Abstract
Purpose
Though febrile neutropenia (FN) risk prediction models are important in clinical practice, their external validation is limited. In this study, we validated the Cycle-Specific Risk of FEbrile Neutropenia after ChEmotherapy (CSRFENCE) score for predicting FN.
Methods
We reviewed the medical records of patients with solid malignancies and diffuse large B-cell lymphoma during chemotherapy cycles 2–6 and recorded if patients developed FN, defined as absolute neutrophil counts less than 500 cells/microL with fever more than or equal to 38.2 ℃. The CSRFENCE score was determined by adding the risk factors' coefficients described by the original study; subsequently, the score was used to classify chemotherapy cycles into the following risk groups for developing FN: low, intermediate, high, and very high risk. The discriminatory ability of the score was assessed using area under the receiver operating characteristics curve (AUROCC) and incidence rate ratios (IRR) within each CSRFENCE risk group.
Results
We analyzed 2870 chemotherapy cycles, of which 42 (1.5%) were associated with FN. Among those, 3 (7.1%), 14 (33.3%), 5 (12%), and 20 (47.6%) were classified as low, intermediate, high, and very high risk for developing FN, respectively. The AUROCC was 0.72 (95% CI 0.64–0.81). Compared with the low risk group (n = 666), the IRR of developing FN was 1.01 (95% CI 0.15–43.37), 0.69 (95% CI 0.08–32.46) and 1.17 (95% CI 0.17–49.49) in the intermediate (n = 1431), high (n = 498) and very high (n = 275) risk groups, respectively.
Conclusion
The CSRFENCE model can moderately stratify patients into four risk groups for predicting FN prior to chemotherapy cycles 2–6.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Febrile neutropenia (FN) is a life-threatening complication of myelosuppresive chemotherapy. FN may result in chemotherapy delays, reduced chemotherapy dose intensity and treatment discontinuation leading to suboptimal treatment effects of cancer, especially in patients receiving chemotherapy for curative intent [1]. Prophylactic use of granulocyte colony-stimulating factors (G-CSF) and antimicrobials, along with non-pharmacological measures, have been the cornerstones of FN prevention in patients at high risk for developing FN [2].
The guidelines recommend assessing the risk of FN at the start of each chemotherapy cycle to initiate preventive measures in high risk patients [3,4,5]. Current guidelines determine the overall risk of developing FN based on the anticipated risk associated with the administered chemotherapy regimen [3]. However, the chemotherapy regimen is one component of risk assessment and must be combined with patient specific risk factors and disease characteristics to estimate the individual’s overall risk of FN [3,4,5]. At present, there is no clear guidance in terms of how to determine the specific risk for FN based on the underlying risk factors. Thus, there is an increasing interest in developing risk prediction models to stratify patients based on their overall risk of developing FN before chemotherapy delivery, taking into consideration patient- and treatment- related factors.
The FEbrile Neutropenia after ChEmotherapy (FENCE) score is a clinical tool that was recently developed by Aagaard et al. to estimate the risk of developing FN at the first cycle of chemotherapy in treatment-naïve patients with solid tumors and diffuse large B-cell lymphoma (DLBCL) [6]. However, the FENCE score does not include several factors that may increase the risk of neutropenic fever in the following cycles, such as chemotherapy delay and previous episodes of FN. To address this issue, a cycle specific risk score was created to predict the risk of developing FN in cycles that follow the initial cycle of chemotherapy, specifically cycles 2 to 6, and referred to it as the “Cycle-Specific Risk of FEbrile Neutropenia after ChEmotherapy (CSRFENCE) score” [7]. Though Aagaard et al. suggested that the CSRFENCE risk score had good discriminatory ability, there was no validation of that prediction score in external cohorts.
Therefore, we sought to externally validate the CSRFENCE risk score in predicting FN prior to chemotherapy cycles 2–6 in a cohort of patients with solid malignancies and DLBCL.
2 Methods
A retrospective chart review conducted between January 2019 and November 2019 at a comprehensive cancer center in Jordan, King Hussein Cancer Center (KHCC). The center is a 350-bed hospital that provides comprehensive cancer care to over 3500 new patients per year. The protocol was approved by the institutional review board of KHCC (study#20 KHCC188) with waiver of consent in view of the retrospective nature of the study [8]. The study was conducted in accordance with the Declaration of Helsinki and adhered to Good Clinical Practice guidelines.
Newly diagnosed adult patients with solid malignancies and DLBCL who had received their second cycle of chemotherapy were included in the study and their medical records were reviewed until discontinuation of chemotherapy, administration of a maximum of 6 chemotherapy cycles, death, or loss to follow-up, whichever came first. Based on the study by Aagaard et al., we excluded patients who received two alternating chemotherapy regimens, patients who received weekly platinum-based chemotherapy, patients who had undergone bone marrow transplantation and those who were receiving cancer-related treatment as part of an investigational study or compassionate protocol [6, 7].
We extracted the patients’ baseline characteristics, demographics, and the risk factors required for the CSRFENCE score calculation, which included the FENCE risk group (based on pre-therapy risk factors used to calculate the FENCE score in the first cycle of chemotherapy), concurrent radiotherapy, cycle number, FN or neutropenia in previous cycles, and G-CSF prophylaxis [7, 8].
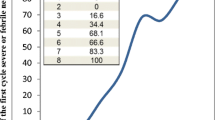
We followed the methodology to calculate the CSRFENCE risk score for each patient’s individual cycle, as described in the original publication by Aagaard et al. First, we summed the assigned coefficients for each pre-therapy risk factor to calculate the CSRFENCE score. Subsequently, we stratified each patient’s risk for developing FN prior to each chemotherapy cycle based on the calculated CSRFENCE score as follows: low risk (score < 0), intermediate risk (score 1- 4), high risk (score 5—6), and very high risk (score ≥ 7) [7].
Patients were evaluated for any visits to the emergency department or admissions to the hospital that may have been associated with FN between cycles 2 and 6 of chemotherapy. We defined FN based on the criteria we used in our earlier study that evaluated the validity of the FENCE score and the criteria recommended by the clinical guidelines [8]. FN was defined as absolute neutrophil counts less than 500 cells/microL with fever more than or equal to 38.2 ℃ [3,4,5]. We recorded the outcomes following each FN episode including hospital admission, mortality, as well as chemotherapy dose reduction and dose delay in subsequent cycles.
2.1 Statistical analysis
For descriptive statistics, median and interquartile range (IQR) were used to present continuous data, while numbers and percentages were used to present nominal data. The discriminatory ability of classifying patients into CSRFENCE risk groups was determined by the area under the receiver operating characteristics curve (AUROCC) and incidence rate ratios (IRR), with their corresponding 95% confidence intervals (CI) within each CSRFENCE risk group. In addition, a sensitivity analysis was performed to test the score performance when excluding patients who received G-CSF during their treatment. All analyses were performed with SAS version 9.4 (SAS Institute Inc, Cary, NC, USA) [8].
3 Results
During the study period, 860 patients received a total of 2870 chemotherapy cycles, 2 through 6. The median follow-up was 3 cycles (IQR 2–4) with a median cycle length of 21 days (IQR 14–28). Table 1 outlines the characteristics of the patients prior to each chemotherapy cycle assessed.
FN was reported in 42 (1.5%) cycles in which one third of the episodes occurred after cycle two (n = 14, 33.3%) and about one third occurred after cycle three (n = 12, 28.6%). Among the reported FN episodes, the majority required hospitalization (n = 35, 83.3%) while the remaining were managed in the emergency department. All patients were discharged from the hospital. Dose reductions and chemotherapy delays occurred in 6 (14.3%) and 9 (21.4%) of the subsequent cycles, respectively.
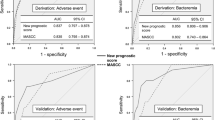
According to the CSRFENCE risk group classification, the chemotherapy cycles administered were considered as being low risk (n = 666, 23.2%), intermediate (n = 1431, 49.8%), high (n = 498, 17.4%) and very high (n = 275, 9.6%) risk for FN. Among the reported FN episodes, 3 (7.1%) were reported in the low risk, 14 (33.3%) were reported in the intermediate, 5 (12%) were reported in the high risk, and 20 (47.6%) were reported in the very high risk group. The AUROCC was 0.72 (95% CI 0.64– 0.81) (Fig. 1). When excluding patients who were on G-CSF, sensitivity analysis resulted in an AUROCC of 0.72 (95% CI 0.62–0.82).
The IRR per point increase in CSRFENCE score was 2.62 (95% CI 1.80–3.82). Compared to those at low risk, the IRR of developing FN was 1.01 (95% CI 0.15–34.37), 0.69 (95% CI 0.08 – 32.46) and 1.17 (95% CI 0.17–49.49) in the intermediate, high, and very high risk groups, respectively.
4 Discussion
In this study, we aimed to assess the ability of utilizing the CSRFENCE risk groups in predicting the risk of developing FN during chemotherapy cycles 2–6 in an independent dataset. When applied to our cohort, the classification based on the CSRFENCE risk groups demonstrated a moderate discriminatory ability for predicting FN. This was consistent with the results of the validation cohort of the original study by Aagaard et al., who also reported good discriminatory ability to predict the underlying risk of FN at chemotherapy cycle initiation and concluded that a model utilizing cycle-specific risk factors performs better than one that solely uses pre-therapy data [7].
Although the FENCE score was used to predict the risk of FN in solid tumors and DLBCL during first cycle of chemotherapy, Aagaard et al. were unable to track treatment changes in DLBCL patients in subsequent chemotherapy cycles and therefore did not include them in the CSRFENCE score. However, in our study, we decided to include DLBCL patients within our validation cohort since the FENCE risk group, which included DLBCL patients, is one of the items used to calculate the CSRFENCE score.
The population in the current study were younger at baseline (median 55 years IQR 44–63) compared to the original study (median 64 years IQR 54–71), where notably age > 65 is considered a risk factor for developing FN [3]. The majority of our patients were initially classified in the low (36.6%) and intermediate (29.9%) FENCE risk groups for developing FN after cycle one of chemotherapy. Furthermore, our population was predominately breast cancer patients (42%), who also made up the majority of FN cases (47%). This may impact the generalizability of our findings to other types of cancer. In addition, about 80% of our patients did not experience previous neutropenia or FN in any of their cycles, and as suggested by the guidelines, having previous episode of FN or a dose-limiting neutropenic event increases the overall FN risk to a high risk group [3].
Our findings showed a significant 2.6-fold increase in the incidence of FN per point increase in the CSRFENCE score. However, the differences in IRR between the stratified risk groups were not statistically significant, and the confidence intervals were wide. This could be explained by the relatively few reported FN events (1.5%) and possibly a limited power to detect a significant difference between the CSRFENCE risk groups.
The incidence of FN (1.5%) reported in our study was relatively similar to that reported by Aagaard et al. (2.1%). In our study, we used the narrow definition of FN, which is utilized by our center and more commonly used in clinical practice [3,4,5]. Due to the lack of certain data in the patients’ records in the original study such as temperature, Aagaard et al. used a wide definition for FN, which included any blood culture or death within 3 days of a neutrophil count < 0.5 × 109/L or a leukocyte count < 2 × 109/L. However, they reported in their sensitivity analysis that the discriminatory ability of the score was similar between the wide and narrow guideline definition of FN (i.e. documented fever and neutropenia) [6, 7].
In this study, the majority of the patients experienced FN following cycles 2 and 3, compared to subsequent cycles. A prospective study by Culakova et al. that evaluated the time course of neutropenic events in patients with early-stage breast cancer concluded that the risk of FN was greatest in the first cycle when most patients receive full-dose chemotherapy. Moreover, they reported a decrease in the incidence of FN during subsequent cycles due to reduced dose intensity of chemotherapy or increased use of supportive care measures [9]. In the present study, we cannot draw a clear conclusion regarding the effect of changes in dose intensity in the subsequent cycles due to infrequent occurrence of FN in our cohort.
Although the main aim of developing the CSRFENCE score was to assess risk factors that only appear in later cycles such as chemotherapy dose delay and reduction, Aagaard et al. did not include them as risk factors when determining the CSRFENCE risk groups. They assumed that there was a high level of correlation between these risk factors and prior FN or neutropenia which were identified as strong predictors of future FN in the subsequent cycles and were included in the final score.
Few studies have addressed the cycle-specific risk factors for predicting FN beyond the first cycle of chemotherapy. Among those, some have assumed that the risk of FN in cycle 1 can be extrapolated to subsequent cycles [10], while others have focused on a single cancer type such as breast cancer [11] or specific risk factors such as early lymphopenia [12]. Furthermore, limited accuracy of some prediction models were reported [11, 13]. Given these limitations as well as the heterogeneity of the published data, it is difficult to compare between the studies [14].
To our knowledge, this represents the first study to validate the CSRFENCE risk groups in an external population. In addition, we included a relatively large cohort of patients with variable risk factors and chemotherapy regimens which would help in the understanding of the performance of the score in different cohorts before clinical implementation.
The current study has several limitations. First, it was conducted at a single center that might not be generalizable to other cancer centers with different healthcare practices. Secondly, patient's data were collected through a retrospective chart review and were limited by the quality of data documented. Third, as discussed in our recent publication, we did not look into independent risk factors for FN such as the dose intensity of the administered chemotherapy, co-morbidities, bone marrow involvement, corticosteroids and other immunosuppressants, as well as the performance status, which would add to the existing literature and might reveal important risk factors [8].
The CSRFENCE score showed moderate discriminatory ability for identifying patients who are at high risk of developing FN during chemotherapy cycles 2–6 and hence could guide physicians in tailoring patient's treatment goals and initiate preventive measures based on pre-defined risk assessment. This may reduce the complications of FN and maintain the chemotherapy dose intensity. However, our findings indicate that the CSRFENCE risk score necessitates some refinements before being used in clinical practice.
5 Conclusion
Our study demonstrated that the CSRFENCE model can moderately stratify patients into four risk groups for predicting FN prior to chemotherapy cycles 2–6. Further prospective validation addressing the CSRFENCE risk score limitations across diverse cohorts are needed before clinical adoption.
Data availability
The data used in this study are available from the corresponding author, upon request.
Code availability
Not applicable.
Abbreviations
- AUROCC:
-
Area under the receiver operating characteristics curve
- CI:
-
Confidence interval
- CSRFENCE:
-
Cycle-Specific Risk of FEbrile Neutropenia after ChEmotherapy
- DLBCL:
-
Diffuse large B-cell lymphoma
- FENCE:
-
FEbrile Neutropenia after ChEmotherapy
- FN:
-
Febrile neutropenia
- G-CSF:
-
Granulocyte colony-stimulating factors
- IQR:
-
Interquartile range
- IRR:
-
Incidence rate ratio
- KHCC:
-
King Hussein Cancer Center
- ROC:
-
Receiver operating characteristic
References
Repetto L, CIPOMO investigators. Incidence and clinical impact of chemotherapy induced myelotoxicity in cancer patients: an observational retrospective survey. Crit Rev Oncol Hematol. 2009;72(2):170–9. https://doi.org/10.1016/j.critrevonc.2009.03.004.
Lucas AJ, Olin JL, Coleman MD. Management and preventive measures for febrile neutropenia. P T. 2018;43(4):228–32.
National Comprehensive Cancer Network. Hematopoietic growth factor (version 2.2020). https://www.nccn.org/professionals/physician_gls/pdf/growthfactors.pdf. Accessed 10 Mar 2022
Klastersky J, de Naurois J, Rolston K, et al. Management of febrile neutropaenia: ESMO clinical practice guidelines. Ann Oncol. 2016;27(suppl 5):v111–8. https://doi.org/10.1093/annonc/mdw325.
Smith TJ, Bohlke K, Lyman GH, et al. Recommendations for the use of WBC growth factors: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol. 2015;33(28):3199–212. https://doi.org/10.1200/JCO.2015.62.3488.
Aagaard T, Roen A, Reekie J, et al. Development and validation of a risk score for febrile neutropenia after chemotherapy in patients with cancer: the FENCE score [published correction appears in JNCI Cancer Spectr. 2019;3(1):pkz009]. JNCI Cancer Spectr. 2018;2(4):pky053. Published 2018 Nov 29. doi:https://doi.org/10.1093/jncics/pky053
Aagaard T, Reekie J, Roen A, et al. Development and validation of a cycle-specific risk score for febrile neutropenia during chemotherapy cycles 2–6 in patients with solid cancers: the CSR FENCE score. Int J Cancer. 2020;146(2):321–8. https://doi.org/10.1002/ijc.32249.
Zatarah R, Faqeer N, Quraan T, et al. Validation of the FENCE risk groups for prediction of febrile neutropenia with first-cycle chemotherapy. JNCI Cancer Spectr. 2022;6(3):038. https://doi.org/10.1093/jncics/pkac038.
Culakova E, Poniewierski MS, Wolff DA, Dale DC, Crawford J, Lyman GH. The impact of chemotherapy dose intensity and supportive care on the risk of febrile neutropenia in patients with early stage breast cancer: a prospective cohort study. Springerplus. 2015;4:396. https://doi.org/10.1186/s40064-015-1165-6.
Lyman GH, Kuderer NM, Crawford J, et al. Predicting individual risk of neutropenic complications in patients receiving cancer chemotherapy. Cancer. 2011;117(9):1917–27. https://doi.org/10.1002/cncr.25691.
Chen K, Zhang X, Deng H, et al. Clinical predictive models for chemotherapy-induced febrile neutropenia in breast cancer patients: a validation study. PLoS ONE. 2014;9(6):e96413. https://doi.org/10.1371/journal.pone.0096413.
Ray-Coquard I, Borg C, Bachelot T, et al. Baseline and early lymphopenia predict for the risk of febrile neutropenia after chemotherapy. Br J Cancer. 2003;88(2):181–6. https://doi.org/10.1038/sj.bjc.6600724.
Jenkins P, Scaife J, Freeman S. Validation of a predictive model that identifies patients at high risk of developing febrile neutropaenia following chemotherapy for breast cancer. Ann Oncol. 2012;23(7):1766–71. https://doi.org/10.1093/annonc/mdr493.
Lyman GH, Abella E, Pettengell R. Risk factors for febrile neutropenia among patients with cancer receiving chemotherapy: a systematic review. Crit Rev Oncol Hematol. 2014;90(3):190–9. https://doi.org/10.1016/j.critrevonc.2013.12.006.
Acknowledgements
The author(s) received no funding and/or grants for the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research and/or authorship of this article.
Author information
Authors and Affiliations
Contributions
RZ, NF and LN contributed to the study conception and design. Material preparation and data collection were performed by RZ, AM, TQ, LM and AK. Data analysis was performed by RZ. The first draft of the manuscript was written by RZ, NF and LN and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol was approved by the institutional review board of King Hussein Cancer Center (study#20 KHCC188) with waiver of consent in view of the retrospective nature of the study. The study was conducted in accordance with the Declaration of Helsinki and adhered to Good Clinical Practice guidelines.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zatarah, R., Faqeer, N., Mahmoud, A. et al. Validation of the CSRFENCE score for prediction of febrile neutropenia during chemotherapy cycles 2–6. Discov Onc 13, 107 (2022). https://doi.org/10.1007/s12672-022-00575-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12672-022-00575-1