehringer Ingelheim Co., Ltd. and Eli Lilly Japan K.K.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
This subgroup analysis of a post-marketing surveillance study, which is a regulatory requirement under Japanese Pharmaceutical Affairs Law, investigated the safety and effectiveness of linagliptin over 3 years by renal function in Japanese patients with type 2 diabetes (T2D) in routine clinical care. |
What was learned from the study? |
No new safety concerns were identified during linagliptin monotherapy for up to 3 years, irrespective of renal function; adverse drug reactions were reported in 6.9–16.2% of patients with varying levels of renal function (grouped by estimated glomerular filtration rate [eGFR]). |
Linagliptin was associated with sustained reductions in glycated hemoglobin across all eGFR subgroups. |
These findings confirm the long-term safety and effectiveness of linagliptin monotherapy in Japanese patients with T2D in routine clinical practice, regardless of renal function. |
Introduction
In 2017, the International Diabetes Federation reported that there were an estimated 7.2 million people in Japan (7.7% of the population) with diabetes and that Japan had the fifth largest diabetes-related healthcare expenditure in the world [1]. Because type 2 diabetes (T2D) is responsible for the majority of diabetes cases in Japan, management of this disease has been designated a healthcare priority by the Ministry of Health, Labor and Welfare of Japan [2].
The Japan Diabetes Society recommends monotherapy with an oral antidiabetic drug, insulin or a glucagon-like peptide-1 receptor agonist as first-line pharmacological treatment for T2D [3]. If monotherapy fails, the recommendation is that combination therapy should be initiated [3].
T2D is often associated with impaired renal function, defined as an estimated glomerular filtration rate (eGFR) of < 90 mL/min/1.73 m2, which corresponds to chronic kidney disease (CKD) stages 2–5 according to the 2012 Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guidelines [4]. T2D is one of the leading causes of end-stage renal disease [5]. In 2013, diabetic nephropathy was the most common primary disease in patients on dialysis in Japan, with 43.8% of patients starting dialysis due to this condition [6].
Results from randomized controlled trials have demonstrated that the oral dipeptidyl peptidase 4 (DPP-4) inhibitor linagliptin significantly improves glucose control without causing weight gain or increasing the risk of hypoglycemia [7, 8]. Impaired renal function can affect the pharmacokinetic properties of drugs that are eliminated primarily through the kidneys, which can in turn affect their safety and pharmacodynamic/pharmacokinetic profiles and necessitate dose adjustments [9]. Unlike other members of the DPP-4 inhibitor class, linagliptin is mostly excreted via the enterohepatic system and can be prescribed to patients with T2D as a single dose irrespective of kidney function [10, 11]. These pharmacokinetic qualities support the use of linagliptin in a broad range of patients with T2D, including those with renal microvascular complications, as well as in patients with declining kidney function [12].
In a 1-year randomized clinical trial conducted in patients with T2D and severe renal impairment, linagliptin provided clinically meaningful improvements in glycemic control with a very low risk of severe hypoglycemia [13]. The Cardiovascular and Renal Microvascular Outcome Study with Linagliptin (CARMELINA) was designed to evaluate the cardiovascular safety and kidney outcomes of linagliptin in patients with T2D at high cardiorenal risk [14]. In CARMELINA, linagliptin, when added to standard of care, demonstrated a reassuring long-term kidney safety profile, with a reduction in albuminuria progression in patients with a wide range of renal function levels [14]. However, to date, no data are available on the safety and effectiveness of the long-term use of linagliptin in Japanese patients with renal impairment in routine clinical care.
Here we present an analysis of the safety and effectiveness of linagliptin therapy for up to 3 years in patients with T2D according to renal function status, based on data from a real-world post-marketing surveillance (PMS) study.
Methods
Study Design
This was a subgroup analysis of data from a prospective observational PMS study of linagliptin conducted in Japan (ClinicalTrials.gov identifier: NCT01650259). The study protocol has been described in detail previously [15]. Briefly, patients with T2D who started linagliptin 5 mg once daily as monotherapy between July 2012 and July 2014 were enrolled from 596 clinical sites and followed for 156 weeks or until linagliptin discontinuation. As a non-interventional study, physicians made all treatment decisions based on their own clinical judgement. Treatment with other glucose-lowering drugs was permitted after enrollment because the study was intended to reflect routine clinical use of linagliptin. The incidence of adverse drug reactions (ADRs) was the primary endpoint, and the change in glycated hemoglobin (HbA1c) from baseline to the last available observation was the secondary endpoint. Other endpoints included eGFR and ADRs of special interest, including hypoglycemia, hypersensitivity, intestinal obstruction, hepatic dysfunction, pancreatitis, skin lesions, pemphigoid, infections, worsening of renal function, pancreatic cancer, cardiac failure and interstitial lung disease. ADRs were defined as adverse events (AEs) for which a causal relationship to linagliptin was definite or probable, or for which such a relationship could not be excluded. AEs were coded using the Medical Dictionary for Regulatory Activities (MedDRA; https://www.meddra.org/) version 20.1. Observational points were at baseline and at 12, 26, 40, 52, 64, 78, 104, 130 and 156 weeks after initiation of linagliptin therapy, or at the time of linagliptin discontinuation.
Data Analysis
The incidence of ADRs was assessed in the safety analysis set (SAS), which included all patients who received linagliptin monotherapy, with the exception of those for whom there were no data after enrollment. The change in HbA1c from baseline to the last available observation was assessed in the effectiveness analysis set (EAS), which included all patients who were also included in the SAS, except for those for whom there were no effectiveness data and/or who did not have T2D.
Subgroup analyses of the primary and secondary endpoints were performed based on the degree of renal dysfunction, with an eGFR of ≥ 90 mL/min/1.73 m2 defined as group G1, that of ≥ 60 to < 90 mL/min/1.73 m2 as group G2, ≥ 30 to < 60 mL/min/1.73 m2 as group G3, ≥ 15 to < 30 mL/min/1.73 m2 as group G4 and < 15 mL/min/1.73 m2 as group G5.
Change in HbA1c was analyzed using a mixed model for repeated measures approach. Least squares means were computed and then averaged across repeated measures, and their respective standard errors and 95% confidence intervals (CI) were estimated. Baseline, safety and effectiveness data were summarized using descriptive statistics, which included mean and standard deviation (SD), median, minimum, maximum and 95% CI for continuous variables and frequencies and proportions for categorical variables. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA).
Ethics
This approach is fully compliant with Japanese Good Post-marketing Study Practice regulations. The protocol for this PMS was approved by the Ministry of Health, Labour and Welfare of the Japanese Government. This study involved the collection of anonymous data from clinical settings and, therefore, it was not necessary to obtain informed consent from patients. All medical institutions who agreed to provide these anonymized data signed a contract with Nippon Boehringer Ingelheim Co., Ltd. or Eli Lilly Japan K.K.
Results
Patients
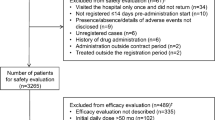
Overall, 2513 patients were enrolled, and case report forms were collected for 2415 patients (Electronic Supplementary Material [ESM] Fig. S1). Of these, 2235 patients were included in the SAS and 2054 patients were included in the EAS. Data on eGFR were available for 1953 patients in the SAS and 1830 patients in the EAS. At 156 weeks, 60.9% of patients (n = 1470/2415) continued to receive linagliptin, while 36.2% of patients (n = 874/2415) had discontinued the study. Reasons for discontinuation included AEs (5.3%, n = 127/2415), improvement (4.3%, n = 105/2415), lack of efficacy (5.9%, n = 143/2415), loss to follow-up (18.0%, n = 435/2415) and other reasons (2.7%, n = 64/2415). In the overall population, most patients (82.3%) received linagliptin as monotherapy, with no additional glucose-lowering drugs. The median duration of linagliptin monotherapy was 153.7 weeks.
Most patients in the SAS with eGFR data were in group G2 (44.5%); 21.7% of patients were in group G3; 16.9% were in group G1; 2.6% were in group G4; and 1.7% were in group G5 (Table 1). A history of cardiovascular disease was present in 4.2% of patients in stage G1, 13.3% in stage G2, 23.7% in stage G3, 48.3% in stage G4 and 29.7% in stage G5.
Safety
The incidence of ADRs was 6.9% in group G1 (n = 26/377), 11.1% in group G2 (n = 110/995), 13.8% in group G3 (n = 67/486), 15.5% in group G4 (n = 9/58) and 16.2% in group G5 (n = 6/37) (Table 2). The incidence of constipation was 0.5% in group G1, 0.9% in group G2, 1.7% in group G3, 1.7% in group G4 and 2.7% in group G5.
Cardiac ADRs occurred in ten patients (1.0%) in group G2, seven patients (1.4%) in group G3, one patient (1.7%) in group G4 and one patient (2.7%) in group G5.
Hypoglycemia was reported in two patients (0.2%) in group G2 and one patient (0.2%) in group G3 (ESM Table S1).
In the entire population of patients for whom eGFR data were available, the mean ± SD eGFR was 70.89 ± 24.21 mL/min/1.73 m2 prior to the initiation of linagliptin therapy (n = 1770) and 68.43 ± 26.51 mL/min/1.73 m2 at the last observation (n = 1577). The mean ± SD change in eGFR from baseline to the last observation was − 1.91 ± 17.14 mL/min/1.73 m2. Renal function remained stable during the study period in all eGFR groups (Fig. 1).
Effectiveness
A decrease in HbA1c over time was observed in all eGFR groups (Table 3; Fig. 2). The mean change in HbA1c from baseline to the last observation was − 1.11% (SD 1.76, 95% CI − 1.29 to − 0.92) in group G1, − 0.64% (SD 1.09, 95% CI − 0.71 to − 0.57) in group G2, − 0.35% (SD 0.96, 95% CI − 0.44 to − 0.26) in group G3, − 0.46% (SD 0.90, 95% CI − 0.71 to − 0.21) in group G4 and − 0.54% (SD 0.80, 95% CI − 0.85 to − 0.23) in group G5 (Fig. 3).
Discussion
This subgroup analysis examined the safety and effectiveness of long-term linagliptin therapy according to renal function.
In the present PMS study, 26% of patients had an eGFR of < 60 mL/min/1.73 m2 (groups G3–G5) and 4.3% had an eGFR of < 30 mL/min/1.73 m2 (groups G4 or G5). This finding is consistent with a previous analysis of Japanese patients with T2D who were on DPP-4 inhibitors (n = 162,116), in which there were more patients with an eGFR status of G4 or G5 on linagliptin (26%) than on any other DDP-4 inhibitor (2–14%) [16].
In the present analysis, the incidence of ADRs in patients on linagliptin ranged from 6.9 to 16.2% during the observation period, with fewer ADRs observed in patients whose renal function was less impaired. Likewise, in pooled analyses of randomized controlled trials, the incidence of ADRs with linagliptin was highest among patients with an eGFR of < 60 mL/min/1.73 m2 (groups G3–G5) [17], and this incidence remained similar to that observed in patients who received placebo [17, 18].
Approximately 50% of patients with T2D globally also show some evidence of CKD; CKD is also one of the strongest risk factors for cardiovascular events [19, 20]. In patients with T2D, reduced renal function is associated with an increased risk of cardiovascular events, such as cardiovascular death, nonfatal myocardial infarction and nonfatal stroke [21]. In CARMELINA, the addition of linagliptin to standard of care was shown to be non-inferior to the addition of placebo for time to first occurrence of cardiovascular death, non-fatal myocardial infarction or non-fatal stroke (3P-MACE) in patients with a wide range of eGFR levels over a median of 2.2 years [14]. In the present study, the incidence of cardiac ADRs increased with worsening renal impairment, ranging from 1.0% in group G2 to 2.7% in group G5. The proportion of patients with a history of cardiovascular disease at baseline also tended to be higher in those with more severe renal impairment.
The risk of hypoglycemia is increased in patients with an eGFR of < 60 mL/min/1.73 m2 (groups G3–G5) for a variety of reasons, including longer duration of action of some glucose-lowering agents (e.g. sulfonylureas and insulin), caloric deprivation and the scarcity of gluconeogenic precursors that occurs with declining renal function [22]. In the present study, the incidence of hypoglycemia was low (two patients [0.2%] in group G2 and one patient [0.2%] in group G3). There appeared to be no correlation between the incidence of hypoglycemia and renal dysfunction, but this could be due to the low numbers of patients in groups G4 (n = 58) and G5 (n = 37) in this study.
Across all renal function groups, eGFR remained stable throughout the entire 3-year study period. These results are in line with those of previous randomized, placebo-controlled studies of linagliptin [13, 23], although these earlier randomized studies were of shorter duration (1 year) than this PMS study (3 years).
The present study also showed that reductions in HbA1c were maintained throughout the 3-year treatment period regardless of renal function. The magnitude of the mean reductions in HbA1c tended to be numerically greater in eGFR groups with higher HbA1c at baseline, although no statistical comparison was undertaken.
This study has a number of limitations. Firstly, all findings were summarized using descriptive statistics, and no statistical tests were performed as this was a PMS study requested by the Japanese Pharmaceuticals and Medical Devices Agency to confirm the safety of linagliptin in routine clinical practice [15]. Secondly, this was a single-arm study that was not designed to compare the safety and effectiveness of linagliptin with any other intervention. Lastly, analyses to control for potential confounding factors during linagliptin therapy, including the use of concomitant drugs and alterations to diet and exercise, were not performed. These limitations are shared with the primary analysis [15] and result from the fact that this study was conducted in the real-world setting.
Conclusion
The findings of this subgroup analysis are important in that they confirm the safety and effectiveness of long-term linagliptin therapy in Japanese patients with T2D by renal function in routine clinical practice. No new safety concerns were identified, and linagliptin was associated with sustained improvements in glycemic control regardless of renal function.
References
International Diabetes Federation (IDF). IDF diabetes atlas 8th edition. 2017. https://www.idf.org/e-library/epidemiology-research/diabetes-atlas/134-idf-diabetes-atlas-8th-edition.html. Accessed 13 Aug 2019.
Neville SE, Boye KS, Montgomery WS, et al. Diabetes in Japan: a review of disease burden and approaches to treatment. Diabetes Metab Res Rev. 2009;25:705–16.
Haneda M, Noda M, Origasa H, et al. Japanese clinical practice guideline for diabetes 2016. J Diabetes Investig. 2018;9:657–97.
Stevens PE, Levin A. Evaluation and management of chronic kidney disease: synopsis of the Kidney Disease: Improving Global Outcomes 2012 clinical practice guideline. Ann Intern Med. 2013;158:825–30.
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2012;35:1364–79.
Masakane I, Nakai S, Ogata S, et al. An overview of regular dialysis treatment in Japan (as of 31 December 2013). Ther Apher Dial. 2015;19:540–74.
Barnett AH, Huisman H, Jones R, et al. Linagliptin for patients aged 70 years or older with type 2 diabetes inadequately controlled with common antidiabetes treatments: a randomised, double-blind, placebo-controlled trial. Lancet. 2013;382:1413–23.
Gallwitz B, Rosenstock J, Rauch T, et al. 2-year efficacy and safety of linagliptin compared with glimepiride in patients with type 2 diabetes inadequately controlled on metformin: a randomised, double-blind, non-inferiority trial. Lancet. 2012;380:475–83.
U.S. Food and Drug Administration. Pharmacokinetics in patients with impaired renal function—study design, data analysis, and impact on dosing and labeling. 2010. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/pharmacokinetics-patients-impaired-renal-function-study-design-data-analysis-and-impact-dosing-and. Accessed 13 Aug 2019.
Blech S, Ludwig-Schwellinger E, Grafe-Mody EU, Withopf B, Wagner K. The metabolism and disposition of the oral dipeptidyl peptidase-4 inhibitor, linagliptin, in humans. Drug Metab Dispos. 2010;38:667–78.
Graefe-Mody U, Friedrich C, Port A, et al. Effect of renal impairment on the pharmacokinetics of the dipeptidyl peptidase-4 inhibitor linagliptin. Diabetes Obes Metab. 2011;13:939–46.
Friedrich C, Emser A, Woerle HJ, Graefe-Mody U. Renal impairment has no clinically relevant effect on the long-term exposure of linagliptin in patients with type 2 diabetes. Am J Ther. 2013;20:618–21.
McGill JB, Sloan L, Newman J, et al. Long-term efficacy and safety of linagliptin in patients with type 2 diabetes and severe renal impairment: a 1-year, randomized, double-blind, placebo-controlled study. Diabetes Care. 2013;36:237–44.
Rosenstock J, Perkovic V, Johansen OE, et al. Effect of linagliptin vs placebo on major cardiovascular events in adults with type 2 diabetes and high cardiovascular and renal risk: the CARMELINA randomized clinical trial. JAMA. 2019;321:69–79.
Yamamoto F, Unno Y, Ikeda R, Ochiai K, Hayashi N. Long-term safety and effectiveness of linagliptin in Japanese patients with type 2 diabetes mellitus: a 3-year post-marketing surveillance study. Diabetes Ther. 2019. https://doi.org/10.1007/s13300-019-00723-x.
Kadowaki T, Sarai N, Hirakawa T, et al. Persistence of oral antidiabetic treatment for type 2 diabetes characterized by drug class, patient characteristics and severity of renal impairment: a Japanese database analysis. Diabetes Obes Metab. 2018;20:2830–9.
Lehrke M, Marx N, Patel S, et al. Safety and tolerability of linagliptin in patients with type 2 diabetes: a comprehensive pooled analysis of 22 placebo-controlled studies. Clin Ther. 2014;36:1130–46.
Ning G, Bandgar T, Hehnke U, Lee J, Chan JCN. Efficacy and safety of linagliptin in 2681 Asian patients stratified by age, obesity, and renal function: a pooled analysis of randomized clinical trials. Adv Ther. 2017;34:2150–62.
Gansevoort RT, Correa-Rotter R, Hemmelgarn BR, et al. Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet. 2013;382:339–52.
Thomas MC, Cooper ME, Zimmet P. Changing epidemiology of type 2 diabetes mellitus and associated chronic kidney disease. Nat Rev Nephrol. 2016;12:73–81.
Ninomiya T, Perkovic V, de Galan BE, et al. Albuminuria and kidney function independently predict cardiovascular and renal outcomes in diabetes. J Am Soc Nephrol. 2009;20:1813–21.
Tuttle KR, Bakris GL, Bilous RW, et al. Diabetic kidney disease: a report from an ADA Consensus Conference. Diabetes Care. 2014;37:2864–83.
Laakso M, Rosenstock J, Groop PH, et al. Treatment with the dipeptidyl peptidase-4 inhibitor linagliptin or placebo followed by glimepiride in patients with type 2 diabetes with moderate to severe renal impairment: a 52-week, randomized, double-blind clinical trial. Diabetes Care. 2015;38:e15–7.
Acknowledgements
The authors thank all the participants in this study.
Funding
Nippon Boehringer Ingelheim Co., Ltd. and Eli Lilly Japan K.K. funded this study and the Rapid Service Fee. As this study was conducted by the manufacturer to comply with regulatory requirements, Nippon Boehringer Ingelheim Co., Ltd. and Eli Lilly K.K. were involved in the study design, data collection, data analysis and preparation of the manuscript.
Medical Writing Assistance
We would like to thank Georgii Filatov of Springer Healthcare Communications for medical writing support in the preparation of this manuscript. Funding for medical writing assistance was provided by Nippon Boehringer Ingelheim Co., Ltd.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for the final version to be published.
Authorship Contributions
Rie Ikeda and Kaori Ochiai made substantial contributions to conception and design; Rie Ikeda made substantial contributions to data acquisition and analysis; Kaori Ochiai provided statistical expertise; all authors contributed to data interpretation, drafting the manuscript, revising for important intellectual content and approval of the final version.
Disclosures
Fumiko Yamamoto, Rie Ikeda, Naoyuki Hayashi and Tomoo Okamura are employees of Nippon Boehringer Ingelheim Co., Ltd. Tetsuaki Hirase is an employee of Eli Lilly Japan K.K., and Kaori Ochiai is an employee of the EPS Corporation.
Compliance with Ethics Guidelines
This approach is fully compliant with Japanese Good Post-marketing Study Practice regulations. The protocol for this post-marketing surveillance was approved by the Ministry of Health, Labour and Welfare of the Japanese Government. This study involved the collection of anonymous data from clinical settings and, therefore, it was not necessary to obtain informed consent from patients. All medical institutions who agreed to provide this anonymized data signed a contract with Nippon Boehringer Ingelheim Co., Ltd. or Eli Lilly Japan K.K.
Data Availability
The data that support the findings of this study are available from the corresponding author, Fumiko Yamamoto, upon reasonable request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to: https://doi.org/10.6084/m9.figshare.11418123.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Yamamoto, F., Ikeda, R., Ochiai, K. et al. Long-Term Safety and Effectiveness of Linagliptin in Japanese Patients with Type 2 Diabetes and Renal Dysfunction: a Post-Marketing Surveillance Study. Diabetes Ther 11, 523–533 (2020). https://doi.org/10.1007/s13300-019-00754-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-019-00754-4