Abstract
This study used both in vitro and in vivo models to evaluate the efficacy of atractylodin as an anticancer treatment for colorectal cancer. The cytotoxicity of atractylodin on colon cancer cells was assessed using the MTT assay, and atractylodin-induced apoptosis was determined using flow cytometry. The expression of cleaved caspase 3 and other apoptotic proteins was examined using Western blotting to determine the mechanism underlying atractylodin's anticancer activity. In addition, the role of PI3K/Akt/mTOR/p70S6K signalling in atractylodin-induced apoptosis in colon cancer cells was analyzed. The study found that atractylodin caused dose-dependent ROS-mediated apoptosis and DNA damage in colon cancer cells and activated caspase 3. Furthermore, atractylodin inhibited the PI3K/Akt/mTOR/p70S6K signalling pathway by targeting PI3Kγ in colon cancer cells. Molecular docking analysis indicated that atractylodin binds to the Akt binding pocket of PI3Kγ. The study also evaluated the antitumour effects of atractylodin on a colon cancer tumour xenograft model and found that it significantly reduced tumour growth and volume by inducing apoptosis. These results suggest that atractylodin has potential as a candidate for the treatment of colorectal cancer, although further research is necessary.
Graphical abstract
Atractylodin induces apoptosis in colon cancer cells.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
After cardiovascular disease, colon carcinogenesis ranks as the second most common cause of cancer death globally. According to reports, there were 1.85 million new cases of colorectal cancer diagnosed in 2018 and there were 880,792 deaths from the disease worldwide (484,224 men and 396,568 women) (1.03 million males; 823,303 females) [1]. Colon cancer is divided into three stages, similar to different oncogeneses, such as initiation, promotion, and progression. The colon epithelium undergoes a pathological transformation, progressing from a hyperproliferative state to invasive and metastatic carcinogenic changes [2]. Surgery and chemotherapy are currently the two major methods for controlling colon cancer, and the reduction in chances is reliant on the size, location, and stage of cancer [3]. Chemotherapy treatment can be initiated at any phase and is usually followed by surgery. On the other hand, surgical treatment begins earlier to identify the tumour and reduce its size [4]. Some studies show that the number of colorectal cancer survivors’ rate has elevated in recent days due to changes in chemotherapy treatments and medical procedures [5]. Unwanted toxicity is observed in approximately 20% of patients, while 1% of patients experience fatal toxicity [6]. Thus, there is a crucial necessity to develop new herbal remedies with zero or fewer side effects.
Cancer cells differ from normal cells in several ways that contribute to their uncontrolled proliferation, resistance to cell death, ability to form new blood vessels, and potential to spread to other parts of the body. These characteristics are known as malignant transformation [7]. Recent research has shown that inflammation, which is both a result of and a cause of malignant transformation, is a good, probable sign of cancer progression [8]. Genetic actions resulting from cancer transformation also initiate inflammatory reactions that lead to tumour growth in the inflammatory cytokines-activated condition [9]. The PI3K/Akt/mTOR/p70S6K signalling pathway controls a number of cellular functions, including metabolism, cytoskeletal remodelling, cell proliferation, and differentiation. Dysregulation of this pathway can contribute to apoptosis and cancer cell survival [10]. Molecular abnormalities can activate the PI3K/Akt/mTOR/p70S6K pathway, resulted in increased tumour growth and resistance to chemotherapy [11]. This pathway is frequently disrupted in various types of cancer, and it has been shown to induces apoptotic cell death and impair the abilities of cancer cells [12,13,14].
New cancer treatments that target specific cell receptors and immune responses have been successful in reducing the morbidity and mortality of cancer [15]. Atractylodes lancea, a plant commonly used in traditional Chinese, Thai, and Japanese medicine, contains the chemical atractylodin, which has been shown to have cytotoxic, proapoptotic, and cell cycle arrest effects on various cancer cells [16,17,18]. Atractylodin also inhibits the phosphorylation of STAT1/3 signalling and the production of heme oxygenase-1 in cholangiocarcinoma cells and persuade apoptosis and autophagy by modulating the PI3K/Akt/mTOR and p38MAPK pathways [19]. However, atractylodin has no significant toxicity on normal cells up to 50 µM concentration, whereas it induced significant cytotoxicity in human mreasr cancer MCF-7 cells [20]. The novelty of this study is to find out whether Atractylodin inhibits the PI3K/Akt/mTOR/p70S6K by targeting the PI3K’s heterodimers catalytic subunits in colon cancer cells. It is well known that inhibiting the PI3K/Akt/mTOR/p70S6K signalling pathway induces apoptosis in cancer cells. However, the mechanism of PI3K/Akt/mTOR/p70S6K signalling inhibition by therapeutic compounds are poorly studied. In this study, we examined the ability of atractylodin to induce apoptosis in colon cancer cells and the underlying molecular mechanism in PI3K/Akt/mTOR/p70S6K signalling inhibition.
2 Materials and methods
2.1 Chemicals
Atractylodin (cat no. TA9947273100, purity 99.82%) (Fig. 1A), 5-diphenyl-tetrazolium bromide, DCFH-DA, EtBr, trypsin–ethylenediaminetetraacetic acid (EDTA), and DMSO were all purchased from Sigma-Aldrich, China. All other analytical chemicals, Dulbecco's modified eagle's medium (DMEM), and phosphate-buffered saline (PBS) solution (pH 7.2) were bought from HiMedia Laboratories in China.
Atractylodin cytotoxicity on colon cancer cells. A Molecular structure of atractylodin. B Cytotoxic effect of atractylodin on HCT116 and C HT29 cells. Atractylodin exhibited concentration-dependent inhibition of colon cancer cell proliferation. D Atractylodin inhibited the colony formation of colon cancer cells in a dose-dependent manner. The graphical representation shows the percentage of colony formation. E Atractylodin-induced ROS production in colon cancer cells according to the dose used. The increased green fluorescence indicates the increased ROS production in both HCT116 and HT29 cells. The graphical representation shows the amount of ROS production determined by a spectrofluorometer. The bars reflect the mean ± standard error of three experiments. The scale bar is 100 μm
2.2 Cell culture
The HCT116 and HT29 human colon cancer cell lines were acquired from the ATCC and cultured in DMEM at 37 °C within a CO2 incubator. Prior to being used for cell treatment, atractylodin was prepared in dimethyl sulfoxide (DMSO) at the desired concentrations.
2.3 Cytotoxicity of atractylodin on HCT116 and HT-29 cells
The antiproliferative effects of atractylodin on colon cancer cells were assessed by MTT assay. The colon cancer HCT116 and HT29 cells were seeded in a 96-well plate at 10,000 cells/well density and incubated in a humidified environment for 24 h. The cells were then exposed to increasing doses (5–80 µM) of atractylodin for 24 h, while control wells received no treatment. MTT reagent (5.0 mg/mL in PBS) was added to the wells and kept in a dark condition for 4 h to generate formazan crystals. After incubation, the formazan crystals were dissolved in each well by adding 100 µL of DMSO. The optical intensity of each well was measured using a Tecan Multimode Reader at 570 nm wavelength. Subsequently, regression analysis was conducted to calculate the concentration of atractylodin that caused 50% cell death.
2.4 Cell colonisation assay
To examine the effects of atractylodin on colon cancer cell colony formation, HCT116 and HT29 cells were cultured in 24-well plates at a density of 1000 cells/well and kept to adhere for 24 h. Subsequently, the cells were exposed to varying doses of atractylodin (0, 20, 40, and 60 µM) for an additional 24 h under humidified conditions. After treatment, the cells were washed with cold PBS, fixed in 70% ethanol at − 20 °C for 24 h, and stained with crystal violet (0.01% wt/vol) for 30 min at room temperature. Finally, the cells were visualised under a light microscope to assess their colonisation ability.
2.5 Determination of ROS
The ROS production in colon cancer cells was measured by exposing the cells to DCFH-DA, which is oxidised into fluorescent DCF upon exposure to ROS [21]. HCT116 and HT29 cells were cultured in six-well plates at a density of 1 × 106 cells/well for 24 h. The cells were then treated with atractylodin at concentrations of 20, 40, and 60 µM for 24 h. Following treatment, the cells were exposed to 100 µL of DCFH-DA for 10 min and observed under a fluorescence microscope with suitable filters. The production of ROS was spectroscopically analysed by measuring the fluorescence intensity of trypsin zed cells using fluorescence spectroscopy. The percentage of ROS activity in the cells was then compared to that of the untreated control cells.
2.6 Apoptosis analysis
To investigate the impact of atractylodin on apoptotic cell death, HCT116 and HT29 cells were seeded in 6-well plates at 4 × 105 cells/well and exposed to atractylodin at concentrations of 0, 20, 40, and 60 µM for 24 h. After treatment, the cells were collected, washed with PBS, and centrifuged at 10,000g for 5 min. The resulting cell pellet was resuspended in 1× binding buffer and subjected to staining with FITC Annexin V following the manufacturer's instructions. Cell death was assessed by flow cytometry utilising a BD LSRFortessa cytometer and BD FACSDiva Software. A total of 10,000 events were analysed per sample, and the percentages of viable, early apoptotic, late apoptotic, and necrotic cells were determined while excluding cellular debris from the analysis.
2.7 Biochemical assay
To evaluate the effects of atractylodin on lipid peroxidation and antioxidant activity, biochemical assays such as LPO, SOD, CAT, and GPx were performed on HCT116 and HT29 cells treated with 0, 20, 40, and 60 µM of atractylodin. The cells were collected by trypsinisation and lysed for biochemical analysis. The LPO biomarker TBARS was measured using a previously described method. The activities of SOD, CAT, and GPx were also determined in the cell lysates. These assays can provide information on the oxidative stress status of the cells and the effectiveness of the antioxidant defense system [22]. The antioxidants in colon cancer cells were analysed by measuring the enzymatic activity of SOD, CAT, and GPx by following the previously mentioned protocol [23,24,25].
2.8 Determination of DNA damage (comet assay)
The DNA cleavage in HCT116 and HT29 cells induced by the treatment of atractylodin was assessed through gel electrophoresis. The cells were collected post-treatment and suspended in PBS. A portion of the cell suspension was combined with low-melting agarose and poured onto slides, which were cooled to solidify the agarose. The slides were then transferred to ice-cold lysis buffer and held for 1 h at 4 °C to release the DNA, followed by a 30-min incubation in an electrophoresis solution. The DNA was separated through electrophoresis at 22 V and 200 mA. Following electrophoresis, the slides were neutralised with Tris (pH 7.5) for 10 min, fixed with 70% ethanol, and stained with EB for 20 min in the dark. The DNA was visualised with a fluorescent microscope at 40× magnification using a digital camera.
2.9 Western blot analysis
Protein expression was analysed by western blotting to understand how atractylodin affects signalling pathways in colon cancer cells. Atractylodin was administered to HCT116 and HT29 cells for 24 h, after which the cells were trypsin zed and collected. RIPA lysis buffer was used to lyse the cell pellet, and SDS-PAGE was used to separate the protein. The separated proteins were then put on a PVDF membrane and left set at room temperature for two hours while being blocked with 5% BSA. After that, the membrane was treated with primary antibodies (1:1000) overnight at 4 °C for cleaved caspase 3, p53, Bcl-2, Bax, PI3K, Akt, mTOR, p70S6K, and -actin. After being washed, the membrane was treated for an hour with secondary antibodies that had been HRP-conjugated. Protein expression was observed using a chemiluminescence kit according to the manufacturer's protocol (Amersham Biosciences, Buckinghamshire, UK).
2.10 In silico molecular docking
In this study, molecular docking analysis was used to understand the binding interactions between atractylodin and the target protein PI3Kγ. The PDB file for the protein was retrieved from the Protein Data Bank (PDB) website https://www.rcsb.org/, and the structure of atractylodin was retrieved from the PubChem database https://pubchem.ncbi.nlm.nih.gov/. Using Discovery Studio 2021 Visualiser, the protein's structure was optimised by getting rid of co-crystallised ligands, heteroatoms, and water molecules. By introducing polar hydrogen bonds and charging the molecules, respectively, the protein and atractylodin were made ready for docking. The protein–ligand interactions and minimum binding energy that resulted from the docking analysis were examined using BIOVIA Discovery Studio and AutoDock Vina, respectively. Protein–ligand sites (amino acids) and minimum binding energy interactions were interpreted following protein and ligand docking analysis.
2.11 Colon carcinoma xenograft model
The C.B-17 SCID mice (20–25 g, n = 24) were obtained and used to test the antitumourogenic effect of atractylodin on the colon cancer xenograft model. The mice were kept in cages for 7 days before the tumour induction was initiated to give animals adapted to laboratory environmental conditions free access to food and water. Lighting was turned on at 6:00 a.m. and there was a 12:12 light–dark cycle in the housing. The institution Soochow University Animal Ethics Committee approved the treatment and use of the mice following the ethical guidelines for using animals in research.
The experimental mice were subcutaneously injected with colon cancer HCT116 cells (2 × 107 cells/500 µL) using an injection needle. All injected mice were randomly alienated into the 4 groups (n6). Group 1 mice received 0 µM of atractylodin with the vehicle (5% DMSO), while groups 2, 3, and 4 received 5, 50, and 100 mg/kg/day of atractylodin with the vehicle, respectively. The treatment began the day after the injection of the cancer cells and was given intraperitoneally once daily for 15 days. After the experiment, animals were euthanised by anaesthetic overdose, and tumours were excised and weighed. Tumour volume was calculated using the formula: ½ (length × width × height).
2.12 Statistical analysis
All data were analysed using GraphPad Prism Ver. 6.0 software. The results are expressed as the mean ± SEM, and statistical significance was determined at a p value of < 0.05. Unpaired t test or one-way ANOVA with Tukey's post hoc test were used to compare the control and treatment groups.
3 Results
3.1 Atractylodin inhibits cell proliferation and colonisation of colon cancer cells
To evaluate the antiproliferative effect of atractylodin on HCT116 and HT29 cells, we performed an MTT assay. The results demonstrated that treatment with atractylodin exhibited a dose-dependent decrease in cell viability. The IC50 concentrations of atractylodin for HCT116 and HT29 cells were found to be 39.28 ± 0.79 µM and 40.88 ± 0.79 µM, respectively (Fig. 1B, C). Furthermore, we assessed the effect of atractylodin on colon cancer cell colonisation by using crystal violet staining. We found that atractylodin treatment hindered the adherence of colon cancer cells in a concentration-established way control to untreated cells (Fig. 1D). These results propose that atractylodin inhibits cell proliferation and colonisation by inducing cell toxicity in colon cancer cells.
3.2 Atractylodin induces ROS-mediated apoptosis and DNA damage in colon cancer cells
To test the effect of atractylodin on ROS production and apoptosis induction in colon cancer cells, we measured the DCF fluorescence and used flow cytometry, respectively. Atractylodin treatment led to a dose-dependent increase in ROS production, as demonstrated by increased green fluorescence (Fig. 1E). Moreover, atractylodin-induced apoptosis in a dose-dependent manner, with HCT116 cells showing greater sensitivity than HT29 cells (Fig. 2A). These findings suggest that atractylodin inhibits cell proliferation in colon cancer cells by inducing ROS production and apoptosis.
A Flow cytometer analysis of atractylodin-induced cell death in HCT116 and HT29 cells. The graphical representation shows the percentage of atractylodin-induced cell death in HCT116 and HT29 cells. B Atractylodin-induced lipid peroxidation (TBARS) activity and reduced the SOD, CAT, and GPx activity in HCT116 and HT29 cells in a concentration-dependant manner. C The comet assay shows the DNA damage in HCT116 and HT29 cells induced by the treatment of atractylodin. The bars reflect the mean ± standard error of three experiments
Treatment with atractylodin significantly increased LPO activity and decreased the activity of SOD, CAT, and GPx in both HCT116 and HT29 cancer cells, according to the doses used. These changes are indicative of apoptosis in cancer cells. This was further confirmed by the augmented expression of cleaved caspase-3, a marker of apoptosis, in both cell lines after atractylodin treatment. Overall, our findings show that atractylodin treatment resulted in concentration-dependent induction of apoptosis in colon cancer cells through the upregulation of cleaved caspase 3 (Fig. 2B).
The present study found that atractylodin treatment caused significant DNA damage in colon cancer cells according to the treated concentrations. Control cells displayed nonfragmented, intact DNA, while atractylodin-treated colon cancer cells exhibited fragmented DNA, which appears as a comet-like structure during electrophoresis. The amount of DNA damage increased with increasing atractylodin concentration. These results suggest that atractylodin-induced apoptosis in colon cancer cells may involve DNA damage (Fig. 2C).
To test the apoptosis inducing mechanism of atractylodin in colon cancer cells, we analysed the expression of apoptotic proteins using western blotting. Our results showed that atractylodin treatment increased the expression of proapoptotic proteins p53 and Bax, while decreased the expression of antiapoptotic protein Bcl-2 in both HCT116 and HT29 cells, according to the concentrations treated. These findings indicate that atractylodin persuaded apoptosis in colon cancer cells may involve the regulation of p53, Bax, and Bcl-2 proteins (Fig. 3A).
Atractylodin increases the activity of cleaved caspase 3 and modulates apoptotic protein expression. A Atractylodin increased the cleaved caspase 3 expression, p53 and Bax expression, whereas downregulated the Bcl-2 expression in HCT-116 cells according to the concentrations used. B Atractylodin downregulated the phosphorylation of p-P13K/P13K, p-AKT/AKT, p-mTOR/mTOR and p70S6K in HCT116 and HT29 cells as per the concentrations used. C Atractylodin downregulated the expression of PI3Kγ in a dose-dependent manner, whereas showed no effect on the expression of PI3Kα, PI3Kβ, and PI3Kδ. D The PI3Kγ specific inhibitor AS605240 and atractylodin together moresignificantly inhibited the expression of PI3Kγ. E Flow cytometer analysis of atractylodin cotreated with PI3Kγ specific inhibitor AS605240-induced cell death in HCT116 and HT29 cells. The graphical representation shows the percentage of atractylodin-induced cell death in HCT116 and HT29 cells. The bars reflect the mean ± standard error of three experiments
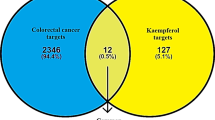
3.3 Atractylodin inhibits the PI3K/Akt/mTOR/ p70S6K signalling by reducing the PI3Kγ-p110 expression
The PI3K/Akt/mTOR/p70S6K signalling pathway regulates several cellular processes, including cell cycle, proliferation, apoptosis, and autophagy, targeting this pathway could be effective in the suppression of cancer progression. The PI3K/Akt/mTOR/p70S6K signalling pathway was tested using western blotting to determine its function in the induction of apoptosis in colon cancer cells. The outcomes demonstrated that atractylodin treatment inhibited p-PI3K, p-Akt, p-mTOR, and p70S6K in both HCT116 and HT29 cells based on the concentrations used (Fig. 3B). To determine if the PI3K/Akt/mTOR/p70S6K signalling pathway was affected by the inhibition of p110γ, we examined the expression of the PI3K catalytic subunits, including p110α, p110β, p110δ, and p110γ. The goal was to determine if any of these subunits were involved in blocking the signalling pathway. In colon cancer cells, atractylodin treatment reduced PI3Kγ-p110 levels in a dose-dependent manner while having little or no impact on PI3Kα, PI3Kβ, and PI3Kδ expression. These results suggest that atractylodin significantly downregulates the PI3K/Akt/mTOR/p70S6K signalling pathway through the inhibition of PI3Kγ in colon cancer cells (Fig. 3C).
The results indicate that inhibition of PI3Kγ may be a crucial factor in atractylodin-induced apoptosis. To confirm this hypothesis, colon cancer cells were treated with a combination of atractylodin and AS605240, a PI3Kγ-specific inhibitor, and the apoptotic response was evaluated. Co-treatment with a nontoxic dose of AS605240 (20 µM; 6.31%) and the IC50 concentration of atractylodin led to a significant increase in apoptosis in colon cancer cells. These findings provide additional support to the notion that suppression of PI3Kγ activity may contribute to the apoptotic effects of atractylodin in colon cancer cells (Fig. 3D, E).
3.4 Atractylodin dock in ATP binding pocket of PI3Kγ
In most cancer cells, PI3K/Akt signalling is involved in regulating cell proliferation. Molecular docking analysis was performed to explore the binding of atractylodin to the ATP binding pocket of the PI3Kγ protein. The results showed that atractylodin forms hydrogen bonds with several residues in the pocket, including LYS-833, LYS-808, LYS-807, VAL-882, TYR-867, and GLU-880. In addition, there are hydrophobic interactions between atractylodin and ASP-964, ILE-963, ILE-873, VAL-882, and ILE-831. The minimum binding energy calculated in the analysis was − 6.7 kcal/mol. These findings suggest that atractylodin can bind to PI3Kγ and interact with residues important for its catalytic activity, such as LYS-833 and ASP-964 (Fig. 4).
3.5 Atractylodin inhibits HCT116 cell growth in the xenograft mice model
We created HCT116 xenograft tumour model in C.B-17 SCID mice and administered daily oral gavages of 5, 50, and 100 mg/kg atractylodin or vehicle to the animals in order to further support the antitumourigenic characteristics of atractylodin that were seen in vitro (Fig. 5A). Body and organ (liver and lung) weights were evaluated at the end of the experiments to evaluate the toxicological effects of atractylodin treatment. The final body weight was significantly reduced in the mice treated with 100 mg/kg of atractylodin than the control group. However, no significant changes were observed in the lung and liver weight in the treatment group compared to the untreated control group (Table 1).
A Schematic presentation of a mice tumour xenograft model of colon cancer. B Xenograft tumour collected from sacrificed mice (n = 6) at the end of treatments. C, D atractylodin reduced the tumour volume and tumoir weight according to the concentrates used. The bars reflect the mean ± standard error of three experiments
At day end of the treatment, 50 and 100 mg/kg of atractylodin treated group displayed lower tumour volume than the controls, while no significant reduction in tumour growth was observed in the 5 mg/kg of atractylodin treated group than the control group (Fig. 5B). Consistently, the tumour weight of 50 and 100 mg/kg of atractylodin-treated animals was lower than controls (Fig. 5C). However, no significant reduction in tumour volume in 5 mg/kg of atractylodin-treated group (Fig. 5D). Collectively our data suggest that the oral intake of atractylodin significantly inhibits the tumour growth in colon cancer tumour xenograft modal by inducing apoptotic cell death through inhibition of PI3K/Akt/mTOR/p70S6K signaling (Fig. 6).
4 Discussion
Atractylodin exhibits notable cytotoxic properties against various cancerous cells, according to numerous studies. Reactive oxygen species (ROS) levels are increased, and intracellular antioxidant activity is decreased [18, 19]. Lipid peroxidation activity significantly increases as a result of oxidative stress brought on by cancer cells' excessive production of endogenous oxidative free radicals [26]. This rise in lipid peroxidation, along with a drop in endogenous antioxidant levels, is a factor in the apoptotic characteristics seen in cancer cells [27, 28]. A vital antioxidant in cellular metabolism, superoxide dismutase (SOD) guards against endogenous free radicals. SOD activity has been found to be lower in cancer and asthma cases than in healthy people [29, 30]. In the current study, we discovered decreased antioxidant and increased ROS activities in atractylodin-treated HCT116 and HT29 cells. Damage to DNA, proteins, and lipids can result from the ROS produced by oxidative stress, which can also cause cancer cells to activate the apoptotic protein p53 expression [31]. Oxidative modifications of oxidative transcriptional regulators and intermediary signalling molecules control ROS-mediated cell regulation [32]. A common apoptotic pathway chemotherapeutic drugs uses is double-strand DNA breaks, which can result from apoptosis and cause DNA damage [33]. In our study, atractylodin treatment caused significant DNA damage in HCT116 and HT29 cells, which was concentration-dependent and ultimately resulted in cell death.
The regulation of cellular processes like apoptotic changes, cell proliferation, and cellular reactions to cancer treatment is greatly regulated by apoptotic markers [34]. Antiapoptotic markers are homologs of proapoptotic markers, and the balance between the two is crucial for controlling apoptosis [35]. Anticancer medications typically work by increasing the expression of proapoptotic markers while decreasing the expression of antiapoptotic markers as part of their adaptive mechanisms. In our investigation, we observed that atractylodin administration significantly modulated the expression of proapoptotic proteins, including p53, Bax, and Cleaved caspase-3, while suppressing the expression of the antiapoptotic marker Bcl-2. Apoptosis in colon cancer cells may begin as a result of atractylodin's suppression of Bcl-2. The p53 gene is activated as cellular oxidative stress occurs, causing cell cycle arrest and self-mediated apoptosis [36]. Additionally, elevated expression of cleaved caspase-3 can result in an immediate and permanent apoptosis in cancer cells. Our study observed increased expression of cleaved caspase-3 in HCT116 and HT29 cells treated with atractylodin, which resulted in a significant increase in apoptotic cells, as demonstrated by flow cytometric analysis. These results suggest that atractylodin alters the balance of proapoptotic and antiapoptotic protein expressions to increase apoptosis in colon cancer cells.
The PI3K pathway plays a significant role in cancer and is a primary target for cancer treatment. Various oncogenes and growth factor receptors stimulate activation of PI3K [37]. The PI3K pathway is a key target for cancer therapy because it plays a significant role in cancer. Different oncogenes and growth factor receptors promote PI3K activation [37]. Due to their role in the growth of human malignancies, Class I PI3Ks have special therapeutic relevance. Class I PI3Ks are heterodimers made up of catalytic (p110α, p110β, p110δ, or p110γ) and regulatory (p85α, p55α, p50α, p85β, p55γ, or p101) subunits. Protein kinase B/AKT and mTOR are two downstream effectors that the active p110 subunit activates [38]. The most often activated pathway in human cancers is the PI3K/Akt/mTOR/p70S6K pathway, making it a promising target for drug development. Cellular proliferation and death can result from inhibiting this pathway's signalling, which includes apoptosis and autophagy [39]. By inhibiting the PI3K/Akt/mTOR/p70S6K pathway, atractylodin found to induce apoptosis in this study effectively. According to the molecular docking results, atractylodin interacts with crucial residues involved in catalysis, including LYS-833 and ASP-964, and binds successfully to the ATP-binding pocket of PI3K. In addition, our findings demonstrated that atractylodin binds to the ATP binding pocket and inhibits the expression of PI3K, but not other PI3K isoforms like PI3K α, β, and δ. These results imply that atractylodin inhibits the PI3K/Akt/mTOR/p70S6K signalling pathway by blocking PI3K.
To assess the in vivo antitumour effect of atractylodin, we conducted the xenograft tumour model. atractylodin exhibited significant suppression of tumour growth in colon cancer tumour xenograft model in concentration-established way. These results show that the atractylodin effectively inhibited the tumour growth by blocking the PI3K/Akt/mTOR/p70S6K as evidenced by in vitro experiments. For example, the extract of Atractylodes lancea showed significant tumour suppression activity in a hamster model of Cholangiocarcinoma [40]
5 Conclusion
Our study's goal was to look into atractylodin's potential anticancer mechanisms in colon cancer xenograft tumour models and human colon cancer cells. Our findings show that atractylodin caused DNA fragmentation, ROS-mediated apoptosis, and cytotoxicity in the colon cancer cells HCT116 and HT29. In addition, it was discovered that atractylodin altered the expression of apoptotic proteins in these cancer cells, including p53, Bax, cleaved caspase 3 and Bcl-2. Interestingly, we found that atractylodin inhibited the PI3K/Akt/mTOR/p70S6K signalling pathway, possibly by downregulating PI3K, which led to the induction of apoptosis in colon cancer cells. As a result of these intriguing findings, atractylodin appears to hold promise as a colon cancer therapeutic.
References
R. Bar-Shalom, M. Bergman, S. Grossman, N. Azzam, L. Sharvit, F. Fares, Inula viscosa extract inhibits growth of colorectal cancer cells in vitro and in vivo through induction of apoptosis. Front. Oncol.Oncol. 9, 227 (2019)
Y. Zhao, X. Hu, X. Zuo, M. Wang, Chemopreventive effects of some popular phytochemicals on human colon cancer: a review. Food Funct.Funct. 9(9), 4548–4568 (2018)
T. Aoyagi, K.P. Terracina, A. Raza, K. Takabe, Current treatment options for colon cancer peritoneal carcinomatosis. World J. Gastroenterol. WJG 20(35), 12493 (2014)
S. Xiong, G.W. Xiao, Reverting doxorubicin resistance in colon cancer by targeting a key signaling protein, steroid receptor coactivator. Exp. Ther. Med.Ther. Med. 15(4), 3751–3758 (2018)
C. Holohan, S. Van Schaeybroeck, D.B. Longley, P.G. Johnston, Cancer drug resistance: an evolving paradigm. Nat. Rev. Cancer 13(10), 714–726 (2013)
J. Wehkamp, J. Harder, K. Wehkamp, B.W.V. Meissner, M. Schlee, C. Enders, U. Sonnenborn, S. Nuding, S. Bengmark, K. Fellermann, J.M. Schröder, Capecitabine as adjuvant treatment for stage III colon cancer. Infect. Immun. 72(10), 5750–5758 (2004)
F. Balkwill, A. Mantovani, Inflammation and cancer: back to Virchow. Lancet 357(9255), 539–545 (2001)
A. Mantovani, P. Allavena, A. Sica, F. Balkwill, Cancer-related inflammation. Nature 454(7203), 436–444 (2008)
M.G. Borrello, L. Alberti, A. Fischer, D. Degl’Innocenti, C. Ferrario, M. Gariboldi, F. Marchesi, P. Allavena, A. Greco, P. Collini, S. Pilotti, induction of a proinflammatory program in normal human thyrocytes by the RET/PTC1 oncogene. Proc. Natl. Acad. Sci. 102(41), 14825–14830 (2005)
K. Kawauchi, T. Ogasawara, M. Yasuyama, K. Otsuka, O. Yamada, Anticancer Agents Med Chem. 9, 1024 (2009)
H. Yamamoto, H. Shigematsu, M. Nomura, W.W. Lockwood, M. Sato, N. Okumura, J. Soh, M. Suzuki, I.I. Wistuba, K.M. Fong, H. Lee, PIK3CA mutations and copy number gains in human lung cancers. Cancer Res. 68(17), 6913–6921 (2008)
B.T. Hennessy, D.L. Smith, P.T. Ram, Y. Lu, G.B. Mills, Exploiting the PI3K/AKT pathway for cancer drug discovery. Nat. Rev. Drug Discov.Discov. 12, 988–1004 (2005)
C. Xu, Q. Wang, X. Feng, Y. Bo, Effect of evodiagenine mediates photocytotoxicity on human breast cancer cells MDA-MB-231 through inhibition of PI3K/AKT/mTOR and activation of p38 pathways. Fitoterapia 99, 292–299 (2014)
J. Yang, C. Pi, G. Wang, Inhibition of PI3K/Akt/mTOR pathway by apigenin induces apoptosis and autophagy in hepatocellular carcinoma cells. Biomed. Pharmacotherapy 103, 699–707 (2018)
S.M. Simoes, A. Rey-Rico, A. Concheiro, C. Alvarez-Lorenzo, Supramolecular cyclodextrin-based drug nanocarriers. Chem. Commun.Commun. 51(29), 6275–6289 (2015)
K. Na-Bangchang, J. Karbwang, Traditional herbal medicine for the control of tropical diseases. Trop. Med. Health 42(2 Suppl), 3–13 (2014). https://doi.org/10.2149/tmh.2014-S01
K. Na-Bangchang, T. Plengsuriyakarn, J. Karbwang, Research and development of Atractylodes lancea (Thunb) DC. As a promising candidate for cholangiocarcinoma chemotherapeutics. Evid. Based Complement Alternat. Med. (2017). https://doi.org/10.1155/2017/5929234
K. Kotawong, W. Chaijaroenkul, P. Muhamad, K. Na-Bangchang, Cytotoxic activities and effects of atractylodin and β-eudesmol on the cell cycle arrest and apoptosis on cholangiocarcinoma cell line. J. Pharmacol. Sci.Pharmacol. Sci. 136(2), 51–56 (2018)
V.B. Mathema, W. Chaijaroenkul, K. Na-Bangchang, Cytotoxic activity and molecular targets of atractylodin in cholangiocarcinoma cells. J. Pharm. Pharmacol.Pharmacol. 71, 185–195 (2019)
Z. Li, Y. Song, W. Hou, Y. Qi, X. Lu, Y. Xue, J. Huang, Q. Fang, Atractylodin induces oxidative stress-mediated apoptosis and autophagy in human breast cancer MCF-7 cells through inhibition of the P13K/Akt/mTOR pathway. J. Biochem. Mol. Toxicol.Biochem. Mol. Toxicol. 36(8), e23081 (2022). https://doi.org/10.1002/jbt.23081
C.P. Wan, E. Myung, B.H. Lau, An automated micro-fluorometric assay for monitoring oxidative burst activity of phagocytes. J. Immunol. MethodsImmunol. Methods 159(1–2), 131–138 (1993)
H. Ohkawa, N. Ohishi, K. Yagi, Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal. Biochem.Biochem. 95(2), 351–358 (1979)
Z.Y.P. Kakkar, B. Das, P.N. Viswanathan, A modified spectrophotometric assay of superoxide dismutase (SOD). Indian J. Biochem. Biophys.Biochem. Biophys. 21, 1302 (1984)
K.A. Sinha, Colorimetric assay of catalase. Anal. Biochem.Biochem. 47, 38994 (1972). https://doi.org/10.1016/0003-2697(72)90132-7
M.S. Moron, J.W. Depierre, B. Mannervik, Levels of glutathione, glutathione reductase and glutathione S-transferase activities in rat lung and liver. Biochimica et biophysica acta (BBA) Gen. Subj. 582(1), 67–78 (1979)
H.U. Simon, A. Haj-Yehia, F. Levi-Schaffer, Role of reactive oxygen species (ROS) in apoptosis induction. Apoptosis 5, 4158 (2000). https://doi.org/10.1023/a:1009616228304
P.N. Shilpa, S. Sivaramakrishnan, D. Niranjali, Induction of apoptosis by methanolic extract of Rubia cordifolia Linn. in HEp-2cell line is mediated by reactive oxygen species. Asian Pac. J. Cancer Prev. 13, 27538 (2012). https://doi.org/10.7314/apjcp.2012.13.6.2753
S. Karthikeyan, S.L. Hoti, N.R. Prasad, Resveratrol loaded gelatin nanoparticles synergistically inhibits cell cycle progression and constitutive NF-kappaB activation, and induces apoptosis in non-small cell lung cancer cells. Biomed. Pharmacotherapy 70, 274–282 (2015)
U. Yadav, K.V. Ramana, Regulation of NF-B-induced inflammatory signaling by lipid peroxidation-derived aldehydes. Oxid. Med. Cell. Longev. 1–11 (2013)
Y. Kamaraj, S. Dhayalan, U. Chinnaiyan, V. Kumaresan, S. Subramaniyan, D. Kumar, K. Muniyandi, G. Punamalai, Triterpenoid compound betulin attenuates allergic airway inflammation by modulating antioxidants, inflammatory cytokines and tissue transglutaminase in ovalbumin-induced asthma mice model. J. Pharm. Pharmacol.Pharmacol. 73(7), 968–978 (2021)
E.A. Murphy, B.K. Majeti, L.A. Barnes, M. Makale, S.M. Weis, K. Lutu-Fuga, W. Wrasidlo, D.A. Cheresh, Nanoparticle-mediated drug delivery to tumor vasculature suppresses metastasis. Proc. Natl. Acad. Sci. 105(27), 9343–9348 (2008)
C.H. Kuo, M.H. Huang, Morphologically controlled synthesis of Cu2O nanocrystals and their properties. Nano Today 5(2), 106–116 (2010)
M.H. Cheng, Y.C. Yang, Y.H. Wong, T.R. Chen, C.Y. Lee, C.C. Yang, S.H. Chen, I.N. Yang, Y.S. Yang, H.S. Huang, C.Y. Yang, B1, a novel topoisomerase II inhibitor, induces apoptosis and cell cycle G1 arrest in lung adenocarcinoma A549 cells. Anticancer Drugs 23(2), 191–199 (2012)
R.J. Youle, A. Strasser, The BCL-2 protein family: opposing activities that mediate cell death. Nat. Rev. Mol. Cell Biol. 9(1), 47–59 (2008)
H. Burger, K. Nooter, A.W. Boersma, C.J. Kortland, G. Stoter, Expression of p53, Bcl-2 and Bax in cisplatin-induced apoptosis in testicular germ cell tumour cell lines. Br. J. Cancer 77(10), 1562–1567 (1998)
S.J. Collis, T.L. DeWeese, P.A. Jeggo, A.R. Parker, The life and death of DNA-PK. Oncogene 24(6), 949–961 (2005)
Z. Li, X. Zhang, Kinases involved in both autophagy and mitosis. Int. J. Mol. Sci. 18(9), 1884 (2017)
P.K. Vogt, J.R. Hart, M. Gymnopoulos, H. Jiang, S. Kang, A.G. Bader, L. Zhao, A. Denley, Phosphatidylinositol 3-kinase: the oncoprotein. Curr. Top. Microbiol. Immunol. 347, 9–104 (2010)
Z.H. Ouyang, W.J. Wang, Y.G. Yan, B. Wang, G.H. Lv, The PI3K/Akt pathway: a critical player in intervertebral disc degeneration. Oncotarget 8(34), 57870 (2017)
P. Sonsomnuek, M. Tarasuk, T. Plengsuriyakarn, K. Boonprasert, K. Na-Bangchang, Apoptotic and anti-metastatic effects of Atractylodes lancea (Thunb.) DC. in a hamster model of cholangiocarcinoma. Asian Pac. J. Cancer Prev. 23(9), 3093–3101 (2022). https://doi.org/10.31557/APJCP.2022.23.9.3093
Acknowledgements
The authors acknowledge the Department of Minimally Invasive Surgery, The First Affiliated Hospital of Soochow University, for the support during the study.
Funding
There was no specific grant funding received for this research from any public, commercial, or nonprofit organisations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lu, W., Liu, J., Wu, B. et al. Atractylodin induces apoptosis through downregulation of PI3Kγ-mediated PI3K/Akt/mTOR/p70S6K signalling in colon cancer cells and suppresses the tumour formation in xenograft mice model. Macromol. Res. 32, 159–171 (2024). https://doi.org/10.1007/s13233-023-00220-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13233-023-00220-y