Abstract
Purpose
Patients with acute exacerbations of chronic obstructive pulmonary disease (AECOPD) suffer not only from somatic symptoms but also from symptoms of anxiety, depression, and stress. Mindfulness-based interventions (MBIs) have been shown to effectively reduce these symptoms in other conditions. In patients with AECOPD, MBIs are under-researched. The present study explored whether patients hospitalized for AECOPD perceive MBIs as appropriate and feasible, and how MBIs might be implemented and adapted for this patient group.
Method
In an exploratory qualitative study, one-time semi-structured interviews were conducted with 20 patients hospitalized for AECOPD (65% women; Mage=70.85 years, SD=7.53). Data were analyzed using reflexive thematic analysis and a codebook approach.
Results
Most patients were interested in add-on treatment options such as MBIs and considered them as potentially beneficial (65%). Patients’ understanding of mindfulness varied and was difficult to separate from other mind-body practices (e.g., autogenic training). Previous experiences with mind-body practices and expectations regarding the effectiveness of MBIs influenced patients’ interest in MBIs. Context factors (e.g., short exercises) were more important than content factors (e.g., type of exercise). General barriers (e.g., scheduling issues) and COPD-related limitations (e.g., decreased mobility) hindered the self-administration of MBIs.
Conclusions
Most patients hospitalized for AECOPD interviewed in this study were interested in MBIs and rated them as potentially helpful and feasible to incorporate in health care settings and everyday life. Future studies investigating MBIs in COPD are needed and should carefully consider patients’ perspectives, addressing context factors (e.g., timing, exercise length), patients’ needs, and COPD-related limitations.
Preregistration
This study is not preregistered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Chronic obstructive pulmonary disease (COPD) is one of the world’s most pressing health problems, listed among the ten main global causes of death and disability in 2019 (World Health Organization, 2020). COPD is a treatable but incurable condition characterized by airflow limitation and persistent respiratory symptoms. Besides the stable or slowly progressing phases of disease, many patients experience acute exacerbations of COPD (AECOPD). AECOPD are acute crises of breathing characterized by intense, temporal deteriorations of respiratory symptoms—such as breathlessness, cough, and sputum production. Some AECOPD are life-threatening and require hospital admission (Global Initiative for Chronic Obstructive Lung Disease, 2023). Due to its chronic nature and consequent long-term morbidity, COPD incurs remarkable economic costs, especially in moderate to severe stages of the disease, which are accompanied by a higher frequency of AECOPD and increased comorbidities (Gutiérrez Villegas et al., 2021).
COPD also entails a significant personal burden for the patient. In addition to somatic comorbidities, symptoms of anxiety and depression are commonly observed in patients with COPD (Global Initiative for Chronic Obstructive Lung Disease, 2023). In turn, both anxiety and depressive symptoms correlate with other negative health outcomes such as an increased risk of exacerbation and a higher likelihood of hospitalization (Laurin et al., 2012; Pooler & Beech, 2014). Chronic conditions such as COPD also constitute major stressors for the affected individuals (Holmes & Rahe, 1967). Indeed, COPD patients rated breathing problems—which accumulate during AECOPD—as their predominant stressor in everyday life (Andenæs et al., 2006). Further, research demonstrating a general sympathetic over-activity of the autonomic nervous system (Van Gestel et al., 2012) and elevated systemic inflammatory response (Singh et al., 2018) in COPD patients, both of which are recognized as bodily stress systems (e.g., Nater et al., 2013), may indicate a dysregulation within the body’s stress systems in relation to COPD pathology. As symptoms of anxiety and depression have consistently been associated with altered functioning of the bodily stress systems (e.g., Schiweck et al., 2019; Zorn et al., 2017), mental health interventions for COPD patients should also target stress, as a possible underlying mechanism linking somatic and mental health outcomes, especially in patients who frequently experience AECOPD.
Besides medication, psychological interventions like cognitive behavioral therapy, as well as multidisciplinary pulmonary rehabilitation and self-management programs, have been shown to reduce symptoms of anxiety and depression in COPD (Gordon et al., 2019; Smith et al., 2014). Psychological interventions have been shown to reduce psychological stress and alter the activity and reactivity of bodily stress systems in other populations (e.g., cortisol measures, Rogerson et al., 2024). However, their effects on regulating the body’s stress systems, or cognitions and emotions related to stress, in patients with COPD remain unclear. Therefore, mindfulness-based interventions (MBIs) may constitute a suitable add-on treatment option for COPD patients. MBIs have been shown to improve various somatic and mental health outcomes, among them also symptoms of anxiety, depression, and stress, as well as biological correlates of stress like immune functioning, in healthy and clinical populations (Goldberg et al., 2021; Oyler et al., 2023; Zhang et al., 2021). Mindfulness includes consciously directing and maintaining one’s attention towards stimuli or experiences that can be perceived internally or externally while orienting to these stimuli or experiences without giving meaning or value to them (Bishop et al., 2004). For people suffering from a chronic somatic condition, mindfulness might modify their relationship with the disease by altering their thoughts, emotions, and maladaptive habitual response patterns regarding the illness and developing a greater sense of acceptance of the condition. Furthermore, mindfulness may be able to promote the early detection of and sense of control over symptoms, as well as regulate the psychobiological response to stressors by altering the activity and functional connectivity of brain regions related to initiating the biological stress response (e.g., prefrontal cortical regions, Creswell, 2017).
With regard to COPD, a recent systematic review summarized the—surprisingly low number of—RCTs on MBIs implemented in primary care settings with outpatients (Clari et al., 2020). The majority of studies investigated an adapted version of Mindfulness-Based Stress Reduction (MBSR) (Kabat-Zinn, 2013) or Mindfulness-Based Cognitive Therapy (MBCT) (Segal et al., 2018), two group-based MBI programs. Qualitative studies have reported positive effects of MBIs, such as improved psychological and emotional well-being, and an enhanced sense of control over COPD symptoms (Clari et al., 2020). While one reviewed study reported a reduction of depressive symptoms (Farver-Vestergaard et al., 2018a), no significant effects emerged on symptoms of anxiety, subjective stress, mindfulness, proinflammatory immune markers, or somatic outcomes (Clari et al., 2020). Studies investigating immediate pre-post effects of single mindfulness-based exercises found reductions in symptoms of anxiety, dyspnea, and respiratory rate in COPD outpatients (Reaves & Angosta, 2021) and hospitalized COPD patients (Tan et al., 2019). However, when compared to an active control group, no significant effects for symptoms of anxiety, depression, and dyspnea could be found for a brief MBI (Perkins-Porras et al., 2018). In sum, it remains unclear whether MBIs can significantly reduce symptoms of anxiety, depression, and stress in COPD.
As most of the data in this area stem from COPD outpatients, the effectiveness of MBIs in hospitalized patients with AECOPD is yet to be determined, and it has not been ascertained whether or how MBIs can be feasibly implemented in health care settings and everyday life for this subgroup of patients. It is important to note that outpatients differ from hospitalized patients. Outpatients mostly report stable COPD symptoms, while hospitalized COPD patients suffer from an intense, temporary deterioration of respiratory symptoms, which is associated with more physical limitations and potentially a higher psychological burden. Given that patients with AECOPD are especially impaired by dyspnea and other physical complaints, and experience elevated levels of anxiety, depression (e.g., Long et al., 2020), and stress, they might be especially motivated and may perceive stronger benefits from MBIs compared to COPD outpatients. On the other hand, due to their increased symptom burden, patients with AECOPD might not be receptive to or interested in engaging in a new and unfamiliar technique like mindfulness, or may have different requirements of an MBI compared to outpatients. Previous studies have demonstrated that MBIs such as adapted versions of MBCT or MBSR are too time-consuming or physically demanding for COPD outpatients, and these issues might be amplified in patients hospitalized for AECOPD (Farver-Vestergaard et al., 2018b; Mularski et al., 2009). Research has also shown that the mode of delivery can be a barrier to conducting an MBI, affecting participation and adherence (Clari et al., 2020). In this regard, digital MBIs might therefore be a promising option for patients hospitalized for AECOPD. Digital MBIs have not only been shown to effectively reduce psychological outcomes (Tan et al., 2022), but digital healthcare interventions are easily accessible, cost-effective, and can be implemented both in health care settings and everyday life (Watson & Wilkinson, 2022).
To explore the feasibility and effects of MBIs in patients hospitalized for AECOPD, it is necessary to first understand hospitalized patients’ needs and perspectives on MBIs and to determine which requirements must be met when implementing an MBI. Therefore, this investigation did not involve conducting an MBI with patients but rather positioned itself one step ahead of conducting an interventional pilot study, aimed at preparing the ground for future intervention studies. In this study, we explored the views and perspectives of hospitalized AECOPD patients regarding MBIs, without conducting an MBI. The aim of this study was to investigate whether MBIs are feasible for patients hospitalized for AECOPD and to identify implementation and adaptation criteria for the future implementation of MBIs in this specific patient group. Specifically, feasibility, as we use the term in this paper, is defined by the possibility that something can be done and is reasonable (aligned with the definition of feasibility in the Cambridge dictionary, Cambridge University Press & Assessment, 2024). In the context of our study, the term feasibility should not be confused with the meaning typically used in interventional pilot studies, where feasibility refers to the evaluation of an implemented intervention. Instead, we use it in its broader conceptualization to describe something that is appropriate, acceptable, practical, and possible to implement.
Method
Participants
We conducted an exploratory qualitative study using semi-structured interviews and questionnaires for participant characterization. We determined a sample size of 20 patients based on sample sizes in studies using similar methodological approaches (commonly ranging from 15 to 30 interviews; e.g., Harrison et al., 2017) and considering theoretical aspects, such as the diversity of the population regarding our research question and the depth of the planned analysis (i.e., analysis at a semantic level; Braun & Clarke, 2013). Expecting a rather homogenous sample due to convenience sampling and self-selection of participants and being interested in explicit rather than latent meaning, we determined that one-time interviews with 20 patients would be sufficient to address our research question. Following the pilot phase (June-August 2019), in which three patients were interviewed in order to evaluate and adapt the interview guide, recruitment lasted from September 2019 to November 2020. Overall, 21 patients were included in the study; however, one patient (ID 14) had to be excluded from the data analysis as they did not meet inclusion Criterion b (for details see Participants section), which became apparent during the interview. Due to the COVID-19 outbreak in Austria in March 2020, recruitment was paused for six months and resumed in September 2020, with the study procedure being adapted in line with the hospital’s COVID-19 regulations (for details see Participants and Procedure sections).
Patients hospitalized for AECOPD were selected using convenience sampling and were recruited by their treating physician at the respiratory unit of the hospital. Participants were included if they were (a) hospitalized for AECOPD, (b) had a spirometry-confirmed COPD diagnosis (post bronchodilator FEV1/ FVC < 0.70) for at least a year, (c) had sufficient German language skills to understand and answer the interview questions, and (d) were at least 40 years old to prevent overlaps with the diagnosis of late-onset asthma. We excluded persons who (a) were in a poor medical condition, (b) had cognitive, (c) severe linguistic or (d) auditory impairments, and (e) had an active asthma diagnosis. Additionally, after the COVID-19 outbreak, all patients admitted to the hospital had been tested for an infection with SARS-CoV-2 using a diagnostic test (antigen or polymerase chain reaction) and were excluded if they were actively infected.
Procedure
Recruited patients were verbally informed about the study and provided written consent at study entry. Semi-structured face-to-face interviews took place several days after the patients’ hospitalization (days after hospitalization: M = 5.35, SD = 4.99, range: 1–23), either in the common patient area or in the patient’s room. The interviews lasted around 50 min (M = 50.75, SD = 21.17, range: 10–90) and were audio-recorded using the app “Recorder” (Version 8.0.0.353) on a smartphone (Huawei Y6 ATU-L21). One research team member (HT, female), a psychologist and PhD student in the field of clinical and health psychology, conducted the interviews using an interview guide. With the exception of training in the pilot phase, the interviewer had no previous experience in conducting semi-structured interviews and had no preceding contact with or information about the participants.
After the interview, the interviewer collected sociodemographic and medical data as well as data on the impact of COPD on the patients’ health status. In addition, the treating physician provided data from the patients’ medical records. The interviewer additionally took notes about non-auditory information presented by the patients, details about the setting and procedure, and relevant interview and patient characteristics. After the resumption of the study in September 2020, the hospital’s COVID-19 protocol (e.g., negative SARS-CoV-2 antigen test result before meeting the patient, wearing an FFP2 face mask) was strictly followed to ensure a safe in-person contact.
Measures
Interviews
The topics and questions of the interview guide (see Table 1 for topics and Online Resource 1 for the full guide) were informed by previous research (Harrison et al., 2017) and the experiences of the authors, and were evaluated and adjusted in the piloting phase.
In addition to the topics listed in Table 1, a single quantitative item, “How strongly do you feel impaired by your lung disease today?”, served as an entry question at the beginning of the interview and was answered on a 5-point Likert scale ranging from 0 = not at all to 4 = very strongly. Furthermore, patients were introduced to and familiarized with mindfulness (with reference to its conceptualization by Kabat-Zinn, 2015, based on the explanation in Segal et al., 2018) prior to Topic 4 (Table 1). This introduction had been elaborated in the piloting phase, resulting in a combination of experiential and theoretical elements: the conduction of a short version of the “stone exercise” (based on the “raisin exercise” used in MBCT by Segal et al., 2018), the explanation of the main pillars of mindfulness (non-judgmental present-moment awareness, purposeful attention, openheartedness; Kabat-Zinn, 2015) and examples of different mindfulness exercises (e.g., sitting meditation), and the conduction of a short 5-min “body scan” (based on the “body scan” used in MBCT by Segal et al., 2018), guided by the interviewer. The introduction was adapted to patients’ previous knowledge about mindfulness, their openness to the exercises, and setting-related factors (e.g., noise, interruptions).
Questionnaires for Participant Characterization
Details on the assessed sociodemographic and medical data are provided in Online Resource 2. The impact of COPD on participants’ health status was assessed using the German version of the COPD Assessment Test (CAT; Jones et al., 2009), a self-report measure comprising eight items rated on a six-point semantic differential scale (0–5) with contrasting statements (e.g., “I never cough” vs. “I cough all the time”). The CAT has very good psychometric properties (internal consistency: Cronbach’s α = 0.88) and is widely used in clinical practice and research. The sum score ranges from 0 to 40, with higher scores indicating a higher impact of COPD on health status.
Data Analyses
Pseudonymized verbal data of the interviews were fully transcribed (software: f4transcript, version 7) and analyzed (software: f4analyse, version 2) by the interviewer, using reflexive thematic analysis (Braun & Clarke, 2006, 2019, 2020), a well-established qualitative analysis method suitable to explore patients’ experiences and meanings. A largely realist and semantic approach was used as the analysis focused on the explicit content reported by the patients. The structured process encompasses the following six steps: (1) transcribing the interviews (transcription system adapted from Kuckartz et al., 2008), (2) generating codes, (3) developing themes, (4) reviewing themes, (5) defining and naming themes, and (6) writing a report (Braun & Clarke, 2006).
Each transcript was re-read to validate the data. The dataset for coding was chosen deductively, based on the research question, meaning that paragraphs of the interviews were selected for the analysis if the information they contained was relevant to the research question. Within the chosen dataset, codes were created inductively, meaning that parts of information were systematically selected from the dataset and assigned a code, without predefined criteria determining the content of the codes. The goal of coding was to organize the data into meaningful groups. Codes were then collated in themes and subthemes, bringing similar codes together to find patterns of meaning within the data. Thematic maps were used to organize the codes into initial themes and subthemes. The analysis process was iterative, meaning that codes and themes were revised, added, or cut several times throughout the analysis. As the original data are in German, the results, including exemplary data extracts, were translated into English by the interviewer.
To complement the results generated in the process of the reflexive thematic analysis, we additionally followed a codebook approach based on the structuring content analysis by Mayring (Mayring, 2022), slightly adapted for the purpose of our analysis. To this end, the interviewer deductively created a coding frame consisting of eight categories, each corresponding to one question of interest (e.g., interest in participating in a MBI during hospitalization). Within six of eight categories, there were three subcategories (agreed, disagreed, or uncertain about the question of interest). The remaining two categories aimed at identifying the suggested duration of mindfulness-based exercises in the ambulant and acute phase of COPD. These categories did not have any subcategories. The coding frame provided definitions and coding rules for each category and subcategory. The data set was analyzed by the interviewer and by an additional independent coder (postgraduate psychology student) using the coding frame. As opposed to the reflexive thematic analysis, in this analysis, the coders sought specific information and structured it according to the predefined categories. Following the recommendations for codebook approaches (O’Connor & Joffe, 2020), intercoder reliability was calculated for each (sub)category (Krippendorff’s alpha, calculated in IBM SPSS Statistics, version 24, using the KALPHA macro by Hayes & Krippendorff, 2007), and in the case of insufficient reliability scores (≤ 0.75) (sub)categories were reviewed and discussed until consensus was reached. The final intercoder reliabilities ranged from 0.95 to 1.00. Finally, frequencies of the (sub)categories were analyzed descriptively, together with the sociodemographic and medical data as well as the CAT scores (software: IBM SPSS Statistics, version 24).
Results
Sample Description
The following participant information is relevant for characterizing the patient sample to determine whether it corresponds or is representative of the population of patients hospitalized after AECOPD. The final sample (see Online Resource 2 for detailed data on the individual level) consisted of 20 COPD patients (age: M = 70.85 years, SD = 7.53, range: 57–87, 65% women) with a mostly lower educational level (75% apprenticeship or vocational school) and no need of home care (60%). 90% of the sample were in an advanced stage of the disease (GOLD stage III or IV) with a mean predicted forced expiratory volume in one second (FEV1) of 36.03% (SD = 12.45, range: 20.60–57.00). Patients’ health impairment was moderate (CAT score: M = 18.33, SD = 8.08, range: 4–29), as was their momentary impairment due to COPD on the day of the interview (M = 2.40, SD = 1.77, range: 0–4), as assessed by the interview’s entry question. On average, patients had been hospitalized 1.33 times (SD = 2.14, range: 0–9) for AECOPD within the last year. Most patients currently had a comorbid somatic disorder (70%) and 40% had been diagnosed with a psychiatric disorder in the past (thereof 60% depression, 30% anxiety, 10% substance abuse). The sample mainly consisted of previous heavy smokers (75%) with a mean pack-years score of 47.79 (SD = 30.08, range: 0.01–120). 70% of the patients reported previous contact with psychologists, psychotherapists, or psychiatrists and 55% stated previous experiences with mind-body practices (thereof most commonly autogenic training), which mainly occurred in the context of rehabilitation programs.
Interview Data
The interview data were analyzed to investigate whether MBIs are feasible for patients hospitalized for AECOPD and to identify implementation and adaptation criteria for the future implementation of MBIs in this specific patient group.
Regarding the data analyzed using the codebook approach, the results showed that 65% of the patients reported having heard of mindfulness before and 65% (15% were uncertain) believed that MBIs might be beneficial for them or other COPD patients. Most of the interviewed patients (65%; 5% were uncertain) would be interested in taking part in an MBI in the hospital setting and 35% (45% were uncertain) would be interested in taking part in an MBI in the outpatient setting. Half of the participants (10% were uncertain) would also be interested in taking part in a digital MBI (75% owned a smartphone). Some of the patients (40%; 35% were uncertain) could also imagine practicing MBI exercises daily in their everyday life but believed that the exercises should generally not last for more than 30 min (M = 30.00, SD = 15.68, range: 10–60).
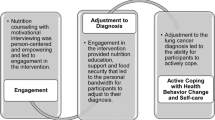
Using the reflexive thematic analysis, five overarching themes were generated to answer the research question regarding the feasibility of MBIs for patients hospitalized for AECOPD and potential implementation and adaptation criteria (see Fig. 1 for an overview of themes and subthemes and Online Resource 3 for the full final thematic map).
Theme 1 – Openness to New Treatment Approaches to Cope with COPD
Most patients expressed an openness to new treatments and to engaging in a new activity that might help them to cope with COPD—in the stable phase, but especially during acute exacerbations (“When you have COPD, at least starting from stage III, you feel it every day. I mean every day. […] I think at this point everyone is open to engaging with something new that could make everyday life a little bit easier”, ID 11). This openness did not solely include MBIs but also covered a general need for interventions focusing on well-being and mental health. The need to actively cope with the disease arose from a feeling of helplessness, a limited ability to act, and a loss of (symptom) control, as well as panic and fear, which were especially prominent during exacerbations (“Then you can tell yourself whatever you want. I know, sit down, I tell myself, breathe, breathe deeply. Nothing. I was in total panic”, ID 5). While patients were grateful for the care provided by family and physicians, they felt that treatments—mostly referring to medication—were only partially effective (“And as I said, I think I am receiving the best treatment, but (…) it has its limits”, ID 9) and negative side effects sometimes further impaired their mental and somatic health. Many patients expressed an active health consciousness, and most had already taken action to manage their symptoms through various strategies (e.g., posture, breathing exercises, pacing), although these were often described as insufficient (“I mean (…), I can reduce it [dyspnea] very rarely with breathing exercises”, ID 9). Moreover, some patients stated the necessity to act now to maintain their functional status or prevent future exacerbations (“And then I said, now it is over, now something has to happen”, ID 7), which further contributed to their openness to new treatments like MBIs.
Theme 2 – Understanding of Mindfulness Varies and is Difficult to Separate from Other Mind-Body Practices
The understanding of mindfulness varied widely within the sample and did not substantially change after the introductory explanation. While some patients were completely unfamiliar with the term, others defined it as being careful (“I am mindful when I cross the street”, ID 1), some thought of mindfulness as a way of living, and Patient 3 recited the definition of mindfulness by Jon Kabat-Zinn. Patients’ previous experiences with mindfulness and other mind-body practices likewise varied and affected their understanding of the concept. However, mindfulness was difficult to separate from other mind-body practices like yoga, relaxation and meditation exercises, and was related to these concepts (“This reminds me a little bit of the autogenic training”, ID 2).
Theme 3 – Expectations of the Effectiveness of MBIs and Previous Experiences with Mind-Body Practices Determine Interest in MBIs
For most patients, the fulfilment of their individual expectations regarding the effectiveness of MBIs was a central component determining their interest in (regularly) conducting mindfulness-based exercises (“You know, if I see that it [mindfulness-based exercises] helps me, then I will also do it. If I don’t see that, it will disappear in a drawer somewhere”, ID 2). The effectiveness of an MBI would mostly manifest in improvements in dyspnea, panic, and anxiety, general health status and well-being, symptom control, calmness, and relaxation. Some patients also hoped that MBIs would distract them from dyspnea or panic (“That I would be more relaxed in general. That I am not so focused on my breathing. […] I can imagine that these [mindfulness-based] exercises could distract me, it’s that simple”, ID 16). Individual experiences with MBIs and other mind-body practices further influenced patients’ interest. While many patients had positive previous experiences with mind-body practices and perceived them as pleasant, relaxing, and as fostering their perception (“I think this [mindfulness-based exercise] was very calming, also for my breathing”, ID 21), some patients had not experienced beneficial effects of mindfulness-based or related exercises in the past (“For me personally, I did not feel anything. Nothing different than usual”, ID 18) and were therefore not interested in MBIs.
Theme 4 – Context Factors of MBIs are More Important than Content Factors
Patients reported the timing of the intervention as an essential factor and most patients thought that MBIs would not be feasible during AECOPD due to feelings of panic and an impaired ability to act (“In an acute case when I’m sitting at home and hoping that I will survive the time until the paramedics ring at my door, I will not do something like this [mindfulness-based exercise]”, ID 11). However, they might be beneficial before or after AECOPD, or during the stable phase. Some patients further verbalized the wish for an initial guided introduction in order to obtain more information and to learn and practice how to self-administer MBIs correctly (“To learn it. (…) Because I might not do it [mindfulness exercises] right. So, to practice it under guidance, at least once”, ID 3). Most patients expressed the need for short and simple exercises which are not physically demanding. Some patients felt that it was important how the exercises are guided and referred to characteristics of the trainer, such as a motivating personality and pleasant voice. Some patients wished for personal contact with the trainer or other participants, while others emphasized that it should be possible to implement the exercises in everyday life, carry them out independently, and select them individually, and that MBIs should be adapted to individual needs and preferences (“And everyone has to find out themselves which exercises they need. […] So, I think you find out your own (…) emergency help, somehow”, ID 6). Some patients could imagine using technology to self-administer MBIs; however, most stated that they would require technical support for this (“Yes, if you are installing it [MBI], because I am a moron with this [technology]”, ID 16). In contrast to context factors, the content of the MBI was less important for patients, and none of the patients stated a preference for specific exercises (“I think everything that is a little bit (…) calming”, ID 6). Three patients wished for a focus on COPD-related issues within the exercises (“I (…) would expect it to (…), if it [mindfulness exercise] would focus on the lungs and on the breath”, ID 9).
Theme 5 – General Barriers and COPD-Specific Limitations Hinder the (Regular) Self-administration of MBIs
Patients described several general barriers such as scheduling or time issues, lack of motivation, and difficulties engaging in and maintaining attention on the exercises as hindering factors for the self-administration of an MBI, especially on a daily basis (“Erm, with daily things it’s always a little bit difficult. (…) You are retired, but you have less time, it is like that”, ID 5). Decreased mobility and physical limitations due to COPD would also hinder the participation in MBIs for most patients (“I would be interested, but how do I get there? That’s the issue”, ID 2). Some patients also reported being stretched with other treatments, leaving no space for additional activities, or felt that COPD symptoms would impair the (regular) self-administration of MBIs.
Discussion
The results of this exploratory qualitative study indicate that among the patients hospitalized for AECOPD who were interviewed, there was a notable interest in MBIs and similar add-on treatment approaches that may help them cope with COPD. However, MBIs should be adapted to the needs of this patient group, considering specific context factors (e.g., timing), general barriers (e.g., time issues) and COPD-related limitations (e.g., decreased mobility), as they substantially influence patients’ interest and motivation as well as the feasibility of MBIs.
Openness to new treatment approaches to cope with COPD. The reported emotional states during exacerbations (e.g., helplessness) indicate that exacerbations were often appraised as stressful (Lazarus & Folkman, 1984). This supports previous findings that breathing problems are a major stressor for hospitalized COPD patients (Andenæs et al., 2006; Halpin et al., 2015). Experiencing these symptoms is often linked to a perceived need to cope with the disease and a consequent interest in MBIs found in our data. Our findings complement theoretical proposals that mental health interventions for patients hospitalized for AECOPD—such as MBIs—may benefit from not only targeting symptoms of anxiety and depression, but also stress, which has been overlooked in many previous studies in this field.
Some patients stated a very high treatment motivation after AECOPD and a need to act now, which might indicate particularly high treatment motivation in this subgroup and suggests that an appropriate timing of MBIs would be after AECOPD (discussed in the paragraph regarding Theme 4). Our findings, connecting high treatment motivation with patients experiencing limited effects of their current treatment, may underscore the importance of non-medical add-on treatments for this population. The active health consciousness reported by many patients in our sample may indicate their awareness of the necessity of their active involvement in treatment. However, they might lack information about symptom self-management, including professional, comprehensible, and implementable strategies, especially for their everyday lives. It might be that due to this lack of information combined with the necessity to cope with COPD, patients come up with their own strategies, which, however, were often described as insufficient in our sample. This may highlight the need for more education about suitable self-management strategies, which were also recommended by the international guidelines for COPD (Global Initiative for Chronic Obstructive Lung Disease, 2023).
Patients’ understanding of mindfulness varied widely and was difficult to separate from other mind-body practices. When talking about mindfulness, patients mainly focused on active engagement, being careful or aware (e.g., regarding symptoms), and on aspects of effectiveness and helpfulness (i.e., symptom relief), which also represented central components for their interest in MBIs. While relief is commonly seen in lay definitions of mindfulness, scientific definitions mostly see relief as a possible outcome (Choi et al., 2021). However, professionals’ definitions do include acceptance (Bishop et al., 2004), which was virtually absent in the patients’ definitions. Researchers should consider this discrepancy and reflect on its implications for the implementation of MBIs (e.g., provide detailed information about mindfulness).
Expectations of the effectiveness of MBIs and previous experiences with mind-body practices determine patients’ interest in MBIs. The data further suggest that most patients were mainly interested in the effects of MBIs (e.g., relaxation, calmness, better health status). By contrast, the actual contents of the activity seem less important for most patients in our sample, which also reflects their broader interest in MBIs and similar techniques. However, patients’ desired treatment outcomes might not always be realistic. While previous research suggests that dyspnea, well-being, symptom control, or symptoms of anxiety and depression as well as stress might be improved by MBIs (Chan & Lehto, 2016; Goldberg et al., 2021; Malpass et al., 2015; Tan et al., 2019), research is inconclusive regarding the potential of MBIs to improve physical health status in long-term conditions (Crowe et al., 2016). Individual expectations should be addressed and discussed with the patients, as realistic treatment expectations might improve adherence and prevent dropouts.
Context factors of MBIs are more important than content factors. As most patients in our sample would be interested in carrying out an MBI during their hospitalization, the hospital may be a suitable setting (also discussed by Clari et al., 2020). While MBIs seemed unfeasible to most interviewed patients during severe AECOPD, practicing mindfulness to calm down during mild dyspnea, or before and after AECOPD, might be a promising option for MBIs in the hospital setting, as reported in our data and proposed elsewhere (Clari et al., 2020). In this vein, another study found that a brief MBI implemented right after AECOPD was rated as useful by most hospitalized patients (Perkins-Porras et al., 2018). However, so far, there is no evidence supporting that MBIs implemented right after AECOPD might be effective in reducing psychological or somatic outcomes (Perkins-Porras et al., 2018).
The relatively low interest in MBIs in the outpatient health care setting reported by many participants might be explained by the reported decreased mobility, which might hinder participation or increase the effort involved, in turn affecting their motivation. Motivation might improve by offering necessary support like transportation for interventions in the outpatient setting (e.g., ambulant pulmonary rehabilitation).
Further, digital interventions could be implemented in health care settings and in everyday life, which would not only overcome barriers like decreased mobility but would also allow patients to maintain their mindfulness practice in the long term, thus enabling lasting changes (Watson & Wilkinson, 2022). While digital MBIs are increasingly implemented in different healthy and clinical populations and have been shown to effectively reduce psychological outcomes (Mrazek et al., 2019; Tan et al., 2022), only half of the patients in the present study would be interested in digital MBIs, and most of these stated that they would need technical support for a digital implementation of MBIs.
A guided introduction to the intervention, including (psychoeducational) information and a practice phase, seemed to be important to most patients in our sample and might ease patients into the intervention and familiarize them with the concept of mindfulness. Additionally, familiarity with different relaxation techniques was found to influence which technique patients preferred in previous research, and might increase patients’ motivation and treatment adherence (Hyland et al., 2016). This phenomenon is also reflected in our data, as previous experiences with MBIs and other mind-body practices often strongly influenced the patients’ interest.
Previous studies reported beneficial effects of mindful movement interventions (e.g., qigong) on respiratory parameters and health-related quality of life in COPD (Wu et al., 2018), and physical exercise training is a crucial component of most health care programs for COPD patients (Global Initiative for Chronic Obstructive Lung Disease, 2023). However, exercises including any movement did not appear feasible to the majority of the interviewed sample. This might be explained by a greater fear of physical activity—which is connected to dyspnea (Hanania & O’Donnell, 2019)—in patients hospitalized for AECOPD, or may be attributable to a higher acceptance of and familiarity with mindful movement exercises in Eastern samples, in which these interventions have mainly been investigated (Wu et al., 2018). Movement elements might be too burdensome for patients who have just experienced AECOPD but mind-body practices should not be ruled out for COPD patients in general—and even for those with frequent AECOPD—as mindful movement may help overcome the fear of physical activity and interrupt the dyspnea-inactivity cycle in COPD (Ramon et al., 2018).
Most patients in our study further wished for short and easy-to-learn exercises, which is consistent with previous literature (Harrison et al., 2017) and has been addressed in previous studies by reducing the length of MBI sessions (e.g., Farver-Vestergaard et al., 2018). However, these time reductions may not have been sufficient (in the case of MBSR or MBCT), as the interviewed patients reported a preference for very short exercises under 30 min. Hence, brief MBIs might be more appropriate for patients hospitalized for AECOPD. However, a regular practice and longer guidance might be necessary to maintain long-term changes and the self-administration of MBIs in everyday life (Creswell, 2017; Taylor et al., 2021).
Some studies investigating MBIs in COPD also made adaptations regarding the focus on COPD- or dyspnea-related issues (e.g., Chan et al., 2015), and some of the patients in our study explicitly wished for such adaptations. As proposed by other researchers, it may be beneficial to add mindful awareness to mechanical respiratory exercises, which could possibly improve physical and mental health outcomes (Benzo, 2013). On the other hand, a focus on the breath might be distressing for patients with AECOPD. This argument speaks for the implementation of a different focus (anchor) within the exercises (e.g., heartbeat) instead of the breath, as implemented elsewhere (Farver-Vestergaard et al., 2018).
General barriers and COPD-specific limitations hinder the (regular) self-administration of MBIs. Importantly, many of the interviewed patients reported physical limitations and decreased mobility, which have been identified as reasons for dropouts in other studies (e.g., Mularski et al., 2009). These barriers might be overcome by using digital interventions, which are easily accessible and can be conducted in hospital settings and everyday life. Digital MBIs have already been shown to be feasible in elderly populations (e.g., Palta et al., 2012) and to improve adherence in intervention programs with COPD patients (Watson & Wilkinson, 2022). Moreover, digital MBIs could be adapted to individual needs and preferences, enabling individualized care programs.
Finally, it should also be highlighted that some patients in our sample were not interested in carrying out any form of MBI, mainly because they did not think that MBIs would be beneficial/effective or did not feel the need for any further support/treatment. There are various potential reasons for this, such as differing levels of health awareness, low psychological distress or symptom burden, negative preconceptions about mindfulness, etc. One explanation, which is often reported in the literature, is that some people may have a predisposition to being mindful while others may not (e.g., discussed in Clari et al., 2020). Therefore, future studies should investigate characteristics of people who particularly benefit from MBIs, enabling the implementation of MBIs as a targeted add-on intervention.
Limitations and Future Research
The present study is the first to investigate the feasibility and implementation criteria of MBIs in patients hospitalized for AECOPD, applying an exploratory qualitative approach. Qualitative research is often overlooked in medical fields, but exploring patients’ views enables interventions to be adapted to patients’ needs and limitations, which may have crucial impact on adherence (Rogliani et al., 2017). This is especially relevant for the COPD population, which is a highly impaired, hard-to-reach group with often poor treatment adherence (Rogliani et al., 2017).
However, some limitations must be considered when interpreting the results of this study. The sample consisted of patients hospitalized for AECOPD, which may limit the generalizability to COPD outpatients and to COPD patients hospitalized for other reasons. The sample was a convenience sample recruited within one institution, limiting its representativeness and external validity. Moreover, the study might have attracted relatively motivated patients with broader previous experiences regarding MBIs, which could have led to a self-selection bias and a low heterogeneity in the sample. Additionally, it should be noted that due to the varying understanding of mindfulness within the sample, the results may not be specific to MBIs but could instead refer to relaxing and calming exercises in general (e.g., relaxation exercises). Additional coders might have improved the validity of the codebook analysis.
Future large-scale intervention studies investigating the feasibility and effects of MBIs and similar techniques in patients hospitalized for AECOPD are needed. They may target symptoms of anxiety, depression, subjective stress, and biological correlates of stress, while also assessing COPD specific outcomes like dyspnea. MBIs could help patients in regaining symptom control, relaxation, and coping with the disease, with professionals informing patients about the intervention’s self-management potential. Patients’ understanding of mindfulness as well as their expectations regarding the effects of MBIs should be considered by researchers and practitioners and should be discussed with patients when implementing an MBI. MBIs could be delivered in the hospital or outpatient setting, while providing the necessary support like transportation. However, MBIs should not be implemented during AECOPD. MBIs should be easy to learn and carry out and should contain a range of short exercises up to 30 min, which are not physically demanding. Furthermore, an initial learning and practice phase with psychoeducational content should be implemented. Digital MBIs could be considered for investigation, as they increase adherence and feasibility both in hospital and in everyday life, while making the intervention accessible for patients with decreased mobility and with physical limitations. For a better understanding of how MBIs could function as self-management tools for COPD patients in their daily lives, it would be interesting to conduct ecological momentary assessment studies. These studies could explore daily dynamics of psychological and respiratory outcomes and immediate effects of the intervention within a naturalistic setting. Especially ecological momentary interventions could be worth considering in future studies, as they allow the targeted delivery and assessment of MBIs when they are needed, for example in situations of increased dyspnea.
Data Availability
De-identified data from this study are not available in a public archive but are available by contacting the corresponding author.
References
Andenæs, R., Kalfoss, M. H., & Wahl, A. K. (2006). Coping and psychological distress in hospitalized patients with chronic obstructive pulmonary disease. Heart and Lung: Journal of Acute and Critical Care, 35(1), 46–57. https://doi.org/10.1016/j.hrtlng.2005.09.009.
Benzo, R. P. (2013). Review series: Collaborative self-management mindfulness and motivational interviewing: Two candidate methods for promoting self-management. Chronic Respiratory Disease, 10(3), 175–182. https://doi.org/10.1177/1479972313497372.
Bishop, S. R., Lau, M., Shapiro, S., Carlson, L., Anderson, N. D., Carmody, J., Segal, Z. V., Abbey, S., Speca, M., Velting, D., & Devins, G. (2004). Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice, 11(3), 230–241. https://doi.org/10.1093/clipsy/bph077.
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/10.1191/1478088706qp063oa.
Braun, V., & Clarke, V. (2013). Successful qualitative research: A practical guide for beginners. 14. SAGE.
Braun, V., & Clarke, V. (2019). Reflecting on reflexive thematic analysis. Qualitative Research in Sport Exercise and Health, 11(4), 589–597. https://doi.org/10.1080/2159676X.2019.1628806.
Braun, V., & Clarke, V. (2020). One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qualitative Research in Psychology, 18(3), 328–352. https://doi.org/10.1080/14780887.2020.1769238.
Cambridge University Press & Assessment (2024). Cambridge free dictionary and thesaurus. https://dictionary.cambridge.org/dictionary/. Accessed 7 May 2024
Chan, R. R., & Lehto, R. H. (2016). The experience of learning meditation and mind/body practices in the COPD population. Explore: The Journal of Science and Healing, 12(3), 171–179. https://doi.org/10.1016/j.explore.2016.02.004.
Chan, R. R., Giardino, N., & Llarson, J. (2015). A pilot study: Mindfulness meditation intervention in COPD. International Journal of COPD, 10(1), 445–454. https://doi.org/10.2147/COPD.S73864.
Choi, E., Farb, N., Pogrebtsova, E., Gruman, J., & Grossmann, I. (2021). What do people mean when they talk about mindfulness? Clinical Psychology Review, 89, 102085. https://doi.org/10.1016/j.cpr.2021.102085.
Clari, M., Conti, A., Fontanella, R., Rossi, A., & Matarese, M. (2020). Mindfulness-based programs for people with chronic obstructive pulmonary disease: A mixed methods systematic review. Mindfulness, 11(8), 1848–1867. https://doi.org/10.1007/s12671-020-01348-z.
Creswell, J. D. (2017). Mindfulness interventions. Annual Review of Psychology, 68, 491–516. https://doi.org/10.1146/annurev-psych-042716-051139.
Crowe, M., Jordan, J., Burrell, B., Jones, V., Gillon, D., & Harris, S. (2016). Mindfulness-based stress reduction for long-term physical conditions: A systematic review. Australian and New Zealand Journal of Psychiatry, 50(1), 21–32. https://doi.org/10.1177/0004867415607984.
Farver-Vestergaard, I., O’Connor, M., Smith, N. C., Løkke, A., Bendstrup, E., & Zachariae, R. (2018). Tele-delivered mindfulness-based cognitive therapy in chronic obstructive pulmonary disease: A mixed-methods feasibility study. Journal of Telemedicine and Telecare, 25(8), 468–475. https://doi.org/10.1177/1357633X18780563.
Farver-Vestergaard, I., O’Toole, M. S., O’Connor, M., Lokke, A., Bendstrup, E., Basdeo, S. A., Cox, D. J., Dunne, P. J., Ruggeri, K., Early, F., & Zachariae, R. (2018b). Mindfulness-based cognitive therapy in COPD: A cluster randomised controlled trial. European Respiratory Journal, 51, 1702082–1702082. https://doi.org/10.1183/13993003.02082-2017
Global Initiative for Chronic Obstructive Lung Disease (2023). Global strategy for prevention, diagnosis and management of COPD: 2023 report. https://goldcopd.org/2023-gold-reports-2/. Accessed 6 Oct 2023
Goldberg, S. B., Riordan, K. M., Sun, S., & Davidson, R. J. (2021). The empirical status of mindfulness-based interventions: A systematic review of 44 meta-analyses of randomized controlled trials. Perspectives on Psychological Science, 17(1), 108–130. https://doi.org/10.1177/1745691620968771.
Gordon, C. S., Waller, J. W., Cook, R. M., Cavalera, S. L., Lim, W. T., & Osadnik, C. R. (2019). Effect of pulmonary rehabilitation on symptoms of anxiety and depression in COPD: A systematic review and meta-analysis. Chest, 156(1), 80–91. https://doi.org/10.1016/j.chest.2019.04.009.
Gutiérrez Villegas, C., Paz-Zulueta, M., Herrero-Montes, M., Parás-Bravo, P., & Madrazo Pérez, M. (2021). Cost analysis of chronic obstructive pulmonary disease (COPD): A systematic review. Health Economics Review, 11(1), 1–12. https://doi.org/10.1186/S13561-021-00329-9.
Halpin, D., Hyland, M., Blake, S., Seamark, C., Pinnuck, M., Ward, D., Whalley, B., Greaves, C., Hawkins, A., & Seamark, D. (2015). Understanding fear and anxiety in patients at the time of an exacerbation of chronic obstructive pulmonary disease: A qualitative study. JRSM Open, 6(12), 2054270415614543. https://doi.org/10.1177/2054270415614543
Hanania, N. A., & O’Donnell, D. E. (2019). Activity-related dyspnea in chronic obstructive pulmonary disease: Physical and psychological consequences, unmet needs, and future directions. International Journal of Chronic Obstructive Pulmonary Disease, 14, 1127–1138. https://doi.org/10.2147/COPD.S188141.
Harrison, S. L., Lee, A., Goldstein, R. S., & Brooks, D. (2017). Perspectives of healthcare professionals and patients on the application of mindfulness in individuals with chronic obstructive pulmonary disease. Patient Education and Counseling, 100(2), 337–342. https://doi.org/10.1016/j.pec.2016.08.018.
Hayes, A. F., & Krippendorff, K. (2007). Answering the call for a standard reliability measure for coding data. Communication Methods and Measures, 1(1), 77–89. https://doi.org/10.1080/19312450709336664.
Holmes, T. H., & Rahe, R. H. (1967). The social readjustment rating scale. Journal of Psychosomatic Research, 11(2), 213–218. https://doi.org/10.1016/0022-3999(67)90010-4.
Hyland, M., Halpin, D. M., Blake, S., Seamark, C., Pinnuck, M., Ward, D., Whalley, B., Greaves, C. J., Hawkins, A., & Seamark, D. (2016). Preference for different relaxation techniques by COPD patients: Comparison between six techniques. International Journal of Chronic Obstructive Pulmonary Disease, 11(1), 2315–2319. https://doi.org/10.2147/COPD.S113108.
Jones, P. W., Harding, G., Berry, P., Wiklund, I., Chen, W. H., & Leidy, K., N (2009). Development and first validation of the COPD Assessment Test. European Respiratory Journal, 34(3), 648–654. https://doi.org/10.1183/09031936.00102509.
Kabat-Zinn, J. (2013). Full catastrophe living: How to cope with stress, pain and illness using mindfulness meditation. Hachette.
Kabat-Zinn, J. (2015). Mindfulness Mindfulness, 6, 1481–1483. https://doi.org/10.1007/s12671-015-0456-x
Kuckartz, U., Dresinger, T., Rädiker, S., & Stefer, C. (2008). Qualitative Evaluation [Qualitative evaluation] (2nd ed.). Verlag für Sozialwissenschaften.
Laurin, C., Moullec, G., Bacon, S. L., & Lavoie, K. L. (2012). Impact of anxiety and depression on chronic obstructive pulmonary disease exacerbation risk. American Journal of Respiratory and Critical Care Medicine, 185(9), 918–923. https://doi.org/10.1164/rccm.201105-0939PP.
Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal and coping. Springer Publication.
Long, J., Ouyang, Y., Duan, H., Xiang, Z., Ma, H., Ju, M., & Sun, D. (2020). Multiple factor analysis of depression and/or anxiety in patients with acute exacerbation chronic obstructive pulmonary disease. International Journal of Chronic Obstructive Pulmonary Disease, 15, 1449–1464. https://doi.org/10.2147/COPD.S245842.
Malpass, A., Kessler, D., Sharp, D., & Shaw, A. (2015). MBCT for patients with respiratory conditions who experience anxiety and depression: A qualitative study. Mindfulness, 6, 1181–1191. https://doi.org/10.1007/s12671-014-0370-7
Mayring, P. (2022). Qualitative inhaltsanalyse: Grundlagen und Techniken [Qualitative content analysis: Basics and techniques] (13th ed.). Beltz.
Mrazek, A. J., Mrazek, M. D., Cherolini, C. M., Cloughesy, J. N., Cynman, D. J., Gougis, L. J., Landry, A. P., Reese, J. V., & Schooler, J. W. (2019). The future of mindfulness training is digital, and the future is now. Current Opinion in Psychology, 28, 81–86. https://doi.org/10.1016/j.copsyc.2018.11.012.
Mularski, R. A., Munjas, B. A., Lorenz, K. A., Sun, S., Robertson, S. J., Schmelzer, W., Kim, A. C., & Shekelle, P. G. (2009). Randomized controlled trial of mindfulness-based therapy for dyspnea in chronic obstructive lung disease. The Journal of Alternative and Complementary Medicine, 15(10), 1083–1090. https://doi.org/10.1089/acm.2009.0037.
Nater, U. M., Skoluda, N., & Strahler, J. (2013). Biomarkers of stress in behavioural medicine. Current Opinion in Psychiatry, 26(5), 440–445. https://doi.org/10.1097/YCO.0b013e328363b4ed.
O’Connor, C., & Joffe, H. (2020). Intercoder reliability in qualitative research: Debates and practical guidelines. International Journal of Qualitative Methods, 19, 160940691989922. https://doi.org/10.1177/1609406919899220.
Oyler, D. L., Hulett, J. M., Pratscher, S. D., Price-Blackshear, M. A., Murphy, E. A., & Bettencourt, B. A. (2023). The influence of meditative interventions on immune functioning: A meta-analysis. Mindfulness, 14(8), 1815–1851. https://doi.org/10.1007/s12671-023-02157-w.
Palta, P., Page, G., Piferi, R. L., Gill, J. M., Hayat, M. J., Connolly, A. B., & Szanton, S. L. (2012). Evaluation of a mindfulness-based intervention program to decrease blood pressure in low-income African-American older adults. Journal of Urban Health, 89(2), 308–316. https://doi.org/10.1007/s11524-011-9654-6.
Perkins-Porras, L., Riaz, M., Okekunle, A., Zhelezna, S., Chakravorty, I., & Ussher, M. (2018). Feasibility study to assess the effect of a brief mindfulness intervention for patients with chronic obstructive pulmonary disease: A randomized controlled trial. Chronic Respiratory Disease, 15(4), 400–410. https://doi.org/10.1177/1479972318766140.
Pooler, A., & Beech, R. (2014). Examining the relationship between anxiety and depression and exacerbations of COPD which result in hospital admission: A systematic review. International Journal of Chronic Obstructive Pulmonary Disease, 9(1), 315–330. https://doi.org/10.2147/COPD.S53255.
Ramon, M. A., Ter Riet, G., Carsin, A. E., Gimeno-Santos, E., Agustí, A., Antó, J. M., Donaire-Gonzalez, D., Ferrer, J., Rodríguez, E., Rodriguez-Roisin, R., Puhan, M. A., & Garcia-Aymerich, J. (2018). The dyspnoea–inactivity vicious circle in COPD: Development and external validation of a conceptual model. European Respiratory Journal, 52(3), 1800079. https://doi.org/10.1183/13993003.00079-2018.
Reaves, C., & Angosta, A. D. (2021). The relaxation response: Influence on psychological and physiological responses in patients with COPD. Applied Nursing Research, 57, 151351. https://doi.org/10.1016/j.apnr.2020.151351.
Rogerson, O., Wilding, S., Prudenzi, A., & O’Connor, D. B. (2024). Effectiveness of stress management interventions to change cortisol levels: A systematic review and meta-analysis. Psychoneuroendocrinology, 159, 106415. https://doi.org/10.1016/j.psyneuen.2023.106415.
Rogliani, P., Ora, J., Puxeddu, E., Matera, M. G., & Cazzola, M. (2017). Adherence to COPD treatment: Myth and reality. Respiratory Medicine, 129, 117–123. https://doi.org/10.1016/j.rmed.2017.06.007.
Schiweck, C., Piette, D., Berckmans, D., Claes, S., & Vrieze, E. (2019). Heart rate and high frequency heart rate variability during stress as biomarker for clinical depression. A systematic review. Psychological Medicine, 49(2), 200–211. https://doi.org/10.1017/S0033291718001988.
Segal, Z. V., Williams, M. T., & Teasdale, J. D. (2018). Mindfulness-based cognitive therapy for depression (2nd ed.). Guilford Press.
Singh, S., Verma, S. K., Kumar, S., Ahmad, M. K., Nischal, A., Singh, S. K., & Dixit, R. K. (2018). Correlation of severity of chronic obstructive pulmonary disease with potential biomarkers. Immunology Letters, 196, 1–10. https://doi.org/10.1016/j.imlet.2018.01.004.
Smith, S. M., Sonego, S., Ketcheson, L., & Larson, J. L. (2014). A review of the effectiveness of psychological interventions used for anxiety and depression in chronic obstructive pulmonary disease. BMJ Open Respiratory Research, 1(1), e000042. https://doi.org/10.1136/bmjresp-2014-000042.
Tan, S. B., Liam, C. K., Pang, Y. K., Leh-Ching Ng, D., Wong, T. S., Wei-Shen Khoo, K., Ooi, C. Y., & Chai, C. S. (2019). The effect of 20-minute mindful breathing on the rapid reduction of dyspnea at rest in patients with lung diseases: A randomized controlled trial. Journal of Pain and Symptom Management, 57(4), 802–808. https://doi.org/10.1016/j.jpainsymman.2019.01.009.
Tan, Z. Y. A., Wong, S. H., Cheng, L. J., & Lau, S. T. (2022). Effectiveness of mobile-based mindfulness interventions in improving mindfulness skills and psychological outcomes for adults: A systematic review and meta-regression. Mindfulness, 13(10), 2379–2395. https://doi.org/10.1007/s12671-022-01962-z
Taylor, H., Strauss, C., & Cavanagh, K. (2021). Can a little bit of mindfulness do you good? A systematic review and meta-analyses of unguided mindfulness-based self-help interventions. Clinical Psychology Review, 89, 102078. https://doi.org/10.1016/j.cpr.2021.102078.
Van Gestel, A., Kohler, M., & Clarenbach, C. (2012). Sympathetic overactivity and cardiovascular disease in patients with chronic obstructive pulmonary disease (COPD). Discovery Medicine, 14(79), 359–368.
Watson, A., & Wilkinson, T. M. A. (2022). Digital healthcare in COPD management: A narrative review on the advantages, pitfalls, and need for further research. Therapeutic Advances in Respiratory Disease, 16, 175346662210754. https://doi.org/10.1177/17534666221075493.
World Health Organization (2020). Global health estimates: Life expectancy and leading causes of death and disability. https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates. Accessed 9 Mar 2022
Wu, L. L., Lin, Z. K., Weng, H. D., Qi, Q. F., Lu, J., & Liu, K. X. (2018). Effectiveness of meditative movement on COPD: A systematic review and meta-analysis. International Journal of COPD, 13, 1239–1250. https://doi.org/10.2147/COPD.S159042.
Zhang, D., Lee, E. K. P., Mak, E. C. W., Ho, C. Y., & Wong, S. S. Y. (2021). Mindfulness-based interventions: An overall review. British Medical Bulletin, 138(1), 41–57. https://doi.org/10.1093/BMB/LDAB005.
Zorn, J. V., Schür, R. R., Boks, M. P., Kahn, R. S., Joëls, M., & Vinkers, C. H. (2017). Cortisol stress reactivity across psychiatric disorders: A systematic review and meta-analysis. Psychoneuroendocrinology, 77, 25–36. https://doi.org/10.1016/j.psyneuen.2016.11.036.
Acknowledgements
We would like to thank our project assistant Katrin Schäfer for serving as a second coder and the physicians at the respiratory unit at the Klinik Ottakring for supporting the recruitment of the study participants.
Funding
Open access funding provided by University of Vienna. The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
Hannah Tschenett: Conceptualization, Methodology, Investigation, Data curation, Formal analysis, Writing – original draft, Visualization. Georg-Christian Funk: Conceptualization, Project administration, Resources, Supervision, Writing - review & editing. Florian Vafai-Tabrizi: Conceptualization, Investigation, Writing - review & editing. Urs M. Nater: Conceptualization, Methodology, Resources, Supervision, Validation, Writing - review & editing.
Corresponding author
Ethics declarations
Ethics Statement
The study was conducted in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments and was approved by the ethics review board of the City of Vienna (serial number EK 19–202 VK).
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Use of Artificial Intelligence
AI was used for editing the manuscript to improve English language.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tschenett, H., Funk, GC., Vafai-Tabrizi, F. et al. Patient Perspectives on Mindfulness-Based Interventions During Hospitalization for Acute Exacerbations of Chronic Obstructive Pulmonary Disease: An Exploratory Interview Study. Mindfulness (2024). https://doi.org/10.1007/s12671-024-02387-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s12671-024-02387-6