Abstract
Background
DNA methylation is an important mechanism in epigenetics, which can change the transcription ability of genes and is closely related to the pathogenesis of ovarian cancer (OC). We hypothesize that DNA methylation is significantly different in OCs compared to controls. Specific DNA methylation status can be used as a biomarker of OC, and targeted drugs targeting these methylation patterns and DNA methyltransferase may have better therapeutic effects. Studying the key DNA methylation sites of immune-related genes (IRGs) in OC patients and studying the effects of these methylation sites on the immune microenvironment may provide a new method for further exploring the pathogenesis of OC, realizing early detection and effective monitoring of OC, identifying effective biomarkers of DNA methylation subtypes and drug targets, improving the efficacy of targeted drugs or overcoming drug resistance, and better applying it to predictive diagnosis, prevention, and personalized medicine (PPPM; 3PM) of OC.
Method
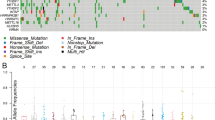
Hypermethylated subtypes (cluster 1) and hypomethylated subtypes (cluster 2) were established in OCs based on the abundance of different methylation sites in IRGs. The differences in immune score, immune checkpoints, immune cells, and overall survival were analyzed between different methylation subtypes in OC samples. The significant pathways, gene ontology (GO), and protein-protein interaction (PPI) network of the identified methylation sites in IRGs were enriched. In addition, the immune-related methylation signature was constructed with multiple regression analysis. A methylation site model based on IRGs was constructed and verified.
Results
A total of 120 IRGs with 142 differentially methylated sites (DMSs) were identified. The DMSs were clustered into a high-level methylation group (cluster 1) and a low-level methylation group (cluster 2). The significant pathways and GO analysis showed many immune-related and cancer-associated enrichments. A methylation site signature based on IRGs was constructed, including RORC|cg25112191, S100A13|cg14467840, TNF|cg04425624, RLN2|cg03679581, and IL1RL2|cg22797169. The methylation sites of all five genes showed hypomethylation in OC, and there were statistically significant differences among RORC|cg25112191, S100A13|cg14467840, and TNF|cg04425624 (p < 0.05). This prognostic model based on low-level methylation and high-level methylation groups was significantly linked to the immune microenvironment as well as overall survival in OC.
Conclusions
This study provided different methylation subtypes for OC patients according to the methylation sites of IRGs. In addition, it helps establish a relationship between methylation and the immune microenvironment, which showed specific differences in biological signaling pathways, genomic changes, and immune mechanisms within the two subgroups. These data provide ones to deeply understand the mechanism of immune-related methylation genes on the occurrence and development of OC. The methylation-site signature is also to establish new possibilities for OC therapy. These data are a precious resource for stratification and targeted treatment of OC patients toward an advanced 3PM approach.









Similar content being viewed by others
Data availability
All data and materials are provided in this article and supplemental materials, which can be available publicly.
Code availability
All protein and gene accession codes can be available in the Swiss-Prot and Genbank databases.
Abbreviations
- ADAR1:
-
Adenosine deaminase 1
- BPs:
-
Biological processes
- CTC:
-
Circulating tumor cells
- cfDNA:
-
Cell-free DNA
- ctDNA:
-
Circulating tumor DNA
- DCs:
-
Dendritic cells
- DMAPT:
-
Dimethylaminoporphanolide
- DMDGs:
-
Differential methylation-driven genes
- DMSs:
-
Differentially methylated sites
- DNMTs:
-
DNA methyltransferases
- DNMTi:
-
DNA methyltransferase inhibitors
- GO:
-
Gene ontology terms
- Hcy:
-
Homocysteine
- ICI:
-
Immune checkpoint inhibitor
- IL-1RL2:
-
Interleukin-1 receptor-like 2
- IRGs:
-
Immune-related genes
- KEGG:
-
Kyoto Encyclopedia of Genes and Genomes
- MDGs:
-
Methylation-driven genes
- MESA:
-
Multimodal epigenetic sequencing analysis
- MSP:
-
Methylation‑specific polymerase chain reaction
- OC:
-
Ovarian cancer
- OS:
-
Overall survival
- PACA:
-
Pancreatic cancer
- PPI:
-
Protein-protein interaction
- Sat2:
-
Satellite near the central point 2
- Satα:
-
Satellite near the central point α
- ssGSEA:
-
Single-sample Gene Set Enrichment Analysis
- TCGA:
-
The Cancer Genome Atlas
- TCRs:
-
T-cell antigen receptors
- TIME:
-
Tumor immune microenvironment
- TME:
-
Tumor microenvironment
- Tregs:
-
T-cell regulatory
- UCEC:
-
Uterus corpus endometrial cancer
- Aza-CdR:
-
5-Aza-2′-deoxycytidine
- 5mC:
-
5-Methylcytosine
References
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660.
Devouassoux-Shisheboran M, Genestie C. Pathobiology of ovarian carcinomas. Chin J Cancer. 2015;34(1):50–5. https://doi.org/10.5732/cjc.014.10273.
Gupta S, Nag S, Aggarwal S, Rauthan A, Warrier N. Maintenance therapy for recurrent epithelial ovarian cancer: current therapies and future perspectives - a review. J Ovarian Res. 2019;12(1):103. https://doi.org/10.1186/s13048-019-0579-0.
Roett MA, Evans P. Ovarian cancer: an overview. Am Fam Physician. 2009;80(6):609–16.
Yu L, Ding Y, Wan T, Deng T, Huang H, Liu J. Significance of CD47 and its association with tumor immune microenvironment heterogeneity in ovarian cancer. Front Immunol. 2021;12: 768115. https://doi.org/10.3389/fimmu.2021.768115.
Usach I, Blansit K, Chen LM, Ueda S, Brooks R, Kapp DS, Chan JK. Survival differences in women with serous tubal, ovarian, peritoneal, and uterine carcinomas. Am J Obstet Gynecol. 2015;212(2):188.e1-6. https://doi.org/10.1016/j.ajog.2014.08.016.
Buys SS, Partridge E, Black A, et al. Effect of screening on ovarian cancer mortality: the prostate, lung, colorectal and ovarian (PLCO) cancer screening randomized controlled trial. JAMA. 2011;305(22):2295–303. https://doi.org/10.1001/jama.2011.766.
Cohen JD, Li L, Wang Y, Thoburn C, Afsari B, Danilova L, et al. Detection and localization of surgically resectable cancers with a multi-analyte blood test. Science. 2018;359(6378):926–30. https://doi.org/10.1126/science.aar3247.
Vinson C, Chatterjee R. CG methylation. Epigenomics. 2012;4(6):655–63. https://doi.org/10.2217/epi.12.55.
Comb M, Goodman HM. CpG methylation inhibits proenkephalin gene expression and binding of the transcription factor AP-2. Nucleic Acids Res. 1990;18(13):3975–82. https://doi.org/10.1093/nar/18.13.3975.
Clark SJ, Harrison J, Molloy PL. Sp1 binding is inhibited by (m)Cp(m)CpG methylation. Gene. 1997;195(1):67–71. https://doi.org/10.1016/s0378-1119(97)00164-9.
Boyes J, Bird A. DNA methylation inhibits transcription indirectly via a methyl-CpG binding protein. Cell. 1991;64(6):1123–34. https://doi.org/10.1016/0092-8674(91)90267-3.
Zhang Y, Ng HH, Erdjument-Bromage H, et al. Analysis of the NuRD subunits reveals a histone deacetylase core complex and a connection with DNA methylation. Genes Dev. 1999;13(15):1924–35. https://doi.org/10.1101/gad.13.15.1924.
Nan X, Ng HH, Johnson CA, et al. Transcriptional repression by the methyl-CpG-binding protein MeCP2 involves a histone deacetylase complex. Nature. 1998;393(6683):386–9. https://doi.org/10.1038/30764.
Herman JG, Merlo A, Mao L, et al. Inactivation of the CDKN2/p16/MTS1 gene is frequently associated with aberrant DNA methylation in all common human cancers. Cancer Res. 1995;55(20):4525–30.
Xing XB, Cai WB, Liang L, et al. The prognostic value of p16 hypermethylation in cancer: a meta-analysis. Plos One. 2013;8. https://doi.org/10.1371/journal.pone.0066587.
Lahtz C, Pfeifer GP. Epigenetic changes of DNA repair genes in cancer. J Mol Cell Biol. 2011;3(1). https://doi.org/10.1093/jmcb/mjq053.
Biswas S, Rao CM. Epigenetics in cancer: fundamentals and beyond. Pharmacol Therapeutics. 2017;173:118–34. https://doi.org/10.1016/j.pharmthera.2017.02.011.
Li QL, Kim HR, Kim WJ, et al. Transcriptional silencing of the RUNX3 gene by CpG hypermethylation is associated with lung cancer. Bioch Biophys Res Commun. 2004;314(1):223–8. https://doi.org/10.1016/j.bbrc.2003.12.079.
Costa FF, Paixao VA, Cavalher FP, et al. SATR-1 hypomethylation is a common and early event in breast cancer. Cancer Genetics Cytogenetics. 2006;165(2):135–43. https://doi.org/10.1016/j.cancergencyto.2005.07.023.
Widschwendter M, Jiang G, Woods C, et al. DNA hypomethylation and ovarian cancer biology. Cancer Res. 2004;64(13):4472–80. https://doi.org/10.1158/0008-5472.CAN-04-0238.
Widschwendter M, Siegmund KD, Müller HM, et al. Association of breast cancer DNA methylation profiles with hormone receptor status and response to tamoxifen. Cancer Res. 2004;64(11):3807–13. https://doi.org/10.1158/0008-5472.CAN-03-3852.
Rodriguez J, Frigola J, Vendrell E, et al. Chromosomal instability correlates with genome-wide DNA demethylation in human primary colorectal cancers. Cancer Res. 2006;66(17):8462–9468. https://doi.org/10.1158/0008-5472.CAN-06-0293.
Qian ZR, Sano T, Yoshimoto K, Asa SL, Yamada S, Mizusawa N, Kudo E. Tumor-specific downregulation and methylation of the CDH13 (H-cadherin) and CDH1 (E-cadherin) genes correlate with aggressiveness of human pituitary adenomas. Mod Pathol. 2007;20(12):1269–77. https://doi.org/10.1038/modpathol.3800965.
Milicic A, Harrison LA, Goodlad RA, et al. Ectopic expression of P-cadherin correlates with promoter hypomethylation early in colorectal carcinogenesis and enhanced intestinal crypt fission in vivo. Cancer Res. 2008;68(19):7760–8. https://doi.org/10.1158/0008-5472.CAN-08-0020.
Paredes J. P-cadherin overexpression is an indicator of clinical outcome in invasive breast carcinomas and is associated with CDH3 promoter hypomethylation. Clinical Cancer Res. 2005;11(16):5869–77. https://doi.org/10.1158/1078-0432.CCR-05-0059.
Ribeiro AS, Albergaria A, Sousa B, et al. Extracellular cleavage and shedding of P-cadherin: a mechanism underlying the invasive behaviour of breast cancer cells. Oncogene. 2010;29(3):392–402. https://doi.org/10.1038/onc.2009.338.
Li T, Li Y, Gan Y, et al. Methylation-mediated repression of MiR-424/503 cluster promotes proliferation and migration of ovarian cancer cells through targeting the hub gene KIF23. Cell Cycle. 2019;18(14):1601–18.
Bandres E, Agirre X, Bitarte N, et al. Epigenetic regulation of microRNA expression in colorectal cancer. Int J Cancer. 2009;125(11):2737–43. https://doi.org/10.1002/ijc.24638.
He Y, Cui Y, Wang W, et al. Hypomethylation of the hsa-miR-191 locus causes high expression of hsa-miR-191 and promotes the epithelial-to-mesenchymal transition in hepatocellular carcinoma. Neoplasia. 2011;13(9):841–53. https://doi.org/10.1593/neo.11698.
Minor J, Wang X, Zhang F, et al. Methylation of microRNA-9 is a specific and sensitive biomarker for oral and oropharyngeal squamous cell carcinomas. Oral Oncol. 2011;48(1):73–8. https://doi.org/10.1016/j.oraloncology.2011.11.006.
Simonini P, Breiling A, Gupta N, et al. Epigenetically deregulated microRNA-375 is involved in a positive feedback loop with estrogen receptor alpha in breast cancer cells. Cancer Res. 2010;70(22):9175–84. https://doi.org/10.1158/0008-5472.CAN-10-1318.
Soto-Reyes E, Gonzalez-Barrios R, Cisneros-Soberanis F, et al. Disruption of CTCF at the miR-125b1 locus in gynecological cancers. BMC Cancer. 2012;12(1):40. https://doi.org/10.1186/1471-2407-12-40.
Yan F, Shen N, Pang J, Molina JR, Yang P, Liu S. The DNA methyltransferase DNMT1 and tyrosine-protein kinase KIT cooperatively promote resistance to 5-Aza-2’-deoxycytidine (Decitabine) and Midostaurin (PKC412) in lung cancer cells. J Biol Chem. 2015;290(30):18480–94. https://doi.org/10.1074/jbc.
Yang X, Han H, De Carvalho DD, et al. Gene body methylation can alter gene expression and is a therapeutic target in cancer. Cancer Cell. 2014;26(4):577–90. https://doi.org/10.1016/j.ccr.2014.07.028.
Sellars M, Huh JR, Day K, et al. Regulation of DNA methylation dictates Cd4 expression during the development of helper and cytotoxic T cell lineages. Nat Immunol. 2015;16(7):746–54. https://doi.org/10.1038/ni.3198.
Emran AA, Chatterjee A, Rodger EJ, et al. Targeting DNA methylation and EZH2 activity to overcome melanoma resistance to immunotherapy. Trends Immunol. 2019;40(4):328–44. https://doi.org/10.1016/j.it.2019.02.004.
Cai Y, Wu G, Peng B, et al. Expression and molecular profiles of the AlkB family in ovarian serous carcinoma. Aging (Albany NY). 2021;13(7):9679–9692. https://doi.org/10.18632/aging.202716.
Li T, Liu R, Zhang G, et al. Pan-cancer analysis of TLE3 revealed its value in tumor microenvironment and prognosis. J Oncol. 2022;2022:4085770. https://doi.org/10.1155/2022/4085770.
Wang C, Cicek MS, Charbonneau B, et al. Tumor hypomethylation at 6p21.3 associates with longer time to recurrence of high-grade serous epithelial ovarian cancer. Cancer Res. 2014;74(11):3084–91. https://doi.org/10.1158/0008-5472.CAN-13-3198.
Sharma S, Kelly TK, Jones PA. Epigenetics in cancer. Carcinogenesis. 2010;31(1):27–36.
Barton CA, Hacker NF, Clark SJ, et al. DNA methylation changes in ovarian cancer: implications for early diagnosis, prognosis and treatment. Gynecologic Oncol. 2008;109(1):129–39. https://doi.org/10.1016/j.ygyno.2007.12.017.
Zheng M, Hu Y, Gou R, et al. Integrated multi-omics analysis of genomics, epigenomics, and transcriptomics in ovarian carcinoma. Aging (Albany NY). 2019;11(12). https://doi.org/10.18632/aging.102047.
Terp SK, Stoico MP, Dybkær K, Pedersen IS. Early diagnosis of ovarian cancer based on methylation profiles in peripheral blood cell-free DNA: a systematic review. Clin Epigenetics. 2023;15(1):24. https://doi.org/10.1186/s13148-023-01440-w.
Luo GF, Chen CY, Wang J, et al. FOXD3 may be a new cellular target biomarker as a hypermethylation gene in human ovarian cancer. Cancer Cell Int. 2019;19:44. https://doi.org/10.1186/s12935-019-0755-8.
Wang J, Zhang T, Yang L, et al. Comprehensive genomic analysis of microenvironment phenotypes in ovarian cancer. Peer J. 2020. https://doi.org/10.7717/peerj.10255.
Ho CM, Lai HC, Huang SH, et al. Promoter methylation of sFRP5 in patients with ovarian clear cell adenocarcinoma. Eur J Clin Invest. 2010;40(4):310–8. https://doi.org/10.1111/j.1365-2362.2010.02266.x.
Giannopoulou L, Chebouti I, Pavlakis K, et al. RASSF1A promoter methylation in high-grade serous ovarian cancer: a direct comparison study in primary tumors, adjacent morphologically tumor cell-free tissues and paired circulating tumor DNA. Oncotarget. 2017;8(13): 21429–21443. https://doi.org/10.18632/oncotarget.15249.
Giannopoulou L, Mastoraki S, Buderath P, et al. ESR1 methylation in primary tumors and paired circulating tumor DNA of patients with high-grade serous ovarian cancer. Gynecol Oncol. 2018;150(2):355–60. https://doi.org/10.1016/j.ygyno.2018.05.026.
Smyth C, Curto J, Siddiqui N, et al. CpG island methylation of DNA damage response genes in advanced ovarian cancer. Cancer Res. 2005;65(19):8961–7. https://doi.org/10.1158/0008-5472.CAN-05-1187.
Su HY, Lai HC, Lin YW, et al. Epigenetic silencing of SFRP5 is related to malignant phenotype and chemoresistance of ovarian cancer through Wnt signaling pathway. Int J Cancer. 2010;127(3):555–67. https://doi.org/10.1002/ijc.25083.
Liu J, Ji C, Wang Y, Zhang C, Zhu H. Identification of methylation-driven genes prognosis signature and immune microenvironment in uterus corpus endometrial cancer. Cancer Cell Int. 2021;21(1):365. https://doi.org/10.1186/s12935-021-02038-z.
Qiao Q, Wang Y, Zhang R, Pang Q. Autophagy related DNA methylation signature predict clinical prognosis and immune microenvironment in low-grade glioma. Transl Cancer Res. 2022;11(7): 2157–2174. https://doi.org/10.21037/tcr-22-310.
Xiao M, Liang X, Yan Z, et al. A DNA-methylation-driven genes based prognostic signature reveals immune microenvironment in pancreatic cancer. Front Immunol. 2022;13: 803962. https://doi.org/10.3389/fimmu.2022.803962.
Yang H, Bueso-Ramos C, Dinardo C, et al. Expression of PD-L1, PD-L2, PD-1 and CTLA4 in myelodysplastic syndromes is enhanced by treatment with hypomethylating agents. Leukemia. 2014;28(6):1280–8. https://doi.org/10.1038/leu.2013.355.
Dongjun P, Ilona K, Nisha N, et al. Epigenetic silencing of TH1-type chemokines shapes tumour immunity and immunotherapy. Nature. 2018;527(7577):249–53. https://doi.org/10.1038/nature15520.
Peng D, Kryczek I, Nagarsheth N, Zhao L, Wei S, Wang W, Sun Y, Zhao E, Vatan L, Szeliga W, Kotarski J, Tarkowski R, Dou Y, Cho K, Hensley-Alford S, Munkarah A, Liu R, Zou W. Epigenetic silencing of TH1-type chemokines shapes tumour immunity and immunotherapy. Nature. 2015;527(7577):249–53. https://doi.org/10.1038/nature15520.
Jung H, Kim HS, Kim JY, Sun JM, Ahn JS, Ahn MJ, Park K, Esteller M, Lee SH, Choi JK. DNA methylation loss promotes immune evasion of tumours with high mutation and copy number load. Nat Commun. 2019;10(1):4278. https://doi.org/10.1038/s41467-019-12159-9.
Schuyler RP, Merkel A, Raineri E, et al. Distinct trends of DNA methylation patterning in the innate and adaptive immune systems. Cell Rep. 2016;17(8):2101–11. https://doi.org/10.1016/j.celrep.2016.10.054.
Gomez S, Cox OL, Walker RR 3rd, et al. Inhibiting DNA methylation and RNA editing upregulates immunogenic RNA to transform the tumor microenvironment and prolong survival in ovarian cancer. J Immunother Cancer. 2022;10(11): e004974. https://doi.org/10.1136/jitc-2022-004974.
Brunckhorst MK, Xu Y, Lu R, et al. Angiopoietins promote ovarian cancer progression by establishing a procancer microenvironment. Am J Pathol. 2014;184(8):2285–96. https://doi.org/10.1016/j.ajpath.2014.05.006.
Jiang W-G, Wang H-C, et al. BDNF activates TrkB/PLCγ1 signaling pathway to promote proliferation and invasion of ovarian cancer cells through inhibition of apoptosis. Eur Rev Med Pharmacol Sci. 2019;23(12):5093–100. https://doi.org/10.26355/eurrev_201906_18173.
Abu-Elmagd M. Leptin protein expression and promoter methylation in ovarian cancer: a strong prognostic value with theranostic promises. Int J Mol Sci. 2021;22. https://doi.org/10.3390/ijms222312872.
Braga Lda C, Silva LM, Piedade JB, Traiman P, da Silva Filho AL. Epigenetic and expression analysis of TRAIL-R2 and BCL2: on the TRAIL to knowledge of apoptosis in ovarian tumors. Arch Gynecol Obstet. 2014;289(5):1061–9. https://doi.org/10.1007/s00404-013-3060-0.
Gallagher NJ, Eliopoulos AG, Agathangelo A, et al. CD40 activation in epithelial ovarian carcinoma cells modulates growth, apoptosis, and cytokine secretion. Mol Pathol. 2002;55(2):110–20. https://doi.org/10.1136/mp.55.2.110.
Yellapa A, Bitterman P, Sharma S, et al. Interleukin 16 expression changes in association with ovarian malignant transformation. Am J Obstet Gynecol. 2014;210(3):272.e1-10. https://doi.org/10.1016/j.ajog.2013.12.041.
Levina V, Nolen BM, Marrangoni AM, et al. Role of eotaxin-1 signaling in ovarian cancer. Clin Cancer Res. 2009;15(8):2647–56. https://doi.org/10.1158/1078-0432.CCR-08-2024.
Yang YI, Wang YY, Ahn JH, et al. CCL2 overexpression is associated with paclitaxel resistance in ovarian cancer cells via autocrine signaling and macrophage recruitment. Biomed Pharmacother. 2022;153: 113474. https://doi.org/10.1016/j.biopha.2022.113474.
Luetke-Eversloh M, Cicek BB, Siracusa F, et al. NK cells gain higher IFN-γ competence during terminal differentiation. Eur J Immunol. 2014;44(7):2074–84. https://doi.org/10.1002/eji.201344072.
Chan HW, Kurago ZB, Stewart CA, et al. DNA methylation maintains allele-specific KIR gene expression in human natural killer cells. J Exp Med. 2003;197(2):245–55. https://doi.org/10.1084/jem.20021127.
Huang HT, Su SC, Chiou TJ, et al. DNA methylation-mediated Siglec-7 regulation in natural killer cells via two 5’ promoter CpG sites. Immunology. 2020;160(1):38–51. https://doi.org/10.1111/imm.13179.
McDonald JI, Diab N, Arthofer E, et al. Epigenetic therapies in ovarian cancer alter repetitive element expression in a TP53-dependent manner. Cancer Res. 2021;81(20):5176–89. https://doi.org/10.1158/0008-5472.CAN-20-4243.
Quan Q, Xiong X, Wu S, Yu M. Identification of immune-related key genes in ovarian cancer based on WGCNA. Front Genet. 2021;12: 760225. https://doi.org/10.3389/fgene.2021.760225.
Zhang M, Pan X, Fujiwara K, et al. Pancreatic cancer cells render tumor-associated macrophages metabolically reprogrammed by a GARP and DNA methylation-mediated mechanism. Signal Transduct Target Ther. 2021;6(1):366. https://doi.org/10.1038/s41392-021-00769-z.
Guan Z, Luo L, Liu S, et al. The role of TGR5 as an onco-immunological biomarker in tumor staging and prognosis by encompassing the tumor microenvironment. Front Oncol. 2022;12: 953091. https://doi.org/10.3389/fonc.2022.953091.
Shi R, Zhao K, Wang T, et al. 5-aza-2’-deoxycytidine potentiates anti-tumor immunity in colorectal peritoneal metastasis by modulating ABC A9-mediated cholesterol accumulation in macrophages. Theranostics. 2022;12(2):875–90. https://doi.org/10.7150/thno.66420.
Baessler A, Novis CL, Shen Z, et al. Tet2 coordinates with Foxo1 and Runx1 to balance T follicular helper cell and T helper 1 cell differentiation. Sci Adv. 2022;8(24):eabm4982. https://doi.org/10.1126/sciadv.abm4982.
Nishizawa S, Sakata-Yanagimoto M, Hattori K, et al. BCL6 locus is hypermethylated in angioimmunoblastic T-cell lymphoma. Int J Hematol. 2017;105(4):465–9. https://doi.org/10.1007/s12185-016-2159-z.
Wei C, Liu X, Wang Q, Li Q, Xie M. Identification of hypoxia signature to assess the tumor immune microenvironment and predict prognosis in patients with ovarian cancer. Int J Endocrinol. 2021;2021:4156187. https://doi.org/10.1155/2021/4156187.
Sun D, Zhao X, Yu Y, et al. Comprehensive characterization of the alternative splicing landscape in ovarian cancer reveals novel events associated with tumor-immune microenvironment. Biosci Rep. 2022;42(2):BSR20212090. https://doi.org/10.1042/BSR20212090.
Pawłowska A, Kwiatkowska A, Suszczyk D, et al. Clinical and prognostic value of antigen-presenting cells with PD-L1/PD-L2 expression in ovarian cancer patients. Int J Mol Sci. 2021;22(21):11563. https://doi.org/10.3390/ijms222111563.
de Vos L, Grünwald I, Bawden EG, et al. The landscape of CD28, CD80, CD86, CTLA4, and ICOS DNA methylation in head and neck squamous cell carcinomas. Epigenetics. 2020;15(11):1195–212. https://doi.org/10.1080/15592294.2020.1754675.
de Vos L, Carrillo Cano TM, et al. CTLA4, PD-1, PD-L1, PD-L2, TIM-3, TIGIT, and LAG3 DNA methylation is associated with BAP1-aberrancy, transcriptional activity, and overall survival in uveal melanoma. J Immunother. 2022;45(7):324–34. https://doi.org/10.1097/CJI.0000000000000429.
Kushlinskii NE, Loginov VI, Utkin DO, et al. Novel miRNAs as potential regulators of PD-1/PD-L1 immune checkpoint, and prognostic value of MIR9–1 and MIR124–2 methylation in ovarian cancer. Mol Biol (Mosk). 2020;54(6):990–6. https://doi.org/10.31857/S0026898420060075.
Hu WL, Zhou XH. Identification of prognostic signature in cancer based on DNA methylation interaction network. BMC Med Genomics. 2017;10(Suppl 4):63. https://doi.org/10.1186/s12920-017-0307-9.
Daniela, Matei, Fang, et al. Epigenetic resensitization to platinum in ovarian cancer. Cancer Res. 2012. https://doi.org/10.1158/0008-5472.CAN-11-3909.
Barton GM, Kagan JC. A cell biological view of Toll-like receptor function: regulation through compartmentalization. Nature Rev Immunol. 2009;9(8):535–42. https://doi.org/10.1038/nri2587.
Rakoff-Nahoum S, Medzhitov R. Toll-like receptors and cancer. Nature Rev Cancer. 2009;9(1):57–63.
Gata V, Florin LI. The role of Toll-like receptors in ovarian cancer. J BUON. 2017;22(5):1092–6.
Hu J, Xu J, Feng X, Li Y, Hua F, Xu G. Differential expression of the TLR4 gene in pan-cancer and its related mechanism. Front Cell Dev Biol. 2021;9: 700661. https://doi.org/10.3389/fcell.2021.700661.
Lino AC, Dang VD, Lampropoulou V, et al. LAG-3 inhibitory receptor expression identifies immunosuppressive natural regulatory plasma cells. Immunity. 2018;49(1):120-133.e9. https://doi.org/10.1016/j.immuni.2018.06.007.
Liu L, Liu B, Yu J, Zhang D, Shi J, Liang P. Development of a Toll-like receptor-based gene signature that can predict prognosis, tumor microenvironment, and chemotherapy response for hepatocellular carcinoma. Front Mol Biosci. 2021;8: 729789. https://doi.org/10.3389/fmolb.2021.729789.
Carmo CR, Lyons-Lewis J, Seckl MJ, et al. A novel requirement for Janus kinases as mediators of drug resistance induced by fibroblast growth factor-2 in human cancer cells. PLoS ONE. 2011;6(5): e19861. https://doi.org/10.1371/journal.pone.0019861.
Hernandez-Vargas H, Ouzounova M, Le Calvez-Kelm F, et al. Methylome analysis reveals Jak-STAT pathway deregulation in putative breast cancer stem cells. Epigenetics. 2011;6(4):428–39. https://doi.org/10.4161/epi.6.4.14515.
Shang AQ, Wu J, Bi F, et al. Relationship between HER2 and JAK/STAT-SOCS3 signaling pathway and clinicopathological features and prognosis of ovarian cancer. Cancer Biol Ther. 2017;18(5):314–22. https://doi.org/10.1080/15384047.2017.1310343.
Mansouri A, Ridgway LD, Korapati AL, et al. Sustained activation of JNK/p38 MAPK pathways in response to Cisplatin leads to Fas ligand induction and cell death in ovarian carcinoma cells. J Biol Chem. 2003;278(21):19245–56. https://doi.org/10.1074/jbc.M208134200.
Chen K, Liu MX, Mak CS, Yung MM, Leung TH, Xu D, Ngu SF, Chan KK, Yang H, Ngan HY, Chan DW. Methylation-associated silencing of miR-193a-3p promotes ovarian cancer aggressiveness by targeting GRB7 and MAPK/ERK pathways. Theranostics. 2018;8(2):423–36. https://doi.org/10.7150/thno.22377.
Li KP, Ladle BH, Kurtulus S, et al. T-cell receptor signal strength and epigenetic control of Bim predict memory CD8+ T-cell fate. Cell Death Differ. 2020;27(4):1214–24. https://doi.org/10.1038/s41418-019-0410-x.
Li C, Ebert PJ, Li QJ. T cell receptor (TCR) and transforming growth factor β (TGF-β) signaling converge on DNA (cytosine-5)-methyltransferase to control forkhead box protein 3 (foxp3) locus methylation and inducible regulatory T cell differentiation. J Biol Chem. 2013;288(26):19127–39. https://doi.org/10.1074/jbc.M113.453357.
Pan X, Chen Y, Gao S. Four genes relevant to pathological grade and prognosis in ovarian cancer. Cancer Biomark. 2020;29(2):169–78. https://doi.org/10.3233/CBM-191162.
Graudenzi A. Pathway-based classification of breast cancer subtypes. Front Bioscience. 2017;22(10):1697. https://doi.org/10.2741/4566.
White KL, Rider DN, Kalli KR, et al. Genomics of the NF-κB signaling pathway: hypothesized role in ovarian cancer. Cancer Causes Control. 2011;22(5):785–801. https://doi.org/10.1007/s10552-011-9745-4.
Li X, Bao C, Ma Z, Xu B, Ying X, Liu X, Zhang X. Perfluorooctanoic acid stimulates ovarian cancer cell migration, invasion via ERK/NF-κB/MMP-2/-9 pathway. Toxicol Lett. 2018;15(294):44–50. https://doi.org/10.1016/j.toxlet.2018.05.009.
Gallagher NJ, Eliopoulos AG, Agathangelo A, Oates J, Crocker J, Young LS. CD40 activation in epithelial ovarian carcinoma cells modulates growth, apoptosis, and cytokine secretion. Mol Pathol. 2002;55(2):110–20. https://doi.org/10.1136/mp.55.2.110.
Rothenburger T, McLaughlin KM, Herold T, et al. SAMHD1 is a key regulator of the lineage-specific response of acute lymphoblastic leukaemias to nelarabine. Commun Biol. 2020;3(1):324. https://doi.org/10.1038/s42003-020-1052-8.
Teschendorff AE, Lee SH, Jones A, et al. HOTAIR and its surrogate DNA methylation signature indicate carboplatin resistance in ovarian cancer. Genome Med. 2015;7:108. https://doi.org/10.1186/s13073-015-0233-4.
Akahane K, Kimura S, Miyake K, et al. Association of allele-specific methylation of the ASNS gene with asparaginase sensitivity and prognosis in T-ALL. Blood Adv. 2022;6(1):212–24. https://doi.org/10.1182/bloodadvances.
Rodríguez D, Quirós LM, Salas JA. MtmMII-mediated C-methylation during biosynthesis of the antitumor drug mithramycin is essential for biological activity and DNA-drug interaction. J Biol Chem. 2004;279(9):8149–58. https://doi.org/10.1074/jbc.M312351200.
Evison BJ, Bilardi RA, Chiu FC, Pezzoni G, Phillips DR, Cutts SM. CpG methylation potentiates pixantrone and doxorubicin-induced DNA damage and is a marker of drug sensitivity. Nucleic Acids Res. 2009;37(19):6355–70. https://doi.org/10.1093/nar/gkp700.
Liu S, Liu Z, Xie Z, et al. Bortezomib induces DNA hypomethylation and silenced gene transcription by interfering with Sp1/NF-kappaB-dependent DNA methyltransferase activity in acute myeloid leukemia. Blood. 2008;111(4):2364–73. https://doi.org/10.1182/blood-2007-08-110171.
Nakshatri H, Appaiah HN, Anjanappa M, et al. NF-κB-dependent and -independent epigenetic modulation using the novel anti-cancer agent DMAPT. Cell Death Dis. 2015;6(1): e1608. https://doi.org/10.1038/cddis.2014.569.
Hu Y, Zheng M, Wang S, et al. Identification of a five-gene signature of the RGS gene family with prognostic value in ovarian cancer. Genomics. 2021;113(4):2134–44. https://doi.org/10.1016/j.ygeno.2021.04.012.
Yu M, Henning R, Walker A, et al. L-asparaginase inhibits invasive and angiogenic activity and induces autophagy in ovarian cancer. J Cell Mol Med. 2012;16(10):2369–78. https://doi.org/10.1111/j.1582-4934.2012.01547.x.
Chan DW, Lam WY, Chen F, et al. Genome-wide DNA methylome analysis identifies methylation signatures associated with survival and drug resistance of ovarian cancers. Clin Epigenetics. 2021;13(1):142. https://doi.org/10.1186/s13148-021-01130-5.
Boyd LR, Muggia FM. Carboplatin/paclitaxel induction in ovarian cancer: the finer points. Oncology (Williston Park). 2018;32(8):418–20, 422–4.
Wang L, Yan W, Li X, et al. S100A10 silencing suppresses proliferation, migration and invasion of ovarian cancer cells and enhances sensitivity to carboplatin. J Ovarian Res. 2019;12(1):113. https://doi.org/10.1186/s13048-019-0592-3.
Deng M, Sun J, Xie S, Zhen H, et al. Inhibition of MCM2 enhances the sensitivity of ovarian cancer cell to carboplatin. Mol Med Rep. 2019;20(3):2258–66. https://doi.org/10.3892/mmr.2019.10477.
Zhang J, Zhang J, Wang F, et al. Overexpressed COL5A1 is correlated with tumor progression, paclitaxel resistance, and tumor-infiltrating immune cells in ovarian cancer. J Cell Physiol. 2021;236(10):6907–19. https://doi.org/10.1002/jcp.30350.
Lin H, Shen L, Lin Q, et al. SNHG5 enhances paclitaxel sensitivity of ovarian cancer cells through sponging miR-23a. Biomed Pharmacother. 2020;123: 109711. https://doi.org/10.1016/j.biopha.2019.109711.
Leija-Martínez JJ, Giacoman-Martínez A, Del-Río-Navarro BE, Sanchéz-Muñoz F, Hernández-Diazcouder A, Muñoz-Hernández O, Romero-Nava R, Villafaña S, Marchat LA, Hong E, Huang F. Promoter methylation status of RORC, IL17A, and TNFA in peripheral blood leukocytes in adolescents with obesity-related asthma. Heliyon. 2022;8(12): e12316. https://doi.org/10.1016/j.heliyon.
Gong G, Lin T, Yuan Y. Integrated analysis of gene expression and DNA methylation profiles in ovarian cancer. J Ovarian Res. 2020;13(1):30. https://doi.org/10.1186/s13048-020-00632-9.
Nimmo ER, Prendergast JG, Aldhous MC, Kennedy NA, Henderson P, Drummond HE, Ramsahoye BH, Wilson DC, Semple CA, Satsangi J. Genome-wide methylation profiling in Crohn’s disease identifies altered epigenetic regulation of key host defense mechanisms including the Th17 pathway. Inflamm Bowel Dis. 2012;18(5):889–99. https://doi.org/10.1002/ibd.21912.
Li T, Xu Y, Shi Y, Chen J, Lin S, Zhu J, Xu X, Lu L, Zou H. Genome-wide analysis of DNA methylation identifies S100A13 as an epigenetic biomarker in individuals with chronic (≥ 30 years) type 2 diabetes without diabetic retinopathy. Clin Epigenetics. 2020;12(1):77. https://doi.org/10.1186/s13148-020-00871-z.
Gérard Benoit, Cooney A, Giguere V, et al. International union of pharmacology. LXVI. Orphan nuclear receptors. Pharmacol Rev. 2007;58(4):798–836. https://doi.org/10.1124/pr.58.4.10.
Muscat GEO, Eriksson NA, Karen B, et al. Research resource: nuclear receptors as transcriptome: discriminant and prognostic value in breast cancer. Mol Endocrinol. 2013;27(2). https://doi.org/10.1210/me.2012-1265.
Dalong, Zihao, Pang, et al. Retinoic acid-related orphan receptor C regulates proliferation, glycolysis, and chemoresistance via the PD-L1/ITGB6/STAT3 signaling axis in bladder cancer. Cancer Res. 2019;79(10): 2604–2618. https://doi.org/10.1158/0008-5472.CAN-18-3842.
Li R, Li W, He F, et al. Systematic screening identifies a TEAD4-S100A13 axis modulating cisplatin sensitivity of oral squamous cell carcinoma cells. J Oral Pathol Med. 2021;50(9):882–90. https://doi.org/10.1111/jop.13224.
Miao S, Qiu T, Zhao Y, et al. Overexpression of S100A13 protein is associated with tumor angiogenesis and poor survival in patients with early-stage non-small cell lung cancer. Thoracic Cancer. 2018;9(9):1136–44. https://doi.org/10.1111/1759-7714.12797.
Gong K, Guo G, Beckley N, et al. Tumor necrosis factor in lung cancer: complex roles in biology and resistance to treatment. Neoplasia. 2021;23(2):189–96. https://doi.org/10.1016/j.neo.2020.12.006.
Misaki F, Yasuhiro M, Kiyoshi T, et al. Relaxin 2/RXFP1 signaling induces cell invasion via the β-catenin pathway in endometrial cancer. Int J Mol Sci. 2018;19(8):2438. https://doi.org/10.3390/ijms19082438.
Chen YC, Gonzalez ME, Burman B, et al. Mesenchymal stem/stromal cell engulfment reveals metastatic advantage in breast cancer. Cell Rep. 2019;27(13):3916–26. https://doi.org/10.1016/j.celrep.2019.05.084.
Wen S, He L, Zhong Z, et al. Prognostic model of colorectal cancer constructed by eight immune-related genes. Front Mol Biosci. 2020;27(7): 604252. https://doi.org/10.3389/fmolb.2020.604252.
Bukhari SA, Zafar K, Rajoka M, İbrahim Z, Javed S, Sadiq R. Oxidative stress-induced DNA damage and homocysteine accumulation may beinvolved in ovarian cancer progression in both young and old patients. Turk J Med Sci. 2016;46(3):583–9. https://doi.org/10.3906/sag-1406-17.
Mazurakova A, Samec M, Biringer K, et al. Homocysteine metabolism as the target for predictive medical approach, disease prevention, prognosis, and treatments tailored to the person. EPMA J. 2021;12(4):477–505. https://doi.org/10.1007/s13167-021-00263-0.
Endicott JL, Nolte PA, Shen H, Laird PW. Cell division drives DNA methylation loss in late-replicating domains in primary human cells. Nat Commun. 2022;13(1):6659. 150. https://doi.org/10.1038/s41467-022-34268-8.
Guo H, Vuille JA, Wittner BS, et al. DNA hypomethylation silences anti-tumor immune genes in early prostate cancer and CTCs. Cell. 2023;186(13):2765-2782.e28. https://doi.org/10.1016/j.cell.2023.05.028.
Li Y, Xu J, Chen C, et al. Multimodal epigenetic sequencing analysis (MESA) of cell-free DNA for non-invasive colorectal cancer detection. Genome Med. 2024;16(1):9. https://doi.org/10.1186/s13073-023-01280-6.
Buckley DN, Lewinger JP, Gooden G, et al. OvaPrint-a cell-free DNA methylation liquid biopsy for the risk assessment of high-grade serous ovarian cancer. Clin Cancer Res. 2023;29(24):5196–206. https://doi.org/10.1158/1078-0432.ccr-23-1197.
Büttner T, Dietrich D, Zarbl R, et al. Feasibility of monitoring response to metastatic prostate cancer treatment with a methylation-based circulating tumor DNA approach. Cancers (Basel). 2024;16(3):482. https://doi.org/10.3390/cancers16030482.
Hussan SS, Ali MS, Fatima M, Altaf M, Sadaf S. Epigenetically dysregulated NOTCH-Delta-HES signaling cascade can serve as a subtype classifier for acute lymphoblastic leukemia. Ann Hematol. 2024;103(2):511–23. https://doi.org/10.1007/s00277-023-05515-9.
Fietz S, Diekmann E, de Vos L, et al. Circulating cell-free SHOX2 DNA methylation is a predictive, prognostic, and monitoring biomarker in adjuvant and palliative anti-PD-1-treated melanoma. Clin Chem. 2024:hvad230. 144. https://doi.org/10.1093/clinchem/hvad230.
Bixby B, Vrba L, Lenka J, et al. Cell-free DNA methylation analysis as a marker of malignancy in pleural fluid. Sci Rep. 2024;14(1):2939.145. https://doi.org/10.1038/s41598-024-53132-x.
Mo S, Ye L, Wang D, et al. Early detection of molecular residual disease and risk stratification for stage I to III colorectal cancer via circulating tumor DNA methylation. JAMA Oncol. 2023;9(6):770–778.147. https://doi.org/10.1001/jamaoncol.2023.0425.
Herzog C, Jones A, Evans I, et al. Plasma cell-free DNA methylation analysis for ovarian cancer detection: analysis of samples from a case-control study and an ovarian cancer screening trial. Int J Cancer. 2024;154(4):679–91. https://doi.org/10.1002/ijc.34757.
Bian S, Hou Y, Zhou X, et al. Single-cell multiomics sequencing and analyses of human colorectal cancer. Science. 2018;362(6418):1060–3. https://doi.org/10.1126/science.aao3791.
Lee SC, Adams DW, Ipsaro JJ, et al. Chromatin remodeling of histone H3 variants by DDM1 underlies epigenetic inheritance of DNA methylation. Cell. 2023;186(19):4100-4116.e15. https://doi.org/10.1016/j.cell.2023.08.001.
Yahsi B, Palaz F, Dincer P. Applications of CRISPR epigenome editors in tumor immunology and autoimmunity. ACS Synth Biol. 2024;13(2):413–27. https://doi.org/10.1021/acssynbio.3c00524.
Barton CA, Hacker NF, Clark SJ, O’Brien PM. DNA methylation changes in ovarian cancer: implications for early diagnosis, prognosis and treatment. Gynecol Oncol. 2008;109(1):129–39. https://doi.org/10.1016/j.ygyno.2007.12.017.
Grech G, Zhan X, Yoo BC, Bubnov R, Hagan S, Danesi R, Vittadini G, Desiderio DM. EPMA position paper in cancer: current overview and future perspectives. EPMA J. 2015;6(1):9. https://doi.org/10.1186/s13167-015-0030-6.
Chiappinelli KB, Strissel PL, Desrichard A, Li H, Henke C, Akman B, Hein A, et al. Inhibiting DNA methylation causes an interferon response in cancer via dsRNA including endogenous retroviruses. Cell. 2015;162(5):974–86. https://doi.org/10.1016/j.cell.2015.07.011.
Hou X, Liao Q, Wu Y, Wang L, Zhao J, Liao X. Hypomethylation-mediated upregulation of NFE2L3 promotes malignant phenotypes of clear cell renal cell carcinoma cells. Mol Biotechnol. 2024;66(2):198–207. https://doi.org/10.1007/s12033-023-00727-w.
Mazurakova A, Samec M, Koklesova L, Biringer K, Kudela E, Al-Ishaq RK, Pec M, Giordano FA, Büsselberg D, Kubatka P, Golubnitschaja O. Anti-prostate cancer protection and therapy in the framework of predictive, preventive and personalised medicine - comprehensive effects of phytochemicals in primary, secondary and tertiary care. EPMA J. 2022;13(3):461–86. https://doi.org/10.1007/s13167-022-00288-z.
Acknowledgements
The authors acknowledge The Cancer Genome Atlas (TCGA) project organizers as well as all study participants to provide the publicly available TCGA RNA-seq data and clinical data.
Funding
This work was supported by the Shandong Provincial Taishan Scholar Engineering Project Special Funds (to X.Z.), the Shandong Provincial Natural Science Foundation (ZR2021MH156; ZR2022QH112; ZR2020LZL012), the Shandong First Medical University Talent Introduction Funds (to X.Z.), the Shandong First Medical University High-level Scientific Research Achievement Cultivation Funding Program (to X.Z.), the China National Nature Scientific Funds (82203592), the CSCO-CSPC Cancer Research Fund Project (Y-SY2021QN-0152), the Clinical Research Fund Project of Shandong Medical Association (YXH2022ZX02149), and the Beijing Science and Technology Innovation Medical Development Foundation (No. KC2021-JX-0186–138).
Author information
Authors and Affiliations
Contributions
W.J. analyzed partial data, performed methylation experiments, and wrote the manuscript draft. N.L. conceived the concept, analyzed data, and wrote the manuscript. J.W., X.G., Y.W., and J.Z. analyzed partial data. S.Y.O and G.G. reviewed and critically revised the manuscript. L.C. supervised the data and edited the manuscript. X.Z. conceived the concept, coordinated and critically revised the manuscript, and was responsible for the corresponding works. All authors approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval
All investigations conformed to the principles outlined in the Declaration of Helsinki, and the research protocol was approved by the Medical Ethics Committee of Shandong First Medical University, China. All the patients were informed about the purposes of the study and consequently have signed their “consent of the patient.”. It includes the following four aspects:
- Approval of the research protocol by an Institutional Reviewer Board: Yes.
- Informed Consent: Yes.
- Registry and the Registration No. of the study: 202105200158.
- Animal Studies: N/A.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jia, W., Li, N., Wang, J. et al. Immune-related gene methylation prognostic instrument for stratification and targeted treatment of ovarian cancer patients toward advanced 3PM approach. EPMA Journal (2024). https://doi.org/10.1007/s13167-024-00359-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13167-024-00359-3