Abstract
Healthy cornea guarantees the refractive power of the eye and the protection of the inner components, but injury, trauma or pathology may impair the tissue shape and/or structural organization and therefore its material properties, compromising its functionality in the ocular visual process. It turns out that biomechanical research assumes an essential role in analysing the morphology and biomechanical response of the cornea, preventing pathology occurrence, and improving/optimising treatments. In this review, ex vivo, in vivo and in silico methods for the corneal mechanical characterization are reported. Experimental techniques are distinct in testing mode (e.g., tensile, inflation tests), samples’ species (human or animal), shape and condition (e.g., healthy, treated), preservation methods, setup and test protocol (e.g., preconditioning, strain rate). The meaningful results reported in the pertinent literature are discussed, analysing differences, key features and weaknesses of the methodologies adopted. In addition, numerical techniques based on the finite element method are reported, incorporating the essential steps for the development of corneal models, such as geometry, material characterization and boundary conditions, and their application in the research field to extend the experimental results by including further relevant aspects and in the clinical field for diagnostic procedure, treatment and planning surgery. This review aims to analyse the state-of-art of the bioengineering techniques developed over the years to study the corneal biomechanics, highlighting their potentiality to improve diagnosis, treatment and healing process of the corneal tissue, and, at the same, pointing out the current limits in the experimental equipment and numerical tools that are not able to fully characterize in vivo corneal tissues non-invasively and discourage the use of finite element models in daily clinical practice for surgical planning.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The cornea is an in vivo pressurized dome-like tissue, constantly stimulated outwards by a net internal pressure, defined as intraocular pressure (IOP), due to the aqueous humor inside the anterior chamber of the eye. Normal IOP values range from 13 to 21 mmHg [1, 2] with cyclic fluctuations of 2–4 mmHg during the day [1], while increases may occur for multiple causes, from simpler conditions like the respiration to more severe reasons like accidental impact on the ocular surface or occurrence of ocular pathology such as glaucoma [2, 3]. Both the thickness and structural organization ensure the corneal mechanical properties needed to guarantee its functionality as protection for the inner ocular components and major refractive power of the ocular system. It has been shown that corneal biomechanics is impaired in myopic patients [4, 5], as well as in patients affected by other ocular diseases (such as keratoconus [6, 7], glaucoma [8], dry eye disease [9]). Therefore, assessing the mechanical behaviour of the cornea is clinically crucial for understanding first of all the physiological behaviour of the tissue and, in this respect, for diagnosing potential pathologies responsible for the weaking, thinning or curvature variation, and quantifying the success of refractive surgery and therapeutic treatments.
Ex vivo uniaxial tensile testing is the most spread method [10,11,12] to study corneal biomechanics, consisting in cutting a rectangular corneal specimen along a specific anatomical direction, usually including a portion of the sclera used to grip the specimen by the mechanical clamps of a tensile machine. The sample is generally stretched with a defined velocity of elongation, and the resulting force is measured and converted to the stress as the ratio between the load and the original cross-section area of the sample. There are many implemented protocols, which can also quantify the time-dependent proprieties (i.e., stress relaxation [12,13,14,15,16,17,18] and cyclic tensile loadings at different strain rates [19, 20] to reproduce slow actions due to IOP variation with posture change and fast actions as accidental impacts [20]) and failure behavior [10, 11, 15,16,17,18, 21,22,23,24,25,26]. Inflation tests were used for structural analysis to overcome the limitations of tensile tests, such as cutting of the samples which may alter the corneal microstructural arrangements and flattening of the corneal curvature, and to propose a more physiological-like environment, assessing more reliably the corneal mechanical properties. They consist of inflating corneal buttons or eye globes by using artificial chambers or ad hoc developed instruments, at an imposed pressure or volume. The main protocols adopted were loading-unloading tests, by increasing-decreasing pressure, and creep tests, where the pressure was maintained constant [12, 27, 28]. By ex vivo tests, the mechanical properties of the corneas, such as Young’s Modulus, tensile strength, and apical displacement, were measured in healthy conditions but also in samples lesioned by means of alkali solution simulating melting ulcers [14, 24] or treated with cross-linking (CXL) by means of the combined action of riboflavin drops and UVA irradiation [14, 29,30,31,32,33,34].
Although ex vivo techniques are relatively simple and low cost and have contributed over the years to achieve important levels of the current knowledge on corneal biomechanics, the interest in direct methods to assess the in vivo mechanical behaviour is growing nowadays. Currently, there are mainly two clinical instruments available, the Ocular Response Analyzer (ORA) and the Corvis ST [7], both studying the dynamic applanation of the cornea in response to an air puff of short duration on the tissue external surface. They provide output parameters related to the characteristics of the puff, which are different from each other and with the ex vivo parameters, so direct comparisons in the measurement of cornea Young’s Modulus cannot be performed.
However, starting from the experimental-derived evidence, novel promising approaches can be introduced by computational modelling, in particular finite element methods (FEMs), that are applied successfully in several surgical fields [35,36,37,38,39] and are spreading also in ophthalmic research [40, 41]. Reliable FEMs require to be validated by means of strong comparisons with physical reality, by implementing healthy and pathological conditions, simulating the experimental set-ups and obtaining numerical results able to correctly report what has happened in clinics or labs. This in silico methodology is complex, time-consuming, expensive [42] and has to be performed meticulously but, once it is completed, a computational clinical tool can be exploited in several ways: quantifying numerically the changes in IOP better and not invasively, improving corrective surgical procedures, optimizing preclinical patient evaluation, personalizing treatments and predicting alterations anticipating diagnosis.
Therefore, given the several samples’ species, conservation and cutting methods, numerous setups and the variety of testing machines, this review was aimed at providing a summary of the recent ex vivo and in vivo experimental studies, highlighting the differences among the works, the results and the limitations of these approaches. At the same time, this work was intended to propose the high-impact potentialities of the computational approach if properly validated with experimental methods, pointing out the extreme variability in terms of geometry, finite element discretization, material formulations and boundary conditions that made them appropriate for basic research, but too immature for surgery and diagnostics.
Methods
Study design
A systematic review was performed using the search engines PUBMED and SCOPUS and the search terms “([{cornea} AND {mechanic* OR stiff*} AND {properties} AND {tensile OR inflation OR indentation OR in vivo OR FEM OR simulation}]).” Searches were limited to the English language and to year of publication from 2001 to 2023 for ex vivo and in vivo studies and from 2014 to 2023 for in silico studies. The latest search was performed on 2th September 2023. PICO framework helped in developing studies evaluation:
P (population/problem): assessing corneal biomechanics.
I (intervention or exposure): experimental and numerical techniques.
C (comparison): ex vivo, in vivo and in silico methods.
O (outcome): testing protocols, instrumentations, samples preparation, mechanical quantities, pro and cons of approaches.
Eligibility criteria
For this review, eligibility criteria included studies which employed ex vivo, in vivo and in silico techniques to mechanically characterize the human cornea or the porcine cornea, recognized in literature as the most human-like model. Studies which did not report details on the methods used for mechanical assessment or focused only on different animal species were excluded, even though some recent publications started reconsidered rabbit model [43,44,45] maybe due to the easier collection and availability. By the inspection of the titles and abstracts, 68 articles met the inclusion criteria and were reviewed by reviewers (M.V.M and I.T.): 32 studies on ex vivo techniques, 17 studies for in vivo techniques, 18 studies on in silico techniques.
Data extraction
For each study, first of all the authors’ name, year of publication, tissue species and type of testing were recorded. Subsequently, based on the nature of the test, the following information were specifically considered: for ex vivo studies, the geometry of corneal specimen and its measurement, the corneal populations, the test protocol, the experimental setup and the mechanical parameters obtained; for in vivo studies the principal methodologies focusing on instruments currently used in the clinic; for in silico studies, the goal, the geometry of the model, the technique for FE discretization, the material formulation, the boundary condition and the software used.
Methods of corneal mechanical characterization
Ex vivo studies
A standard and not-invasive procedure to collect the biomechanical properties of human and animal corneas through in vivo tests is still not been implemented. The best compromise consists of using human wastes derived from refractive surgery or animal eye cornea derived from local abattoirs, and in very few cases, human corneas obtained from eye banks. The latter is very complicated because of the shortage in having samples suitable for transplants, preferring to allocate the samples for that aim instead of for scientific testing.
In this paragraph, the existing studies on corneal biomechanics investigated by means of ex vivo uniaxial tensile testing (Table 1), inflation test (Table 2) and other mechanical tests (Table 3) are proposed, classifying them in terms of corneal species (human or porcine), typology of the test (such as, tensile up to failure, stress-relaxation or loading/unloading cycles), corneal populations analysed (such as related to the specimen orientation and/or experimental condition), measures of corneal strips, mechanical protocol and experimental setup, including the tensile machine, the corneal preservation, hydration and treatment methods. All the samples considered in the studies were extracted in healthy corneal conditions without any active pathological condition affecting the tissue. Animal corneas were generally obtained from pigs aged between 4 and 6 months from slaughterhouse [11,12,13,14,15,16,17, 19, 20, 23,24,25,26, 29, 30, 32], while human corneal specimens were harvested from cadaver donor eyes as full-thickness samples [12, 13, 22, 29, 30], or removed as stromal lenticules from the central cornea during surgery [5, 10, 21, 27, 46].
Most of studies tested corneas in the healthy condition as they were extracted, while some works investigated also the tissue mechanical behaviour in lesioned and treated conditions. Lesioned corneas with structural damage of the stromal layer, simulating melting ulcers, were obtained by means of a chemical burn due to Alkali solution by soaking the sample in NaOH [24] or by applying on its surface a paper disk soaked with NaOH [14] (Table 1). Moreover, the effect of the CXL treatment on corneal biomechanics was studied by using drops of riboflavin to the sample surface and then UVA irradiation with specific irradiance wavelength, exposition time and distance from the cornea [14, 29,30,31,32,33,34] (Tables 1, 2 and 3).
The thickness was a crucial parameter, for the quantification of the transverse section in tensile tests, but also for the development of geometries in computational modelling. The thickness was obtained by surgery data [10, 21, 22, 46] or measured by pachymetry [11, 13, 20, 25, 26, 29, 30], digital calliper [14, 24], ultrasonic thickness measurement [32], optical-magnifying scale [12] or microscope [23]. All these methods have some limitations in terms of accuracy due to thickness variation between central and peripherical regions and to tissue swelling during all the experimental procedures for sample preservation and preparation [5, 23]. Only in two studies [5, 47], the exact thickness was acquired during the testing with an optical coherence tomography (OCT) imaging. In general, the measured thickness ranged from 543.96 to 720 μm for human corneas [5, 22, 27, 46] and from 0.80 to 1.76 mm for porcine corneas [11, 20, 24,25,26, 29]. Before testing, corneas were preserved in Eusol C (Alchimia, Padova, Italy) [5, 10, 11, 20, 21, 46] or Optisol [28, 46] medium or soaked in physiological saline solution (PSS) [14, 25], 0.9% NaCl solution [48,49,50], phosphate buffer saline (PBS) [17], 5% [19], 6% [34, 51], 15% [27] or 20% Dextran solution [26] or OBSS solution (ALCON laboratories, Inc., FortWorth) [52]. In addition, different methods were adopted to hydrate corneas during the tests: by immersing the specimen in a chamber filled with Eusol-C [13, 15, 20], 5% Dextran [19], NaCl [44, 49, 50] or OBSS solution [52], by dropping PSS on the specimen surface [14], by spraying the sample with PBS [17], by using an ultrasound moistener [26, 27]. To minimize hydration before and during the test, in one study samples were coated with mineral oil [23].
The storage and hydration seemed to affect the mechanical properties of the cornea [15, 28], in particular the stiffness decreased for more hydrated corneas and the mean corneal thickness varied strongly among the different hydration conditions.
Uniaxial tensile testing
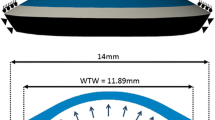
All corneas were cut in rectangular strips with length ranging from 7 to 20 mm and width ranging from 2.5 to 5 mm [11,12,13,14,15,16,17, 19, 20, 22,23,24,25,26, 29, 30], except stromal lenticules (approximately length 6.5 mm and 1 mm width) [5, 10, 21, 46]. Corneal strips were extracted along the superior-inferior (SI), nasal-temporal (NT) and/or diagonal (45° or 135°) anatomical directions.
Most of studies analysed the tensile behaviour only in one anatomical direction of the cornea (SI [13, 17, 20, 23, 29, 30], NT [14, 24]), others in both directions (SI and NT directions [10, 15, 21, 25, 44] or also in diagonal directions [11, 19, 26]) while in the remaining studies the direction was not specified [5, 12, 16, 22, 46].
Regarding the tensile instrument, the majority of the tests were performed by using Instron testing machine (model 3366 [11, 13, 20, 25], 5566 [22], 5544 [17] or 5848 [26]), while others by means of IBTC-50 tensile machine [10, 21, 44, 46], Minimat tester [29, 30], custom-built testing system [5, 24], Bose ElectroForce® Planar Biaxial Test Bench instrument [14], Ustretch device [19] and MTS SynergieEden Prairie [15]. Samples were clamped by machine grips and almost all used the sclera tissue at the ends of the specimen for the mechanical attachment [11, 13,14,15,16,17, 20, 22,23,24,25,26, 30, 44]. Multiple techniques were adopted to avoid the slippage, by using clamps with rough surfaces [10, 11, 20, 21] or with 320-grit sandpaper [26], custom grips coated with water-proof sand paper [17], by cyanoacrylate glue on surface of the ends [23] or by interposing the ends by patches of balsa wood and Velcro [14] or biological material holder [16]. Instead of clamps as other studies, only one study used BioRake (CellScale, Waterloo, Canada) attachments to test thin stromal layers, avoiding the sample squeezing and allowing some lateral contraction of the specimen [19].
A greater proportion of studies investigated the short-term mechanical response by stretching the cornea [5, 29, 30, 46] up to failure [10, 11, 15,16,17, 21,22,23,24,25,26] or through loading/unloading cycles [19, 20], while few studies investigated the long-term behaviour by stress-relaxation tests [12,13,14,15,16,17]. In tensile experiments up to failure, the typical stress-strain curve reported a nonlinear behaviour composed by an initial toe region followed by a region of higher stiffness [10, 15,16,17, 20, 21, 23, 26]. In detail, the curve can be divided in approximately four segments (Fig. 1): at the linear elastic OA segment, stress changes slowly and the strain rises rapidly; at the AB segment, a nonlinear relationship increases exponentially; at the BC segment, the relationship is approximated to a straight line; at the final CD segment, the curve reflected a nonlinear relationship where D is fracture point [10, 21, 26]. The initial two segments generally refer to normal physiological stress state of the corneal tissue (strain less than 0.1) [16, 26], and in particular, in the BC tract the Young’s Modulus is usually calculated as the curve’s slope. On the other hand, in stress-relaxation tests, the characteristic stress-time curve is shown in Fig. 1 and it can be described by an initial peak stress corresponding to the application of the sudden deformation and its subsequent gradual decrease over time up to a steady-state region where all the time-dependent phenomena are completely occurred [14,15,16,17]. Moreover, in literature, two additional tensile tests are reported: the contraction test, to measure the transversal contraction index by using an optical method [15], and the trouser tear test considering strips with a sharp notch prior to test (Table 1), to investigate the fracture toughness of the cornea [17]. In trouser tear tests, a quasi-linear increase of the load resulted at small extension up to a plateau region in which the crack started to propagate [17]. The main corneal mechanical properties obtained by the reviewed studies were grouped in terms of Young’s Modulus, failure parameters, stress-relaxation parameters, tear toughness and transversal contraction index, expect those reported by [22, 23]. Mahdian et al. [22] determined the nonlinear anisotropic fiber-reinforced hyper-viscoelastic (AFHVE) model parameters by combining the results of tensile tests up to failure on human corneal strips (Table 1) to the coupled finite element-optimization analysis to predict the tissue behavior. 8 parameters of the AFHVE model were obtained (3 for the viscoelasticity and 5 for the anisotropic hyperelasticity) and their sensitivity was evaluated by studying the convergence of the tissue response between simulation and experiment [22]. Elsheikh et al. [23] proposed a mathematical procedure to remedy the overestimation of corneal stiffness due to the inaccuracy sources of tensile tests, reducing the difference between the stiffness determined by extensometry and inflation tests approximately from 32 to 5%.
Young’s modulus
For human stromal lenticules, contrasting results in terms of Young’s Modulus in the early region of the stress-strain curve resulted under the same elongation rate of 0.01 mm s−1: for strain less than 5%, [10] obtained slightly higher values in NT direction if compared to the SI (NT: 1.30 ± 0.51 MPa; SI: 1.14 ± 0.28 MPa) while [21] showed higher values in the SI direction at stress of 0.01 MPa (NT: 1.17 ± 0.50 MPa; SI. 1.28 ± 0.70 MPa), 0.02 MPa (NT: 1.46 ± 0.47; SI: 1.57 ± 0.67 MPa) and 0.03 MPa (NT: 1.75 ± 0.45 MPa; SI: 1.84 ± 0.64 MPa).
Similarly, the SI human corneal orientation resulted statistically significantly higher also by considering the low-strain tangent modulus (LSTM) for strain less than 20% (NT: 1.17 ± 0.43 MPa; SI: 1.32 ± 0.50 MPa) and the high-strain tangent modulus (HSTM) for strain between 35% and 55% (NT: 43.59 ± 7.96 MPa; SI: 51.26 ± 8.23 MPa) [21]. By studies on human cornea with no indication about the anatomical direction investigated [5, 46], overall higher values of Young’s Modulus at stress of 0.02 MPa (2.45 ± 1.72 MPa [46]) and lower values of both LSTM (0.204 ± 0.189 MPa) and HSTM (5.114 ± 1.958 MPa) [5] were obtained if compared respectively to the corresponding values reported above [21], when different testing machine was used [5, 46] and the sample thickness was acquired during the testing by OCT imaging [5] instead of the estimation from surgery data. However, the Young’s Modulus reported by [46] resulted negatively correlated to corneal densitometry values in some corneal layers and statistically significantly positively correlated to age, probably due to the mechanical improvement for thicker collagen fibres caused by aging. LSTM and HSTM reported by [5] resulted significantly correlated with a newly introduced in vivo stiffness metric and individually the LSTM resulted positively correlated with the in vivo Corvis ST indicators related to the segment/region of the corneal surface due to the first applanation and the HSTM resulted to decrease with the degree of myopia, in agreement with previous in vivo studies [5].
For full-thickness corneas, generally, porcine samples exhibited an average slope of 3.193 ± 1.589 MPa in the low strain range up to 4% and of 41.806 ± 10.920 MPa for strain range 6 − 12% [15]. In SI direction, Young’s Modulus at 6% strain resulted, on average, 1.5 MPa and 2.7 MPa respectively in untreated and CXL treated porcine corneas and 1.3 MPa and 5.9 MPa respectively in untreated and CXL treated human ones [30]. In addition, along the depth of the tissue, in SI corneal specimens the human anterior layer resulted stiffer than the posterior one (at 5% strain, mean 3.6 MPa and 1.3 MPa for anterior and posterior samples) and a stronger effect of the CXL treatment resulted in the anterior layer (at 5% strain, mean 6.0 MPa and 1.0 MPa for anterior and posterior treated samples) [29]. The same CXL effect resulted for porcine SI corneal specimens (at 5% strain, mean 2.9 MPa [26, 29] and 6.3 MPa for untreated and treated anterior samples, while 2.8 MPa and 2.7 MPa respectively for posterior samples [29]). Therefore, considering both the total thickness and the distinction in layers, a greater increase in stiffness due to CXL treatment resulted in human corneas than in porcine ones [29, 30]. Furthermore, for porcine samples in SI direction, when two corneal layers were distinct from the anterior to the posterior surface, no difference in stiffness resulted from each other (at 5% strain, mean 2.9 MPa and 2.8 MPa respectively for anterior and posterior samples [29]), while, in case of splitting in three layers, the Young’s Modulus was found to decrease gradually along the depth (at the stress of 0.03 MPa, 2.869 ± 0.584 MPa, 2.333 ± 0.337 MPa and 1.640 ± 0.331 MPa respectively for anterior, central and posterior layers) [26]. Similarly, the stiffness reduction along the corneal thickness was also observed in the diagonal direction (at stress of 0.03 MPa 2.706 ± 0.707 MPa, 2.071 ± 0.584 MPa and 1.415 ± 0.228 MPa respectively for anterior, central and posterior layers) [26] and in the NT direction (at stress of 0.03 MPa, 2.484 ± 0.740 MPa, 2.098 ± 0.536 MPa and 1.746 ± 0.386 MPa respectively for anterior, central and posterior layers) [26]. Additionally, the Young’s Modulus for porcine NT specimens was also investigated in control and NaOH-treated conditions respectively about 10 MPa and 5 MPa, showing a significant difference between them [24].
For porcine corneas, the Young’s Moduli in different orientations were proved to be equal to each other in the anterior layer (at stress of 0.03 MPa, 2.869 ± 0.584 MPa, 2.484 ± 0.740 MPa and 2.706 ± 0.707 MPa respectively in SI, NT and diagonal directions) [26], as well as in the central layer (at stress of 0.03 MPa, 2.333 ± 0.337 MPa, 2.098 ± 0.536 MPa and 2.071 ± 0.584 MPa respectively in SI, NT and diagonal directions) [26] and in the posterior layer (at stress of 0.03 MPa, 1.640 ± 0.331 MPa, 1.746 ± 0.386 MPa and 1.415 ± 0.228 MPa respectively in SI, NT and diagonal directions) [26]. Focusing on corneal stroma at depth of 100, 350 and 600 μm, lower stiffness in the most posterior layer was confirmed even in this case [19], as well as the independence from the orientation for the anterior layers, contrary to the most posterior one exhibiting a stiffer response in the SI direction compared to the NT and diagonal directions [19]. Such stiffer behavior in SI orientation was reported also by [15], with SI porcine specimens 21% more rigid than NT ones, with significant differences for strain levels higher than 12%.
In porcine corneas, the Young’s Modulus was also studied for different strain rates [11, 17, 20] and results are related to the protocol adopted. By testing the same porcine specimen under different strain rates ranging between 0.8 and 430% min−1 (Table 1), a large (40.2% on average) and statistically significant increase of stiffness in SI orientation resulted only from 0.8 to 8% min–1, while subsequent increases in strain rate led to much lower and not statistically increase in stiffness [20]. Moreover, when different porcine specimens under different strain rates were compared, the Young’s Modulus in SI direction showed the insensitivity to the rate not only considering high and distant values (9.59 ± 1.28 MPa, 10.29 ± 0.85 MPa and 9.82 ± 1.39 MPa respectively for 3, 30 and 300 mm min−1 [17]; for 0.01 MPa stress, 0.349 ± 0.053 MPa and 0.397 ± 0.056 MPa respectively for 8.3 and 210% min−1 [11]; for 0.0 MPa stress, 1.036 ± 0.155 MPa and 1.181 ± 0.164 MPa respectively for 8.3 and 210% min−1 [11]), but also fr low strain values (for 0.01 MPa, 0.343 ± 0.064 and 0.349 ± 0.053 MPa respectively for 0.8 and 8.3% min−1 [11]; for 0.03 MPa stess, 1.016 ± 0.183 MPa and 1.036 ± 0.155 MPa respectively for 0.8 and 8.3% min−1 [11]). Similarly, small icreases of the stiffness by increasing the strain rate from low to high values were obtained also in the other orientations in porcine corneas, the NT direction (for 0.01 MPa stress, 0.379 ± 0.054 MPa, 0.382 ± 0.030 MPa and 0.423 ± 0.031 MPa respectively for 0.8, 8.3 and 210% min−1, for 0.03 MPa stress, 1.14 ± 0.155 MPa, 1.133 ± 0.090 MPa and 1.252 ± 0.090 MPa respectively for 0.8, 8.3 and 210% min−1) and the diagonal directin (for 0.01 MPa stress, 0.374 ± 0.022 MPa, 0.426 ± 0.103 MPa and 0.427 ± 0.037 MPa respectively for 0.8, 8.3 and 210% min−1; for 0.03 MPa stress, 1.19 ± 0.065 MPa, 1.249 ± 0.302 MPa and 1.264 ± 0.111 MPa respectively for 0.8, 8.3 and 210% min−1) [11]. In addition, for 0.8, 0.3 and 210% min−1 strain rates, SI and NT speciens had almost the same stiffness and appeared to be slightly stiffer than diagonal ones by about 2–13%, except for the 0.8% min−1 for which diagonal samples resulted stiffer than the NT ones by 12% [11], while for values from 0.1 to 50 mm min−1 the SI porcine specimens resulted on average 34% stiffer than the NT ones [25].
Failure parameters
The tensile behaviour up to failure can be described by means of the tensile strength, or named failure stress, as the maximum stress that the tissue can sustain before failure, the yield stress/strain, as the stress/strain at which a permanent deformation begins, and the failure strain, as the strain at which the failure happens.
The tensile strength resulted slightly larger in SI direction rather than NT direction for both human stromal lenticules (SI: 14.05 ± 1.95 MPa; NT: 13.25 ± 2.16 MPa) [10] and porcine corneas [25]. Under the same strain rate of 10 mm min−1, the average tensile strength resulted very similar for human (3.81 ± 0.40 MPa) and porcine corneas (3.70 ± 0.24 MPa), as well as the stress-strain pattern [12]. Lower values of porcine tensile strength were obtained when only the NT direction was investigated, both in control and NaOH-treated conditions (respectively about 2.5 MPa and 1 MPa) [24].
Additionally, the porcine corneal behaviour up to failure was also described, on average, by yield stress of 3.837 ± 1.312 MPa, yield strain 15.4 ± 2.4%, failure stress 4.763 ± 1.251 MPa and failure strain 19.2 ± 2.3% [15], with higher yield stress and higher failure stress in SI specimens with respect to NT ones [15].
Stress relaxation parameters
Generally, the stress-relaxation behaviour can be described by the peak stress, the stress at the end of relaxation, the relaxation percentage and the time constant [15]. Porcine corneas for 2% strain constant for 50 s exhibited a relaxation stress percentage of 16.1% from a peak stress of 0.059 ± 0.039 MPa with a time constant of 6.165 ± 1.649 s, while for 10% strain constant for 2000 s respectively the corresponding values 0.322 ± 0.049%, 0.654 ± 0.611 MPa and 471.101 ± 75.229 s [15]. The strain-dependence of the stress relaxation was observed also in [17], where the equilibrium normalized load resulted in 0.19 ± 0.02 and 0.41 ± 0.02 respectively for 2 and 4 mm displacements fixed for 120 s. On the other hand, considering stretch level up to 4 mm applied for 1000 s [16], porcine corneas exhibited, on average, the initial and the last stress respectively as 2.33 MPa and 0.88 MPa and the stress-relaxation curve was fitted by the modified Maxwell viscoelastic model (relaxation modulus E1: 0.69 MPa, E2: 0.43 MPa, E3: 0.31 MPa, E4: 0.40 MPa, E5: 0.43 MPa; relaxation time τ1: 8.83 s, τ2: 65.33 s, τ3: 876.93 s and τ4: 2.84 × 103 s) [16].
When human corneal strips of 10-mm initial length were stretched and held for 400 s with the length reached under the 4 N load [13] (Table 1), the average stress reductions resulted in 27.7 ± 5.6%, while 30.5 ± 5.7% after 800 s and 32.0 ± 5.7% after 1200 s respectively with the length under the 8 and 12 N loads [13]. The corresponding average stress reductions for porcine corneas was 49.2 ± 8.3%, 55.6 ± 8.2% and 5.2 ± 8.1% respetively after 400, 800 and 1200 s [13]. In addition, the stress-relaxation behaviour can be described also by the slope K of the normalized relaxation G(t) curve in function of a log time t and the value P of G(t) at the end of relaxation. For a stretch ratio of 1.5 (Table 1), the slope K of the G(t)-ln t and the value P for relaxation of 1000 s resulted respectively 0.0165 ± 0.0024 and 85.6 ± 1.5 for human corneas, while 0.0553 ± 0.0069 and 64.6 ± 3.3 corresponding values for porcine corneas [12]. Therefore, these studies [12, 13] showed that porcine corneas relax quicker and lose more of their initial stresses than human ones with statistically significant differences in relaxation rates [12, 13].
Moreover, stress-relaxation tests on porcine corneas were performed also in alkali-lesioned and CXL-treated conditions and following preservation in culture medium [14] (Table 1). The time-dependent behaviour of the porcine cornea resulted in being influenced by the structural modifications due to both the lesion and the CXL treatment, showing lower relaxation times if compared to the healthy corneas both in fresh and cultured conditions [14].
Tear toughness
Tear toughness of the cornea was calculated at different extension rates considering the peak force, defined as the mean load at the plateau region of the load-extension curve and the thickness of the specimen [17]. Peak force resulted larger for greater extension rates and the tear toughness exhibited values from 3.39 ± 0.57 to 5.40 ± 0.48 kJm−2, depending on the extension rate [17]. A linearly positive relationship resulted between the tear toughness and the extension rate in a semi-log plot and toughness increasing approximately by 1.00 kJm−2 for everyone order of magnitude increase in extension rate [17].
Transversal contraction index
The transversal contraction index was measured in porcine corneas which exhibited in general values greater than 0.5, confirming the tissue nonlinearity and anisotropy, and dependent on strain level: 1.005 ± 0.496, 2.082 ± 0.196 and 1.908 ± 0.237 respectively for strain of 5, 10 and 15% [15].
Inflation testing
Inflation testing has taken hold with the aim of keeping the tissue intact loading the whole structure with an internal pressure that simulates intraocular pressure. The pressure is applied by fluid injection using a water column or syringe pump that can be controlled by computer [53]. In inflation tests, the deformation of the specimens that result from the change in internal pressure is measured by a system of high-resolution digital cameras that are spatially distributed around the specimen and, together with the initial specimen size and applied pressure, is analyzed using shell analysis to determine the stress-strain behaviour of the tissue. In contrast to uniaxial tensile tests, the inflation test does not involve flattening of the tissue and separation of collagen fibrils along the edges of the specimen and for these reasons, preconditioning is rarely performed [54].
Samples may consist of the corneal component alone or the entire eyeball. Corneas are mounted on a pressure chamber and held in place using mechanical clamps. For whole globes either a needle connected to the pumping system is introduced through the optic nerve head or an air puff acting from the outside hits the cornea directly. Different protocols were used to perform inflation tests, details are reported in Table 2. The main tests consisted of cycling, creep and stress relaxation tests.
The relationship between intraocular pressure and apical elevation of the cornea was analysed in several studies [13, 31, 32, 55] on both porcine and human corneas, even in the presence of treatment, and the results showed the non-linearity of the mechanical response. The initial behaviour or toe region is located in different pressure ranges: up to 10 mmHg [13], in 12–15 mmHg range [32] or in the 2-4 kPa as physiological range [31]. Human corneas showed low stiffness up to pressure values of about 15–20 mmHg, while later stiffness increased [13]. Furthermore, human eye showed higher stiffness at the limbal region reducing gradually towards the posterior pole, while the central cornea had a higher stiffness than the peripheral cornea [51]. Pig corneas showed nonlinear behaviour with a less gradual transition respect human ones from the initial stage of low rigidity to the final stage with greater rigidity. Porcine corneas treated with CXL had a lower corneal apex elevation at all loading stages compared to untreated corneas [31]. Moreover, the relationship between Young’s Modulus (calculated on the basis of shell theory [56]) and IOP appeared to be linear. Bao et al. [32] demonstrated that porcine corneas treated with CXL had a higher stiffness (Young Modulus 356 ± 159 kPa) respect untreated ones (Young Modulus 247 ± 169 kPa) in the region 2–4 kPa. The average Young’s Modulus of the human anterior cornea ranged between 2.28 and 3.30 MPa in specimens with and without intact epithelium, respectively, while for the posterior cornea was on average 0.21 and 0.17 MPa, respectively [27].
The stress-strain relationship was also identified using the pressure rise and the specimen dimensions, resulting non-linear as well. In details, the study by Elsheikh et al. [13] for human corneas reported an exponential equation that was derived for each age range, while a third-grade polynomial equation for the porcine corneas. A comparison among species revealed that porcine corneas appeared to have lower initial and final stiffness values than all groups of human corneas. In the creep tests [13], a gradual decrease in mean human corneal creep was recorded with the increase of age. In addition, porcine corneas experienced significantly more creep deformation than all human corneas, and the overlap between porcine and human creep time results was limited to the early stages of the test, beyond which there was a clear separation. Also, another study [27] reported differences between anterior and posterior human cornea with and without epithelium. The results showed that the anterior cornea of specimens with epithelium took a longer time to relax compared to that without epithelium and when the load was released the specimens with epithelium recovered corneal strain faster. The posterior cornea of specimens with epithelium showed a slower creep response to sudden stress application than specimens without epithelium. After sudden stress release, no immediate elastic recovery of the posterior cornea was found in a few samples. A permanent strain was found immediately after stress release [27]. In Kling et al. [33], corneal buttons and whole eye globes were compared showing that the sclera slightly affected the temporal symmetry, while the ocular muscles drastically changed the amount of corneal recovery. CXL produced a change in the viscoelastic properties with treatment. In another study, Kling et al. [28] demonstrated that the mechanical response was influenced if the corneas were treated with different solutions. Dehydration induced by dextran solution increased the hysteresis after the inflation cycle, while corneas treated with 0.125% riboflavin–20% dextran recorded higher strains, indicating a softening of the corneal tissue compared to untreated corneas and corneas treated with 8% dextran and 20% dextran.
Other mechanical testing
Other ex vivo methods were also used to study the mechanical properties of cornea (Table 3). By indentation test in creep condition, the effect of the CXL treatment was studied in human corneas (age ranged from 48 to 98 years) [34]. A significant increase in Young’s Modulus from the peripheral to the central region resulted for both the control (23.2 ± 5.7 kPa, 36.4 ± 12.5 kPa and 43.2 ± 12 kPa respectively for peripheral, paracentral and central regions) and CXL-treated corneas (37.7 ± 20.4 kPa, 65.0 ± 17.9 kPa and 89.9 ± 42.4 kPa respectively for peripheral, paracentral and central regions) [34]. In addition, the stiffness of the central and paracentral regions increased almost two times after the crosslinking, while not significantly difference resulted for the peripheral region. The creep value, defined according to ISO 14,577, resulted lower in the central and paracentral regions for both the control (62.3 ± 15.7%, 73.3 ± 30.4% and 61.6 ± 15.0% respectively for peripheral, paracentral and central regions) and the CXL-treated corneas (52.3 ± 13.2%, 49.1 ± 14.9% and 4.6 ± 14.7% respetively for peripheral, paracentral and central regions), with a ~ 30% lower value for the treated samples in the central and paracentral regions rather than in control corneas for the same regions [34].
Ex vivo indentation was performed also on porcine corneas to test a new method to measure the IOP-dependent corneal tangent modulus in vivo [47]. Results showed corneal elasticity ranged from 0.05 to 0.55 MPa for IOP from 10 to 40 mmHg and rate-independent at rates > 20 mm min−1.
Additionally, two studies performed unconfined compression tests on porcine corneal stroma (Table 3) and determined the out-of-plane Young’s Modulus as the slope of the equilibrium stress-strain curve and the in-plane Young’s Modulus and the permeability coefficient by fitting the experimental data with a transversely isotropic bi-phasic model [49, 50]. By increasing the compressive strain, the in-plane Young’s Modulus (on average, 1.33 ± 0.51 MPa) linearly increased with increasing strain while out-of-plane Young’s Modulus (on average, 5.61 ± 2.27 kPa) was almost independent of the compressive strain [49]. On the other hand, the permeability coefficient (average 2.14 ± 0.68 × 10−14 m4/N s) decayed exponentially with increasing strain [49].
Considering also different displacements rates, the in-plane Young’s Modulus increased with increasing strain (such as, 0.7 ± 0.2 MPa and 1.6 ± 0.2 MPa respectively for 4 and 16% strain at 0.15 μm s−1, while 0.8 ± 0.2 MPa and 2.9 ± 0.6 MPa respectively for 4 and 16% strain at 1.00 μm s−1), while the permeability coefficient decayed with increasing compressive strain (such as 3.1 ± 0.6 × 10−14 and 1.7 ± 0.3 × 10−14 m4/N s respectively for 4 and 16% strain at 0.15 μm s−1, while 5.4 ± 1.3 × 10−14 and 2.6 ± 0.1 × 10−14 m4/N s respectively for 4 and 16% strain at 0.15 μm s−1) [50]. Regardless of loading rates and compressive strains, a range of out-of-plane Young’s Modulus of 0.6 kPa to 13.8 kPa, in-plane Young’s Modulus of 0.5 MPa to 4.8 MPa, and permeability coefficient of 1 to 7 × 10−14 m4/N s were found [50], in accordance to [49] .
Furthermore, Dynamo-Mechanical Analysis tests were conducted according to torsional shear conditions at different levels of compressive strain on porcine corneas [52], showing average shear storage modulus and loss modulus respectively from 2 to 8 kPa and from 0.3 to 1.2 kPa and increased shear moduli by increasing the compressive strain. By varying the shear strain level at the same frequency, the loss modulus was almost constant, while the storage modulus exhibited a sudden drop at shear strain larger than about 1.5%. In addition, at the same shear amplitude, the storage modulus increased at each compressive strain step [52].
In vivo studies
In vivo techniques are gaining importance in clinical ophthalmology for the assessment of corneal biomechanics because of the need to avoid the disruptive action performed by ex vivo experimentations. Techniques currently available and in development can be divided between perturbatory, consisting in imposing an external load, and non-perturbatory techniques that collect innate properties of corneal tissue [57]. In the first category, ORA and Corvis ST appear in the in vivo biomechanical testing characterized by high-speed and high-magnitude dynamic deformation of the cornea under air-puff excitation to identify the abnormities in the morphological and biomechanical properties of the cornea. They combine in vivo optical imaging systems with an in-situ non-contact air-puff tonometer, thus they can assess a series of high-speed dynamic biomechanical parameters of the cornea [58,59,60,61,62]. They are the only tests used in clinical medicine. Digital Imaging Correlation (DIC) method was applied to the in vivo high-speed corneal deformation measurement in combination with the Corvis ST tonometer, permitting spatiotemporal dynamic strain/strain rate maps of the cornea at the tissue for the clinical recognition and diagnosis of keratoconus at a more underlying level [63] .
The promising aspect of Corvis ST consists in the possibility to link Corvis ST data to material stiffness parameter, which are quantities more used to describe biological tissues, by using a new algorithm, the stress-strain index (SSI) algorithm, which proposed.
a stress-strain curve for a given cornea based on finite element modelling and generates a property that is largely independent of IOP and corneal thickness, two confounders of biomechanical property measurement [64].
A study with a follow-up of about 41 months revealed a significant reduction in corneal stiffness expressed by a significant reduction in the SSI, demonstrating that in-vivo biomechanical deterioration occurred with keratoconus progression [65].
Other not-used-in-clinics techniques are Brilluoin optical microscopy [66, 67] that, together with Phase-decorrelation OCT [57], corneal indentation [68], estimation of Young’s Modulus based on a fluid-filled spherical shell model with Scheimpflug imaging [69] and ultrasound surface wave elastography [70,71,72] and optical coherence elastography to measure shear modulus of the human cornea [71] fall into the non-perturbatory techniques. Despite the capability of evaluating in vivo corneal biomechanics in combination with in-situ loading and/or imaging technologies, these methods still face challenges in addressing the issue on high-speed biomechanical measurements and the nonlinear material behaviour of the cornea.
In silico studies
As reported in the previous paragraphs, an optimal understanding of corneal biomechanical features is essential to analyse not only the refractive surgical procedures and their consequences in terms of stiffness and microstructure, but also the effects of corneal treatments, such as CXL, in order to predict side effects and avoid them, to detect eventual weakening or enhancement of corneal mechanical response and to improve the management of ectatic corneal diseases. Advances in computational modelling have the potential to enhance diagnosis, enable personalized risk assessment, and optimize treatment design toward the goal of improving safety and outcomes for corneal and refractive surgery patients [73].
At the state of art, FE models of cornea and whole eye have been developed for different purposes: to prevent complications after modern laser refractive surgical procedures and iatrogenic ectasia [74], to study the mechanical response of the cornea subjected to a non-contact air-jet tonometry differentiating the contributions related to geometry, the corneal material behaviour and the loading [75], to analyse the blunt impact of foreign bodies [3], to study the effect of surgical factors on the cornea, to improve keratoconus treatment [41, 76, 77], to analyse the wave propagation for a better understating the differences between healthy subjects and glaucoma patients [78], to measure the deformation after airbag impact [79] and to quantify the biomechanical change caused by the LASIK flap [80]. The most ambitious goal stays on the development of a daily clinical computational tool for the planning and optimization of corrective procedures and in preclinical optimization of diagnostic procedures [40], permitting the personalization of the surgical procedure [81] by using a multi-physics model that permits not only to analyse biomechanical aspects, but also treatments, as CXL, by adding the migration of the riboflavin (i.e., the photo-initializer), UV light absorption, the photochemical reaction that forms the cross-links, and biomechanical changes caused by changes to the microstructure [82].
For what concerns the biomechanical aspects, the geometry and the constitutive formulation of the material vehiculate the outputs. Numerous studies simplified the cornea as a linear, time-independent and isotropic material [76, 78, 79], omitting the “true” mechanical aspects of corneal tissues. More sophisticated papers described the corneas as a material presenting all or part of the following features: anisotropy, visco-hyperelasticity and inhomogeneity [3, 40, 74, 75, 81], respecting more the experimental evidences and permitting more solid simulations-derived considerations.
The ideal geometry consists of a 3D patient-specific cornea (or whole eye ball) [75] obtained from biomedical images or tool as Pentagram or Corvis, avoiding spherical shape, with a thickness differentiated by region. The FE mesh is another crucial parameter, and the number of nodes and elements depends on the geometry, element type and the level of accuracy that has to be reached. A sensibility mesh analysis is encouraged with a proper number of elements describing the thickness. More details about the FE models are reported in Table 4.
The results proposed by the numerous analysed studies differed in the mechanical quantities that were proposed and varied according to the imposed boundary conditions, the aim of the study and the methodology adopted. For these reasons, the potentialities and the main evidence are reported below but for details the authors invite to refer to the corresponding paper (a list is reported in Table 4).
FE models can analyse vast scenarios and consider the multiple factors, which play a role in the results, differing each single contribution, while this differentiation is not possible in experimentations, unless having at disposal a varied and numerous animal/human samples, making the tests expensive and time-consuming. In fact, Whitford et al. [40] isolated the age-related stiffening behaviour from the age-related viscoelastic changes and Shih et al. [74] found out that the Bowman’s membrane and Descemet’s membrane accounted for 20% of the bending rigidity of the cornea and became the force pair dominating the bending behaviour of the cornea. Also, the relationship among the main quantities as corneal apex displacement, internal ocular pressure (IOP), global and local stress and strain were analysed: Ariza-Gracia et al. [75] showed that the maximum apex displacement varied linearly with IOP, while it followed a cubic relation with corneal thickness. For what concerns the corneal pathology analysis, Karimi et al. [77] revealed the important role of stress among healthy and keratoconus eyes, since healthy eyes showed a higher amount of stress compared to the keratoconus ones, leading to a bigger and more tolerated deformation in health eyes compared to the keratoconus ones. Baek at al [76]. studied the effect of surgical factors on the deformation and curvature of the cornea, finding out that if the suturing depth increased, the local curvature did not significantly change, but the contact position between the thread and the cornea was modified. Curvature variations eventually led to changes in light refraction, which greatly affected the recovery of the patient’s visual acuity. Bagheri et al. [81] and De Oteyza et al. [41] studied the intracorneal ring segment as a keratoconus treatment finding that increasing ring thickness and base width along the arc of the asymmetric ring segment produced a more pronounced flattening in this part of the ring. The asymmetric ring design did find a good balance between maximizing corneal flattening at one end and minimizing it at the other end, compared to the isolated effect of ring thickness and width. Fang et al. [80] studied the LASIK surgery and affirmed that the changes in the biomechanical properties of cornea after refractive surgery should not be ignored because the results showed that the corneal flap can cause the deformation of the anterior cornea and the displacement was enough to change aberrations and stress/strain distribution.
Discussion
In this work, corneal biomechanics has been studied considering ex vivo, in vivo and in silico techniques, highlighting the differences among methodologies, instruments, protocols, and conditions applied, and analysing them by their intended purpose.
All the reported experimental and numerical studies were affected by limitations, some of which inevitable because of the need to simplify the physiological eye conditions, while others more related to the nature of tests.
Comparing different studies result almost impossible for several reasons. A single experimental curve (such as stress-strain relation) has a limited meaning in the comprehensive assessment of the tissue biomechanical properties, as each mechanical test and each specific protocol allow to study only one feature. In addition, there are many variables that can influence the accuracy of the results and cause the discrepancy among studies, as the origin of the samples, the presence of the epithelium and/or endothelium, the methods for preservation and hydration, the testing machine and protocol and the experimental conditions [5, 15] according to the tissue mechanical properties intended to be analysed. Higher values of loading rate (such as, 4.17 mm s−1 [12] or 80 mm s−1 [14] ) were usually used to simulate an ideally instantaneous application of a certain deformation level in case of stress-relaxation tests, while lower values were considered when the interest laid on the tissue response during elongation (such as, 0.01 mm s−1 [10, 21, 46] for tensile up to failure). There was not a strong guideline in choosing loading rate and other protocol parameters, depending on the typology of the properties. Also, the lack of a standardized post-processing analysis technique of experimental results, used for the extraction of mechanical parameters, makes it risky to draw some conclusions in terms of single values (i.e.: comparison of Young’s moduli). For instance, both [10, 21] performed tensile tests up to failure on human stromal lenticules under the same elongation rate but contrasting results are reported regarding the Young’s Modulus values obtained in NT and SI directions: by [10] the NT direction exhibited higher values than the SI direction (NT: 1.30 ± 0.51 MPa; SI: 1.14 ± 0.28 MPa) while the opposite was obtained by [21] (NT: 1.46 ± 0.47; SI: 1.57 ± 0.67 MPa). Additionally, when also different techniques are used, the comparison between the values could lead to confusion among the results if the procedure of the testing method is not taken into account: such as, Young’s Modulus for porcine corneas reported on average as 1.5 MPa by tensile test at 6% strain [30] and as 247 ± 169 kPa by inflation test for IOP between 2 and 4 kPa [32]; for corneas treated with CXL, Young’s Modulus increased in both tensile (2.7 MPa at 6% strain [30]) and inflation tests (356 ± 159 kPa for IOP between 2 and 4 kPa [32]). Also in vivo studies (i.e., Corvis ST approach) can estimate the Young’s Modulus obtaining values around 0.2 MPa, however the Young’s moduli reported in the literature were within the range of 0.1–10 MPa from in vitro tests [87], making assumptions and clinically applications still complex. The major restriction in the corneal experimentations regards the difficulty in harvesting intact human samples in sufficient amounts. Among the 32 ex vivo studies reviewed, few works tested human corneal specimens available from cadaver donors due to their unsuitability for transplantation [12, 13, 22, 29, 30], or human fresh stromal lenticules obtained during refractive surgery [5, 10, 21, 27, 46]. The resting ex vivo studies considered the porcine cornea as approximate model of the human one, thanks to the similar anatomy and the wide availability and easiness to obtain fresh animal specimens and several comparative studies between the mechanical behaviour of the two species were performed in literature [12, 13, 29, 30, 51] (Tables 1 and 2). Considering the biomechanical properties of human and porcine corneas, even though the complexity of comparing different studies mentioned in the first paragraphs of Discussion section,
both the species shared similar mechanical features: non-linear stress-strain behaviour with no significant difference in terms of stress–strain patterns [12, 30] and very similar average tensile strength [12] for what concerns uniaxial test. Inflation test revealed that the nonlinear mechanical response of porcine corneas showed a sharper transition from the initial stage of low rigidity to the final stage with greater rigidity [31]. Moreover, porcine corneas recorded lower initial and final stiffness values than all groups of human corneas [13]. Investigating along the corneal depth, in human corneas the anterior region resulted stiffer than the posterior one and also than the anterior porcine region probably due to the human Bowman’s membrane [29]. On the other hand, in stress-relaxation conditions, human corneas resulted significantly stiffer [13] while porcine corneas exhibited more and quicker relaxation with statistically significant differences in relaxation rates [12, 13]. Therefore, based on the experimental data reported in literature, the porcine cornea appears a suitable model of the human cornea when the investigation is related to tensile strength and stress–strain relation, while not perfectly appropriate if the research interest also includes the stress-relaxation behaviour [12, 13].
Regarding the limitations of the methods, uniaxial tensile tests, by considering a strip starting from the corneal curved surface, did not account for the variation in specimen length between the longitudinal centreline and the edges, the flatting of the initial curvature inducing initial stress and the thickness variation between centre and periphery. Although the corneal thickness is minimal in the centre and increases towards the ends, the central value was usually considered to extract the stress-strain behaviour from experimental results. Moreover, the need of rectangular strips implies a cutting procedure which may alter the microstructure of the corneal tissue. All these simplifications were shown in computing of the stress by dividing the measured force for the transversal area, resulting in an overestimation of the corneal stiffness by about 32% compared with the structural inflation test [23]. This difference was reduced to approximately 5% by means of the novel procedure introduced by Elsheikh et al. [23] to remedy the inaccuracy sources in tensile tests on corneal specimens. Despite the tensile limitations in the accuracy of the corneal global properties, this easy, low-cost and practise test remains useful when the focus regards the comparisons of tissue behaviour in different experimental conditions, for example in the case of healthy and treated corneas or different corneal directions. Moreover, among all the other mechanical techniques, tensile testing allows to study the different anatomical orientations and the different layers composing the thickness of the cornea, by stretching strips cut along the SI, NT and diagonal directions and in the different regions along the depth. By comparing the corneal behaviour in different orientations, the SI specimens resulted more rigid than the NT ones [15, 21], expect in [10]. When the mechanical behaviour was studied along the depth, the Young’s Modulus was found to decrease gradually from the anterior to the posterior surface [19, 26, 29] and it resulted equal in SI, NT and diagonal directions for each layer by Du et al. [26] while greater in SI direction for the posterior layer by Nambiar et al. [19].
Regarding the inflation testing, the cutting procedure for the corneal button extraction is less destructive than that for the tensile strip as it regards only the edge region, but the corneal physiological connections to other ocular components are destroyed and simulated by un-optimal support chambers. In this case, a scleral ring is usually used for clamping the cornea and this could influence the corneal stiffness measurement. For this reason, the whole eye globe appears to be more adequate to inflate the cornea because it allows to reproduce more likely in vivo situations. However, the measurement of corneal deformation for the application of the internal pressure requires sophisticated instruments with high accuracy.
While tensile and inflation tests were largely performed to determine the in-plane biomechanical properties, corneal behaviour under other mechanical conditions was rarely investigated. Only a few studies carried out unconfined compression tests [49, 50], although this test does not involve so complex sample preparation as it is performed on corneal buttons but, differently than the inflation test, the tissue is interposed between two surfaces without any clamps for gripping. In addition, it allows to study the corneal mechanical response to an external loading, which is something not too far beyond the reality, as in in vivo conditions cornea may be subjected to compressive deformation due to, for example, eye rubbing or accidental impact on the ocular surface.
Moreover, another important aspect not yet researched in detail regards the local mechanical properties of the cornea, as the tensile studies considered the central cornea and the inflation studies the whole corneal surface. To mechanically characterize the cornea from the centre to the edges, indentation tests can be used over the whole radiation field with an indenter sufficiently adequate to differentiate the different regions. In addition, by keeping constant the indentation load, also the creep properties can be evaluated. The first attempts were done by Nohava et al. [34], which, by indenting the central, paracentral and peripheral regions on corneal slices, showed a significant increase in Young’s Modulus moving to the centre, a stiffening due to CXL treatment in the centre (as obtained in tensile tests by [14, 29, 30] ) and also in the paracentral region, and a creep behaviour inversely proportional to the stiffness. All the ex vivo techniques reported above did not include shear deformation, thus they were unable to investigate the shear properties that are important for more complex material models for predicting the corneal biomechanics. To study them, the shear test can be performed on corneal buttons placed between two parallel surfaces with different types of oscillatory experiments (such as strain or frequency sweep experiments). Differently from the tensile and inflation experiments exhibiting stiffer elasticity for increased deformation, a significant decrease in the stiffness for strains larger than the critical value resulted in shear tests [52].
Therefore, despite all the limitations of performing the experiments outside the living organism, the ex vivo techniques remain essential tools when the in vivo evaluation is not applicable, such as in testing corneal treatments for different doses or exposition times or in applying loading patterns greater than those physiologically allowed to assess the response in extreme damage conditions.
Currently, there is an intensive and continuous interest in the development of techniques that allow the in vivo evaluation of corneal biomechanical properties. However, although important findings have been obtained in recent years, only the ORA and Corvis ST are commercially available and only the dynamic response of the cornea can be assessed by means of these methods. Concerning the quantities measured by ORA, corneal hysteresis and rupture factor, do not provide relationships able to link classic constitutive properties such as elastic modulus, limiting their applicability in computational models, and are unable to resolve spatial differences within the tissue, limiting sensitivity and specificity for detecting early regional property changes in keratoconus. Also, the modulation of the air puff pressure in response to corneal deformation introduces inter-measurement variability, which limits comparison even between measurements of the same eye over time. This aspect was overcome by Corvis ST, but, at the same time, it is affected by the analysis of a single (axial) component of bulk corneal behaviour with no depth-dependent biomechanical resolution.
On the other hand, also the FE models presented several limits, not laying the foundations for a computational tool that can be used as a gold standard in clinical practise because of the partial validations of the models, the absence of a recognized methodology to automatically obtained patient-specific models in terms of geometry and material properties. Furthermore, the derivation of the of material relationships from ex vivo instead of in vivo experimental studies [40], the simplified material formulations [76, 78, 79] that did not account for the hyperelasticity, viscosity [74, 75, 81], anisotropy, simulations of pathologies without tuning the material parameters (healthy material parameters utilized) [77, 81], reduced range of strain rates applicable [40], applanation principle not satisfied at very low and very high IOPs [74], one-patient (single case) study or different pathological stages [75, 81] make FEMs complex to be compared and to be trusty. Moreover, the absence of uniqueness in material formulation, and consequently in material parameters, and, in the case of high-sophisticated formulation, the use of a not open-source material subroutine made the computational results not reliable or not reproducible. Considering the evidence found through ex vivo, in vivo and in silico tests, all the methodologies can describe the hight non-linearity in the mechanical response, the anisotropy, the time-dependent behaviour of the cornea. Ex vivo analysis permit to analyse the mechanical properties in terms of stiffness (Young’s Modulus) and viscous constants, but the conservation and the hydration of the samples, together with the lack of the surrounding biological structures and the active response of the muscular system, can alter the results. In vivo methods overcome these limits, but researchers have to deal with the enrolling of health and pathological subjects, the invasiveness of the measurements (trying to reduce the discomfort of the candidates) and the reproducibility of the test. In silico models have the potentialities to analyse several scenarios, different surgical procedures, acquiring mechanical quantities that in ex vivo and in vivo tests are almost impossible to be measured, as the stress and strain distribution in all the region of the cornea, and in general of the model. However, the reliability of the numerical results is linked to the mechanical characterisation and geometrical morphology acquired experimentally. Hence, the mutual exploitation of the methodologies is the only way to proper quantify the biomechanics of cornea. A potential approach involves conducting an experimental campaign on animal samples (considered more accessible than human samples and surgical waste), following a specific protocol based on the features of interest in the research study (such as anisotropy, viscoelasticity, and hydration). Subsequently, the second step entails computationally modelling the experimental tests to validate the material model through an experimental-computational coupled approach [88, 89]. The model is then adapted to describe human tissues in FE modelling by adjusting sample thickness using human values from histological analysis, and the results are compared with existing literature. In the author’s perspective, future studies should prioritize the development of non-invasive, in vivo machines, equipment, and algorithms to quantify human corneal properties. This data can further validate the FE results. After validating the computational model, various scenarios, including morphological corneal alterations and eye pathology, can be simulated to predict the mechanical behaviour under different conditions. This simulation approach allows for testing the reliability and effectiveness of potential treatments in development.
Conclusion
This review proposed a critical overview of state-of-art of the bioengineering techniques to analyse the corneal biomechanics because of the need to shine the unstudied aspects of ophthalmic field, to improve diagnosis, treatment, and healing process of the corneal tissue. The potentialities of all the methodologies were clearly reported, as well as the requirement to simplify physiological and pathological conditions, proposing in the experimental set-up only a limited number of features governing the eye district. However, discussion about the limits were fully reasoned, not to demean the type of analysis but to give the reader the bases to choose the experimental test typology and numerical approach and the corresponding negative aspects to consider, trying to overcome them. In future, it is desirable to have a non-invasive in vivo procedure able to assess the healthy or the pathological (and in case, identifying the stage of pathology) condition of the cornea, to improve earlier diagnosis, to predict the evolution of eye functionality, to optimize and personalize surgical refractive treatments and to customize new treatments (as CXL).
For the moment, the in vivo methods consisting of air-puff have proposed no physiological mechanical conditions to measure the biomechanical features of the cornea, imposing a reverse curvature. On the other side, in silico models have been proposed exploiting multiple approaches but not posing the fundamentals for the development of a recognized and standardised clinical tool yet.
References
Kelly DJ, Farrell SM (2018) Physiology and role of intraocular pressure in contemporary anesthesia. Anesth Analg 126:1551–1562. https://doi.org/10.1213/ANE.0000000000002544
Dawson DG, Edelhauser HF (2011) Adler’s Physiology of the Eye: Expert Consult, 11th Edition, https://www.researchgate.net/publication/281572472
Bharathi RB, Poojary RG, Prabhu GK, Ve RS (2022) Finite element method for estimation of applanation force and to study the influence of intraocular pressure of eye on tonometry. Int Ophthalmol 42:1997–2005. https://doi.org/10.1007/s10792-021-02157-6
Hon Y, Chen GZ, Lu SH, Lam DCC, Lam AKC (2017) High myopes have lower normalised corneal tangent moduli (less ‘stiff’ corneas) than low myopes. Ophthalmic Physiol Opt 37:42–50. https://doi.org/10.1111/opo.12335
Song Y, Wu D, Shen M, Wang L, Wang C, Cai Y, Xue C, Cheng GPM, Zheng Y, Wang Y (2022) Measuring human corneal stromal biomechanical properties using tensile testing combined with optical coherence tomography. Front Bioeng Biotechnol. https://doi.org/10.3389/fbioe.2022.882392
Zhao Y, Shen Y, Yan Z, Tian M, Zhao J, Zhou X (2019) Relationship among corneal stiffness, thickness, and biomechanical parameters measured by Corvis ST, Pentacam and ORA in Keratoconus. Front Physiol. https://doi.org/10.3389/fphys.2019.00740
Vellara HR, Patel DV (2015) Biomechanical properties of the keratoconic cornea: a review. Clin Exp Optom 98:31–38. https://doi.org/10.1111/cxo.12211
Wu N, Chen Y, Yu X, Li M, Wen W, Sun X (2016) Changes in corneal biomechanical properties after long-term topical Prostaglandin therapy. PLOS ONE. https://doi.org/10.1371/journal.pone.0155527
Satitpitakul V, Taweekitikul P, Puangsricharern V, Kasetsuwan N, Reinprayoon U, Kittipibul T (2021) Alteration of corneal biomechanical properties in patients with dry eye disease. PLOS ONE. https://doi.org/10.1371/journal.pone.0254442
Xiang Y, Shen M, Xue C, Wu D, Wang Y (2018) Tensile biomechanical properties and constitutive parameters of human corneal stroma extracted by SMILE procedure. J Mech Behav Biomed Mater 85:102–108. https://doi.org/10.1016/j.jmbbm.2018.05.042
Elsheikh A, Alhasso D (2009) Mechanical anisotropy of porcine cornea and correlation with stromal microstructure. Exp Eye Res 88:1084–1091. https://doi.org/10.1016/j.exer.2009.01.010
Zeng Y, Yang J, Huang K, Lee Z, Lee X (2001) A comparison of biomechanical properties between human and porcine cornea. J Biomech 34(4):533–537
Elsheikh A, Alhasso D, Rama P (2008) Biomechanical properties of human and porcine corneas. Exp Eye Res 86:783–790. https://doi.org/10.1016/j.exer.2008.02.006
Fontanella CG, Carniel EL, Corain L, Peruffo A, Iacopetti I, Pavan PG, Todros S, Perazzi A (2021) Mechanical behaviour of healthy versus alkali-lesioned corneas by a porcine organ culture model. BMC Vet Res. https://doi.org/10.1186/s12917-021-03050-1
Boschetti F, Triacca V, Spinelli L, Pandolfi A (2012) Mechanical characterization of porcine corneas. J Biomech Eng. https://doi.org/10.1115/1.4006089
Su P, Yang Y, Xiao J, Song Y (2015) Corneal hyper-viscoelastic model: derivations, experiments, and simulations. Acta Bioeng Biomech 17:73–84. https://doi.org/10.5277/ABB-00142-2014-03
Tonsomboon K, Koh CT, Oyen ML (2014) Time-dependent fracture toughness of cornea. J Mech Behav Biomed Mater 34:116–123. https://doi.org/10.1016/j.jmbbm.2014.01.015
Toniolo I, Mascolini MV, Neri S, Perazzi A, Fontanella CG (2023) Experimental analysis of the biomechanics of healthy porcine corneas. In: Patron Editore S.r.l., 2023. Convegno Nazionale di Bioingegneria2023 8th National Congress of Bioengineering, GNB 2023 Padova 21 June 2023 through 23 June 2023, Code 193282. scopus link: https://www.scopus.com/record/display.uri?eid=2-s2.0-85175876905&origin=resultslist
Nambiar MH, Liechti L, Müller F, Bernau W, Studer H, Roy AS, Seiler TG, Büchler P (2022) Orientation and depth dependent mechanical properties of the porcine cornea: Experiments and parameter identification. Exp Eye Res. https://doi.org/10.1016/j.exer.2022.109266
Elsheikh A, Kassem W, Jones SW, Jones S (2011) Strain-rate sensitivity of porcine and ovine corneas. https://www.researchgate.net/publication/51495138
Xue C, Xiang Y, Shen M, Wu D, Wang Y (2018) Preliminary investigation of the mechanical anisotropy of the normal human corneal stroma. J Ophthalmol. https://doi.org/10.1155/2018/5392041
Mahdian M, Seifzadeh A, Mokhtarian A, Doroodgar F (2021) Characterization of the transient mechanical properties of human cornea tissue using the tensile test simulation. Mater Today Commun. https://doi.org/10.1016/j.mtcomm.2021.102122
Elsheikh A, Anderson K (2005) Comparative study of corneal strip extensometry and inflation tests. J R Soc Interface 2:177–185. https://doi.org/10.1098/rsif.2005.0034
Ashofteh Yazdi A, Melchor J, Torres J, Faris I, Callejas A, Gonzalez-Andrades M, Rus G (2020) Characterization of non-linear mechanical behavior of the cornea. Sci Rep. https://doi.org/10.1038/s41598-020-68391-7
Arsalan Khan M, Elsheikh A, Ahmad Khan I (2018) Biomechanical behaviour - anisotropy of eye cornea through experimental strip tests. IOP Conf Ser Mater Sci Eng Inst Phys Publishing. https://doi.org/10.1088/1757-899X/310/1/012075
Du R, Tian H, Xu X, Shao Y, Song F (2017) Depth-dependent mechanical characteristics of porcine cornea. Soft Mater 15:27–33. https://doi.org/10.1080/1539445X.2016.1242497
Lombardo G, Serrao S, Rosati M, Lombardo M (2014) Analysis of the viscoelastic properties of the human cornea using scheimpflug imaging in inflation experiment of eye globes. PLOS ONE. https://doi.org/10.1371/journal.pone.0112169
Kling S, Marcos S (2013) Effect of hydration state and storage media on corneal biomechanical response from in vitro inflation tests. J Refract Surg 29:490–497. https://doi.org/10.3928/1081597X-20130617-08
Kohlhaas M, Spoerl E, Schilde T, Unger G, Wittig C, Pillunat LE (2006) Biomechanical evidence of the distribution of cross-links in corneastreated with riboflavin and ultraviolet a light. J Cataract Refract Surg 32:279–283. https://doi.org/10.1016/j.jcrs.2005.12.092
Wollensak G, Spoerl E, Seiler T (2003) Stress-strain measurements of human and porcine corneas after riboflavin-ultraviolet-A-induced cross-linking. J Cataract Refract Surg 29:1780–1785. https://doi.org/10.1016/S0886-3350(03)00407-3
Matteoli S, Virga A, Paladini I, Mencucci R, Corvi A (2016) Investigation into the elastic properties of ex vivo porcine corneas subjected to inflation test after cross-linking treatment. J Appl Biomater Funct Mater 14:e163–e170. https://doi.org/10.5301/jabfm.5000262
Bao F, Jiang L, Wang X, Zhang D, Wang Q, Zeng Y (2012) Assessment of the ex vivo biomechanical properties of porcine cornea with inflation test for corneal xenotransplantation. J Med Eng Technol 36:17–21. https://doi.org/10.3109/03091902.2011.629276
Kling S, Marcos S (2013) Contributing factors to corneal deformation in air puff measurements. Invest Ophthalmol Vis Sci 54:5078–5085. https://doi.org/10.1167/iovs.13-12509
Nohava J, Swain M, Lang SJ, Maier P, Heinzelmann S, Reinhard T, Eberwein P (2018) Instrumented indentation for determination of mechanical properties of human cornea after ultraviolet-A crosslinking. J Biomed Mater Res A 106:1413–1420. https://doi.org/10.1002/jbm.a.36337
Mascolini MV, Fontanella CG, Berardo A, Carniel EL (2023) Influence of transurethral catheters on urine pressure-flow relationships in males: a computational fluid-dynamics study. Comput Methods Programs Biomed. https://doi.org/10.1016/j.cmpb.2023.107594
Caragiuli M, Mandolini M, Landi D, Bruno G, De Stefani A, Gracco A, Toniolo I (2021) A finite element analysis for evaluating mandibular advancement devices. J Biomech. https://doi.org/10.1016/j.jbiomech.2021.110298
Toniolo I, Berardo A, Foletto M, Fiorillo C, Quero G, Perretta S, Carniel EL (2022) Patient-specific stomach biomechanics before and after laparoscopic sleeve gastrectomy. Surg Endosc 36:7998–8011. https://doi.org/10.1007/s00464-022-09233-7
Chen J, Xu Y, Li C, Zhang L, Yi F, Lu Y (2021) Displacement and stress distribution of the craniomaxillofacial complex under different surgical conditions: a three-dimensional finite element analysis of fracture mechanics. BMC Oral Health. https://doi.org/10.1186/s12903-021-01941-1
Eltes PE, Bartos M, Hajnal B, Pokorni AJ, Kiss L, Lacroix D, Varga PP, Lazary A (2021) Development of a computer-aided design and finite element analysis combined method for affordable spine surgical navigation with 3D-printed customized template. Front Surg. https://doi.org/10.3389/fsurg.2020.583386
Whitford C, Movchan NV, Studer H, Elsheikh A (2018) A viscoelastic anisotropic hyperelastic constitutive model of the human cornea. Biomech Model Mechanobiol 17:19–29. https://doi.org/10.1007/s10237-017-0942-2
de Oteyza GG, de Toledo JÁ, Barraquer RI, Kling S (2021) Refractive changes of a new asymmetric intracorneal ring segment with variable thickness and base width: a 2D finite-element model. PLOS ONE. https://doi.org/10.1371/journal.pone.0257222
Carniel EL, Toniolo I, Fontanella CG (2020) Computational biomechanics: In-silico tools for the investigation of surgical procedures and devices. Bioengineering 7:1–12. https://doi.org/10.3390/bioengineering7020048
Zhang D, Qin X, Zhang H, Li L (2021) Time-varying regularity of changes in biomechanical properties of the corneas after removal of anterior corneal tissue. Biomed Eng Online. https://doi.org/10.1186/s12938-021-00948-7
Zhang H, Zhang D, Qin X, Wang H, Li L (2018) Study of the transversal deformation of corneal strip under uniaxial loading. J Mech Med Biol. https://doi.org/10.1142/S0219519418400183
Wang X, Li X, Chen W, He R, Gao Z, Feng P (2017) Effects of ablation depth and repair time on the corneal elastic modulus after laser in situ keratomileusis. Biomed Eng Online. https://doi.org/10.1186/s12938-017-0311-5
Zheng Y, Xue C, Wang J, Chen X, Wang X, Wang Y (2023) Analysis of the correlation between biomechanical properties and corneal densitometry in myopic eyes. Front Bioeng Biotechnol. https://doi.org/10.3389/fbioe.2023.1182372
Ko MWL, Leung LKK, Lam DCC, Leung CKS (2013) Characterization of corneal tangent modulus in vivo. Acta Ophthalmol. https://doi.org/10.1111/aos.12066
Dorronsoro C, Pascual D, Pérez-Merino P, Kling S, Marcos S (1980) Optical coherence tomography; (170.3880) Medical and biological imaging. www.vision.csic.es
Hatami-Marbini H, Etebu E (2013) An experimental and theoretical analysis of unconfined compression of corneal stroma. J Biomech 46:1752–1758. https://doi.org/10.1016/j.jbiomech.2013.03.013
Hatami-Marbini H, Etebu E (2013) Rate dependent biomechanical properties of corneal stroma in unconfined compression. Biorheology 50:133–147. https://doi.org/10.3233/BIR-130634
Whitford C, Joda A, Jones S, Bao F, Rama P, Elsheikh A (2016) Ex vivo testing of intact eye globes under inflation conditions to determine regional variation of mechanical stiffness. Eye Vis. https://doi.org/10.1186/s40662-016-0052-8
Hatami-Marbini H (2014) Viscoelastic shear properties of the corneal stroma. J Biomech 47:723–728. https://doi.org/10.1016/j.jbiomech.2013.11.019
Kling S, Hafezi F (2017) Corneal biomechanics – a review. Ophthalmic Physiol Opt 37:240–252. https://doi.org/10.1111/opo.12345
Wang JJ, Liu XY, Bao FJ, Lopes BT, Wang LZ, Eliasy A, Abass A, Elsheikh A (2021) Review of ex-vivo characterisation of corneal biomechanics. Med Nov Technol Devices. https://doi.org/10.1016/j.medntd.2021.100074
Wang L, Tian L, Huang Y, Huang Y, Zheng Y (2018) Assessment of corneal Biomechanical properties with inflation test using Optical Coherence Tomography. Ann Biomed Eng 46:247–256. https://doi.org/10.1007/s10439-017-1973-7
Anderson K, El-Sheikh A, Newson T (2004) Application of structural analysis to the mechanical behaviour of the cornea. J R Soc Interface 1:3–15. https://doi.org/10.1098/rsif.2004.0002
Chong J, Dupps WJ (2021) Corneal biomechanics: measurement and structural correlations. Exp Eye Res. https://doi.org/10.1016/j.exer.2021.108508
Ambrósio R, Ramos I, Luz A, Faria FC, Steinmueller A, Krug M, Belin MW, Roberts CJ (2013) Dynamic ultra high speed Scheimpflug imaging for assessing corneal biomechanical properties. Revista Brasileira de Oftalmologia 72:99–102
Luce DA (2005) Determining in vivo biomechanical properties of the cornea with an ocular response analyzer. J Cataract Refract Surg 31:156–162. https://doi.org/10.1016/j.jcrs.2004.10.044
Qin X, Tian L, Zhang H, Chen X, Li L (2019) Evaluation of corneal elastic modulus based on corneal visualization scheimpflug technology. Biomed Eng Online. https://doi.org/10.1186/s12938-019-0662-1
Zhang D, Zhang H, Tian L, Zheng Y, Fu C, Zhai C, Li L (2021) Exploring the biomechanical properties of the human cornea in vivo based on corvis ST. Front Bioeng Biotechnol. https://doi.org/10.3389/fbioe.2021.771763
Koprowski R (2019) Air Puff Tonometers: Challenges and insights, 2019, Patron. Iop Publishing Ltd
Wang B, Yang L, Cheng J, Wang J, Mei Y (2023) In-vivo high-speed biomechanical imaging of the cornea using corvis ST and digital image correlation. Comput Biol Med. https://doi.org/10.1016/j.compbiomed.2023.106540
Eliasy A, Chen K-J, Vinciguerra R, Lopes BT, Abass A, Vinciguerra P, Ambrósio R Jr., Roberts CJ, Elsheikh A (2019) Determination of corneal biomechanical behavior in-vivo for healthy eyes using corvis ST tonometry: stress-strain index. Front Bioeng Biotechnol. https://doi.org/10.3389/fbioe.2019.00105
Padmanabhan P, Lopes BT, Eliasy A, Abass A, Elsheikh A (2022) Vivo Biomechanical Changes Associated with Keratoconus Progression. Curr Eye Res 47:982–986. https://doi.org/10.1080/02713683.2022.2058020
Yun SH, Chernyak D (2018) Brillouin microscopy: assessing ocular tissue biomechanics. Curr Opin Ophthalmol 29:299–305. https://doi.org/10.1097/ICU.0000000000000489
Scarcelli G, Yun SH (2012) In vivo Brillouin optical microscopy of the human eye. Opt Express 20(8):9197–202
Lam AKC, Hon Y, Leung LKK, Lam DCC (2015) Repeatability of a novel corneal indentation device for corneal biomechanical measurement. Ophthalmic Physiol Opt 35:455–461. https://doi.org/10.1111/opo.12219
Shih PJ, Cao HJ, Huang CJ, Wang IJ, Shih WP, Yen JY (2015) A corneal elastic dynamic model derived from Scheimpflug imaging technology. Ophthalmic Physiol Opt 35:663–672. https://doi.org/10.1111/opo.12240
Sit AJ, Lin SC, Kazemi A, McLaren JW, Pruet CM, Zhang X (2017) In vivo noninvasive measurement of young’s modulus of elasticity in human eyes: a feasibility study. J Glaucoma 26:967–973. https://doi.org/10.1097/IJG.0000000000000774
Ramier A, Eltony AM, Chen YT, Clouser F, Birkenfeld JS, Watts A, Yun SH (2020) In vivo measurement of shear modulus of the human cornea using optical coherence elastography. Sci Rep. https://doi.org/10.1038/s41598-020-74383-4
Esporcatte LPG, Salomão MQ, Lopes BT, Vinciguerra P, Vinciguerra R, Roberts C, Elsheikh A, Dawson DG, Ambrósio R (2020) Biomechanical diagnostics of the cornea. Eye Vis. https://doi.org/10.1186/s40662-020-0174-x
De Stefano VS, Dupps WJ (2017) Biomechanical Diagnostics of the Cornea. http://journals.lww.com/internat-ophthalmology
Shih PJ, Wang IJ, Cai WF, Yen JY (2017) Biomechanical simulation of stress concentration and intraocular pressure in corneas subjected to myopic refractive surgical procedures. Sci Rep. https://doi.org/10.1038/s41598-017-14293-0
Ariza-Gracia M, Zurita JF, Piñero DP, Rodriguez-Matas JF, Calvo B (2015) Coupled biomechanical response of the cornea assessed by non-contact tonometry. A simulation study. PLOS ONE. https://doi.org/10.1371/journal.pone.0121486
Baek JW, Park SJ (2019) Finite element analysis of cornea deformation and curvature change during the keratoplasty suturing process. Biomed Eng Lett 9:203–209. https://doi.org/10.1007/s13534-019-00100-4
Karimi A, Meimani N, Razaghi R, Rahmati SM, Jadidi K, Rostami M (2019) Biomechanics of the healthy and Keratoconic Corneas: a combination of the Clinical Data, Finite element analysis, and Artificial neural network. Curr Pharm Des 24:4474–4483. https://doi.org/10.2174/1381612825666181224123939
Zhou B, Sit AJ, Zhang X (2017) Noninvasive measurement of wave speed of porcine cornea in ex vivo porcine eyes for various intraocular pressures. Ultrasonics 81:86–92. https://doi.org/10.1016/j.ultras.2017.06.008
Kobayashi A, Izaki R, Fujita H, Harada K, Ozaki H, Kadonosono K, Uchio E (2023) Finite element analysis of changes in tensile strain and deformation by airbag impact in eyes of various axial lengths. Int Ophthalmol 43:2143–2151. https://doi.org/10.1007/s10792-022-02609-7
Fang L, Wang Y, Yang R, Deng S, Deng J, Wan L (2020) Effects of the LASIK flap thickness on corneal biomechanical behavior: a finite element analysis. BMC Ophthalmol. https://doi.org/10.1186/s12886-020-01338-8
Bagheri NM, Kadkhodaei M, Pirhadi S, Mosaddegh P (2021) Effects of intracorneal ring segments implementation technique and design on corneal biomechanics and keratometry in a personalized computational analysis. Sci Rep. https://doi.org/10.1038/s41598-021-93821-5
Wang S, Chester SA (2021) Multi-physics modeling and finite element formulation of corneal UV cross-linking. Biomech Model Mechanobiol 20:1561–1578. https://doi.org/10.1007/s10237-021-01463-3
Asejczyk-Widlicka M, Srodka W (2020) Finite element simulation of Goldmann tonometry after refractive surgery. Clin Biomech Elsevier Ltd 71:24–28. https://doi.org/10.1016/j.clinbiomech.2019.09.007
Lago MA, Rupérez MJ, Martínez-Martínez F, Monserrat C, Larra E, Güell JL, Peris-Martínez C (2015) A new methodology for the in vivo estimation of the elastic constants that characterize the patient-specific biomechanical behavior of the human cornea. J Biomech 48:38–43. https://doi.org/10.1016/j.jbiomech.2014.11.009
Sinha Roy A, Kurian M, Matalia H, Shetty R (2015) Air-puff associated quantification of non-linear biomechanical properties of the human cornea in vivo. J Mech Behav Biomed Mater 48:173–182. https://doi.org/10.1016/j.jmbbm.2015.04.010
Qin X, Tian L, Zhang H, Zhang D, Jie Y, Zhang HX, Li L (2022) Determine corneal biomechanical parameters by finite element simulation and parametric analysis based on ORA measurements. Front Bioeng Biotechnol. https://doi.org/10.3389/fbioe.2022.862947
Shih PJ, Huang CJ, Huang TH, Lin HC, Yen JY, Wang IJ, Cao HJ, Shih WP, Dai CA (2017) Estimation of the corneal young’s modulus in vivo based on a fluid-filled spherical-shell model with scheimpflug imaging. J Ophthalmol. https://doi.org/10.1155/2017/5410143
Salmaso C, Toniolo I, Fontanella CG, Da Roit P, Albanese A, Polese L, Stefanini C, Foletto M, Carniel EL (2020) Computational tools for the Reliability Assessment and the Engineering Design of procedures and devices in bariatric surgery. Ann Biomed Eng 48:2466–2483. https://doi.org/10.1007/s10439-020-02542-9
Toniolo I, Fontanella CG, Foletto M, Carniel EL (2022) Coupled experimental and computational approach to stomach biomechanics: Towards a validated characterization of gastric tissues mechanical properties. J Mech Behav Biomed Mater. https://doi.org/10.1016/j.jmbbm.2021.104914
Funding
Open access funding provided by Università degli Studi di Padova within the CRUI-CARE Agreement. This work was supported by MIUR, FISR 2019, Project n FISR2019_03221, titled CECOMES: CEntro di studi sperimentali e COmputazionali per la ModElliStica applicata alla chirurgia.
Author information
Authors and Affiliations
Contributions
Idealization and conceptualization: I.T. and M.V.M.; Literature review: I.T. and M.V.M.; Writing: I.T. and M.V.M.; Editing and Review: E.L.C. and C.G.F.; Funding: E.L.C. and C.G.F.
Corresponding author
Ethics declarations
Competing interests
All authors have given approval to the final version of the manuscript. The authors Ilaria Toniolo, Maria Vittoria Mascolini, Emanuele Luigi Carniel and Chiara Giulia Fontanella have no conflicts of interest or financial ties to disclose.
Ethical approval
No need.
Consent to participate
No need.
Consent for publication
No need.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mascolini, M.V., Toniolo, I., Carniel, E.L. et al. Ex vivo, in vivo and in silico studies of corneal biomechanics: a systematic review. Phys Eng Sci Med 47, 403–441 (2024). https://doi.org/10.1007/s13246-024-01403-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13246-024-01403-2