Abstract
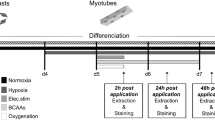
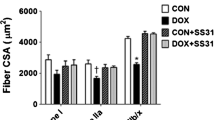
Hypobaric hypoxia (HH) leads to various adverse effects on skeletal muscles, including atrophy and reduced oxidative work capacity. However, the effects of HH on muscle fatigue resistance and myofiber remodeling are largely unexplored. Therefore, the present study aimed to explore the impact of HH on slow-oxidative fibers and to evaluate the ameliorative potential of exercise preconditioning and nanocurcumin formulation on muscle anti-fatigue ability. C2C12 cells (murine myoblasts) were used to assess the effect of hypoxia (0.5%, 24 h) with and without the nanocurcumin formulation (NCF) on myofiber phenotypic conversion. To further validate this hypothesis, male Sprague Dawley rats were exposed to a simulated HH (7620 m) for 7 days, along with NCF administration and/or exercise training. Both in vitro and in vivo studies revealed a significant reduction in slow-oxidative fibers (p < 0.01, 61% vs. normoxia control) under hypoxia. There was also a marked decrease in exhaustion time (p < 0.01, 65% vs. normoxia) in hypoxia control rats, indicating a reduced work capacity. Exercise preconditioning along with NCF supplementation significantly increased the slow-oxidative fiber proportion and exhaustion time while maintaining mitochondrial homeostasis. These findings suggest that HH leads to an increased transition of slow-oxidative fibers to fast glycolytic fibers and increased muscular fatigue. Administration of NCF in combination with exercise preconditioning restored this myofiber remodeling and improved muscle anti-fatigue ability.










Similar content being viewed by others
Data Availability
N/A
References
Abdelmalki A, Fimbel S, Mayet-Sornay MH et al (1996) Aerobic capacity and skeletal muscle properties of normoxic and hypoxic rats in response to training. Pflugers Arch 431(5):671–679
Agrawal A, Rathore R, Kumar R et al (2018) Role of altered proteostasis network in chronic hypobaric hypoxia induced skeletal muscle atrophy. PLoS ONE 13(9):e0204283
Agrawal A, Rathore R, Kumar R et al (2020) Redox modification of ryanodine receptor contributes to impaired Ca(2+) homeostasis and exacerbates muscle atrophy under high altitude. Free Radic Biol Med 160:643–656
Al-Dashti YA, Holt RR, Stebbins CL et al (2018) Dietary flavanols: a review of select effects on vascular function, blood pressure, and exercise performance. J Am Coll Nutr 37(7):553–567
Avci G, Kadioglu H, Sehirli AO et al (2012) Curcumin protects against ischemia/reperfusion injury in rat skeletal muscle. J Surg Res 172(1):e39-46
Bassel-Duby R, Olson EN (2006) Signaling pathways in skeletal muscle remodeling. Annu Rev Biochem 75:19–37
Bo H, Wang YH, Li HY et al (2008) Endurance training attenuates the bioenergetics alterations of rat skeletal muscle mitochondria submitted to acute hypoxia: role of ROS and UCP3. Sheng Li Xue Bao 60(6):767–776
Booth FW, Ruegsegger GN, Toedebusch RG et al (2015) Endurance exercise and the regulation of skeletal muscle metabolism. Prog Mol Biol Transl Sci 135:129–151
Bottinelli R, Reggiani C (2000) Human skeletal muscle fibers: molecular and functional diversity. Prog Biophys Mol Biol 73(2–4):195–262
Bradwell AR, Dykes PW, Coote JH et al (1986) Effect of acetazolamide on exercise performance and muscle mass at high altitude. Lancet 1(8488):1001–1005
Canto C, Gerhart-Hines Z, Feige JN et al (2009) AMPK regulates energy expenditure by modulating NAD+ metabolism and SIRT1 activity. Nature 458(7241):1056–1060
Chaillou T (2018) Skeletal muscle fiber type in hypoxia: adaptation to high-altitude exposure and under conditions of pathological hypoxia. Front Physiol 9:1450
Chaillou T, Koulmann N, Meunier A et al (2014) Effect of hypoxia exposure on the recovery of skeletal muscle phenotype during regeneration. Mol Cell Biochem 390(1–2):31–40
Chalkiadaki A, Igarashi M, Nasamu AS et al (2014) Muscle-specific SIRT1 gain-of-function increases slow-twitch fibers and ameliorates pathophysiology in a mouse model of Duchenne muscular dystrophy. PLoS Genet 10(7):e1004490
Chaudhary P, Suryakumar G, Prasad R et al (2012) Chronic hypobaric hypoxia-mediated skeletal muscle atrophy: role of ubiquitin-proteasome pathway and calpains. Mol Cell Biochem 364(1–2):101–113
Chaudhary P, Suryakumar G, Sharma YK et al (2012) Differential response of the gastrocnemius and soleus muscles of rats to chronic hypobaric hypoxia. Aviat Space Environ Med 83(11):1037–1043
Chen X, Liang D, Huang Z et al (2021) Quercetin regulates skeletal muscle fiber type switching via adiponectin signaling. Food Funct 12(6):2693–2702
Chen X, Zhang M, Xue Y et al (2022) Effect of dietary L-theanine supplementation on skeletal muscle fiber type transformation in vivo. J Nutr Biochem 99:108859
Chicco AJ, Le CH, Gnaiger E et al (2018) Adaptive remodeling of skeletal muscle energy metabolism in high-altitude hypoxia: lessons from AltitudeOmics. J Biol Chem 293(18):6659–6671
Chitra L, Boopathy R (2013) Adaptability to hypobaric hypoxia is facilitated through mitochondrial bioenergetics: an in vivo study. Br J Pharmacol 169(5):1035–1047
Dei Cas M, Ghidoni R (2019) Dietary curcumin: correlation between bioavailability and health potential. Nutrients 11(9):2147
Edwards LM, Murray AJ, Tyler DJ et al (2010) The effect of high-altitude on human skeletal muscle energetics: P-MRS results from the Caudwell Xtreme Everest expedition. PLoS ONE 5(5):e10681
Flora G, Gupta D, Tiwari A (2013) Nanocurcumin: a promising therapeutic advancement over native curcumin. Crit Rev Ther Drug Carrier Syst 30(4):331–368
Hirabayashi T, Nakanishi R, Tanaka M et al (2021) Reduced metabolic capacity in fast and slow skeletal muscle via oxidative stress and the energy-sensing of AMPK/SIRT1 in malnutrition. Physiol Rep 9(5):e14763
Hoppeler H, Klossner S, Vogt M (2008) Training in hypoxia and its effects on skeletal muscle tissue. Scand J Med Sci Sports 18(Suppl 1):38–49
Hoppeler H, Vogt M (2001) Muscle tissue adaptations to hypoxia. J Exp Biol 204(Pt 18):3133–3139
Hoppeler H, Vogt M, Weibel ER et al (2003) Response of skeletal muscle mitochondria to hypoxia. Exp Physiol 88(1):109–119
Howald H, Hoppeler H (2003) Performing at extreme altitude: muscle cellular and subcellular adaptations. Eur J Appl Physiol 90(3–4):360–364
Hwang PS, Machek SB, Cardaci TD et al (2020) Effects of pyrroloquinoline quinone (PQQ) supplementation on aerobic exercise performance and indices of mitochondrial biogenesis in untrained men. J Am Coll Nutr 39(6):547–556
Itoh K, Moritani T, Ishida K et al (1990) Hypoxia-induced fiber type transformation in rat hindlimb muscles. Histochemical and electromechanical changes. Eur J Appl Physiol Occup Physiol 60(5):331–336
Jacobs RA, Boushel R, Wright-Paradis C et al (2013) Mitochondrial function in human skeletal muscle following high-altitude exposure. Exp Physiol 98(1):245–255
Jezek P, Holendova B, Plecita-Hlavata L (2020) Redox signaling from mitochondria: signal propagation and its targets. Biomolecules 10(1):93
Kushwaha AD, Saraswat D (2022) A nanocurcumin and pyrroloquinoline quinone formulation prevent hypobaric hypoxia-induced skeletal muscle atrophy by modulating NF-kappaB signaling pathway. High Alt Med Biol 2022(3):249–263
Liang D, Zhuo Y, Guo Z et al (2020) SIRT1/PGC-1 pathway activation triggers autophagy/mitophagy and attenuates oxidative damage in intestinal epithelial cells. Biochimie 170:10–20
Liu W, Zhai Y, Heng X et al (2016) Oral bioavailability of curcumin: problems and advancements. J Drug Target 24(8):694–702
Ma W, Zhang R, Huang Z et al (2019) PQQ ameliorates skeletal muscle atrophy, mitophagy, and fiber type transition induced by denervation via inhibition of the inflammatory signaling pathways. Ann Transl Med 7(18):440
MacDougall JD, Green HJ, Sutton JR et al (1991) Operation Everest II: structural adaptations in skeletal muscle in response to extreme simulated altitude. Acta Physiol Scand 142(3):421–427
Magalhaes J, Ascensao A, Soares JM et al (2005) Acute and severe hypobaric hypoxia increases oxidative stress and impairs mitochondrial function in mouse skeletal muscle. J Appl Physiol (1985) 99(4):1247–53
Mannino MH, Patel RS, Eccardt AM et al (2019) Myoglobin as a versatile peroxidase: Implications for a more important role for vertebrate striated muscle in antioxidant defense. Comp Biochem Physiol B Biochem Mol Biol 234:9–17
Medeiros DM (2008) Assessing mitochondria biogenesis. Methods 46(4):288–294
Mesquita PHC, Vann CG, Phillips SM et al (2021) Skeletal muscle ribosome and mitochondrial biogenesis in response to different exercise training modalities. Front Physiol 12:725866
Miura S, Kai Y, Ono M et al (2003) Overexpression of peroxisome proliferator-activated receptor gamma coactivator-1alpha downregulates GLUT4 mRNA in skeletal muscles. J Biol Chem 278(33):31385–31390
Murray AJ (2009) Metabolic adaptation of skeletal muscle to high altitude hypoxia: how new technologies could resolve the controversies. Genome Med 1(12):117
Nehra S, Bhardwaj V, Bansal A et al (2017) Combinatorial therapy of exercise-preconditioning and nanocurcumin formulation supplementation improves cardiac adaptation under hypobaric hypoxia. J Basic Clin Physiol Pharmacol 28(5):443–453
Nehra S, Bhardwaj V, Ganju L et al (2015) Nanocurcumin prevents hypoxia-induced stress in primary human ventricular cardiomyocytes by maintaining mitochondrial homeostasis. PLoS ONE 10(9):e0139121
Nioka S, Moser D, Lech G et al (1998) Muscle deoxygenation in aerobic and anaerobic exercise. Adv Exp Med Biol 454:63–70
Pette D, Staron RS (1997) Mammalian skeletal muscle fiber type transitions. Int Rev Cytol 170:143–223
Pette D, Staron RS (2001) Transitions of muscle fiber phenotypic profiles. Histochem Cell Biol 115(5):359–372
Pilegaard H, Saltin B, Neufer PD (2003) Exercise induces transient transcriptional activation of the PGC-1alpha gene in human skeletal muscle. J Physiol 546(Pt 3):851–858
Rahar B, Chawla S, Tulswani R et al (2019) Acute hypobaric hypoxia-mediated biochemical/metabolic shuffling and differential modulation of S1PR-SphK in cardiac and skeletal muscles. High Alt Med Biol 20(1):78–88
Rathor R, Suryakumar G, Singh SN (2021) Diet and redox state in maintaining skeletal muscle health and performance at high altitude. Free Radic Biol Med 174:305–320
Schiaffino S, Reggiani C (2011) Fiber types in mammalian skeletal muscles. Physiol Rev 91(4):1447–1531
Shome S, Talukdar AD, Choudhury MD et al (2016) Curcumin as a potential therapeutic natural product: a nanobiotechnological perspective. J Pharm Pharmacol 68(12):1481–1500
Spinazzi M, Casarin A, Pertegato V et al (2012) Assessment of mitochondrial respiratory chain enzymatic activities on tissues and cultured cells. Nat Protoc 7(6):1235–1246
Sumi D, Kojima C, Goto K (2018) Impact of endurance exercise in hypoxia on muscle damage, inflammatory, and performance responses. J Strength Cond Res 32(4):1053–1062
Tanaka M, Mizuta K, Koba F et al (1997) Effects of exposure to hypobaric-hypoxia on body weight, muscular and hematological characteristics, and work performance in rats. Jpn J Physiol 47(1):51–57
Wehrlin JP, Hallen J (2006) Linear decrease in VO2 max and performance with increasing altitude in endurance athletes. Eur J Appl Physiol 96(4):404–412
Wen W, Chen X, Huang Z et al (2021) Lycopene increases the proportion of slow-twitch muscle fiber by AMPK signaling to improve muscle anti-fatigue ability. J Nutr Biochem 94:108750
West JB (1990) Limiting factors for exercise at extreme altitudes. Clin Physiol 10(3):265–272
Yadav A, Yadav SS, Singh S et al (2022) Natural products: potential therapeutic agents to prevent skeletal muscle atrophy. Eur J Pharmacol 925:174995
Yeung YG, Stanley ER (2009) A solution for stripping antibodies from polyvinylidene fluoride immunoblots for multiple reprobing. Anal Biochem 389(1):89–91
Ying F, Zhang L, Bu G et al (2016) Muscle fiber-type conversion in the transgenic pigs with overexpression of PGC1alpha gene in muscle. Biochem Biophys Res Commun 480(4):669–674
Yu T, Dohl J, Park YM et al (2022) Protective effects of dietary curcumin and astaxanthin against heat-induced ROS production and skeletal muscle injury in male and female C57BL/6J mice. Life Sci 288:120160
Zmijewski JW, Banerjee S, Bae H et al (2010) Exposure to hydrogen peroxide induces oxidation and activation of AMP-activated protein kinase. J Biol Chem 285(43):33154–33164
Zou D, Chen K, Liu P et al (2014) Dihydromyricetin improves physical performance under simulated high altitude. Med Sci Sports Exerc 46(11):2077–2084
Funding
The authors sincerely thank the Director of the Defense Institute of Physiology and Allied Science for providing the necessary resources for conducting the present study. One of the authors, Ms. Asha D Kushwaha, is thankful for obtaining a research fellowship from DRDO.
Author information
Authors and Affiliations
Contributions
All authors participated in the conceptualization and design of the study. ADK experimented and analyzed the data. ADK wrote the manuscript. RV helped during planning and conceptualization of this work. DS has read and approved the final manuscript. The authors declare that all data were generated in-house and that no paper mill was used.
Corresponding author
Ethics declarations
Ethics approval
The Institutional Animal Ethical Committee (IAEC) approved the present research work on animal experiments with reference no. DIPAS/IAEC/2018/10–02, and the experiments were performed following the regulations specified by the IAEC and conformed to the National Guidelines on the Care and Use of Laboratory Animals, India.
Consent for publication
All the authors have read and approved this manuscript and consent for submission.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
1. Hypobaric hypoxia augments the transition of myofibers from slow (oxidative fatigue-resistant) to fast (glycolytic fatigue-susceptible), resulting in a decreased oxidative work capacity.
2. Combinatorial therapy of exercise preconditioning with nanocurcumin formulation (NCF) prevents myofiber transition and thus improves exercise time to exhaustion.
3. NCF administration along with exercise preconditioning also maintains mitochondrial and metabolic homeostasis through PGC1α/SIRT1/AMPK signaling under hypobaric hypoxia condition.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kushwaha, A.D., Varshney, R. & Saraswat, D. Effect of hypobaric hypoxia on the fiber type transition of skeletal muscle: a synergistic therapy of exercise preconditioning with a nanocurcumin formulation. J Physiol Biochem 79, 635–652 (2023). https://doi.org/10.1007/s13105-023-00965-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13105-023-00965-1