Abstract
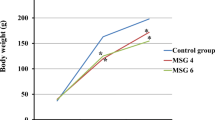
The purpose of this study was to determine whether magnesium L-lactate is responsible for having a beneficial effect on the myocardium and the skeletal muscles and how this substrate acts at the molecular level. Twenty seven young male Wistar rats were supplied with a magnesium L-lactate (L) solution, a magnesium chloride (M) solution and/or water (W) as a vehicle for 10 weeks. The treated animals absorbed the L and M solutions as they wished since they also had free access to water. After 9 weeks of treatment, in vivo cardiac function was determined ultrasonically. The animals were sacrificed at the end of the tenth week of treatment and the heart was perfused according to the Langendorff method by using a technique allowing the determination of cardiomyocyte activity (same coronary flow in the two groups). Blood was collected and skeletal muscles of the hind legs were weighed. The myocardial expressions of the sodium/proton exchange 1 (NHE1) and sodium/calcium exchange 1 (NCX1), intracellular calcium accumulation, myocardial magnesium content, as well as systemic and tissue oxidative stress, were determined. Animals of the L group absorbed systematically a low dose of L-lactate (31.5 ± 4.3 µg/100 g of body weight/day) which was approximately four times higher than that ingested in the W group through the diet supplied. Ex vivo cardiomyocyte contractility and the mass of some skeletal muscles (tibialis anterior) were increased by the L treatment. Myocardial calcium was decreased, as was evidenced by an increase in total CaMKII expression, without any change in the ratio between phosphorylated CaMKII and total CaMKII. Cardiac magnesium tended to be elevated. Our results suggest that the increased intracellular magnesium concentration was related to L-lactate-induced cytosolic acidosis and to the activation of the NHE1/NCX1 axis. Interestingly, systemic oxidative stress was reduced by the L treatment whereas the lipid profile of the animals was unaltered. Taken together, these results suggest that a chronic low-dose L-lactate intake has a beneficial health effect on some skeletal muscles and the myocardium through the activation of the NHE1/NCX1 axis, a decrease in cellular calcium and an increase in cellular magnesium. The treatment can be beneficial for the health of young rodents in relation to chronic oxidative stress-related diseases.





Similar content being viewed by others
Abbreviations
- AAT:
-
Abdominal adipose tissue
- Ac-SOD2:
-
Acetylated superoxide dismutase 2
- ADP:
-
Adenosine diphosphate
- ATP:
-
Adenosine triphosphate
- CaCl2 :
-
Calcium chloride
- CaMKII:
-
Calcium calmodulin ATPase II
- CaMKIIP:
-
Calcium calmodulin ATPase II phosphorylated at threonine 287; ATPase II
- CAT:
-
Catalase
- CLDML:
-
Chronic low-dose dietary magnesium L-lactate treatment
- CO2 :
-
Carbon dioxide
- CPT1β:
-
Carnitine palmitoyl-CoA transferase 1β
- ddCT:
-
2-ΔΔCT algorithm
- EDL:
-
Extensor digitorum longus
- EDTA:
-
Ethylene diamine tetraacetic acid
- EGTA:
-
Ethylene guanine tetraacetic acid
- FRAP:
-
Ferric reducing antioxidant power
- GPR81:
-
G protein-coupled receptor 81
- GPX:
-
Glutathione peroxidase
- HAD:
-
Hydroxyacyl coenzyme A dehydrogenase
- HDL:
-
High-density lipoproteins
- HEPES:
-
4-(2-Hydroxyethyl)-1-piperazineethanesulfonic acid
- HRP:
-
Horseradish peroxidase
- IL-1b:
-
Interleukin 1β
- IL-6:
-
Interleukin 6
- IL-10:
-
Interleukin 10
- KCl:
-
Potassium chloride
- L:
-
Magnesium L-lactate
- LDH:
-
Lactate dehydrogenase
- LDL:
-
Low-density lipoproteins
- LSD:
-
Least square difference
- MCT1:
-
Monocarboxylate transporter 1
- MgSO4 :
-
Magnesium sulphate
- MOPS:
-
3-Morpholino-1-propanesulfonic acid
- mPTP:
-
Mitochondrial permeability transition pore
- mRNA:
-
Messenger ribonucleic acid
- mTOR:
-
Mechanistic target of rapamycin
- NaCl:
-
Sodium chloride
- NAD:
-
Oxidized nicotinamide adenine dinucleotide
- NADH:
-
Reduced nicotinamide adenine dinucleotide
- NaHCO3 :
-
Sodium carbonate
- NHE1:
-
Sodium/proton exchange-1
- NCSS:
-
Number cruncher statistical software
- NCX1:
-
Sodium/calcium exchange-1
- O2 :
-
Dioxygen
- PAT:
-
Perirenal adipose tissue
- PD4K:
-
Pyruvate dehydrogenase 4 kinase
- PDH:
-
Pyruvate dehydrogenase
- PDHP:
-
Pyruvate dehydrogenase phosphorylated at serine 293
- PFK:
-
Phosphofructokinase
- PGC1α:
-
Peroxisome proliferator-activated receptor gamma coactivator 1-alpha
- PVDF:
-
Polyvinylidene fluoride
- RNA:
-
Ribonucleic acid
- ROS:
-
Reactive oxygen species
- RPM:
-
Rotation per min
- RT-qPCR:
-
Real-time quantitative polymerase chain reaction
- SDS-PAGE:
-
Sodium dodecyl sulphate polyacrylamide gel electrophoresis
- SEM:
-
Standard error of the mean
- SOD1:
-
Cytosolic superoxide dismutase
- SOD2:
-
Mitochondrial superoxide dismutase
- TA:
-
Tibialis anterior
- TBARS:
-
Thiobarbituric acid reactive substances
- TNF-α:
-
Tumour necrosis factor alpha
- VAT:
-
Visceral adipose tissue
- VDAC:
-
Voltage-dependent anion channel
- W:
-
Water
References
Baker SK, McCullagh KJ, Bonen A (1998) Training intensity-dependent and tissue-specific increases in lactate uptake and MCT-1 in heart and muscle. J Appl Physiol 84:987–994
Ben-Hamouda N, Haesler L, Liaudet L (2013) Hyperlactatemia and lactic acidosis in the critically ill patient. Rev Med Suisse 9:2335–2340
Bergmeyer HU, Bernt E (1974) UV-assay with pyruvate and NADH. In: Bergmeyer HU (ed) Methods of Enzymatic Analysis. London: Academic Press, pp 574–579
Berthet C, Lei H, Thevenet J, Gruetter R, Magistretti PJ, Hirt L (2009) Neuroprotective role of lactate after cerebral ischemia. J Cereb Blood Flow Metab 29:1780–1789
Berthet C, Castillo X, Magistretti PJ, Hirt L (2012) New evidence of neuroprotection by lactate after transient focal cerebral ischaemia: extended benefit after intracerebroventricular injection and efficacy of intravenous administration. Cerebrovasc Dis 34:329–335
Briston T, Roberts M, Lewis S, Powney B, JM S, Szabadkai G, Duchen MR (2017) Mitochondrial permeability transition pore: sensitivity to opening and mechanistic dependence on substrate availability. Sci Rep 7:10492
Brooks GA (2020) Lactate as a fulcrum of metabolism. Redox Biol 35:101454
Brooks GA, Dubouchaud H, Brown M, Sicurello JP, Butz CE (1999) Role of mitochondrial lactate dehydrogenase and lactate oxidation in the intracellular lactate shuttle. Proc Nat Acad Sci USA 96:1129–1134
Capel F, Demaison L, Maskouri F, Diot A, Buffiere C, Patureau Mirand P, Mosoni L (2005) Calcium overload increases oxidative stress in old rat gastrocnemius muscle. J Physiol Pharmacol 56:369–380
Cerretelli P, Samaja M (2003) Acid-base balance at exercise in normoxia and in chronic hypoxia. Revisiting the “lactate paradox.” Eur J Appl Physiol 90:431–448
Chen YD, Varasteh BB, Reaven GM (1993) Plasma lactate concentration in obesity and type 2 diabetes. Diab Metab 19:348–354
de Groot R, Sprenger RA, Imholz AL, Gerding MN (2011) Type B lactic acidosis in solid malignancies. Neth J Med 69:120–123
Dienel GA (2014) Lactate shuttling and lactate use as fuel after traumatic brain injury: metabolic considerations. J Cereb Blood Flow Metab 34:1736–1748
El Imad T, El Khoury L, Geara AS (2014) Warburg’s effect on solid tumors. Saudi J Kidney Dis Transpl 25:1270–1277
Erickson JR (2014) Mechanisms of CaMKII activation in the heart. Front Pharmacol 5:59
Falkowska A, Gutowska I, Goschorska M, Nowacki P, Chlubek D, Baranowska-Bosiacka I (2015) Energy metabolism of the brain, including the cooperation between astrocytes and neurons, especially in the context of glycogen metabolism. Int J Mol Sci 16:25959–25981
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18:499–502
Gardner PR, Nguyen DD, White CW (1994) Aconitase is a sensitive and critical target of oxygen poisoning in cultured mammalian cells and in rat lungs. Proc Ntl Acad Sci USA 91:12248–12252
Halestrap AP, Wilson MC (2012) The monocarboxylate transporter family–role and regulation. IUBMB Life 64:109–119
Hall MM, Rajasekaran S, Thomsen TW, Peterson AR (2016) Lactate: friend or foe. PM & R J Inj Funct Rehab 8:S8–S15
Horn T, Klein J (2013) Neuroprotective effects of lactate in brain ischemia: dependence on anesthetic drugs. Neurochem Int 62:251–257
Jacobs RA, Meinild AK, Nordsborg NB, Lundby C (2013) Lactate oxidation in human skeletal muscle mitochondria. Am J Physiol 304:E686-694
Kalogeris T, Baines CP, Krenz M, Korthuis RJ (2012) Cell biology of ischemia/reperfusion injury. Int Rev Cell Mol Biol 298:229–317
Kemp G (2005) Lactate accumulation, proton buffering, and pH change in ischemically exercising muscle. Am J Physiol 289:R895-901
Kinnally KW, Peixoto PM, Ryu SY, Dejean LM (2011) Is mPTP the gatekeeper for necrosis, apoptosis, or both? Biochim Biophys Acta 1813:616–622
Leger T, Azarnoush K, Traore A, Cassagnes L, Rigaudiere JP, Jouve C, Pages G, Bouvier D, Sapin V, Pereira B et al (2019) Antioxidant and cardioprotective effects of EPA on early low-severity sepsis through UCP3 and SIRT3 upholding of the mitochondrial Redox potential. Oxid Med Cell Long 2019:9710352
Levitsky DO, Takahashi M (2012) Interplay of Ca2+ and Mg2+ in sodium-calcium exchanger and in other Ca2+-binding proteins: magnesium, watchdog that block each turn if able. In: Advances in experimental medicine and biology - sodium calcium exchange: a growing spectrum of pathophysiological implications. Springer, pp 65–78
Lezi E, Lu J, Selfridge JE, Burns JM, Swerdlow RH (2013) Lactate administration reproduces specific brain and liver exercise-related changes. J Neurochem 127:91–100
Li X, Chen M, Yang Z, Wang W, Lin H, Xu S (2018) Selenoprotein S silencing triggers mouse hepatoma cells apoptosis and necrosis involving in intracellular calcium imbalance and ROS-mPTP-ATP. Biochim Biophys Acta 1862:2113–2123
Martin C, Dubouchaud H, Mosoni L, Chardigny JM, Oudot A, Fontaine E, Vergely C, Keriel C, Rochette L, Leverve X et al (2007) Abnormalities of mitochondrial functioning can partly explain the metabolic disorders encountered in sarcopenic gastrocnemius. Aging Cell 6:165–177
Mavric Z, Zaputovic L, Zagar D, Matana A, Smokvina D (1991) Usefulness of blood lactate as a predictor of shock development in acute myocardial infarction. Am J Cardiol 67:565–568
Mithieux G (2001) New data and concepts on glutamine and glucose metabolism in the gut. Curr Op Clin Nutr Metab Care 4:267–271
Mosienko V, Teschemacher AG, Kasparov S (2015) Is L-lactate a novel signaling molecule in the brain? J Cereb Blood Flow Metab 35:1069–1075
Mourmoura E, Couturier K, Hininger-Favier I, Malpuech-Brugere C, Azarnoush K, Richardson M, Demaison L (2014) Functional changes of the coronary microvasculature with aging regarding glucose tolerance, energy metabolism, and oxidative stress. Age (Dordr) 36:9670
Neely JR, Whitmer M, Mochizuki S (1976) Effects of mechanical activity and hormones on myocardial glucose and fatty acid utilization. Circ Res 38:I22-30
Nijsten MW, van Dam GM (2009) Hypothesis: using the Warburg effect against cancer by reducing glucose and providing lactate. Med Hyp 73:48–51
Nuutinen EM (1984) Subcellular origin of the surface fluorescence of reduced nicotinamide nucleotides in the isolated perfused rat heart. Basic Res Cardiol 79:49–58
Ohkuwa T, Tsukamoto K, Yamai K, Itoh H, Yamazaki Y, Tsuda T (2009) The relationship between exercise intensity and lactate concentration on the skin surface. Int J Biomed Sci 5:23–27
Panov A, Scarpa A (1996) Mg2+ control of respiration in isolated rat liver mitochondria. Biochem 35:12849–12856
Panov A, Scarpa A (1996) Independent modulation of the activity of alpha-ketoglutarate dehydrogenase complex by Ca2+ and Mg2+. Biochem 35:427–432
Percie du Sert N, Hurst V, Ahluwalia A, Alam S, Avey MT, Baker M, Browne WJ, Clark A, Cuthill IC, Dirnagl U et al (2020) The ARRIVE guidelines 2.0: Updated guidelines for reporting animal research. PLoS Biol 18:e3000410
Rice AC, Zsoldos R, Chen T, Wilson MS, Alessandri B, Hamm RJ, Bullock MR (2002) Lactate administration attenuates cognitive deficits following traumatic brain injury. Brain Res 928:156–159
Romani A, Marfella C, Scarpa A (1993) Regulation of magnesium uptake and release in the heart and in isolated ventricular myocytes. Circ Res 72:1139–1148
Schurr A (2002) Lactate, glucose and energy metabolism in the ischemic brain. Int J Mol Med 10:131–136
Shulman RG, Rothman DL (2001) The “glycogen shunt” in exercising muscle: a role for glycogen in muscle energetics and fatigue. Proc Ntl Acad Sci USA 98:457–461
Suranadi IW, Demaison L, Chate V, Peltier S, Richardson M, Leverve X (2012) An increase in the redox state during reperfusion contributes to the cardioprotective effect of GIK solution. J Appl Physiol 113:775–784
Taher M, Leen WG, Wevers RA, Willemsen MA (2016) Lactate and its many faces. Eur J Paediatric Neurol 20:3–10
Tapsell LC (2015) Fermented dairy food and CVD risk. Br J Nutr 113:S131–S135
Tun-Abraham ME, Martinez-Ordaz JL, Vargas-Rivas A, Sanchez-Fuentes JJ, Perez-Cerna E, Zaleta-Gonzalez O (2015) L-lactate as a serum marker of intestinal ischemia in patients with complicated intestinal obstruction. Cir Cir 83:65–69
Varanasi UR, Carr B, Simpson DP (1980) Lactic acidosis associated with metastatic breast carcinoma. Cancer Treat Rep 64:1283–1285
Vial G, Dubouchaud H, Couturier K, Lanson M, Leverve X, Demaison L (2008) Na+/H+ exchange inhibition with cariporide prevents alterations of coronary endothelial function in streptozotocin-induced diabetes. Mol Cell Biochem 310:93–102
Vitiello D, Cassirame J, Menetrier A, Rupp T, Schuster I, Reboul C, Obert P, Tordi N, Nottin S (2013) Depressed systolic function after a prolonged and strenuous exercise. Med Sci Sports Exer 45:2072–2079
Vitiello D, Rupp T, Bussiere JL, Robach P, Polge A, Millet GY, Nottin S (2013) Myocardial damages and left and right ventricular strains after an extreme mountain ultra-long duration exercise. Int J Cardiol 165:391–392
Won SJ, Jang BG, Yoo BH, Sohn M, Lee MW, Choi BY, Kim JH, Song HK, Suh SW (2012) Prevention of acute/severe hypoglycemia-induced neuron death by lactate administration. J Cereb Blood Flow Metab 32:1086–1096
Zhang D, Tang Z, Huang H, Zhou G, Cui C, Weng Y, Liu W, Kim S, Lee S, Perez-Neut M et al (2019) Metabolic regulation of gene expression by histone lactylation. Nature 574:575–580
Acknowledgements
The authors warmly thank the staff of the Experimental Unit of Animal Nutrition of the National Institute of Agronomical Research (INRAE) of Theix/Saint-Genès-Champanelle for animal care. They also wish to thank Patricia Mabrut for editing the manuscript.
Funding
This work was supported by the French National Institute of Agronomical Research (INRAE).
Author information
Authors and Affiliations
Contributions
MMP, HD, CJ, JPR, VP, IH-F, DB and LD contributed to the technical part of the study. LD performed the statistical analyses. LD contributed to the study conception and design, analysis and interpretation of data. LD wrote the manuscript; HD and SW revisited it critically and gave final approval of the version to be published.
The authors declare that all data were generated in-house and that no paper mill was used.
Corresponding author
Ethics declarations
Ethics approval
All experiments followed the European Union recommendations concerning the care and use of laboratory animals for experimental and scientific purposes. All animal work was approved by the national board of ethics for animal experimentation (authorization Apafis n° 00958.02). The performed research was in compliance with the ARRIVE guidelines on animal research.
Conflict of interest
The authors declare that they have no conflicts of interest with the contents of this article. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Agronomical Research (INRAE).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
- Dietary magnesium L-lactate increases myocardial contractility and skeletal muscle mass.
- In the heart, this phenomenon results from increased cellular magnesium.
- Increased magnesium is due to acidosis-induced stimulation of the NHE1/NCX1 axis.
- Dietary magnesium L-lactate can be used to maintain health in physically handicapped people.
Rights and permissions
About this article
Cite this article
Pinto, M.M., Dubouchaud, H., Jouve, C. et al. A chronic low-dose magnesium L-lactate administration has a beneficial effect on the myocardium and the skeletal muscles. J Physiol Biochem 78, 501–516 (2022). https://doi.org/10.1007/s13105-021-00827-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13105-021-00827-8