Abstract
Purpose
Coronary flow is affected by evolving events such as atherosclerotic plaque formation, rupture, and thrombosis, resulting in myocardial ischemia and infarction. Highly resolved 3D hemodynamic data at the stenosis is essential to model shear-sensitive thrombotic events in coronary artery disease.
Methods
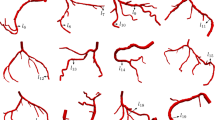
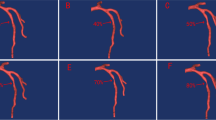
We developed a hybrid 1D–3D simulation framework to compute patient-specific coronary hemodynamics efficiently. A 1D model of the coronary flow is coupled to an image-based 3D model of the region of interest. This framework affords the advantages of reduced-order modeling, decreasing the global computational cost, without sacrificing the accuracy of the quantities of interest.
Results
We validated our 1D–3D model against full 3D coronary simulations in healthy and diseased conditions. Our results showed good agreement between the 3D and the 1D–3D models while reducing the computational cost by 40-fold compared to the 3D simulation. The 1D–3D model predicted left/right coronary flow distribution within 3% and provided an accurate estimation of fractional flow reserve and wall shear stress distribution at the stenosis comparable to the 3D simulation.
Conclusion
Savings in computational cost may be significant in situations with changing geometry, such as growing thrombosis. Also, this approach would allow quantifying the time-dependent effect of thrombotic growth and occlusion on the global coronary circulation.







Similar content being viewed by others
References
Blanco, P. J., C. A. Bulant, L. O. Müller, G. D. M. Talou, C. G. Bezerra, P. A. Lemos, and R. A. Feijóo. Comparison of 1D and 3D models for the estimation of fractional flow reserve. Sci. Rep. 8:1–12, 2018.
Blanco, P. J., and R. A. Feijóo. A dimensionally-heterogeneous closed-loop model for the cardiovascular system and its applications. Med. Eng. Phys. 35:652–667, 2013.
Blanco, P. J., M. R. Pivello, S. A. Urquiza, and R. A. Feijóo. On the potentialities of 3D–1D coupled models in hemodynamics simulations. J. Biomech. 42:919–930, 2009.
Blanco, P. J., S. A. Urquiza, and R. A. Feijóo. Assessing the influence of heart rate in local hemodynamics through coupled 3D–1D–0D models. Int. J. Numer. Method. Biomed. Eng. 26:890–903, 2010.
Bluestein, D., L. Niu, R. T. Schoephoerster, and M. K. Dewanjee. Fluid mechanics of arterial stenosis: relationship to the development of mural thrombus. Ann. Biomed. Eng. 25:344–356, 1997.
Boileau, E., P. Nithiarasu, P. J. Blanco, L. O. Müller, F. E. Fossan, L. R. Hellevik, W. P. Donders, W. Huberts, M. Willemet, and J. Alastruey. A benchmark study of numerical schemes for one-dimensional arterial blood flow modelling. Int. J. Numer. Method Biomed. Eng. 31:1–33, 2015.
Boileau, E., S. Pant, C. Roobottom, I. Sazonov, J. Deng, X. Xie, and P. Nithiarasu. Estimating the accuracy of a reduced-order model for the calculation of fractional flow reserve (FFR). Int. J. Numer. Method Biomed. Eng. 2018. https://doi.org/10.1002/cnm.2908.
Esmaily Moghadam, M., I. E. Vignon-Clementel, R. Figliola, and A. L. Marsden. A modular numerical method for implicit 0D/3D coupling in cardiovascular finite element simulations. J. Comput. Phys. 244:63–79, 2013.
Flamm, M. H., and S. L. Diamond. Multiscale systems biology and physics of thrombosis under flow. Ann. Biomed. Eng. 40:2355–2364, 2012.
Fleeter, C. M., G. Geraci, D. E. Schiavazzi, A. M. Kahn, and A. L. Marsden. Multilevel and multifidelity uncertainty quantification for cardiovascular hemodynamics. Comput. Methods Appl. Mech. Eng. 2020. https://doi.org/10.1016/j.cma.2020.113030.
Fogelson, A. L., and K. B. Neeves. Fluid mechanics of blood clot formation. Annu. Rev. Fluid. Mech. 47:377–403, 2015.
Formaggia, L., J.-F. Gerbeau, F. Nobile, and A. Quarteroni. On the coupling of 3D and 1D Navier-Stokes equations for flow problems in compliant vessels. Comput. Methods Appl. Mech. Eng. 191:561–582, 2001.
Formaggia, L., D. Lamponi, and A. Quarteroni. One-dimensional models for blood flow in arteries. J. Eng. Math. 47:251–276, 2003.
Fossan, F. E., J. Sturdy, L. O. Müller, A. Strand, A. T. Bråten, A. Jørgensen, R. Wiseth, and L. R. Hellevik. Uncertainty quantification and sensitivity analysis for computational FFR estimation in stable coronary artery disease. Cardiovasc. Eng. Technol. 9:597–622, 2018.
Hughes, T. J. R., and J. Lubliner. On the one-dimensional theory of blood flow in the larger vessels. Math. Biosci. 18:161–170, 1973.
Kim, H. J., I. E. Vignon-Clementel, J. S. Coogan, C. A. Figueroa, K. E. Jansen, and C. A. Taylor. Patient-specific modeling of blood flow and pressure in human coronary arteries. Ann. Biomed. Eng. 38:3195–3209, 2010.
Krams, R., J. J. Wentzel, J. A. F. Oomen, R. Vinke, J. C. H. Schuurbiers, P. J. de Feyter, P. W. Serruys, and C. J. Slager. Evaluation of endothelial shear stress and 3d geometry as factors determining the development of atherosclerosis and remodeling in human coronary arteries in vivo. Arterioscler. Thromb. Vasc. Biol. 17:2061–2065, 1997.
Leiderman, K., and A. L. Fogelson. Grow with the flow: a spatial-temporal model of platelet deposition and blood coagulation under flow. Math. Med. Biol. 28:47–84, 2011.
Lu, Y., M. Y. Lee, S. Zhu, T. Sinno, and S. L. Diamond. Multiscale simulation of thrombus growth and vessel occlusion triggered by collagen/tissue factor using a data-driven model of combinatorial platelet signalling. Math. Med. Biol. 34:523–546, 2017.
Mahmoudi, M., A. Farghadan, D. R. McConnell, A. J. Barker, J. J. Wentzel, M. J. Budoff, and A. Arzani. The story of wall shear stress in coronary artery atherosclerosis: biochemical transport and mechanotransduction. J. Biomech. Eng. 2021. https://doi.org/10.1115/1.4049026.
Mirramezani, M., S. Diamond, H. Litt, and S. C. Shadden. Reduced order models for transstenotic pressure drop in the coronary arteries. J Biomech Eng. 2018. https://doi.org/10.1115/1.4042184.
Moake, J. L., N. A. Turner, N. A. Stathopoulos, L. H. Nolasco, and J. D. Hellums. Involvement of large plasma von Willebrand factor (vWF) multimers and unusually large vWF forms derived from endothelial cells in shear stress-induced platelet aggregation. J. Clin. Invest. 78:1456–1461, 1986.
Nesbitt, W. S., E. Westein, F. J. Tovar-Lopez, E. Tolouei, A. Mitchell, J. Fu, J. Carberry, A. Fouras, and S. P. Jackson. A shear gradient-dependent platelet aggregation mechanism drives thrombus formation. Nat. Med. 15:665–673, 2009.
Nobile, F. Coupling strategies for the numerical simulation of blood flow in deformable arteries by 3D and 1D models. Math. Comput. Model. 49:2152–2160, 2009.
Nobili, M., J. Sheriff, U. Morbiducci, A. Redaelli, and D. Bluestein. Platelet activation due to hemodynamic shear stresses: damage accumulation model and comparison to in vitro measurements. ASAIO J. 54:64–72, 2008.
Seeley, B. D., and D. F. Young. Effect of geometry on pressure losses across models of arterial stenoses. J. Biomech. 9:439–448, 1976.
Seo, J., D. E. Schiavazzi, A. M. Kahn, and A. L. Marsden. The effects of clinically-derived parametric data uncertainty in patient-specific coronary simulations with deformable walls. Int. J. Numer. Method. Biomed. Eng. 2020. https://doi.org/10.1002/cnm.3351.
Sheriff, J., D. Bluestein, G. Girdhar, and J. Jesty. High-shear stress sensitizes platelets to subsequent low-shear conditions. Ann. Biomed. Eng. 38:1442–1450, 2010.
Sheriff, J., J. S. Soares, M. Xenos, J. Jesty, M. J. Slepian, and D. Bluestein. Evaluation of shear-induced platelet activation models under constant and dynamic shear stress loading conditions relevant to devices. Ann. Biomed. Eng. 41:1279–1296, 2013.
Sherwin, S. J., V. Franke, J. Peiró, and K. Parker. One-dimensional modelling of a vascular network in space-time variables. J. Eng. Math. 47:217–250, 2003.
Si, H. TetGen, a Delaunay-based quality tetrahedral mesh generator. ACM Trans. Math. Softw. 41:11, 2015.
Team, T. T. P. The Trilinos Project Website, 2020. At https://trilinos.github.io.
Tonino, P. A. L., B. De Bruyne, N. H. J. Pijls, U. Siebert, F. Ikeno, M. vant Veer, V. Klauss, G. Manoharan, T. Engstrøm, and K. G. Oldroyd. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N. Engl. J. Med. 360:213–224, 2009.
Updegrove, A., N. M. Wilson, J. Merkow, H. Lan, A. L. Marsden, and S. C. Shadden. SimVascular: an open source pipeline for cardiovascular simulation. Ann. Biomed. Eng. 45:525–541, 2017.
Urquiza, S. A., P. J. Blanco, M. J. Vénere, and R. A. Feijóo. Multidimensional modelling for the carotid artery blood flow. Comput. Methods Appl. Mech. Eng. 195:4002–4017, 2006.
Wan, J., B. Steele, S. A. Spicer, S. Strohband, G. R. Feijóo, T. J. Hughes, and C. A. Taylor. A one-dimensional finite element method for simulation-based medical planning for cardiovascular disease. Comput. Methods Biomech. Biomed. Eng. 5:195–206, 2002.
Watanabe, I., T. A. Johnson, J. Buchanan, C. L. Engle, and L. S. Gettes. Effect of graded coronary flow reduction on ionic, electrical, and mechanical indexes of ischemia in the pig. Circulation. 76:1127–1134, 1987.
Wilson, R. F., K. Wyche, B. V. Christensen, S. Zimmer, and D. D. Laxson. Effects of adenosine on human coronary arterial circulation. Circulation. 82:1595–1606, 1990.
Xiao, N., J. Alastruey, and C. Alberto Figueroa. A systematic comparison between 1-D and 3-D hemodynamics in compliant arterial models. Int. J. Numer. Method. Biomed. Eng. 30:204–231, 2014.
Xu, Z., N. Chen, M. M. Kamocka, E. D. Rosen, and M. Alber. A multiscale model of thrombus development. J. R. Soc. Interface. 5:705–722, 2008.
Xu, Z., N. Chen, S. C. Shadden, J. E. Marsden, M. M. Kamocka, E. D. Rosen, and M. Alber. Study of blood flow impact on growth of thrombi using a multiscale model. Soft Matter. 5:769–779, 2009.
Yazdani, A., H. Li, J. D. Humphrey, and G. E. Karniadakis. A general shear-dependent model for thrombus formation. PLoS Comput. Biol. 2017. https://doi.org/10.1371/journal.pcbi.1005291.
Yin, M., A. Yazdani, and G. E. Karniadakis. One-dimensional modeling of fractional flow reserve in coronary artery disease: uncertainty quantification and Bayesian optimization. Comput. Methods Appl. Mech. Eng. 353:66–85, 2019.
Young, D. F. Fluid mechanics of arterial stenoses. J. Biomech. Eng. 101:157–175, 1979.
Zheng, X., A. Yazdani, H. Li, J. D. Humphrey, and G. E. Karniadakis. A three-dimensional phase-field model for multiscale modeling of thrombus biomechanics in blood vessels. PLoS Comput. Biol. 2020. https://doi.org/10.1371/journal.pcbi.1007709.
Funding
This work was supported by R01-HL-103419 (N.G.G and S.L.D).
Data Availability
Not applicable.
Code Availability
Code developed for this study will be available via online code repository.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Igor Efimov oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file 2 (MP4 6598 kb)
Rights and permissions
About this article
Cite this article
Grande Gutiérrez, N., Sinno, T. & Diamond, S.L. A 1D–3D Hybrid Model of Patient-Specific Coronary Hemodynamics. Cardiovasc Eng Tech 13, 331–342 (2022). https://doi.org/10.1007/s13239-021-00580-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-021-00580-5