Abstract
This study aims to determine if younger men, across racial and ethnic groups, discussed the benefits/risks/harms of PSA screening with health care professionals. Publicly available data were obtained from the Health Information National Trends Survey https://hints.cancer.gov/ in March 2019. Cross-sectional analysis of 518 men between the ages of 18 and 49 years from men who completed the survey between October 2011 and February 2012 (HINTS cycle 4) was performed. We used logistic regression to evaluate the association between race/ethnicity and discussions around PSA. Less than 10% of the participants reported a prior PSA; Black and Hispanic men were more likely compared with White men. Compared with White men, Black and other race men reported receiving less communications from some doctors recommending PSA screening (ORblack: 0.16, 95% CIblack: 0.07-0.38; ORother: 0.10, 95% CIother: 0.04-0.25), and that no one is sure PSA testing saves lives (ORblack: 0.49, 95% CIblack: 0.04-6.91; ORother: 0.17, 95% CIother: 0.06-0.48). Minority men, while more likely to have had a PSA, were less likely to be told of the harms and benefits of PSA testing, compared with White men. Increasing communication surrounding screening advantages and disadvantages between providers and patients can increase awareness and knowledge among younger men. In a post-COVID-19 environment, communication regarding the return to preventative screenings within vulnerable populations is an important message to convey. Research shows preventive screenings have dropped across all population groups due to the pandemic yet the decline disproportionately affects Black and other minority men.
Similar content being viewed by others
Introduction
Prostate cancer (PCa) is the most commonly diagnosed cancer and the second leading cause of death among all men in the USA, with an estimated 190,000 new cases and over 33,0000 deaths in 2020 [1]. Data from the nationally representative Surveillance, Epidemiology, and End Results (SEER) program show that Black men have an increased risk of overall prostate cancer and a 2-fold increased risk of dying from prostate cancer, compared to White men [2, 3]. Health disparities in PCa remain significant contributors to negative outcomes in quality of life and morbidity for Black men. The reasons for PCa disparities are likely multifactorial, including access to care and biological mechanisms.
Prostate cancer-specific antigen (PSA)-based screening, measuring the level of PSA in the blood, was approved by the FDA in 1994 to test asymptomatic men for prostate cancer. The goal of screening is to identify high-risk, localized prostate cancer to prevent morbidity and mortality from the disease. However, in 2012, the United States Preventive Services Task Force (USPSTF) recommended against PSA screening for all men, due to the perceived harms outweighing reported survival benefits [4]. In that recommendation, the USPSTF suggested the use of informed decision-making in patient-provider communications on case-by-case basis. In 2018, updated recommendations more explicitly state that men aged 55-69 should discuss the benefits and harms of screening with their provider [5].
These screening recommendations promulgated by the USPSTF have created a conundrum for health care providers. Following supposedly detailed discussions with their health care provider, men are to share in the decision-making process as it relates to initiation and termination of screening, incorporating their values and preferences into the decision. Using data from the Health Information National Trends Survey (HINTS), Leyva and colleagues [6] found among older men, discussions between providers and their patients were less likely to occur when the patient was Black or had lower educational achievement. Other studies report similar conclusions regarding the lack of discussions between health care providers and patients on PCa screening and treatment options [7,8,9]. In these studies, the focus has mainly been older adult males, typically >55 and above.
Guidelines from the American Cancer Society recommend that men receive information regarding PCa somewhere between the ages of 40 and 50 [10]. This is particularly recommended for those men at high risk for developing PCa, such as men with a family history of the disease or those of African ancestry. Racial disparities relative to diagnosis and treatment options for PCa among minority men in general and Black men in particular are well known and continue to have long-term adverse consequences for mortality and morbidity among that population. Black men are more likely to have a longer screening interval before diagnosis [11] and are less likely to receive appropriate treatment when diagnosed with PCa [12]. It is unknown if younger minority men (< 55 years) have received any information regarding PCa from their health providers or participated in PCa screening. Therefore, we sought to examine if younger men, particularly those under the recommended age for PCa screening to begin, discussed with their health care providers the benefits, risks, and potential harms of PCa screening using the nationally representative HINTS study.
Methods
Study Population
We obtained publicly accessible data from the Health Information National Trends Survey (HINTS) (https://hints.cancer.gov/). The HINTS collects cross-sectional data from a nationally representative random sample of the adult (18+) population about cancer-related information using computer-assisted telephone interviews. The HINTS began collecting data in 2003 and is administered by the National Cancer Institute (NCI). Additional background on the HINTS is described by Nelson et al. [13].
For this analysis, we used data from HINTS 4 cycle 1. Data from this questionnaire were collected between October 2011 and February 2012. We restricted the study population to male respondents (n = 1552) and excluded those with a prior history of prostate cancer (n = 77). Finally, because we were interested in the experience of younger men, we restricted our analytic population to those aged 18-49 years (n = 518).
Measures of Shared Decision-making and Communication
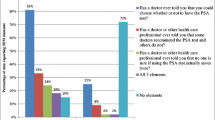
Questions assessing communication and shared decision-making between men and their provider included the following: (1) Has a doctor ever told you that you could choose whether or not to have the PSA test?; (2) Has a doctor or other health care professional ever told you that no one is sure if using the PSA test actually saves lives?; and (3) Has a doctor or other health care professional told you that some doctors recommend the PSA test and others do not?. These questions have been characterized as a physician’s discussion of advantages, disadvantages, and uncertainty associated with the PCa screening [9]. Additionally, we assessed the use of PSA testing among this younger population of men at risk of prostate cancer by analyzing the question: “have you ever had a PSA test?” Response choices to these questions were “yes,” “no,” and “not sure”.
Statistical Analysis
Descriptive statistics were calculated (means and frequencies) comparing demographic characteristics for the different PSA-related questions. We conducted multivariable logistic regression to calculate odds ratios and 95% confidence intervals (95% CIs) for the association between race, categorized as non-Hispanic White, non-Hispanic Black, Hispanic, and non-Hispanic other, and each measure of shared decision-making and communication, adjusting for age insurance, urban/rural, marital status, income, education, and trust in doctor. All statistical analyses were conducted in SAS v 9.4 9 (SAS, Cary, NC) taking into account the survey weights and survey design of the HINTS.
Results
Among the 518 men who met the eligibility criteria for this study, the majority were 18-34 years old (53.6%). In addition, 61% were non-Hispanic White and 11.5% non-Hispanic Black. The majority of participants were also living in an urban area (86.1%), had insurance (72.9%), had a regular doctor (65.6%), and had a lot of trust in their doctor (70.4%) (Table 1).
Less than 10% of the younger participants had ever had a PSA test (8.5%) and 11% reported receiving information about a choice surrounding PSA testing. Furthermore, less than 5% of participants reported knowing that some doctors recommend the PSA test (4.3%) and 2.7% reported that their doctor ever told them no one is sure if using the PSA test actually saves lives (Table 1).
Among younger men, non-Hispanic Black men were more likely to report ever having had a PSA test, compared with non-Hispanic White men but this result did not reach statistical significance (Table 2). Similarly, non-Hispanic Black men were more likely to report having a doctor tell them one could choose whether or not to have the PSA test (OR: 3.13, 95% CI: 0.88-11.18). However, non-Hispanic Black and other minority men were less likely to report being told that some doctors recommend a PSA test and others do not as well as being told that no one is sure PSA testing saves lives (Table 2). To compare our results to previously published papers [6], we also conducted the analysis among older men (50-74 years). We found, contrary to the results among younger men, non-Hispanic Black men (OR: 0.34, 95% CI: 0.14-0.81) and Hispanic men (OR: 0.88, 95% CI: 0.26-3.01) were less likely to report being told that you could choose whether or not to have the PSA test, compared with non-Hispanic White men.
Discussion and Conclusions
In this study, we found that among younger men, 8% reported having ever had a PSA test, and Black and Hispanic men were more likely to report having had a prior PSA, compared with non-Hispanic White men. However, we also found that Black men were less likely to be told of the harms and benefits of the PSA test, including whether or not medical professionals recommend the test and its potential effectiveness in saving lives. These findings lend support to the idea that ineffective communication between some health care providers and Black men regarding PCa and PSA screening in particular contributes to lack of shared decision-making, and may contribute to observed racial disparities in disease epidemiology and outcome [7]. Improving communication by both clinicians and community-based educators [9] is essential to closing the disparity gap with this disease.
Black men are more likely to have a longer screening interval before diagnosis [11] and are less likely to receive appropriate treatment when diagnosed with PCa [12]. Indeed, Black men are 2.20 times more likely to die from PCa than non-Hispanic White men [1]. Taken together, these findings strongly suggest that Black men with at least moderate risk tumors and a life expectancy of more than 10 years would likely benefit from early detection and treatment [13]. Current data [7, 14] clearly indicate the benefit of aggressive PCa screening in the Black population. However, in order for patients to participate in truly informed decision-making, it is imperative for there to be mechanisms put into place to educate high-risk populations of the benefits, risks, and harms of screening and treatment.
Due to COVID-19 implications, there has been a significant reduction in preventive cancer screenings and diagnoses since lockdowns were instituted in response to the pandemic [15, 16]. In a post-COVID environment, it will be essential for health care providers to educate and inform vulnerable populations of the need to return to or begin participation in cancer screenings or the potential for further increases in health disparities associated with PCa and other health conditions will continue to increase.
Prior studies have shown differences between Black and non-Black men surrounding knowledge of PCa and PSA screening [17,18,19,20,21,22], as well as likelihood of PSA screening prior to diagnosis. Carter et al. [11] utilizing the SEER database found that Blacks were less likely to have received PSA screening prior to being diagnosed. Additionally, Black men had higher odds of being diagnosed with a more advanced stage of cancer thus limiting treatment options in certain situations. Similarly, Sammon et al. [23], using the Behavioral Risk Factor Surveillance System (BRFSS) data, found that non-Hispanic White men reported higher rates of PSA screening than Black men. However, similar to our study, they also showed that Black men between the ages of 40 and 60 were more likely to have had a prior PSA test in the preceding year than non-Hispanic White men.
In order for individuals to participate actively and knowledgeably in decisions regarding PSA screening, health care providers must provide an adequate level of patient counseling regarding the natural history of PCa and the risks and benefits of screening. However, the literature suggests that Black men across the age spectrum possess limited knowledge regarding PCa [21, 22, 24], which in turn limits their ability to effectively communicate and participate in shared decision-making with their providers. Early intervention, including addressing deficiencies in knowledge of PCa and PSA screening at a younger age, may mitigate the disparities in disease outcomes that become apparent later in life. Indeed, PCa among younger men is a growing challenge with data showing increased incidence of PCa in younger men (<55) increased from 5.6 to 32 cases per 100,000 between 1986 and 2008, a change that was more pronounced than that among older men; younger men diagnosed with PCa also have lower survival rates. Therefore, younger men may benefit from earlier screening for PCa. However, research assessing the level of knowledge of younger men is limited in the current literature [21, 22]. A prior study by Ogusanya et al. [22] found Black men between the ages of 18 and 40 possessed less knowledge of PCa compared to that of older men. We similarly found that although Black men were more likely to have had a PSA test, they were less likely to have had conversations about the pros and cons of screening, compared to non-Hispanic White men. As Ogunsanya and colleagues posit, assessing the knowledge of younger men may contribute to the development of strategies that can improve PCa awareness among high-risk and yet underserved populations of men.
The continued controversy surrounding PCa screening recommendations needs further examination as well. Organizations such as the American Cancer Society along with Black physicians’ groups have voiced opposition as well as recommended earlier and universal screening for high-risk populations (i.e., Black men) beginning at earlier ages. It must be kept in mind the USPSTF recommendations were based on studies in which there were insufficient numbers of Black men participating [7, 25].
The current study further investigates the impact of patient-provider communication on the likelihood of PSA screening. Examining and understanding patient-provider communication (and deficiencies therein) with men prior to the recommended screening age for PCa may identify interventions for both patients and providers that can ultimately improve disease outcomes. Our study was limited by the cross-sectional nature of the design and the use of secondary data. We could only analyze the questions asked of the respondents. Nonetheless, given the nationally representative sampling used, we believe the findings shed additional insight into the discussions between providers and young men, particularly those of color, regarding PSA screening.
PCa disparities remain even as the incidence of the condition has held steady or declined slightly over the decades. As research into biological and environmental factors associated with the disease expands, increasing the communication between the providers may serve to further the awareness and knowledge of the patients. This clearly targeted communication may further reduce the persistent gap between Black and White men regarding PCa. It is imperative to continue examining patient-provider communication regarding health information particularly when discussing matters involving cancer screening and assessing family history of the disease. Early exposure to information regarding screening options, advantages, and disadvantages could facilitate younger men seeking additional information on their own.
Data availability
Data in this study are publicly available from the National Cancer Institute Health Information National Trends Survey (NCI HINTS) website: https://hints.cancer.gov/.
References
American Cancer Society (2019) Cancer Facts & Figures for African Americans; 2019-2021. American Cancer Society, Atlanta
Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds) SEER Cancer Statistics Review, 1975-2017. National Cancer Institute, Bethesda
https://seer.cancer.gov/csr/1975_2017/, based on November 2019 SEER data submission, posted to the SEER web site, April 2020. Retrieved 1 June 2020
Chou R, Croswell JM, Dana T et al (2012) Screening for prostate cancer: a review of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 155:762–771
Grossman DC, Curry SJ, Owens DK et al (2018) Screening for Prostate Cancer US Preventive Services Task Force Recommendation statement. JAMA. 319(18):1901–1913. https://doi.org/10.1001/jama.2018.3710
Leyva B, Persoskie A, Ottenbacher A, Hamilton JG, Allen JD, Kobrin SC, Taplin SH (2016) Do men receive information required for shared decision making about PSA testing? Results from a national study. J Cancer Educ. 31:693–701. https://doi.org/10.1007/s13187-015-0870-8
Carpenter WR, Howard DL, Taylor YJ, Ross LE, Wobker SE, Godley PA (2010) Racial differences in PSA screening interval and stage at diagnosis. Cancer Causes Control. 21:1071–1080. https://doi.org/10.1007/s105552-010-9535-4
Fleshner K, Carlsson SV, Roobol MJ (2017) The effect of the USPSTF PSA screening recommendation on prostate cancer incidence patterns in the USA. Nat Rev Urol. 14:26–37. https://doi.org/10.1038/nrurol.2016.251
Han PK, Kobrin S, Breen N, Joseph DA, Li J, Frosch DL, Klabunde CN (2013) National evidence of the use of shared decision making Prostate-Specific Antigen screening. Ann Fam Med. 11(4):306–314. https://doi.org/10.1370/afm.1539
Wolf AMD, Wender RC (2010) Etzioni et al. American Cancer Society guideline for the early detection of prostate cancer: update 2010. CA Cancer J Clin. 60:70–98
Carter HB, Ferrucci L, Kettermann A, Landis P, Wright EJ, Epstein JI, Trock BJ, Metter EJ (2006) Detection of life-threatening prostate cancer with prostate-cancer antigen velocity during a window of curability. J Nat Cancer Inst. 98(21):1521–1527. https://doi.org/10.1093/jnci/djj410
Mahal BA, Zizer AA, Ziehr DR et al (2014) The association between insurance status and prostate cancer outcomes: implications for the Affordable Care Act. Prostate Cancer Prostatic Dis 17:273–279
Nelson DE, Kreps GL, Hesse BW, Croyle R, Willis G, Arora N, Rimer B, Vish Viswanath K, Weinstein N, Alden S (2004) The Health Information National Trends Survey (HINTS): development, design, and dissemination. J Health Commun 9:443–460. https://doi.org/10.1080/10810730490504233
Powell I, Vigneau FD, Bock CH, Ruterbusch J, Heilbrun LK (2014) Reducing prostate cancer racial disparity: evidence for aggressive early prostate cancer PSA testing of African American men. Cancer Epidemiol Biomarkers Prev 23(8):1505–1511
Sharpless NE (2020) COVID-19 and cancer. Science. 368(6497):1290
Schrag D, Hershman DL, Basch E (2020) Oncology practice during the COVID-19 Pandemic. [Published ahead of print April 13, 2020]. JAMA. https://doi.org/10.1001/jama.2020.6236
Halbert C, Gattoni-Celli S, Savage S et al (2017) Ever and annual use of prostate cancer screening in African American men. Am J Mens Health. 11(1):99–107. https://doi.org/10.1177/1557988315596225
Presley CJ, Raldow AC, Cramer LD, Soulos PR, Long JB, Yu JB, Makarov DV, Gross CP (2013) A new approach to understanding racial disparities in prostate cancer treatment. J Geriat Oncol. 4(1):1–8. https://doi.org/10.1016/j.jgo.2021.07.005
Bleyer A, Spreafico F, Barr R (2019) Published online 25 September 2019. Retrieved from) Prostate cancer in young men: an emerging young adult and older adolescent challenge. Cancer. https://doi.org/10.1002/cncr.32498
Salinas CA, Tsodikov A, Ishak-Howard M, Cooney KA (2014) Prostate cancer in young men: an important clinical entity. Nat Rev Urol. 11:317–323
Miller DB (2014) Pre-Screening Age African American Males: what do they know about Prostate Cancer screening, knowledge, and risk perceptions? Social Work in Health Care. 53(3):268–288. https://doi.org/10.1080/00981389.2013.875503
Ogunsanya ME, Brown CM, Odedina FT, Barner JC, Adedipe TB, Corbell B (2017) Knowledge of prostate cancer and screening among young multiethnic black men. Am J Mens Health. 11(4):1008–1018. https://doi.org/10.1177/1557988316689497
Sammon JD, Dalela Abdollah F, Choueiri Han PK et al (2016) Determinants of Prostate Specific Antigen screening among black men in the United States in the contemporary era. J Urol. 195:913–918. https://doi.org/10.1016/j.juro.2015.11.023
Daum LM, Reamer EN, Ruterbusch JJ, Liu J, Holmes-Rovner M, Xu J (2017) Patient knowledge and quality to treatment decisions for localized prostate cancer. J Am Board Fam Med. 30:288–297
Dess RT, Hartman HE, Mahal BA et al (2019) Association of black race with prostate cancer-specific and other-cause mortality [published ahead of print May 23, 2019]. JAMA Oncol. https://doi.org/10.1001/jamaoncol.2019.0826
Code Availability
Not applicable.
Author information
Authors and Affiliations
Contributions
David B. Miller: conceptualization, writing—original draft, and writing—review and editing; Sarah Markt: formal analysis, writing—review and editing, resources, and data curation; Carvell Nguyen: writing—review and editing and visualization; Oita K. Coleman: writing—review and editing and visualization.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable, data publicly available.
Competing Interests
The authors declare no competing interests.
Disclaimer
The research and interpretation of the data presented in this paper are that of the authors and do not reflect the official policy or opinion of the Health Information National Trends Survey.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Miller, D.B., Markt, S.C., Nguyen, C.T. et al. Prostate Cancer Screening and Young Black Men: Can Early Communication Avoid Later Health Disparities?. J Canc Educ 37, 1460–1465 (2022). https://doi.org/10.1007/s13187-021-01984-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-021-01984-6